Published online Apr 6, 2024. doi: 10.12998/wjcc.v12.i10.1824
Peer-review started: November 30, 2023
First decision: January 29, 2024
Revised: February 3, 2024
Accepted: March 4, 2024
Article in press: March 4, 2024
Published online: April 6, 2024
Processing time: 123 Days and 21.9 Hours
Combined spinal-epidural (CSE) anesthesia is the preferred anesthesia method for cesarean delivery. The use of an epidural catheter is essential for administering additional drugs intraoperatively and managing postoperative pain. However, the insertion of epidural catheters is associated with various complications, such as total spinal anesthesia, symptoms indicative of spinal nerve root irritation, and challenges in epidural catheter removal.
We present a case report of a challenging epidural catheter removal due to knot
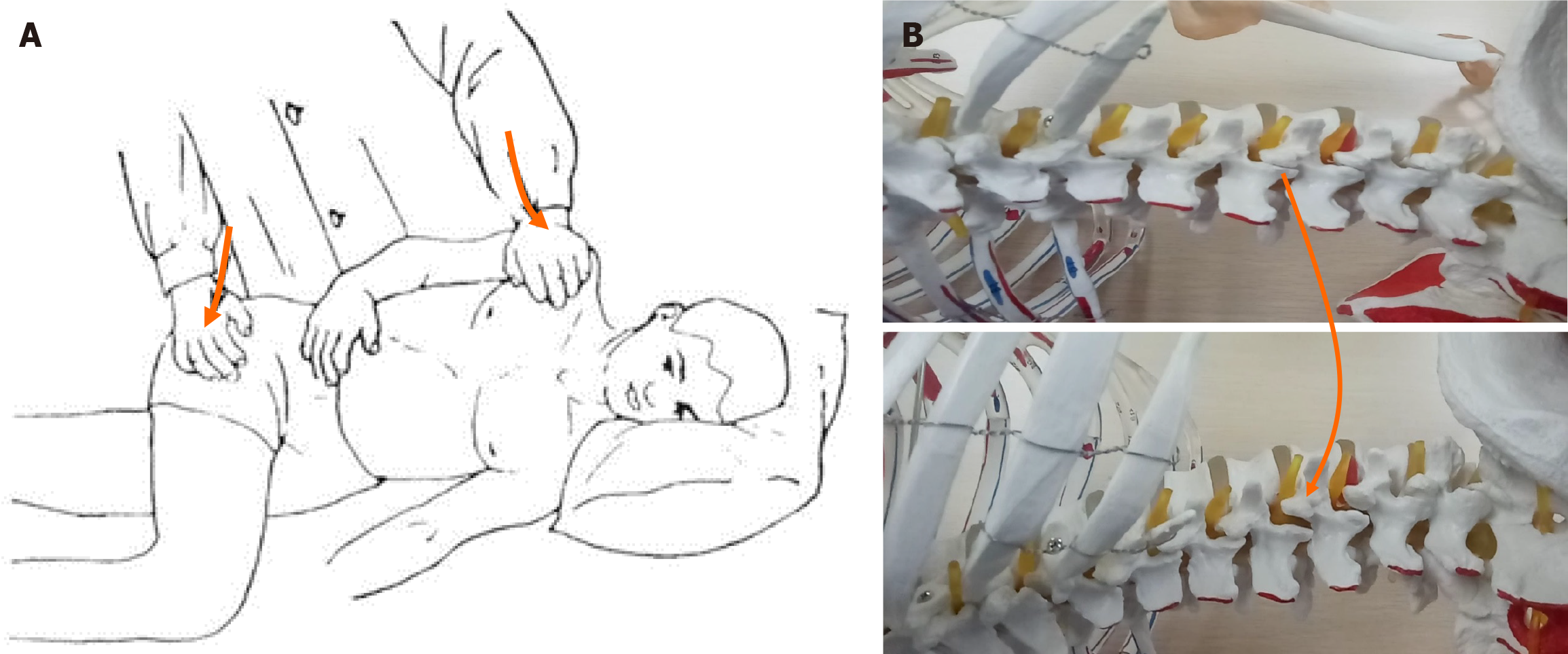
The operator can use opposite forces to "spiral" apart the spinal joints by posi
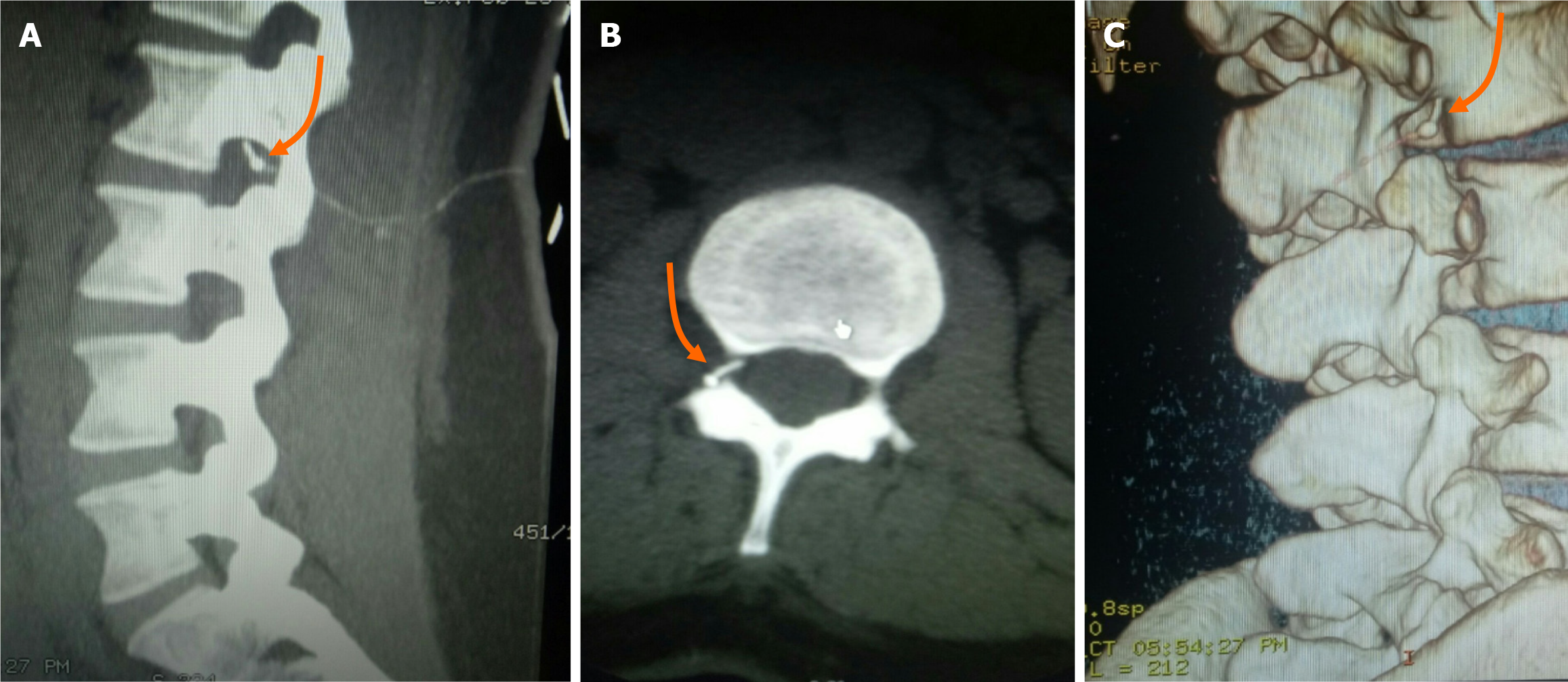
Core Tip: Lumbar computed tomography imaging showed that the reinforced catheter formed a tight knot in the epidural space. The patient's body was placed in a specific position, and the doctor's hands were respectively at the right scapula and the right hip joint of the patient, and the force in the opposite direction was used to "spiral" the spinal joint, and the catheter was successfully removed.
- Citation: Deng NH, Chen XC, Quan SB. Unique method for removal of knotted lumbar epidural catheter: A case report. World J Clin Cases 2024; 12(10): 1824-1829
- URL: https://www.wjgnet.com/2307-8960/full/v12/i10/1824.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i10.1824
Challenging removal of the epidural catheter is among the complications associated with continuous epidural anesthesia. This challenge is attributed to the compression of the catheter in the narrow intervertebral space or the formation of loops, tangles, or knots within the epidural space. The occurrence of catheter knotting, which leads to challenging removal, is extremely rare[1].
A 30-year-old female patient (38 wk pregnant, single pregnancy) underwent cesarean section. After the surgery, the anesthesiologist found it difficult to remove the epidural catheter.
The pregnant patient was placed in a right lateral tilt position. The midline puncture through the L2-3 intervertebral space was executed, but the medical staff encountered resistance after several needle direction adjustments. An alternate paramedian puncture technique was used, resulting in reduced resistance. A sensation of ligamentum flavum penetration was experienced at a depth of approximately 7 cm. A negative pressure test confirmed the entry of the epidural puncture needle into the epidural space. Subsequently, a spinal needle was inserted through the epidural needle, resulting in a sensation of dura mater puncture without evidence of nerve stimulation. Clear cerebrospinal fluid flow was observed and 1.8 mL of 0.5% ropivacaine was administered slowly. After removing the spinal needle, the left hand of the anesthesiologist held in place the epidural puncture needle, and an enhanced epidural catheter (MaiChuang Medical, Jiangsu Province, China) was advanced with the right hand until the 15 cm scale. The epidural puncture needle was retracted using the left hand, ensuring that the catheter was retreated outward of the skin to the 12 cm scale, leaving the catheter positioned at a length of 5 cm in the epidural cavity. The catheter was smoothly inserted, and no blood or cerebrospinal fluid was observed upon syringe withdrawal. The patency of the catheter was good, as demonstrated by the physiological saline test. The exposed end of the catheter was fixed to the patient's back using adhesive tape. The anesthesia administered during the surgery was effective, and the procedure was conducted smoothly.
Ten minutes before the conclusion of the operation, the injection of the initial dose of analgesia through the epidural catheter failed due to significant resistance during administration. Preliminary speculation suggested that a section of the catheter might have formed a knot under pressure on the patient's back. However, no knots were observed in the catheter after the surgery. The patient’s position was adjusted to a right lateral tilt, but an attempt to remove the catheter was unsuccessful. The patient did not experience any pain or abnormal sensations during the catheter traction process. Consequently, a decision was reached to postpone the catheter removal. The exposed portion of the catheter was disin
The patient had a history of ectopic pregnancy three years ago, and the ectopic pregnancy lesions were removed under laparoscopy.
The patient had good living habits and denied any family history of disease or other genetic diseases.
The vital signs of the patient were as follows: Body temperature, 36.8 °C; heart rate, 89/min; respiratory rate, 18/min; blood pressure, 138/86 mmHg; weight, 80 kg; and height, 154 cm.
The patient’s platelet count was 132 109, thrombin time was 16 s, prothrombin time was 10.4 s, fibrinogen was 3.85 g/L, and activated partial thromboplastin time ratio was 0.98.
The reinforced catheter formed a knot in the epidural space.
The doctor placed the patient's body in a specific position, with both hands at the right shoulder blade and the right hip joint of the patient, used the "spiral" force in the opposite direction to separate the spinal joint, and successfully removed the catheter.
We used a novel extubation method and successfully removed the catheter.
The occurrence of epidural catheter knotting is rare, with an incidence of 1 in 65140 catheters and an average of 0.0015%[2]. The length of the part of the catheter retained in the epidural space is a highly debated issue as it is associated with the incidence of catheter knotting. Some researchers believe that retaining a catheter length of 5 cm in the epidural space is optimal, balancing effective analgesia with the reduction of risks such as catheter looping, extrusion, or inadvertent arterial placement[3,4]. Researchers also propose that retaining the catheter length within 3-4 cm from the catheter tip could prevent a 180° rotation and subsequent knot formation[1]. However, some studies report knot formation even when the catheter length is maintained within 3 cm from the tip[2]. In our study, the knot was located approximately 3.2 cm from the catheter tip. Brichant et al[5] reported the formation of a tight single knot at a distance of 4 mm from the ca
Researchers are exploring alternative methods for reducing the occurrence of catheter knotting. Enhancing the puncture success rate and catheter placement is important to reduce complications. Obesity is associated with a higher failure rate of epidural puncture and catheter placement[9]. Ultrasound-guided intrathecal puncture and needle guidance techniques are used to improve the puncture success rate and catheter placement[10] and to accurately identify the position of the puncture needle tip[11]. Oscar et al[12] observed that visualizing the blood flow in the epidural space and tracking the path of the catheter in the epidural space could be indirectly achieved by injecting 1 mL of normal saline into the catheter and performing color Doppler ultrasound. This technique aids in determining whether the catheter is forming loops or knots in the epidural space.
A flexed lateral position during removal should be considered if challenges are encountered during the removal of the epidural catheter[13-16]. Although in most cases of catheter knotting, a continuous, gentle pull successfully facilitates catheter removal, approximately 30% of these cases ultimately require surgical intervention due to catheter breakage[14,17-19]. Previous studies reported successful catheter removal under general anesthesia with muscle relaxation[20,21]. However, this approach should only be considered if the patient remains awake and has not experienced neurological pains or sensory abnormalities during previous catheter removal. If any abnormal neurologic symptoms are observed during catheter removal, the procedure must be stopped because there is a potential risk of the catheter entangling with nerve roots, blood vessels, or other structures[22]. In the present case, it is postulated that during the paramedian puncture, the epidural needle did not penetrate the epidural space in the correct sequence of the supraspinous ligament, interspinous ligament, and ligamentum flavum. The epidural needle traversed through the adjacent paraspinal tissue and entered the epidural space through the vertebral lamina fissure near the right upper and lower facets of the L2-3 ver
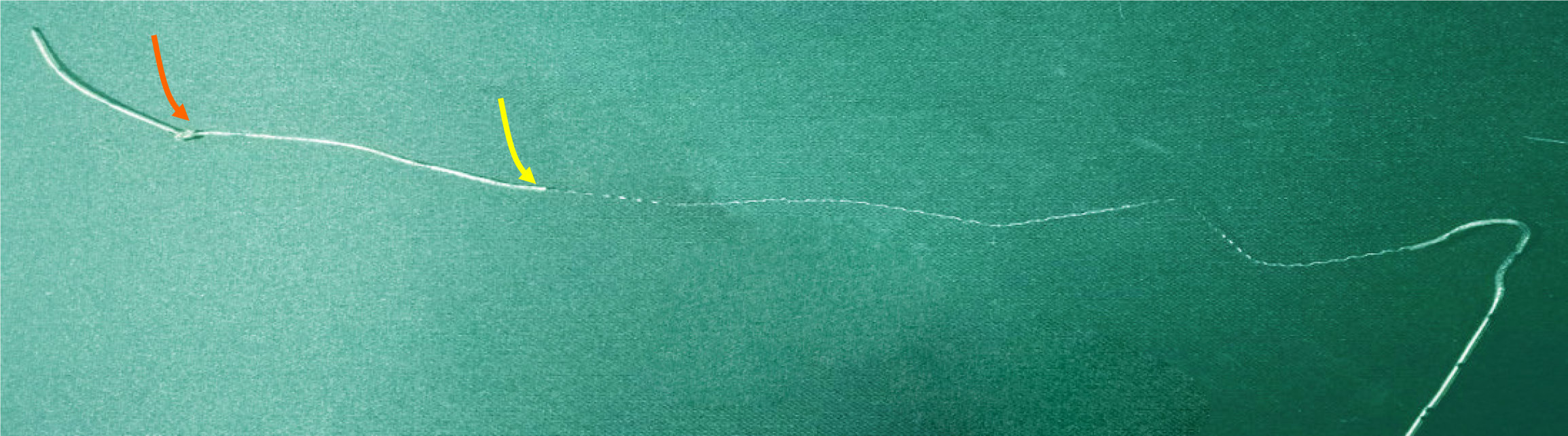
Previous results indicated that reinforced catheters have higher tensile strength than traditional polyethylene or polyurethane catheters[23]. Asai et al reported a case in which a reinforced catheter broke approximately 7-8 cm from the catheter tip during removal, leaving the broken distal end inside the patient's body, while the steel wire from the distal end remained attached to the removed segment of the catheter[19]. Therefore, continuous strong pulling should be minimized even when using reinforced catheters. In this study, we observed that the fracture of the catheter sheath occurred at a distance of 8 cm from the distal end, which could be attributed to the low-density distal end of wire coils in the 7-8 cm segment[19]. In our case, the complete removal of the entire catheter could have been due to the catheter knotting, which prevented the fractured distal end of the catheter from detaching from the inner wire coils. Although reinforced catheters have higher tensile strength, they are more flexible than traditional polyethylene or polyurethane catheters. This prompts the question of whether reinforced catheters may have a higher risk of tangling and knotting when they encounter resistance during insertion into the epidural space.
In summary, knotting of the epidural catheter is a rare complication of spinal anesthesia, with limited clinical reports available. The approach for catheter removal must be tailored to the individual circumstances. In our case, a new and previously unreported method of removing the interdural catheter was reported, and it was done without the assistance of an orthopaedic surgeon, and we recommend using the method presented in Figure 2 of this case report, which involves the use of opposite forces to separate the spinal facet joints in a "spiral" manner based on the imaging examination findings. The results indicate that this technique is more effective for catheter removal and can serve as a reference method in challenging catheter removal situations.
The operator can use opposite forces to "spiral" apart the spinal joints by positioning the patient's body in a specific position. The findings indicate that, when combined with imaging examination results, this method is effective for the removal of epidural catheters.
We thank the patient for her collaboration and all the medical staff who contributed to this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: DeSousa K, India S-Editor: Gong ZM L-Editor: Wang TQ P-Editor: Zhao S
| 1. | Arnaoutoglou HM, Tzimas PG, Papadopoulos GS. Knotting of an epidural catheter: a rare complication. Acta Anaesthesiol Belg. 2007;58:55-57. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Fibuch EE, McNitt JD, Cussen T. Knotting of the Theracath after an uneventful epidural insertion for cesarean delivery. Anesthesiology. 1990;73:1293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Cartagena R, Gaiser RR. Advancing an epidural catheter 10 cm then retracting it 5 cm is no more effective than advancing it 5 cm. J Clin Anesth. 2005;17:528-530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 4. | Beilin Y, Bernstein HH, Zucker-Pinchoff B. The optimal distance that a multiorifice epidural catheter should be threaded into the epidural space. Anesth Analg. 1995;81:301-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Brichant JF, Bonhomme V, Hans P. On knots in epidural catheters: a case report and a review of the literature. Int J Obstet Anesth. 2006;15:159-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 30] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Mizota T, Kimura K, Takeda C. Knot formation in a thoracic epidural catheter: a case report. JA Clin Rep. 2021;7:45. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Browne RA, Politi VL. Knotting of an epidural catheter: a case report. Can Anaesth Soc J. 1979;26:142-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Muneyuki M, Shirai K, Inamoto A. Roentgenographic analysis of the positions of catheters in the epidural space. Anesthesiology. 1970;33:19-24. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 9. | Kula AO, Riess ML, Ellinas EH. Increasing body mass index predicts increasing difficulty, failure rate, and time to discovery of failure of epidural anesthesia in laboring patients. J Clin Anesth. 2017;37:154-158. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Vernon TJ, Vogel TM, Dalby PL, Mandell G, Lim G. Ultrasound-assisted epidural labor analgesia for landmark identification in morbidly obese pregnant women: A preliminary investigation. J Clin Anesth. 2020;59:53-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Riveros-Perez E, Albo C, Jimenez E, Cheriyan T, Rocuts A. Color your epidural: color flow Doppler to confirm labor epidural needle position. Minerva Anestesiol. 2019;85:376-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | van den Bosch OFC, Gleicher Y, Arzola C, Siddiqui N, Downey K, Carvalho JCA. Color flow Doppler in spinal ultrasound: a novel technique for assessment of catheter position in labor epidurals. Reg Anesth Pain Med. 2022;47:775-779. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 13. | Boey SK, Carrie LE. Withdrawal forces during removal of lumbar extradural catheters. Br J Anaesth. 1994;73:833-835. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 39] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 14. | Hajnour MS, Khokhar RS, Ejaz AA, Al Zahrani T, Kanchi NU. Difficulty in the removal of epidural catheter for labor analgesia. Saudi J Anaesth. 2017;11:117-119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 15. | Sia-Kho E, Kudlak TT. How to dislodge a severely trapped epidural catheter. Anesth Analg. 1992;74:933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Morris GN, Warren BB, Hanson EW, Mazzeo FJ, DiBenedetto DJ. Influence of patient position on withdrawal forces during removal of lumbar extradural catheters. Br J Anaesth. 1996;77:419-420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 37] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 17. | Asai T, Sakai T, Murao K, Kojima K, Shingu K. More difficulty in removing an arrow epidural catheter. Anesth Analg. 2006;102:1595-1596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Bréget JM, Fischer C, Ben Meftah R, Tabary N. [Impossible withdrawal of an epidural catheter]. Ann Fr Anesth Reanim. 2008;27:1016-1018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Asai T, Yamamoto K, Hirose T, Taguchi H, Shingu K. Breakage of epidural catheters: a comparison of an arrow reinforced catheter and other nonreinforced catheters. Anesth Analg. 2001;92:246-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 20. | Jongleux EF, Miller R, Freeman A. An entrapped epidural catheter in a postpartum patient. Reg Anesth Pain Med. 1998;23:615-617. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 21. | Singh V, Bhakta P, Ahuja A. Epidural catheter knot immediately after catheter insertion. Anaesth Intensive Care. 2015;43:280-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 22. | Sidhu MS, Asrani RV, Bassell GM. An unusual complication of extradural catheterization in obstetric anaesthesia. Br J Anaesth. 1983;55:473-475. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Gonzalez Fiol A, Horvath R, Schoenberg C, Ahmed N, Dhar SK, Le V. Comparison of Changes in Tensile Strength in Three Different Flexible Epidural Catheters Under Various Conditions. Anesth Analg. 2016;123:233-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |