Published online Aug 6, 2024. doi: 10.12998/wjcc.v12.i22.5258
Revised: May 23, 2024
Accepted: June 11, 2024
Published online: August 6, 2024
Processing time: 68 Days and 7.6 Hours
Hemolymphangioma is a very rare benign tumor in clinical practice caused by abnormalities of the vasculature. Its clinical features are often atypical, and it is easy to miss and misdiagnose. When the time of nuclear magnetic T1 is significantly reduced, the diagnosis of hemangioma should be considered. Therefore, we report this case in the hope of raising clinicians' awareness of the disease.
A 37-year-old man presented with a giant retroperitoneal hemolymphangioma. Computed tomography and magnetic resonance imaging indicated the possibility of a large perirenal lymphatic cyst. The postoperative pathological diagnosis is retroperitoneal hemolymphangioma. The patient underwent surgical excision after adequate drainage. The postoperative recovery was smooth and there were no complications. There was no recurrence during half a year of follow-up.
This case reiterates that large retroperitoneal cystic masses with significantly shortened nuclear T1 time should be considered hemolymphangioma. Specific clinical basis and experience for the diagnosis and treatment of these diseases is necessary.
Core Tip: The clinical features of hemolymphangioma are often atypical, and it is easy to miss and misdiagnose. When the time of nuclear magnetic T1 is significantly reduced, the diagnosis of hemolymphangioma should be considered. Retroperitoneal hemolymphangiomas are usually very large and puncture drainage can be an early treatment option.
- Citation: Wang YK, Liu YH, Shuang WB. Giant retroperitoneal hemolymphangioma: A case report and review of literature. World J Clin Cases 2024; 12(22): 5258-5262
- URL: https://www.wjgnet.com/2307-8960/full/v12/i22/5258.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i22.5258
Hemolymphangioma is divided into primary and secondary tumors. Primary hemolymphangioma is a congenital malformation of the vascular system, which may be related to obstruction of the venous lymphatic pathway between the abnormal vascular tissue and the systemic circulation. Secondary hemolymphangioma is usually caused by inadequate lymphatic drainage due to injury of lymphatic vessels caused by trauma or surgery[1]. It has been reported in pancreas, limbs, neonatal mediastinum, chest wall, anterior mediastinum, posterior mediastinum, pericardium, tongue, orbit, retroperitoneum, esophagus, cervix, adrenal gland, kidney, liver, and spleen. However, there are few reports of retroperitoneal hemolymphangioma[1-5]. In this study, we report a case of giant retroperitoneal hemolymphangioma and discuss the clinical, imaging, and treatment options based on the literature.
A 37-year-old male patient presented with upper abdominal distension and discomfort, accompanied by low back pain.
Two months ago, the patient presented with upper abdominal distension and discomfort, accompanied by low back pain without apparent causes.
He had no past medical history.
He had no past family history.
On physical examination, the abdomen was distended, and a large abdominal mass was palpated.
Laboratory tests showed no abnormalities.
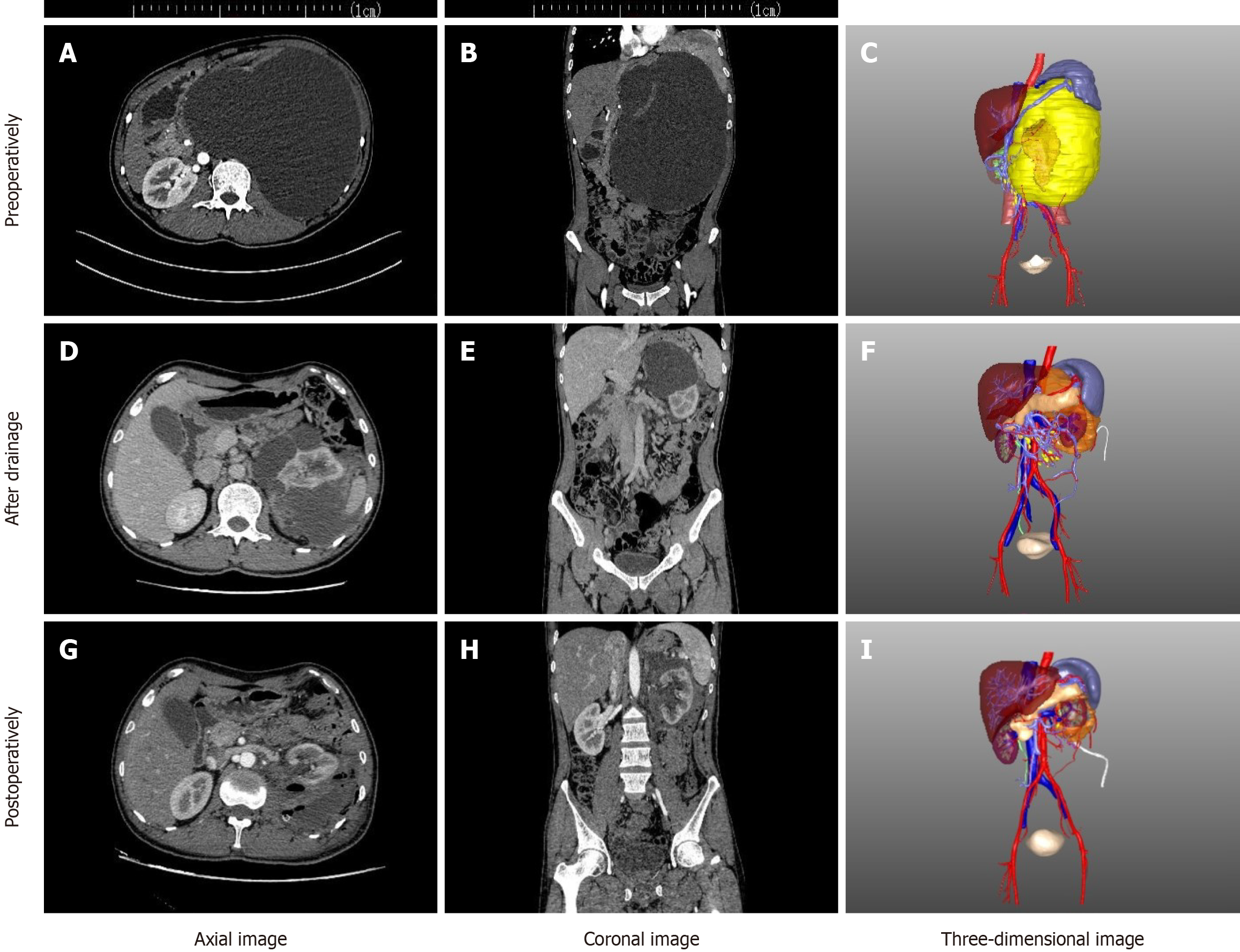
One month prior to presentation to our hospital, the patient's symptoms worsened, and a computed tomography (CT) examination performed at the local hospital revealed a giant hepatic cyst. In our hospital, the enhanced CT and magnetic resonance imaging revealed a left retroperitoneal cystic mass and a giant left perirenal lymphangioma. The lesion extended along the left kidney and wrapped around the left kidney (Figure 1).
Finally diagnosed as giant retroperitoneal hemolymphangioma.
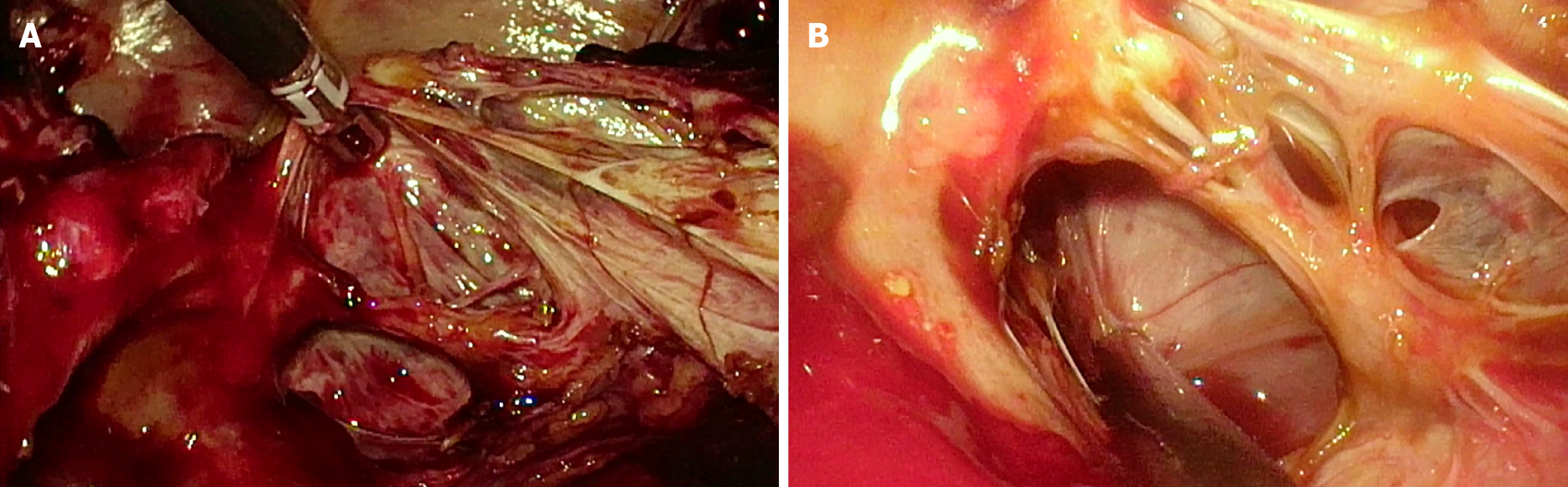
In order to relieve compression symptoms and make a better diagnosis, we performed ultrasound-guided percutaneous nephrostomy, which drained a large amount of dark red fluid. Histopathological examination of the drainage fluid showed the presence of histiocytes and inflammatory cells. On the fifth day after the operation, enhanced CT of the urinary system showed that the scope of the lesion was reduced, and the patient was discharged on the same day. Approximately 7000 mL of drainage fluid was drained by intermittent clamping after the operation. The patient underwent adequate drainage for 2 wk before readmission, at which he had lost approximately 25 kg of body weight. During the operation, multiple cystic and solid masses on the surface of the kidney were found, and dark red blood fluid flowed out after the incision of the cyst wall. Multiple follicular masses and cord-like tissues were observed in the cyst. Part of the cord-like tissue was removed and subjected to pathological examination (Figure 2).
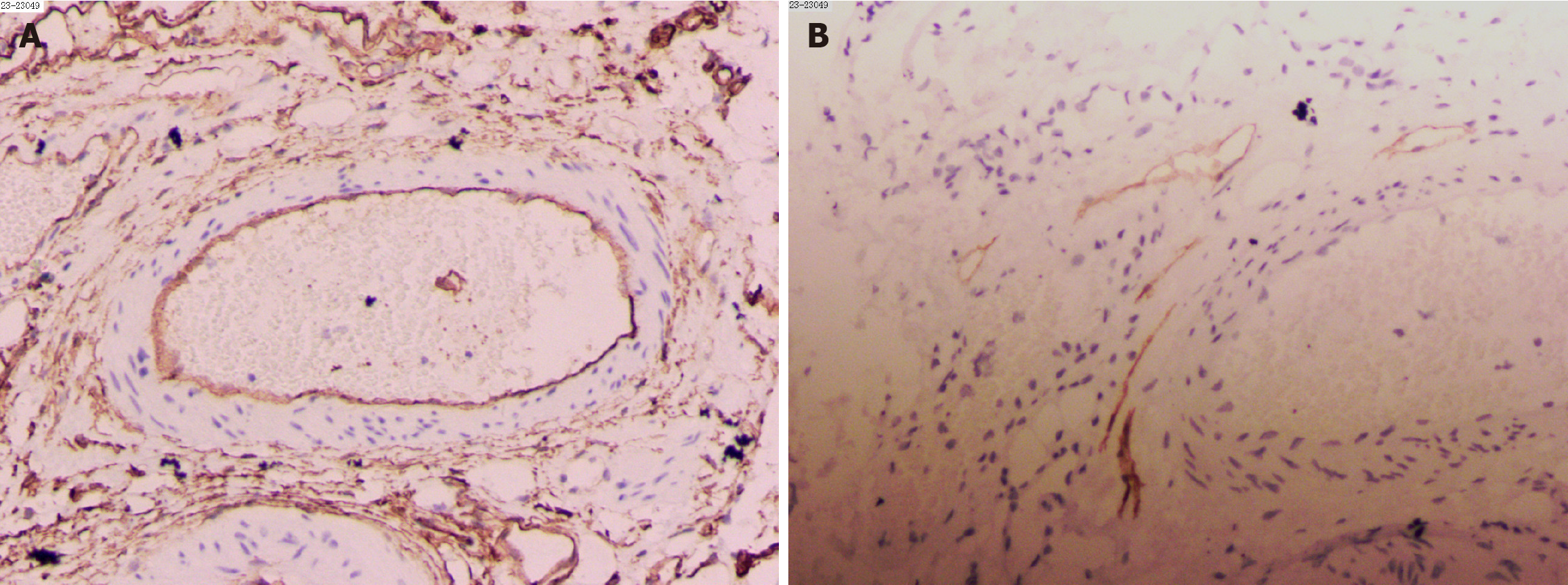
Pathology and further immunohistochemical analysis revealed hemolymphangioma, CD34 (vascular +), D2-40 (lymphatic +), Ki67 (2%+), and CK (focal +) (Figure 3). The patient was followed up for 3 mo without recurrence.
Hemolymphangioma is a benign condition that may be a slowly growing cyst over time or a tumor that grows aggressively but has no invasive capacity[6]. Therefore, it usually does not have typical clinical manifestations. In this case, the patient's symptoms of upper abdominal distension and low back pain may be caused by compression from the large tumor. Preoperative diagnosis and evaluation by imaging are essential, and these lesions should be differentiated from ganglioneuroma, myelolipoma, epidermoid cyst, lymphangioma, and cystic teratoma. The typical appearance of hemolymphangioma is cystic or solid. The cystic lesion may be due to rupture and fusion of the vascular cavity, and the solid one may be residual compressed vascular tissue[7]. A T1-weighted magnetic resonance imaging (MRI) indicates that the cystic mass contains old blood[8].
In this study, we used the PubMed database to review the literature up to December 2023, and found only three reports of hemolymphangioma occurring in the retroperitoneal space. French scholars first reported a case of infected retroperitoneal hemolymphangioma in a patient with venomusculoskeletal hypertrophy syndrome in 1983. We did not have the details of the case[9]. In 1987, Japanese researchers reported a case of giant retroperitoneal hemolymphangioma and discussed its appearance based on MRI. In addition, factor VIII-related antigen staining was also used to differentiate lymphatic vessels from blood vessels[8]. Another Japanese research group reported a 68-year-old man with retroperitoneal hemolymphangioma in 2018[1].
As shown in Table 1, all four patients were male, three had large tumors, and the tumor volume reported in our study was the largest. We speculate that patients did not pay attention to this disease because there are no special symptoms in the early stage of hemolymphangioma originating from the retroperitoneal space, and the increasing tumor volume leads to compression symptoms or signs of a large mass in the late stage. Because hemolymphangioma is rare, various imaging methods are often needed for differential diagnosis before surgery. Among them, MRI is very helpful for determining the nature of the content of the mass. When the T1 time is significantly shortened, hemolymphangioma should be considered. Although hemolymphangioma is a benign tumor, surgical resection is recommended to avoid further aggressive tumor growth or recurrence. The final diagnosis depends on pathological examination. Immunohistochemical staining for D2-40, CD31 and CD34 was often positive.
| Country | Sex | Age in yr | Size in cm | Preoperative diagnosis | Treatment | Prognosis |
| France | Male | 29 | 22 × 9 | None | Tumor resection | None |
| Japan | Male | 17 | 25 × 15 × 7 | Lymphangioma with bleeding | Tumor resection | None |
| Japan | Male | 68 | 4 × 3.2 | Liposarcoma or lymphoma | Tumor resection | No recurrence |
| China | Male | 37 | 20.0 × 16.3 × 31.3 | Lymphangioma | Tumor resection | No recurrence |
In summary, retroperitoneal hemolymphangioma is a rare lesion of blood vessels and lymphatic vessels. In the early stage, patients are often asymptomatic, and tumors are not found until they are large enough to cause symptoms. It is difficult to differentiate it from lymphangioma via preoperative imaging, but MRI is helpful for confirming the diagnosis. Surgery is the preferred treatment, and the long-term prognosis is good.
The authors thank doctors, nurses, and clinical staff who provided care for the patient.
| 1. | Ohsawa M, Kohashi T, Hihara J, Mukaida H, Kaneko M, Hirabayashi N. A rare case of retroperitoneal hemolymphangioma. Int J Surg Case Rep. 2018;51:107-111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Hu R, Li H. Giant cystic hemolymphangioma of the postmediastinum. Thorac Cancer. 2010;1:175-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Wu J, Shangguan H, Zhou S, Dong L. Hemolymphangioma in the posterior mediastinum: a case report and literature review. Clin Respir J. 2018;12:302-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Wang H, Cao J, Huang H, Yang D, Wu Z, Luo Y, Ling W. Contrast-enhanced ultrasound-based Bosniak classification for evaluating of a cystic renal mass: a rare case description of renal hemolymphangioma. Quant Imaging Med Surg. 2023;13:1221-1226. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 5. | Li Y, Pang X, Yang H, Gao C, Peng B. Hemolymphangioma of the waist: A case report and review of the literature. Oncol Lett. 2015;9:2629-2632. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Sun LF, Ye HL, Zhou QY, Ding KF, Qiu PL, Deng YC, Zhang SZ, Zheng S. A giant hemolymphangioma of the pancreas in a 20-year-old girl: a report of one case and review of the literature. World J Surg Oncol. 2009;7:31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 7. | Mao CP, Jin YF, Yang QX, Zhang QJ, Li XH. Radiographic findings of hemolymphangioma in four patients: A case report. Oncol Lett. 2018;15:69-74. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Kanaitsuka T, Itani K, Shigeta H, Yamamura Y, Kogawa T, Yoshikawa T, Sugino S, Kanatsuna T, Kondou M, Takashina K. [A case report of giant retroperitoneal hemolymphangioma]. Nihon Naika Gakkai Zasshi. 1987;76:1595-1603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Houdart R, Palau R, Auclair E, Costa JC, Potet F. [Infected retroperitoneal hemolymphangioma in an adult with the Klippel-Trenaunay syndrome. Ultrasonic diagnosis]. Presse Med. 1986;15:216. [PubMed] |