Published online Mar 26, 2023. doi: 10.12998/wjcc.v11.i9.2110
Peer-review started: January 13, 2023
First decision: January 30, 2023
Revised: February 1, 2023
Accepted: February 27, 2023
Article in press: February 27, 2023
Published online: March 26, 2023
Processing time: 63 Days and 1.2 Hours
Many cases of emphysema associated with blow-out fractures occur before surgery due to trauma. However, emphysema can occur even after surgery, and most of such cases are managed conservatively and allowed to resolve. Swelling in the periorbital area due to emphysema that occurs after surgery can make early recovery difficult.
Herein, we describe a case of postoperative subcutaneous emphysema that was treated using a simple needle aspiration method. A 48-year-old male patient visited the hospital with a blow-out fracture of the left medial orbital wall and nasal bone fracture. One day postoperatively, swelling and crepitus in the left periorbital area were observed, and follow-up computed tomography showed emphysema in the left periorbital subcutaneous area. Needle aspiration using an 18-gauge needle and syringe was used to relieve the emphysema. The symptoms of sudden swelling improved immediately, and no recurrence was observed.
We conclude that needle aspiration is a useful method that could help in relieving symptom, resolving discomfort, and enabling early return to daily life in patients with postoperative subcutaneous emphysema.
Core Tip: A cases of postoperative subcutaneous emphysema is relatively rare. Though orbital emphysema is usually self-limited, we report a case report of postoperative subcutaneous emphysema that treated with a simple method using immediate needle aspiration to relieve discomfort and enable recovery to daily life.
- Citation: Nam HJ, Wee SY. Successful treatment of a rare subcutaneous emphysema after a blow-out fracture surgery using needle aspiration: A case report. World J Clin Cases 2023; 11(9): 2110-2115
- URL: https://www.wjgnet.com/2307-8960/full/v11/i9/2110.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i9.2110
The orbit is highly exposed to physical facial injuries because of its anatomical location and the lack of protective tissues. Isolated orbital fractures account for in 4%-16% of all facial fractures, and orbital fracture combined with any other type of fracture occurs in 30%-55% of zygomatic complex fractures and naso-orbital-ethmoid fractures[1,2].
Orbital emphysema, which is the abnormal presence of air within the orbit, is a typical finding in blow-out fractures owing to its communication with the paranasal sinus[3]. In the setting of trauma, the presence of orbital emphysema significantly increases the likelihood of an orbital fracture, with up to 75% of patients having medial orbital wall fractures with some degree of orbital emphysema[4]. Orbital emphysema can also occur after surgery as a complication that causes postoperative discomfort and delays recovery to daily life. In previous literature, case reports and treatment of preoperative emphysema have been reported; however, there is a tendency to rely on conservative treatment for subcutaneous emphysema that occur postoperatively because the symptoms in such cases are often not severe. However, this may be time-consuming and cause discomfort to the patient until spontaneous resolution is achieved.
Herein, we describe a case of postoperative subcutaneous emphysema that was treated with a simple method using immediate needle aspiration to relieve discomfort and enable recovery to daily life.
A 48-year-old male patient visited the hospital after experiencing direct trauma to the nose and periorbital area 9 d prior.
He had mild swelling and tenderness in nose and periorbital area due to the direct trauma. The day after hospitalization, orbital wall reconstruction using a bioresorbable polycaprolactone mesh implant (Osteomesh, Osteopore International, Singapore) and closed reduction of the nasal bone were performed. One day after the operation, the patient complained of difficulty in opening his left eye, and severe swelling in the left periorbital area was observed.
He had no remarkable medical history or chronic illness.
There was no significant personal or family history.
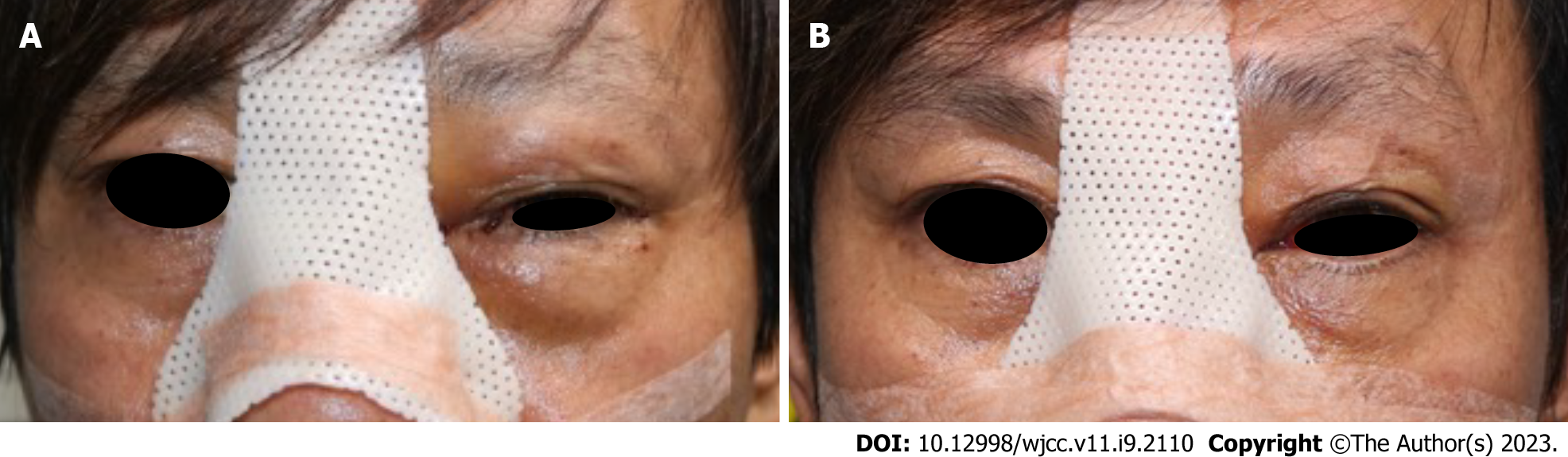
At the time of admission, periorbital swelling was not significant (Figure 1). Extraocular movement was normal, and the patient did not complain of other visual symptoms including blurred vision or diplopia. One day after the operation, crepitus was observed during skin palpations.
The blood results were within normal limit; a white blood cell count of 7.2 × 103/mL; a red blood cell count of 4.3 × 106/mL; a platelet count of 192 × 103/mL; a hemoglobin count of 12.9 g/dL; a blood urea nitrogen value of 11 mg/dL; serum creatinine value of 0.63 mg/dL; potassium, 3.3 mmol/L; sodium, 141 mmol/L; albumin, 35 g/L; total bilirubin of 3 µmol/L; alanine aminotransferase, 17 IU/L; aspartate aminotransferase, 15 IU/L; and alkaline phosphatase, 65 IU/L.
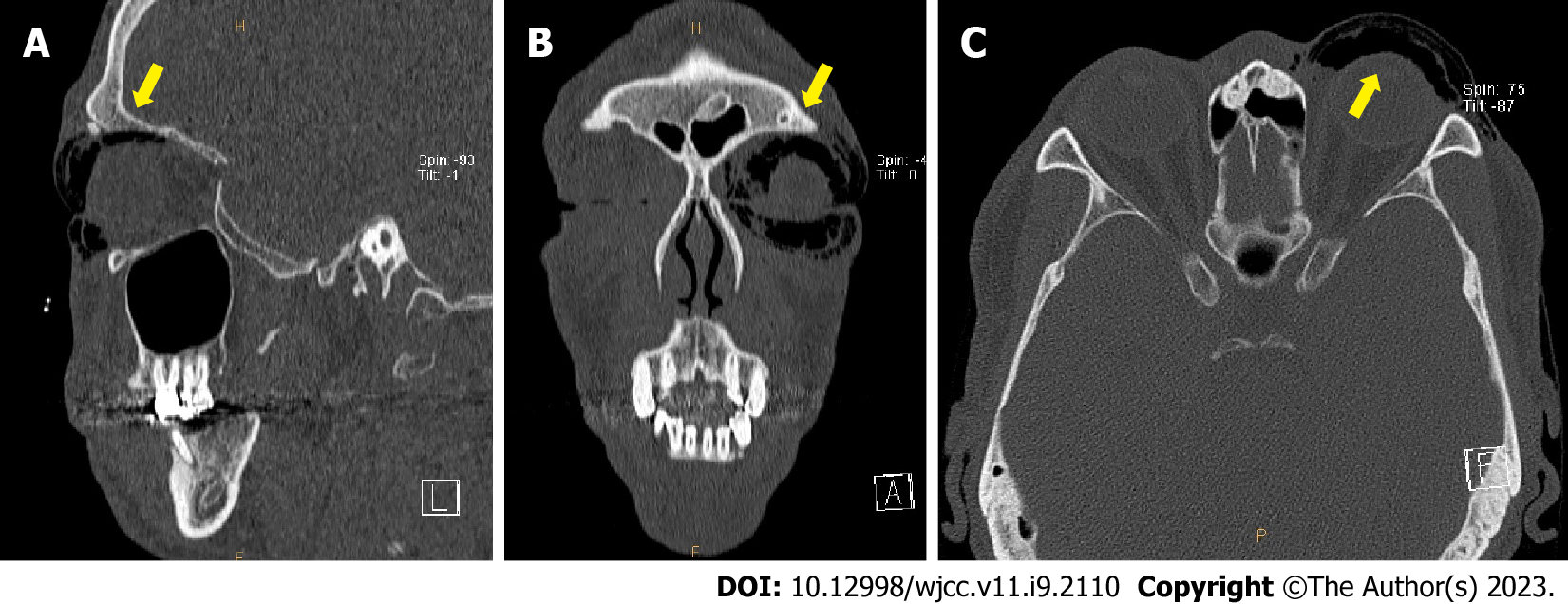
The size of the blow-out fracture was 25 mm × 20 mm accompanied by a nasal bone fracture on computed tomography that was performed after visiting the hospital.
Postoperatively, follow-up computed tomography was done and revealed emphysema in the form of scattered air bubbles in the left periorbital subcutaneous area (Figure 2).
The patient was diagnosed as postoperative subcutaneous emphysema.
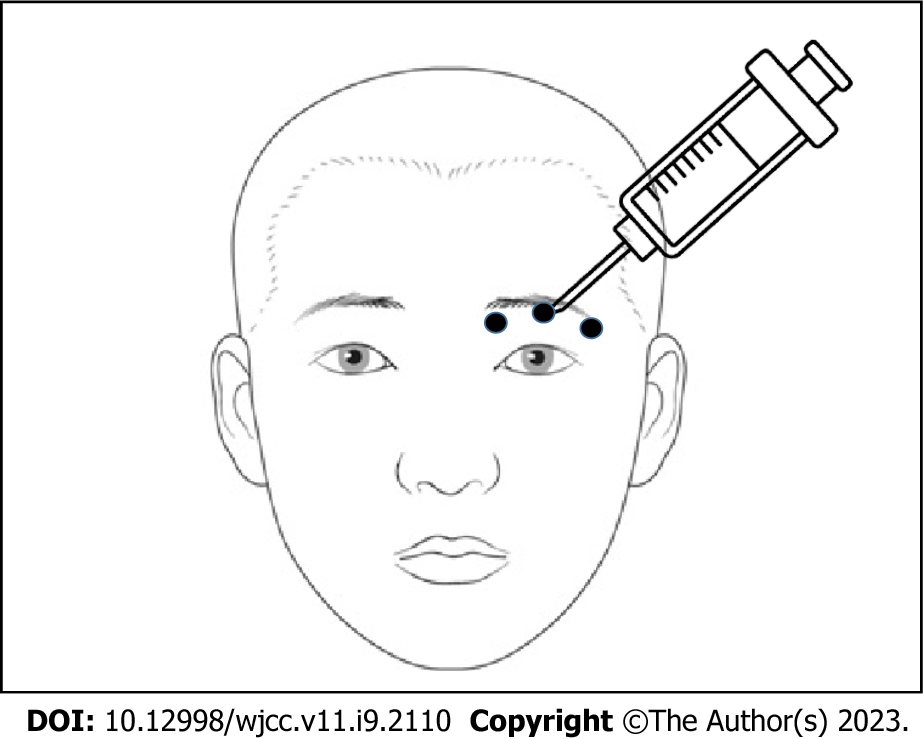
Negative pressure was applied using the needle and syringe pull-back method at three points above the eyelid crease with an 18-gauge needle, and approximately 2 mL of air was removed at each point (Figure 3). The symptoms of sudden swelling immediately improved (Figure 4). Simple foam dressing and mild compression after aspiration were performed.
No symptoms, such as bleeding or hematoma, were observed in the upper eyelid. On the fourth day postoperatively, there was no recurrence of swelling, the patient was discharged, and could immediately returned to his daily activities (Figure 5). During outpatient follow-up, recurrence of emphysema was not observed.
Orbital emphysema is commonly observed in orbital fractures[5]. A large retrospective study spanning 10 years concluded that clinically apparent orbital emphysema had a specificity of 99.6% and a positive predictive value of 98.4% for orbital fracture[6]. In cases of orbital emphysema related to orbital fractures, there is often a history of post-traumatic sneezing, coughing or nose blowing precipitating orbital emphysema[7-11]. An acute incident resulting in increased intranasal pressure, such as sneezing or nose blowing, usually promote the episode[12].
The clinical presentation of orbital emphysema varies, depending on its severity. Patients often experience tenderness, pain or pressure sensation and may complain of changes in visual acuity or field. Signs of orbital emphysema include periorbital subcutaneous crepitus, proptosis, decreased vision, relative afferent pupillary defect, and subconjunctival emphysema[5]. Given the tendency of air to localize superiorly, a crescent-shaped area of radiolucency in the superior aspect of the orbit demonstrated on a radiograph termed the “black eyebrow sign” is highly suggestive of orbital emphysema[13,14].
Most cases of orbital emphysema are self-limited and typically resolve within 7-10 d[15-18]. Moon et al[7] reviewed 348 orbits with isolated medial wall fractures and concluded that the majority of these patients recovered spontaneously without the need for surgical intervention. Patients who underwent needle aspiration and decompression tended to have a moderately decreased visual acuity. Those who underwent orbital decompression were more likely to have additional signs of optic nerve compression, indicated by the presence of a relative afferent pupillary defect and more severe impairment in visual acuity[10,19].
In our case, a sudden increase in swelling was observed, and follow-up computed tomography revealed a black eyebrow sign. As shown in the literature, orbital emphysema is often caused by trauma or soft tissue injury. However, in this case, it occurred postoperatively after reconstruction of the orbital blow-out fracture, and it is different from reports in the literature of cases, as this case was caused by an increase in intranasal pressure during sneezing. The patient experienced spontaneous sneezing, which prompted him to blow his nose the night prior to the onset of symptoms. The patient also had a nasal bone fracture, suggesting that an increase in intranasal pressure caused air to enter the surrounding subcutaneous tissue. In this case, the method of needle aspiration was used. Although it is highly likely that the emphysema would have resolved gradually, this method allowed immediate and dramatic resolution, enabling quick recovery to daily life. In addition, it has the advantage of being more comfortable and less burdensome to the patient than removal through surgical intervention.
The limitation of the method used in this case is that it was not possible to target the exact air collection area, and the procedure was performed based on palpation. In addition, resolution of emphysema after the procedure was not confirmed by follow-up imaging. As a point for improvement, we suggest that if additional diagnostic devices, such as handheld sonography are used during the procedure, needle aspiration would be a useful treatment option for orbital emphysema. Moreover, because our study represents only a single case, further investigations are required to validate our method as a viable treatment option for postoperative subcutaneous emphysema.
Orbital emphysema is a rare complication that can occur after blow-out surgery. Although orbital emphysema is often self-limiting, needle aspiration is a useful treatment method that could relieve symptoms, resolve discomfort, and enable early return to daily life in patients with postoperative subcutaneous emphysema.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Fan L, China; Jian X, China; Sultana N, Bangladesh S-Editor: Yan JP L-Editor: A P-Editor: Yan JP
| 1. | Nakamura T, Gross CW. Facial fractures. Analysis of five years of experience. Arch Otolaryngol. 1973;97:288-290. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 47] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Khojastepour L, Moannaei M, Eftekharian HR, Khaghaninejad MS, Mahjoori-Ghasrodashti M, Tavanafar S. Prevalence and severity of orbital blowout fractures. Br J Oral Maxillofac Surg. 2020;58:e93-e97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (1)] |
| 3. | Sarbajna T, Valencia MRP, Kakizaki H, Takahashi Y. Orbital Blowout Fracture and Orbital Emphysema caused by Nose Blowing. J Craniofac Surg. 2020;31:e82-e84. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Shinohara H, Shirota Y, Fujita K. Implication of differences in the incidence of orbital emphysema in ethmoidal and maxillary sinus fractures. Ann Plast Surg. 2004;53:565-569. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Rubinstein TJ, Sires BS. Re: "Orbital Emphysema: A Case Report and Comprehensive Review of the Literature". Ophthalmic Plast Reconstr Surg. 2019;35:300. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 6. | Büttner M, Schlittler FL, Michel C, Exadaktylos AK, Iizuka T. Is a black eye a useful sign of facial fractures in patients with minor head injuries? Br J Oral Maxillofac Surg. 2014;52:518-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 7. | Moon H, Kim Y, Wi JM, Chi M. Morphological characteristics and clinical manifestations of orbital emphysema caused by isolated medial orbital wall fractures. Eye (Lond). 2016;30:582-587. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 8. | Tomasetti P, Jacbosen C, Gander T, Zemann W. Emergency decompression of tension retrobulbar emphysema secondary to orbital floor fracture. J Surg Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Ababneh OH. Orbital, subconjunctival, and subcutaneous emphysema after an orbital floor fracture. Clin Ophthalmol. 2013;7:1077-1079. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Jordan DR, White GL Jr, Anderson RL, Thiese SM. Orbital emphysema: a potentially blinding complication following orbital fractures. Ann Emerg Med. 1988;17:853-855. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 35] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 11. | Gauguet JM, Lindquist PA, Shaffer K. Orbital Emphysema Following Ocular Trauma and Sneezing. Radiol Case Rep. 2008;3:124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Gonzalez F, Cal V, Elhendi W. Orbital emphysema after sneezing. Ophthalmic Plast Reconstr Surg. 2005;21:309-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 26] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Feyaerts F, Hermans R. The black eyebrow sign in orbital blowout fracture. JBR-BTR. 2009;92:251-252. [PubMed] |
| 14. | Sawicki WK, Hunter G. Eyebrow sign in facial trauma. Emerg Med J. 2011;28:962. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Ozdemir O. Orbital Emphysema Occurring During Weight Lifting. Semin Ophthalmol. 2015;30:426-428. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Chiu WC, Lih M, Huang TY, Ku WC, Wang W. Spontaneous orbital subcutaneous emphysema after sneezing. Am J Emerg Med. 2008;26:381.e1-381.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | Tseng WS, Lee HC, Kang BH. Periorbital emphysema after a wet chamber dive. Diving Hyperb Med. 2017;47:198-200. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | van Issum C, Courvoisier DS, Scolozzi P. Posttraumatic orbital emphysema: incidence, topographic classification and possible pathophysiologic mechanisms. A retrospective study of 137 patients. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:737-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Chaudhry IA, Al-Amri A, Shamsi FA, Al-Rashed W. Visual recovery after evacuation of orbital emphysema. Orbit. 2007;26:283-285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |