Published online Mar 16, 2023. doi: 10.12998/wjcc.v11.i8.1782
Peer-review started: September 30, 2022
First decision: January 3, 2023
Revised: January 17, 2023
Accepted: February 15, 2023
Article in press: February 15, 2023
Published online: March 16, 2023
Processing time: 150 Days and 14.9 Hours
Solitary hamartomatous polyps (SHPs) are rare lesions. Endoscopic full-thickness resection (EFTR) is a highly efficient and minimally invasive endoscopic procedure that benefits from complete lesion removal and high safety.
A 47-year-old man was admitted to our hospital after experiencing hypogastric pain and constipation for over fifteen days. Computed tomography and endos
On the basis of clinical and pathological evaluations, the mass was considered an SHP.
Core Tip: Solitary hamartomatous polyps (SHPs) are rarely encountered and seldom reported in the literature. Most SHPs occur in the stomach and small intestine. An SHP in the descending colon has not been reported previously. In this report, we describe a giant pedunculated polyp, approximately 18 cm long, diagnosed as an extensively pedunculated giant SHP. We successfully resected this polyp using endoscopic full-thickness resection, which provides a viable option for the clinical resection of giant pedunculated polyps.
- Citation: Ye L, Zhong JH, Liu YP, Chen DD, Ni SY, Peng FQ, Zhang S. Extensively infarcted giant solitary hamartomatous polyp treated with endoscopic full-thickness resection: A case report. World J Clin Cases 2023; 11(8): 1782-1787
- URL: https://www.wjgnet.com/2307-8960/full/v11/i8/1782.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i8.1782
Solitary hamartomatous polyps (SHPs) are a rare type of gastrointestinal disorder that in 65% of cases occur in the stomach and small intestine. Previously, this type of polyp has been considered a variant of Peutz–Jeghers syndrome; however, it is now believed to be a distinct disease[1]. Notably, the disease has no typical clinical manifestations or signs, with most cases being discovered incidentally during physical examinations or visits for complications, such as intestinal bleeding, intussusception, and obstruction. The treatment of SHP involves endoscopic or surgical resection. In this report, we describe an extensively infarcted giant SHP, which was successfully resected using EFTR. We also describe the characteristics of colonic SHP and its treatment.
Abdominal pain with constipation of over fifteen days duration.
The patient reported to our hospital with a slight pain in the hypogastrium. The course of the disease was accompanied by the passage of pellet-like stools.
The patient had no history of past illness.
There was no history of personal or family illness.
Physical examination revealed a soft, mobile, and ill-defined mass, with tenderness, in the hypo
The results of all laboratory examinations were within normal limits.
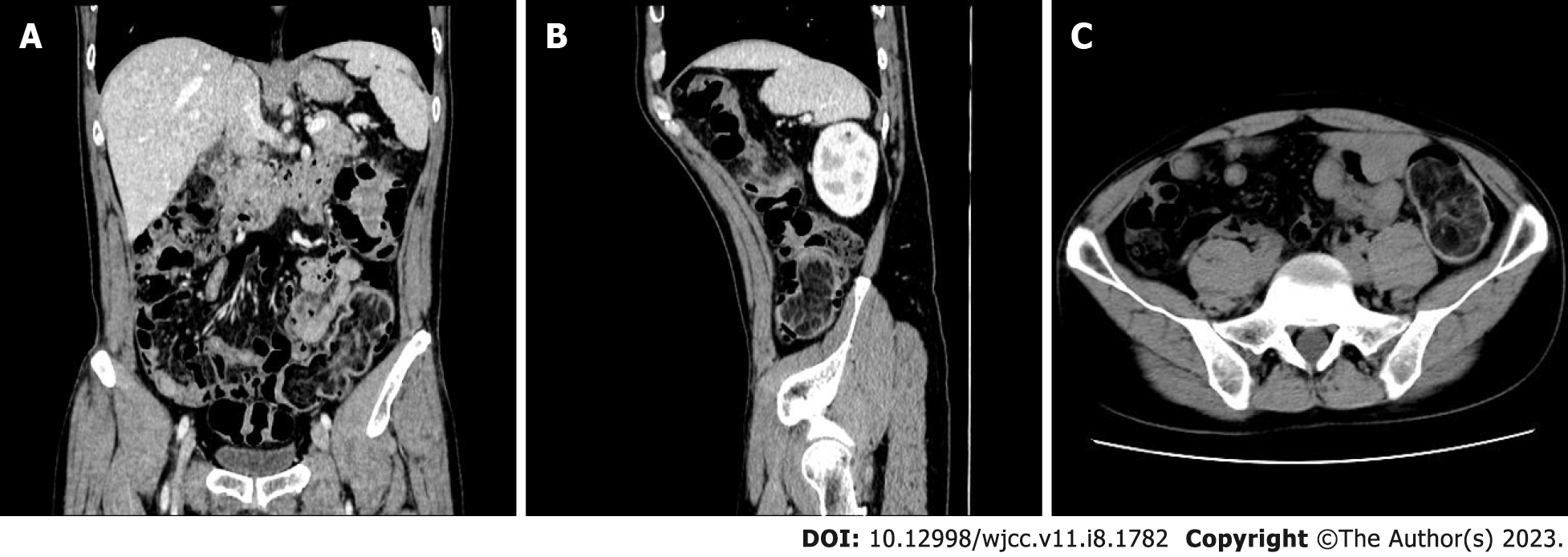
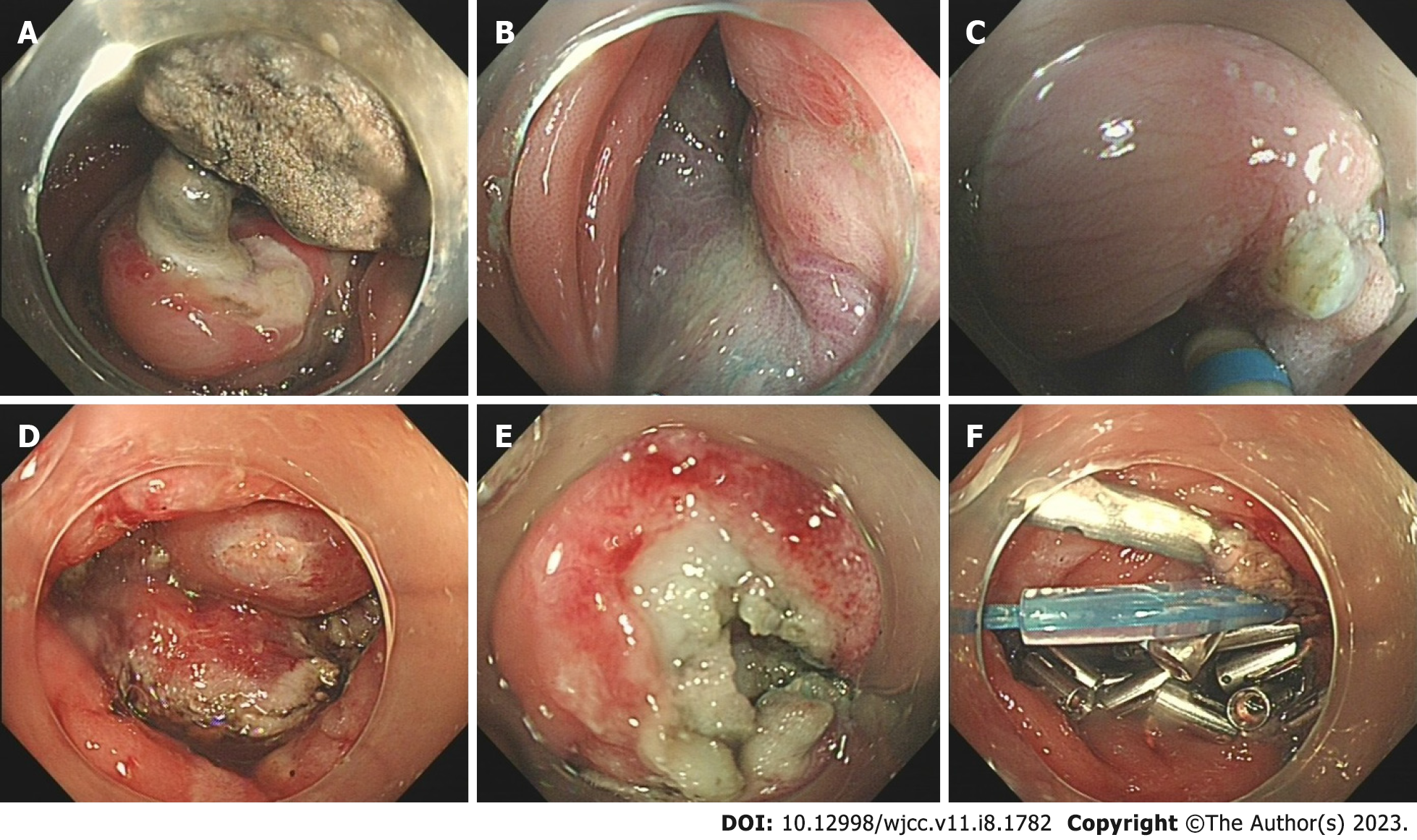
Computerized tomography revealed a lipid-laden mass, leading to intussusception (Figure 1). Endoscopy revealed a giant mass in the descending and sigmoid colons. The stalk of the mass was attached to the colonic cavity 50 cm from the anus, and the surface of the surrounding colonic cavity was eroded (Figure 2).
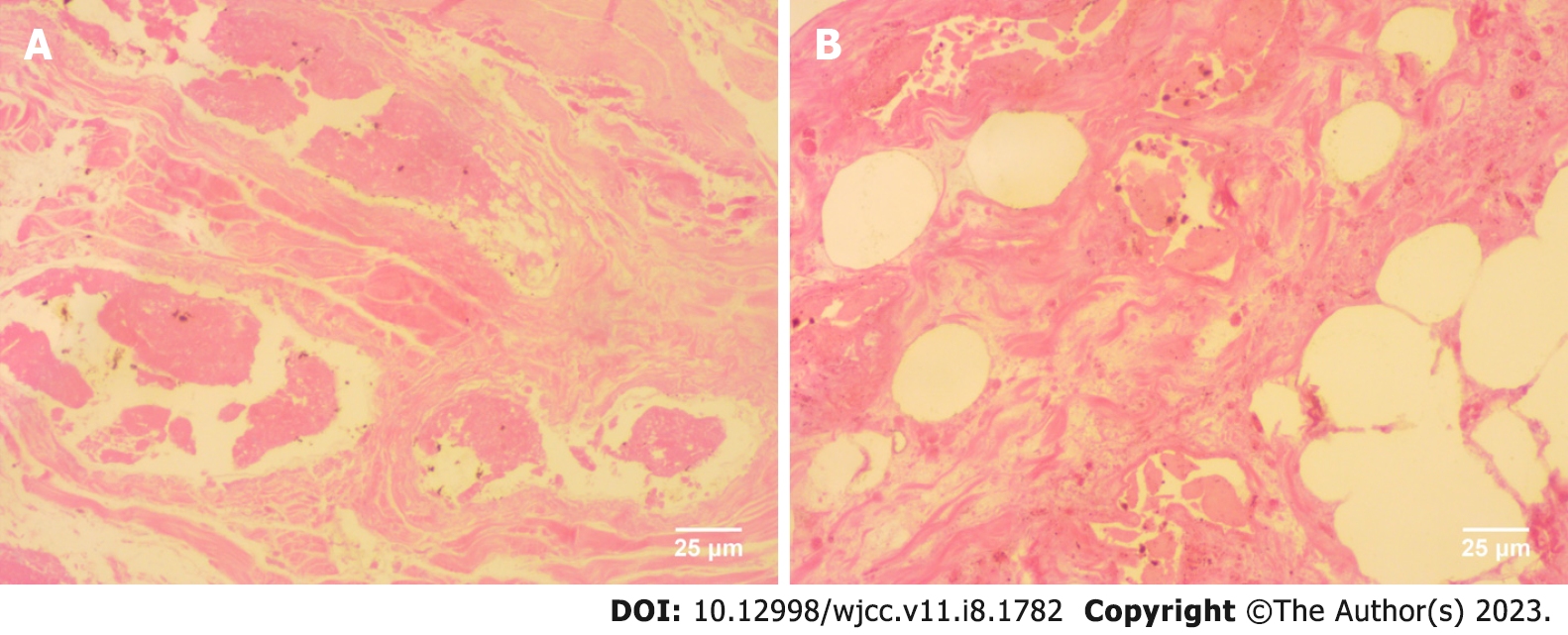
The resected specimen revealed an abnormally shaped polyp (Figure 3), and on the basis of clinical and pathological evaluations, the mass was diagnosed as an SHP.
After a detailed discussion with the patient and his family, the decision was made to perform endoscopic full-thickness resection (EFTR) to clarify the diagnosis. Having defined the extent of the lesion, an endoscopist performed a submucosal injection, followed by circumferential dissection of the submucosa along the perimeter of the lesion, using a Dual Knife (KD-611L; Olympus, Tokyo, Japan). The mass associated with the lesion was then resected using an insulated-tip knife (KD-640L; Olympus, Tokyo, Japan). Nylon loops (L-L08-04; Leo Med, Changzhou, China) and resolution clips (M00522610; Boston Scientific, Marlborough, United States) were used to ligate the wounds (Figure 2). Following suturing, the distal end of the polyp was encircled with an endoscopic snare and slowly pulled toward the rectum. Although difficulty was experienced in passing the resected polyp through the anal canal, the polyp was pulled out of the intestine intact after the application of glycerin and manual dilatation of the anus (Figure 4). Subsequently, the entire gastric and colonic cavity were examined endoscopically, which revealed no other polyps. The patient experienced vague abdominal pain after EFTR. The findings of routine blood and C-reactive protein (CRP) tests revealed that the patient had a high white blood cell count (average: 15.9 × 109/L, normal range: 3.9–9.5 × 109/L) and high levels of CRP (33.81 mg/L, normal range: 0–10 mg/L). Consequently, the administration of antibiotics (levofloxacin 0.5 g once daily) was continued to combat infection, and the patient was managed with fasting and parenteral nutrition. He was subsequently discharged from hospital after 10 d of monitoring.
At the time of discharge, the patient had no abdominal pain. Although he passed a flatus, the bowel was not voided. The final follow-up session took place nine months after the initial consultation, and he currently remains free of symptoms. Colonoscopy indicated a slight narrowing of the intestinal canal 50 cm from the anus, although no significant edema of the surrounding mucosa.
Colonic polyps, including adenomatous, inflammatory, hyperplastic, and hamartomatous polyps, and miscellaneous lesions, are among the most common diseases of the digestive tract. Hamartomatous polyps are particularly rare, with SHPs being the rarest type of gastrointestinal polyp. The SHP is a benign polyp with a considerably low incidence rate. Our review of reported cases of colonic SHP published in the EMBASE and PubMed databases revealed only five such cases[1-5]. Although patients with SHP lack specific clinical symptoms, they may have clinical manifestations, such as constipation, hematochezia, and changes in defecation habits associated with intestinal bleeding, intussusception, intestinal obstruction, and other complications. Among the cases we reviewed, one of the patients was diagnosed due to an intestinal obstruction, whereas in the other four cases, the patients were incidentally found to have a mass on physical examination. In general, colonic SHPs are less than 2 cm in size (Table 1). Endoscopically, colonic SHPs are lobulated and red, whereas microscopically, the polyp consists of glands, smooth muscle, and focal mature lymphoid tissue with a normal lamina propria structure[6]. On the basis of our analysis of the literature, we established that small hamartomatous polyps are commonly treated with endoscopic excision, whereas large polyps or polyps with other comorbidities are treated surgically. All but one of the aforementioned five patients did not have a follow-up visit, and the remainder of the patients experience no recurrence, regardless of surgical or endoscopic treatment. In the case reported herein, the polyp was endoscopically red in color and lobulated, and microscopically was characterized by widespread necrotic and liquified degenerated fibrous, smooth muscle and vascular adipose tissue. Lacunae of varying sizes were interspersed with smooth muscle tissues, and a necrotic epithelial lining was observed within the lumens. To the best of our knowledge, the extensive necrotic degeneration of the tissue owing to infarction was caused by interruption of the blood supply and obstruction of the venous return caused by twisting of the stalk of the mass.
| No. | Ref. | Size (cm) | Location | Treatment | Complications | Follow-up |
| 1 | Oluyemi et al[1], 2021 | Not mentioned | Sigmoid colon | Endoscopic | No complications | No recurrence |
| 2 | Papalampros et al[2], 2017 | Not mentioned | Sigmoid colon | Surgery | Intestinal obstruction | No recurrence |
| 3 | Vanoli et al[3], 2015 | 0.18 | Transverse colon | Endoscopic | Malignant transformation | No recurrence |
| 4 | Putra et al[4], 2019 | 2 | Transverse colon | Not mentioned | No complications | Not mentioned |
| 5 | Itaba et at[5], 2009 | 1.8 | Sigmoid colon | Endoscopic | No complications | No recurrence |
Although gastrointestinal hamartomatous polyps are not classed as tumors, they are associated with the risk of cancer. In the case presented by Vanoli et al[3], the authors reported the occurrence of an intramucosal carcinoma arising within a solitary juvenile polyp of the transverse colon. Consequently, following a diagnosis of SHP, polyp removal and general examination are considered necessary. However, although there are no established guidelines; endoscopy and surgical resection are the main surgical methods. Compared with surgical procedures, endoscopy facilitates the examination of the entire intestine at a single time and can be used to directly remove polyps. In addition, EFTR leaves only small wounds and causes less blood loss. The procedure causes less disruption of the physiological structure, thereby ensuring maximal preservation of the normal physiological function of the digestive tract and minimizing complications caused by surgery. Moreover, EFTR is typically less expensive than other procedures and causes less operative morbidity and trauma, whilst facilitating a more rapid recovery and a better quality of life than surgery[7]. The EFTR procedure can, nevertheless, have certain complications, among which, infection and wound dehiscence are two most commonly reported[8]. Infections can, however, be successfully managed using antiseptics and wound dehiscence can be minimized under endoscopic treatment. Otherwise, additional surgery should be applied. Although the safety and efficacy of laparoscopic and endoscopic cooperative surgery (LECS) is similar to that of EFTR, the operator is required to master both endoscopic and laparoscopic techniques. Consequently, we believe that LECS could be used as a treatment option for patients with large SHPs that cannot be treated using the endoscopic procedure. In the case reported herein, the experienced endoscopist removed the 18-cm-long polyp via EFTR, having taken into consideration the patient’s condition and the characteristics of the polyp. However, owing to the large nature of the resulting wound, prior to being discharged, the patient remained hospitalized for 10 d in order to prevent complications.
SHPs are a rare type of lesion that can lead to complications, including intussusception and bleeding. Consequently, SHPs should be excised at the earliest opportunity. Traditionally, surgery has been the standard approach for treating SHPs; however, with the development of endoscopic techniques, giant polyps can now be successfully removed using endoscopic surgery. EFTR thus provides a viable treatment option for the clinical removal of giant polyps.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Meshikhes AW, Saudi Arabia; Oura S, Japan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Oluyemi AO, Odeghe EA, Awolola NA. Solitary peutz-jeghers type hamartoma in a Nigerian: A case report of a rare finding and review of literature. Ann Afr Med. 2021;20:307-309. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (1)] |
| 2. | Papalampros A, Vailas MG, Sotiropoulou M, Baili E, Davakis S, Moris D, Felekouras E, Deladetsima I. Report of a case combining solitary Peutz-Jeghers polyp, colitis cystica profunda, and high-grade dysplasia of the epithelium of the colon. World J Surg Oncol. 2017;15:188. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Vanoli A, Lucioni M, Biletta E, Chiaravalli AM, Alvisi C, Luinetti O. A Wolf in Sheep's Clothing: A Sporadic Juvenile Polyp of the Colon Harboring an Intramucosal Adenocarcinoma. Int J Surg Pathol. 2015;23:571-574. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Putra J, Mulder DJ. Solitary Peutz-Jeghers type hamartomatous polyp in the transverse colon of an adolescent with ulcerative colitis. Dig Liver Dis. 2019;51:1738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 5. | Itaba S, Iboshi Y, Nakamura K, Kanayama K, Akiho H, Goto A, Yao T, Takayanagi R. Education and imaging. Gastrointestinal: Solitary Peutz-Jeghers-type hamartoma of the colon. J Gastroenterol Hepatol. 2009;24:498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Cauchin E, Touchefeu Y, Matysiak-Budnik T. Hamartomatous Tumors in the Gastrointestinal Tract. Gastrointest Tumors. 2015;2:65-74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 22] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 7. | Liu Q, Ding L, Qiu X, Meng F. Updated evaluation of endoscopic submucosal dissection vs surgery for early gastric cancer: A systematic review and meta-analysis. Int J Surg. 2020;73:28-41. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 113] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 8. | ASGE Technology Committee; Aslanian HR, Sethi A, Bhutani MS, Goodman AJ, Krishnan K, Lichtenstein DR, Melson J, Navaneethan U, Pannala R, Parsi MA, Schulman AR, Sullivan SA, Thosani N, Trikudanathan G, Trindade AJ, Watson RR, Maple JT. ASGE guideline for endoscopic full-thickness resection and submucosal tunnel endoscopic resection. VideoGIE. 2019;4:343-350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 147] [Cited by in RCA: 138] [Article Influence: 23.0] [Reference Citation Analysis (0)] |