Published online Apr 16, 2024. doi: 10.12998/wjcc.v12.i11.1974
Peer-review started: January 19, 2024
First decision: February 23, 2024
Revised: February 28, 2024
Accepted: March 21, 2024
Article in press: March 21, 2024
Published online: April 16, 2024
Processing time: 83 Days and 4.4 Hours
This case of gestational gingival tumor is huge and extremely rare in clinical practice. As the growth location of this gingival tumor is in the upper anterior tooth area, it seriously affects the pregnant woman's speech and food, causing great pain to the patient. The use of Nd:YGA water mist laser to remove the gingival tumor resulted in minimal intraoperative bleeding, minimal adverse reactions, and good postoperative healing, which is worthy of clinical promotion and application.
The patient, a pregnant woman, reported a large lump in her mouth on the first day of postpartum treatment. Based on medical history and clinical examination, the diagnosis was diagnosed as gestational gingival tumor. Postoperative pathological biopsy also confirmed this diagnosis. The use of Nd:YAG water mist laser to remove the tumor resulted in minimal intraoperative bleeding, clear surgical field of view, short surgical time, and good postoperative healing.
In comparison to traditional surgery, Nd:YAG water mist laser surgery is minimally invasive, minimizes cell damage, reduces bleeding, ensures a clear field of vision, and virtually eliminates postoperative edema, carbonization, and the risk of cross infection. It has unique advantages in oral soft tissue surgery for pregnant patients. Therefore, the clinical application of Nd:YAG water mist laser for the treatment of gestational gingival tumors is an ideal choice.
Core Tip: Pregnant gingival tumors are more common in clinical practice, usually smaller than 1 cm, but gestational gingival tumors with a size of nearly 4 cm are relatively rare. There have been reports of using semiconductor lasers to treat gestational gingival tumors in clinical practice, but the tumors are relatively small and have less bleeding. In this case, Nd:YAG water mist laser was used to remove large tumors. The intraoperative bleeding was minimal, the field of vision was clear, and there was water mist cooling without carbonization. The postoperative effect was ideal.
- Citation: Chen HY, Xu JJ, Chang XL, Wu P. Nd:YAG water mist laser treatment for giant gestational gingival tumor: A case report. World J Clin Cases 2024; 12(11): 1974-1979
- URL: https://www.wjgnet.com/2307-8960/full/v12/i11/1974.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i11.1974
Gingival tumors during pregnancy are usually non-malignant lesions[1]. On the basis of gingivitis and chronic periodontitis, the tumor-like lesions are caused by increased levels of sex hormones leading to gingival papillary hyperplasia and enlargement are often seen as single lesions[2,3]. Pregnant gingival tumors belong to the class of granulomatous gingival tumors[4], with abundant blood vessels in the tumor body, generally with diameters less than 2 cm, and have little impact on daily life. However, in severe cases, the tumors may hinder eating, speaking, or even be accidentally bitten, leading to repeated bleeding and secondary infections, thereby endangering the health of mother and child[5]. A case of clinically rare gestational giant gingival tumor was admitted to Ningbo University Affiliated Women and Children's Hospital. On the first postpartum day, Nd:YAG water mist laser resection was performed. The report details our findings.
A 28-year-old female patient developed redness, swelling, and congestion of the gums during the third month of pregnancy. By the seventh month, it was discovered that the upper front teeth had swollen gums on the lip side, about the size of fava beans. Fearful of aggravating the condition while brushing her teeth, she occasionally experienced bleeding while eating. There was no obvious pain initially, but it gradually increased and affected the palatal side. Although it seriously affected food intake and daily activities, she refused surgery due to concerns about the fetus during pregnancy. She came to our department for treatment on the first day after delivery.
By the seventh month, it was discovered that the upper front teeth had swollen gums on the lip side, about the size of fava beans.
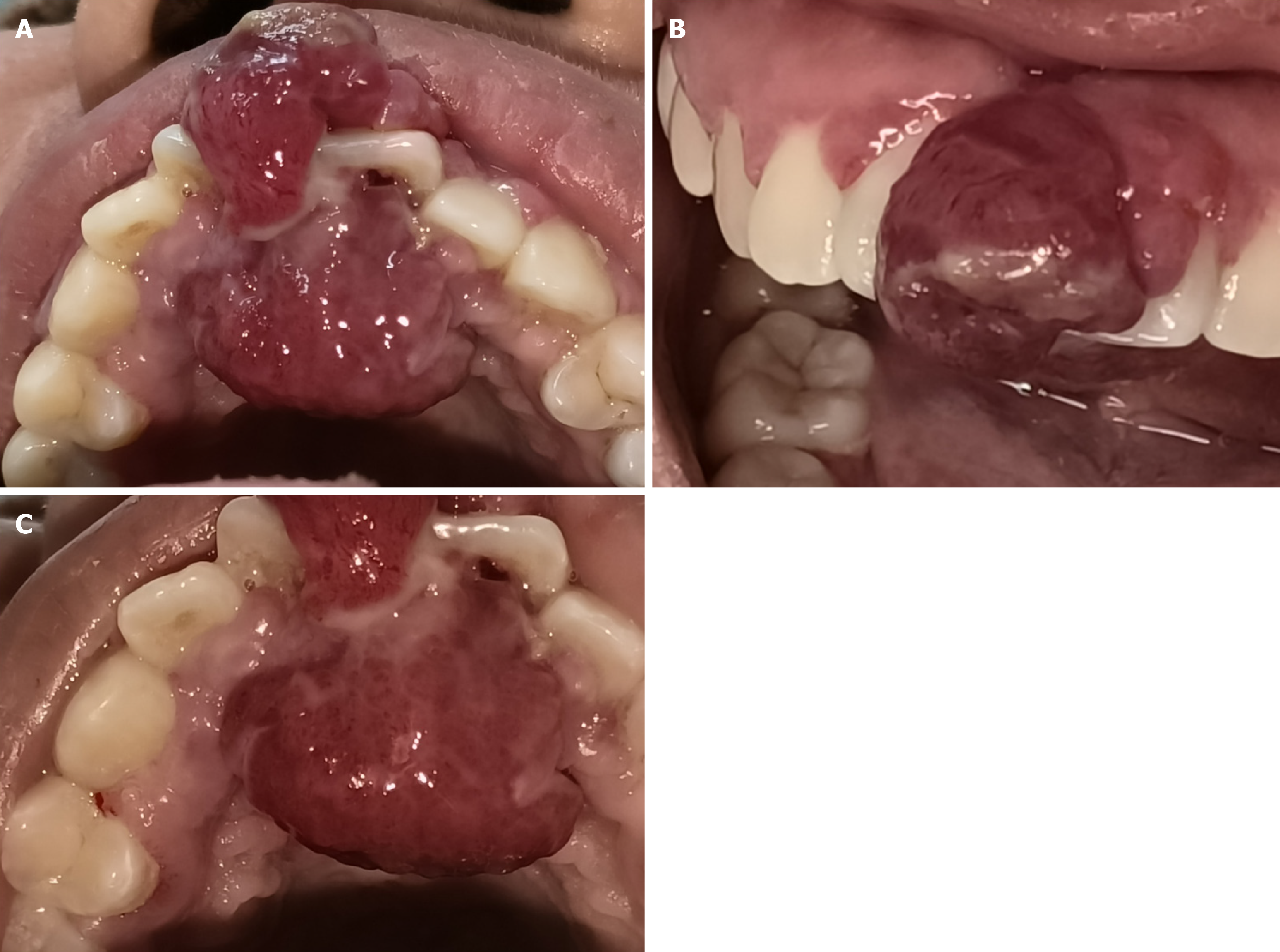
There is a huge lump in the front tooth area, and the patient is afraid to close her mouth forcefully. The tumor is dumbbell-shaped and affects the lips and palate on the 11th and 21st teeth. Its dimensions measured approximately 1.9 cm × 1.4 cm × 0.8 cm on the lip side, with a palatal size of approximately 3.2 cm × 2.5 cm × 1.2 cm in size, with a clitoris on the lip side, soft textured, and had a dark purple red color. The surface appeared smooth, with an ulcer approximately 0.6 cm × 0.3 cm × 0.1 cm in size on the labial mass near the cutting end of the tooth. The ulcer surface has slightly white edges and a slightly tough texture. The gap between teeth 11 and 21 has widened to 3 mm, with lip displacement and no looseness of teeth (Figure 1). Poor oral hygiene, along with redness, swelling, and congestion of other gingival papillae and the presence of dental calculus, were also observed.
No abnormalities in the coagulation function test and infectious markers were observed in the elevated white blood cells and neutrophils.
Gestational gingival tumors involving teeth 11 and 21, along with chronic periodontitis.
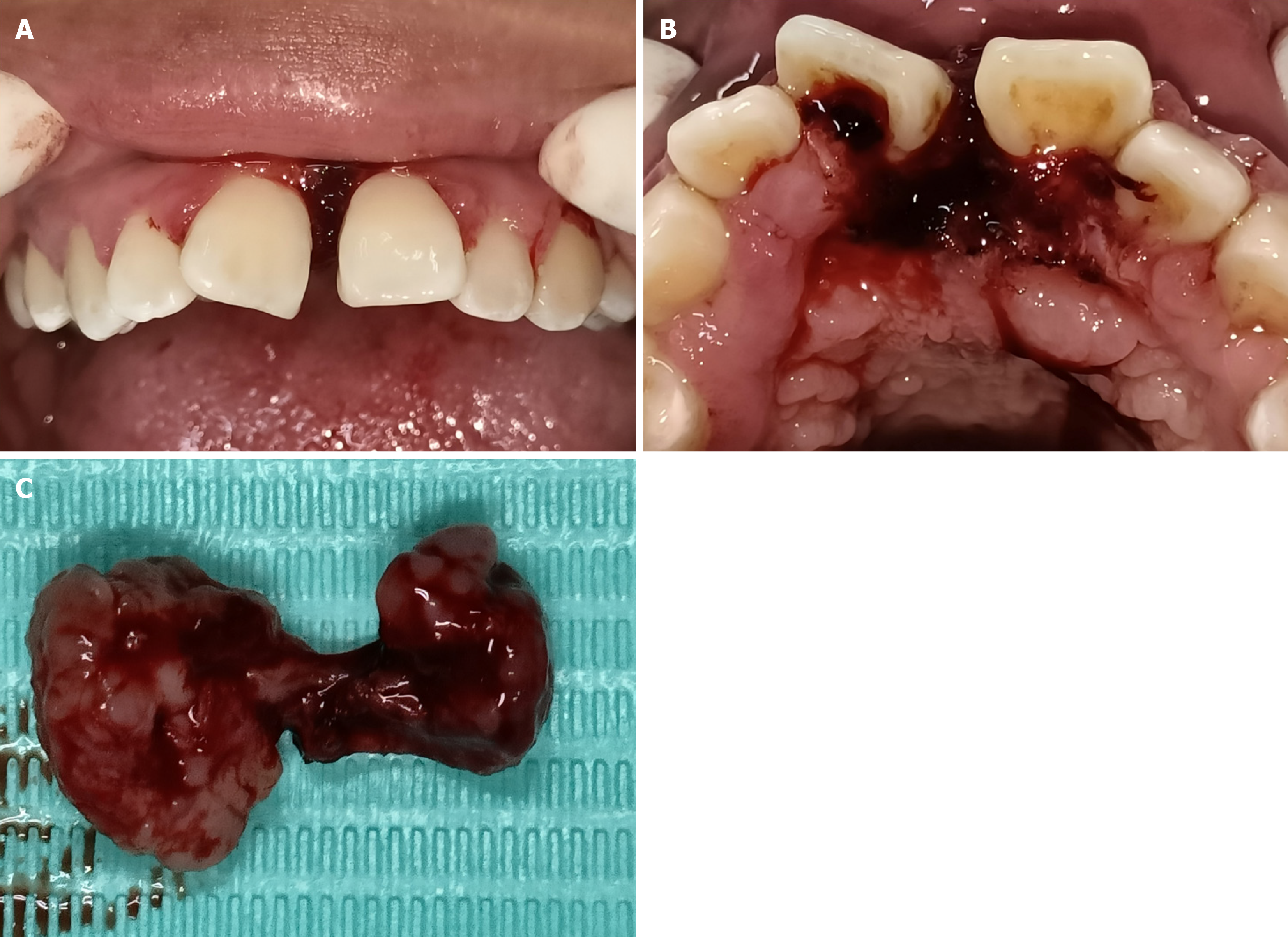
Prior to surgery, an informed consent form was signed, and local infiltration anesthesia with articaine and epinephrine Injection was performed. Routine disinfection and drape were used. During the surgery, an incision was made along the normal tissue 0.2 cm around the tumor. The Nd:YAG water mist laser (Wisdom, China) was used in gingival tumor cutting mode, with settings of activated fiber, energy at 140 mJ, frequency at 60 Hz, and water 1, gas 3; this completely removed the tumor tissues associated with teeth 11 and 21. Hemostasis mode (activated fiber, energy of 35 mJ, without water vapor) was then employed to seal and stop bleeding on the surgical site (Figure 2). Due to the patient's weak body and absence of loose teeth on the first day after delivery, no X-rays or further periodontal treatment were taken. Post-surgery instructions included rinsing the mouth with Chlorhexidine mouthwash three times a day, carefully cleaning the teeth every day, and refraining from consuming hard or overheated foods for three days after surgery. After the surgery, the tumor was removed and sent for biopsy. The pathological results showed that it was consistent with granulomatous gingival tumor, with proliferative blood vessels accompanied by a large amount of inflammatory cell infiltration.
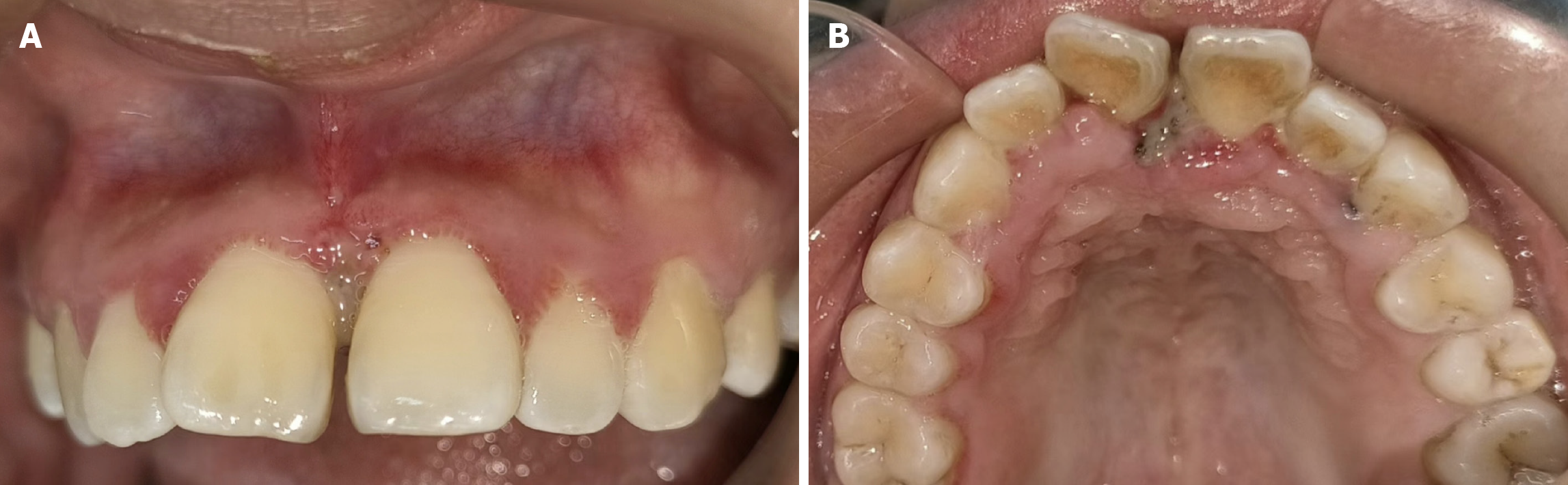
One week after surgery, the wound healed well, and there was no recurrence. The interdental space has become smaller, now about 1mm in size, and the inflammation of the entire gums has improved (Figure 3).
Gestational gingival tumors are common in clinical practice[6], with the reason for their occurrence being twofold. Firstly, during pregnancy, there is a significant increase in the types of subgingival bacteria, especially the detection rate of periodontal pathogens, which leads to the occurrence of gingivitis and periodontitis[7]. Secondly, there are progesterone and estrogen receptors in gingival, periodontal ligament fibroblasts, and osteoblasts[8]. Elevated levels of sex hormones during pregnancy, combined with continuous inflammatory stimulation, lead to local hyperplasia and swelling of the gums, resulting in the formation of gingival tumors. Therefore, local plaque and sex hormones are the main causes of gestational gingival tumors. Hence, for the treatment of gingival tumors in pregnant women presenting with small tumors that do not affect oral function and daily life, basic periodontal treatment can be carried out as soon as possible after delivery when the hormone levels return to normal. The gingival tumors may disappear, thus avoiding surgery for patients[9].
Gestational gingival tumors are often accompanied by massive bleeding and can interfere with chewing, affect eating, and thus have adverse effects on the mother's nutrient intake. As the disease progresses, gingival tumors can also damage the alveolar bone, leading to tooth loosening and displacement. In this case, the upper central incisor lip is displaced, and a 3 mm gap appears between teeth 11 and 21, yet fortunately, tooth loosening has not yet occurred. The main treatment method for larger gingival tumors is conventional surgery combined with periodontal scraping to remove irritant factors. Traditional surgery requires gingival tumor resection, extraction of relevant affected teeth, scraping of periodontal ligaments and periosteum, and removal of adjacent bone tissue to prevent recurrence. However, sacrificing the affected teeth and surrounding alveolar bone may have a negative impact on the patient's postoperative quality of life[10]. Alternatively, a non-surgical treatment method of injecting a mixture of Pingyangmycin and dexamethasone into the tumor cavity has achieved certain results[11], but may not be suitable for pregnant patients.
Gingival tumors are not true tumors, and those with a diameter greater than 2.5 cm are relatively rare[12]. The gingival tumor, in this case, is huge, with a size exceeding 4 cm, which seriously affects the patient's eating, speaking, and daily life. As a result, the patient urgently requests surgery to remove the gingival tumor on the first day after giving birth. The Wisdom Nd:YAG water mist Laser, a neodymium laser that uses crystal material Nd:YAG to generate 1064 nm wavelength, was employed[13]. After being activated by a triggered fiber, it forms an extremely fine beam under the protection of the water mist effect. The high temperature generated vaporizes the tissue to achieve a cutting effect. In addition, by utilizing the absorption characteristics of hemoglobin by Nd:YAG laser, tissue can be quickly vaporized, and capillaries and lymphatic vessels inside the tissue can be sealed, hence reducing intraoperative bleeding and postoperative water reactions. This case achieved good results in the removal of giant gingival tumors using Nd:YAG water mist laser characterized by minimal intraoperative bleeding, clear field of vision, and small wound size. The postoperative reaction is mild, the recovery is fast, and there are no systemic side effects. Therefore, using Nd:YAG water mist laser can reduce intraoperative bleeding, lower suture requirements, shorten surgical time, and promote wound healing. Previous reports have found that the smoke released by ordinary lasers in soft tissue cutting may affect soft tissue healing[14,15]. However, Nd:YAG lasers have a water mist function, which perfectly utilizes the advantages of lasers while avoiding the drawbacks of smoke release, resulting in better surgical results.
In comparison to traditional surgery, Nd:YAG water mist laser surgery is minimally invasive, minimizes cell damage, reduces bleeding, ensures a clear field of vision, and virtually eliminates postoperative edema, carbonization, and the risk of cross infection. It has unique advantages in oral soft tissue surgery for pregnant patients. Therefore, the clinical application of Nd:YAG water mist laser for the treatment of gestational gingival tumors is an ideal choice.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gupta D, India S-Editor: Zheng XM L-Editor: A P-Editor: Guo X
| 1. | Manegold-Brauer G, Brauer HU. Oral pregnancy tumour: an update. J Obstet Gynaecol. 2014;34:187-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Truschnegg A, Acham S, Kiefer BA, Jakse N, Beham A. Epulis: a study of 92 cases with special emphasis on histopathological diagnosis and associated clinical data. Clin Oral Investig. 2016;20:1757-1764. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Zhu YQ, Wang YQ, Tang YC, Li CZ. Initial periodontal therapy for the treatment of gingival pregnancy tumor. Genet Mol Res. 2016;15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Bilińska M, Sokalski J. [Pregnancy gingivitis and tumor gravidarum]. Ginekol Pol. 2016;87:310-313. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 5. | Lianjia Y, Yan J, Doi T, Sekine I, Ogawa K, Mori M. Immunohistochemical localization of bone morphogenetic protein (BMP) in calcifying fibrous epulis. J Oral Pathol Med. 1993;22:406-410. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Ye C, You M, Cheng G, Zhao L, Huang P, Tang J, Chen Y, Wang X. A puzzling pregnancy epulis with aggressive bone loss mimicking malignant neoplasm: A case report. J Stomatol Oral Maxillofac Surg. 2020;121:312-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Liu C, Qin ZP, Fan ZN, Zhao WJ, Wang YM, Wei FC, Li KL, Liu SH. New treatment strategy for granulomatous epulis: intralesional injection of propranolol. Med Hypotheses. 2012;78:327-329. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Mijiritsky E, Assaf HD, Peleg O, Shacham M, Cerroni L, Mangani L. Use of PRP, PRF and CGF in Periodontal Regeneration and Facial Rejuvenation-A Narrative Review. Biology (Basel). 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 72] [Article Influence: 18.0] [Reference Citation Analysis (0)] |
| 9. | Isola G, Matarese G, Cervino G, Matarese M, Ramaglia L, Cicciù M. Clinical Efficacy and Patient Perceptions of Pyogenic Granuloma Excision Using Diode Laser Versus Conventional Surgical Techniques. J Craniofac Surg. 2018;29:2160-2163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 10. | Gisotti M, Lops D, Valente NA. Esthetic management of space and soft tissue deficiencies in implant therapy: combined orthodontic-mucogingival approach. Int J Esthet Dent. 2022;17:42-56. [PubMed] |
| 11. | Cai Y, Sun R, He KF, Zhao YF, Zhao JH. Sclerotherapy for the recurrent granulomatous epulis with pingyangmycin. Med Oral Patol Oral Cir Bucal. 2017;22:e214-e218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 12. | Shumway BS, Eskan MA, Bernstein ML. Recurrent gingival fibrous lesions: comparison of 2 cases and potential need for additional classification. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;116:e287-e296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Shang J, Gong K, Xu DP, Sun LW, Qu WD. The Nd:YAG Laser or Combined with Er:YAG Laser Therapy for Oral Venous Lakes. Photobiomodul Photomed Laser Surg. 2020;38:244-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Karimi A, Sobouti F, Torabi S, Bakhshandehfard A, Amirian A, Shariati M, Morshedi E, Barati M. Comparison of Carbon Dioxide Laser With Surgical Blade for Removal of Epulis Fissuratum. A Randomized Clinical Trial. J Lasers Med Sci. 2016;7:201-204. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Azma E, Safavi N. Diode laser application in soft tissue oral surgery. J Lasers Med Sci. 2013;4:206-211. [PubMed] |