Published online Apr 26, 2024. doi: 10.12998/wjcc.v12.i12.2086
Peer-review started: November 14, 2023
First decision: January 24, 2024
Revised: February 5, 2024
Accepted: March 27, 2024
Article in press: March 27, 2024
Published online: April 26, 2024
Processing time: 153 Days and 16 Hours
Venous variations are uncommon and usually hard to identify, and basilic vein variation is particularly rare. Basilic vein variation usually presents without any clinical symptoms and is often regarded as a benign alteration. This case was a patient with congenital basilic vein variation encountered during surgery for an infusion port.
We documented and analyzed an uncommon anatomical variation in the basilic vein encountered during arm port insertion. This peculiarity has hitherto re
Venous variation is rare and requires detailed intraoperative and postoperative examination to ensure accuracy, so as not to affect subsequent treatment.
Core Tip: Venous variation refers to structural malformations caused by abnormal development of venous vessels. At present, the etiology is still unknown. In the process of implanting the arm port for a tumor postoperative patient, we found and reported a case of successful treatment of basilic vein variation encountered during the operation, which can provide a reference for such cases in the future.
- Citation: Hu CD, Lv R, Zhao YX, Zhang MH, Zeng HD, Mao YW. Basilic vein variation encountered during surgery for arm vein port: A case report. World J Clin Cases 2024; 12(12): 2086-2091
- URL: https://www.wjgnet.com/2307-8960/full/v12/i12/2086.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i12.2086
Breast cancer is one of the most common tumors afflicting women, and chemotherapy is an essential method of treat
The basilic vein is one of the superficial veins of the upper limb, on the ulnar side of the forearm. After receiving blood from the ulnar side, it gradually turns from the back of the hand to the flexor side of the forearm. It receives blood from the median cubital vein in the elbow fossa and travels up along the inside of the biceps brachii muscle. It penetrates through the fascia propria at about the midpoint of the upper arm and connects to the brachial vein or accompanies it to the axillary vein. The basilic vein has characteristics such as a straight course, few valves, gradually thickening lumen, and easy external touch[6]. However, arm venous access still poses some specific challenges, because the arm venous rou
After the right breast cancer surgery, the arm port is required to be placed for further chemotherapy.
The patient had previously undergone surgery to confirm right-sided breast cancer (T2N0M0), and postoperative pa
The patient had undergone a modified radical mastectomy with sentinel lymph node biopsy for right-sided breast cancer, and had no other significant past medical history.
The patient had no previous history of venous variation or personal and family history of cancer, no smoking or alcohol consumption, no special medication or exposure to toxic substances.
The patient had no right breast, and a surgical scar about 15 cm long was seen on the right chest wall; no obvious mass or abnormality was seen on the left breast.
The laboratory tests for blood, urine, stool, coagulation function, infectious diseases, etc. were all normal.
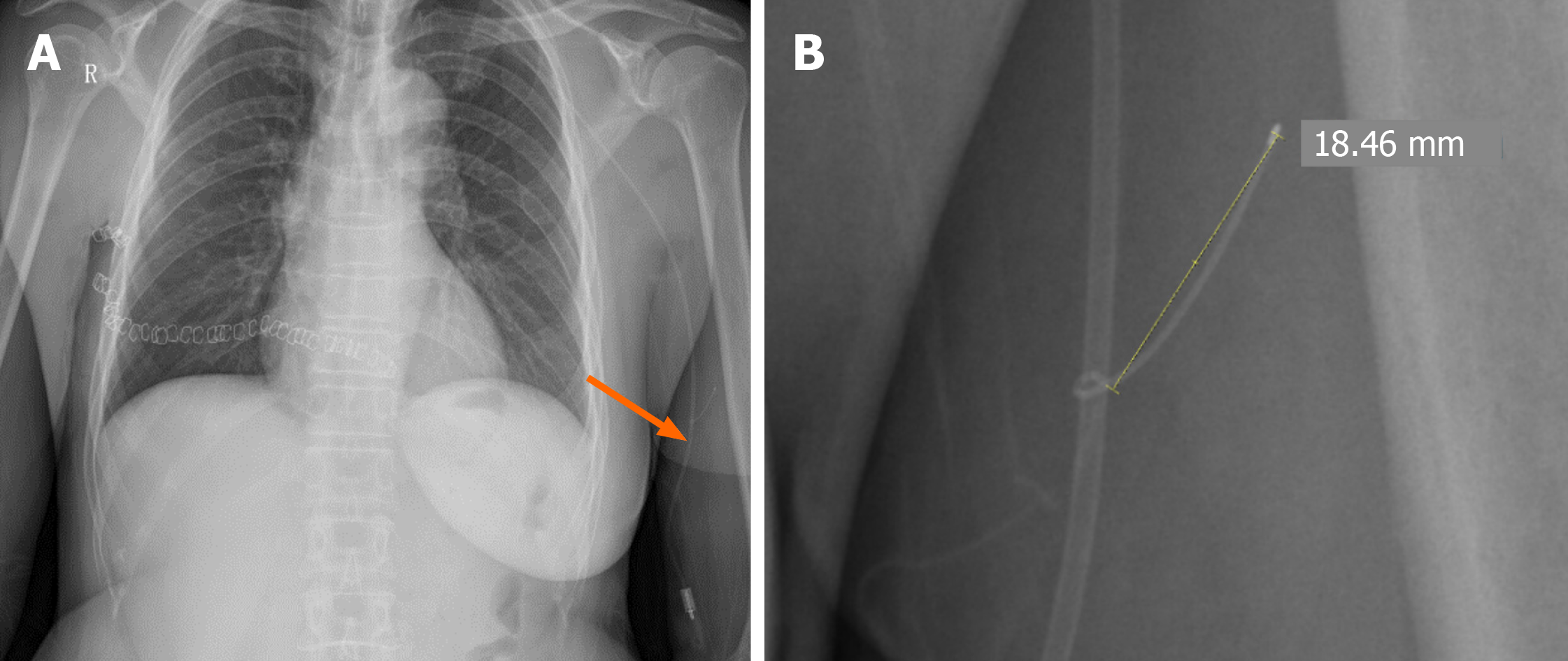
Postoperative X-ray showed that the end of the patient’s peripherally inserted central catheter was located on the right side of the T7 intervertebral foramen (Figure 1A), and an abnormal guidewire about 1.8 cm long was seen on the upper part of the left elbow (Figure 1B).
After the operation, imaging showed a branch of the left upper limb basilic vein, suggesting a congenital venous variation (Figure 1B).
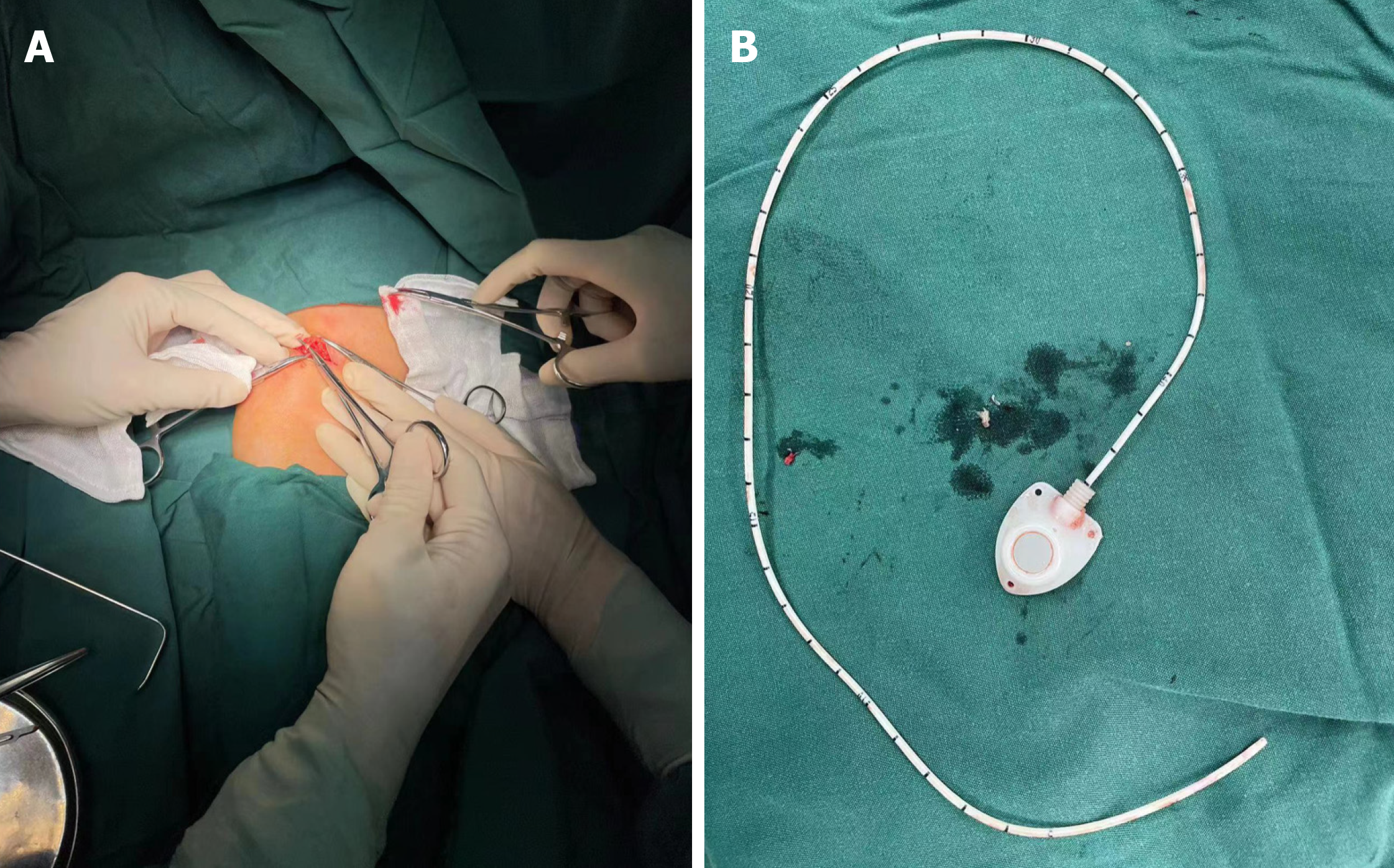
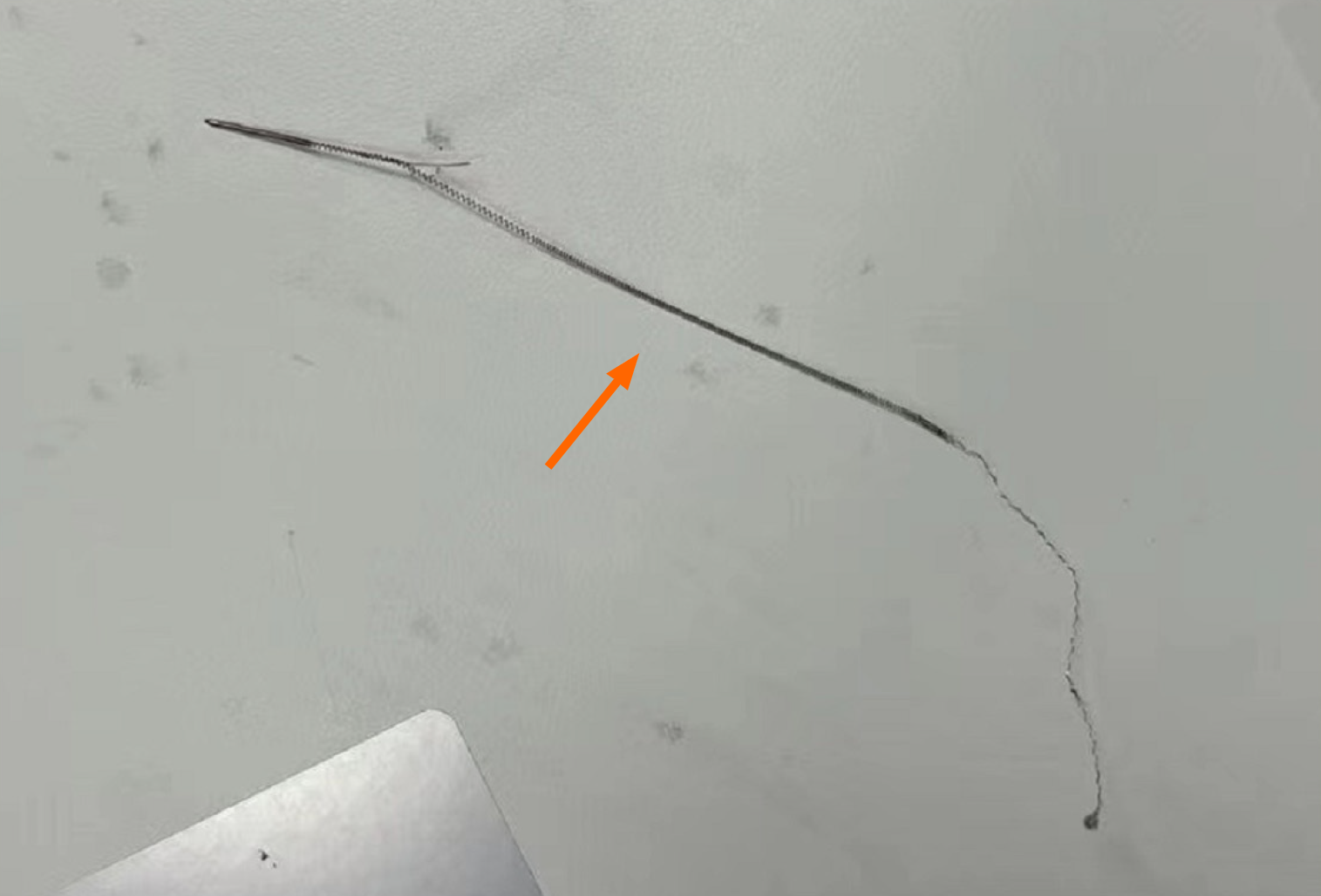
The patient underwent emergency removal of a foreign body from the left upper arm. Before the operation, a C-arm machine was used to locate the foreign body in the left upper arm and a transverse surgical incision was made. The foreign body was freed to the location position, and a guidewire about 1.8 cm long was seen during exploration (Figure 2). The guidewire was completely removed, which was confirmed by radiography.
The patient was considered to have basilic vein variation, and the guidewire entered the variant branch of the basilic vein during arm port insertion. Fortunately, postoperative X-ray detected it in time and handled it properly. During sub
Breast cancer has become the most common malignant tumor among women worldwide, and its incidence is increasing annually. The current treatment mainly includes multidisciplinary methods such as surgery, radiotherapy, neoadjuvant therapy, and adjuvant therapy[8]. For patients who need chemotherapy, traditional totally implantable vascular access devices are installed in the chest wall, through subclavian or internal jugular vein implantation. However, as an al
Our patient chose an arm port after consideration. Before arm port implantation, we signed relevant informed consent forms with the patient, understood the patient’s past history and drug allergy history, asked the patient to undergo blood routine and electrocardiographic examination, measured biochemical indicators and coagulation function, etc., and checked the skin condition of the implantation site. Finally, according to the location of breast cancer, we chose the basilic vein on the left (healthy) side as the infusion port catheter entry route. The patient was placed on the operating table in a supine position, and the target arm was kept perpendicular to the body[10]. We checked the patient’s vascular condition under ultrasound guidance, and the basilic vein looked normal. We marked the pre-puncture point and pouch site and disinfected the entire arm three times. A sterile towel was placed under the punctured side limb, and the operator wore sterile clothing and gloves. The Surgical drape was spread around the puncture point to maximize the sterile area. After preparation, the vascular ultrasound probe was coated with a coupling agent and wrapped in a sterile ultrasound pro
We routinely performed chest X-rays after surgery, to confirm the position of the catheter. The ideal position of the catheter should be at the T5-7 level[5]. The catheter was located at the right side of the T7 intervertebral foramen level, which met the placement requirements. According to the chest X-ray, we could see an abnormal guidewire about 1.8 cm long on the upper part of the left elbow (Figure 1). We immediately consulted a hand microsurgeon, who performed emergency removal of the foreign body from the left upper arm. The hand microsurgery procedure involved making a transverse incision of approximately 7 cm in length, according to the preoperative positioning of the C-arm machine. The incision was made through the skin and subcutaneous tissue, and the flap was then freed up to the C-arm machine positioning position. During the procedure, an abnormal guidewire measuring approximately 1.8 cm was discovered and explored (Figure 2). After removing the guidewire (Figure 4), another radiograph was taken to confirm its complete removal, and hemostasis was performed on the wound surface, and the subcutaneous tissue and skin were sutured layer by layer. During the operation, no adjustment was made that affected the infusion catheter position and the patient also underwent adjuvant chemotherapy as planned. The chemotherapy side effects were not significantly different from those in other arm port patients. The possible reason was that the basilic vein variation occurred at a place that did not affect the normal infusion catheter position, and there was no obvious impact on the absorption, distribution, metabolism, and excretion of drugs in the subsequent period. No common intraoperative complications such as air embolism or arterial injury, occurred during surgery. There was no skin soft tissue damage, catheter-related infection, catheter-related thrombosis, or other common postoperative complications. During the subsequent adjuvant chemotherapy period, the arm port continued to function normally, all indicators were normal during regular examinations, and the patient did not have any obvious discomfort. After completing eight cycles of chemotherapy, the patient successfully underwent arm port removal under local anesthesia on February 8, 2023. All indicators were normal during regular re-examination. Subsequent intermittent follow-ups showed that health status and quality of life improved significantly.
We conducted a literature search on PubMed, Web of Science and China National Knowledge Infrastructure (CNKI), and retrieved all studies published before July 2022. In many clinical case reports, the venous variations encountered had an impact on diagnosis and treatment, and the problems encountered during the treatment process, such as the impact of central venous anatomical variation on venous access, etc[11]. However, regarding basilic vein a variation, only one case was found in CNKI. The patient was an adult male, and variation of the left basilic vein was found during dissection. The report and discovery of this case had some significance for our operation[12].
Many studies have shown that an arm port is a feasible long-term chemotherapy option, with a high level of patient satisfaction and minimal negative impact on quality of life. These findings are important for the treatment of breast cancer, because long-term chemotherapy may have a negative impact on quality of life. The use of arm catheters can reduce pain and discomfort for patients, and improve patient satisfaction, thereby improving treatment outcomes[13]. This case report has some implications for breast cancer patients who are undergoing arm port implantation. Before clinical arm port implantation, a vascular ultrasound must be performed to confirm whether there is any abnormality in the basilic vein, whether the blood vessels have sufficient volume and whether they meet the relevant implantation con
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Bansal C, India; Tokumine J, Japan S-Editor: Liu H L-Editor: A P-Editor: Xu ZH
| 1. | Tang TT, Liu L, Li CX, Li YT, Zhou T, Li HP, Wang J. Which is Better for Patients with Breast Cancer: Totally Implanted Vascular Access Devices (TIVAD) or Peripherally Inserted Central Catheter (PICC)? World J Surg. 2019;43:2245-2249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 2. | Burbridge B, Chan IY, Bryce R, Lim HJ, Stoneham G, Haggag H, Roh C. Satisfaction and Quality of Life Related to Chemotherapy With an Arm Port: A Pilot Study. Can Assoc Radiol J. 2016;67:290-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Gong Y, Yu L, Wang F, Wang L, Sun M, Li H. The Radiographic Changes of Catheter Tip in Different Positions of Arm Infusion Port. Contrast Media Mol Imaging. 2022;2022:9374774. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 4. | Tabatabaie O, Kasumova GG, Eskander MF, Critchlow JF, Tawa NE, Tseng JF. Totally Implantable Venous Access Devices: A Review of Complications and Management Strategies. Am J Clin Oncol. 2017;40:94-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 67] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 5. | Kreis H, Loehberg CR, Lux MP, Ackermann S, Lang W, Beckmann MW, Fasching PA. Patients' attitudes to totally implantable venous access port systems for gynecological or breast malignancies. Eur J Surg Oncol. 2007;33:39-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 6. | Bertoglio S, Cafiero F, Meszaros P, Varaldo E, Blondeaux E, Molinelli C, Minuto M. PICC-PORT totally implantable vascular access device in breast cancer patients undergoing chemotherapy. J Vasc Access. 2020;21:460-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 7. | Burbridge B, Lim H, Dwernychuk L, Le H, Asif T, Sami A, Ahmed S. Comparison of the Quality of Life of Patients with Breast or Colon Cancer with an Arm Vein Port (TIVAD) Versus a Peripherally Inserted Central Catheter (PICC). Curr Oncol. 2021;28:1495-1506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Libson S, Lippman M. A review of clinical aspects of breast cancer. Int Rev Psychiatry. 2014;26:4-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 119] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 9. | Li G, Zhang Y, Ma H, Zheng J. Arm port vs chest port: a systematic review and meta-analysis. Cancer Manag Res. 2019;11:6099-6112. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 23] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 10. | Liu Y, Li LL, Xu L, Feng DD, Cao Y, Mao XY, Zheng J, Jin F, Chen B. Comparison between Arm Port and Chest Port for Optimal Vascular Access Port in Patients with Breast Cancer: A Systematic Review and Meta-Analysis. Biomed Res Int. 2020;2020:9082924. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Xu H, Chen R, Jiang C, You S, Zhu Q, Li Y, Li S, Zha X, Wang J. Implanting totally implantable venous access ports in the upper arm is feasible and safe for patients with early breast cancer. J Vasc Access. 2020;21:609-614. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 12. | Xu KG, Huan HL, Li T, Li ZSC, Ma QY, Ma CDJ, Ma YX. [One case of left basilic vein variation]. Yixue Lilun Yu Shijian. 2019;05:767. [DOI] [Full Text] |
| 13. | Shaikh UH, Powell SK, Allsop EJ, McWilliams RG. Central venous anatomical variation: implications for venous access. J Vasc Access. 2011;12:385-386. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |