Published online Mar 16, 2023. doi: 10.12998/wjcc.v11.i8.1694
Peer-review started: November 5, 2022
First decision: January 11, 2023
Revised: January 28, 2023
Accepted: February 21, 2023
Article in press: February 21, 2023
Published online: March 16, 2023
Processing time: 121 Days and 22.6 Hours
To optimize the efficiency of ileocolic anastomosis following right hemicolectomy, several variations of the surgical technique have been tested. These include performing the anastomosis intra- or extracorporeally or performing a stapled or hand-sewn anastomosis. Among the least studied is the configuration of the two stumps (i.e., isoperistaltic or antiperistaltic) in the case of a side-to-side anastomosis. The purpose of the present study is to compare the isoperistaltic and antiperistaltic side-to-side anastomotic configuration after right hemicolectomy by reviewing the relevant literature. High-quality literature is scarce, with only three studies directly comparing the two alternatives, and no study has revealed any significant differences in the incidence of anastomosis-related complications such as leakage, stenosis, or bleeding. However, there may be a trend towards an earlier recovery of intestinal function following antiperistaltic anastomosis. Finally, existing data do not identify a certain anastomotic configuration (i.e., isoperistaltic or antiperistaltic) as superior over the other. Thus, the most appropriate approach is to master both anastomotic techniques and select between the two configurations based on each individual case scenario.
Core Tip: This review assesses and compares two side-to-side anastomotic configurations (isoperistaltic and antiperistaltic) following right hemicolectomy. Current literature does not identify any anastomotic configuration as superior over the other. Thus, the most appropriate approach is to master both anastomotic techniques and select between the configurations based on each individual case scenario.
- Citation: Symeonidis D, Karakantas KS, Kissa L, Samara AA, Bompou E, Tepetes K, Tzovaras G. Isoperistaltic vs antiperistaltic anastomosis after right hemicolectomy: A comprehensive review. World J Clin Cases 2023; 11(8): 1694-1701
- URL: https://www.wjgnet.com/2307-8960/full/v11/i8/1694.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i8.1694
Colorectal cancer is one of the most common cancers globally, with an increasing incidence in developing countries and stabilizing trends in highly-developed countries[1]. For right-sided colon cancer, right hemicolectomy is the surgical treatment of choice[2]. Following resection, an anastomosis is performed between the terminal ileus and the transverse colon. For example, an ileocolic anastomosis may be performed to reestablish gastrointestinal tract continuity. Over the past decades, two major advances in the field of colon cancer surgery have been observed: The development of the laparoscopic approach and the concept of complete mesocolic excision (CME). Several studies have demonstrated superior short-term results and similar long-term oncological outcomes with the laparoscopic approach as compared to the traditional open approach[3,4]. Similar to the concept of total mesorectal excision for rectal tumors, Hohenberger et al[5] proposed CME for the surgical treatment of colon cancer. A recent meta-analysis has shown that a right hemicolectomy with CME is not inferior in terms of safety. Furthermore, this approach is associated with a greater lymph node yield, as well as better overall and disease-free survival as compared to traditional surgery[6]. Additionally, apart from colon cancer, terminal ileitis seen with Crohn’s disease is a common indication for a more limited type of resection (i.e., ileocecal resection) including the affected part of the small bowel, followed by an ileocolic anastomosis[7,8].
Following the resection, the efficiency and functionality of the ileocolic anastomosis influence operative outcomes and patient recovery. In the quest for optimal results, several variations of the surgical technique have been extensively tested, with studies often reporting conflicting results[9-11]. Some of the tested alternatives include conducting the anastomosis intra- or extracorporeally when the laparoscopic approach is followed, using a side-to-side or an end-to-end configuration and performing a stapled or hand-sewn anastomosis[9-11]. Parameters of success in the early postoperative period (e.g., incidence of anastomosis-related complications, time to first flatus, time to recommencing oral feeding) as well as parameters reflecting long-term results (e.g., functional recovery of the gastrointestinal tract, post-resection quality of life scores) have been commonly used as comparison end points. However, among the least-studied surgical technique aspects is the configuration of the stumps in the case of side-to-side anastomosis, (i.e., isoperistaltic or antiperistaltic stump configurations). The purpose of the present article is to assess and compare the isoperistaltic vs antiperistaltic side-to-side anastomotic configurations following a right hemicolectomy by reviewing relevant literature.
Anastomotic leakage is a clinical manifestation of a failing anastomosis. With a reported prevalence ranging between 1% and 19%, it is considered the most dramatic complication following colorectal surgery[12]. Several factors negatively influencing the physiological healing of the anastomosis have been identified. For prevention and early detection, risk factors for anastomotic leakage have been classified into preoperative, tumor-related, and intraoperative risk factors[13]. Table 1 displays potentially modifiable risk factors for anastomotic leakage, which are of the utmost importance in the preoperative setting[12,13]. From a technical perspective, the three most important factors for mastering a bowel anastomosis include: (1) Meticulous surgical technique, taking extra care to prevent hematoma formation and to achieve optimal seromuscular apposition; and (2) Adequate blood supply of the two bowel stumps; and (3) Elimination of tension at the anastomosis[14-16].
| Preoperative | Tumor related | Intraoperative | |
| Non- modifiable | Male sex | Distal tumor site | Excessive blood loss |
| ASA score > II | Tumor size > 3 cm | Need for transfusion | |
| Chronic renal disease | Advanced stage disease | Duration > 4 hours | |
| History of radiotherapy | Non-elective surgery | ||
| Metastatic disease | |||
| Modifiable | Smoking | ||
| Obesity | |||
| Poor nutrition | |||
| Alcohol abuse | |||
| Immunosuppressant use |
After right hemicolectomy, a favorable operative outcome depends primarily on the efficiency of the ileocolic anastomosis. A functional, complication-free anastomosis can guarantee an uneventful postoperative course and improved quality of life in the long-term. To identify the optimal approach, various anastomotic techniques altering several technical parameters have been proposed. In general, anastomosis can be performed either by the use of sutures (i.e., hand-sewn anastomosis) or by the use of stapling devices (i.e., stapled anastomosis).
Hand-sewn anastomosis can be performed with the use of various suture materials. Materials such as silk, linen, catgut, and nylon were traditionally utilized for colorectal anastomosis. Generally, the use of absorbable or multi-filament sutures can increase tissue reaction and damage, without the guarantee of uneventful anastomosis healing[17]. Today, most gastrointestinal anastomoses are performed using slowly absorbable monofilament polydioxanone sutures[17]. In earlier decades, a double-layer inverting anastomotic technique was the standard for gastrointestinal anastomosis[18]. However, single-layer anastomosis became popular following favorable results reported by various studies[18,19]. More recent studies have failed to demonstrate a difference between the double- and single-layer techniques[20,21]. However, a single-layer continuous anastomosis costs less and can be constructed in significantly less time, with a similar complication rate as compared to the two-layer technique[22]. The dilemma in choosing between interrupted or continuous sutures arose when single-layer anastomoses became the standard of practice. As existing literature on the subject is limited and does not show obvious trends, a continuous suture may be preferable to interrupted sutures for creating intestinal anastomosis, since it is less time-consuming and technically simpler[23,24].
Conversely, stapled anastomosis can include the use of different types of stapling devices. These include linear, transverse, and circular staplers with two- or three-row stapling line systems. Following the introduction of stapled colorectal anastomosis in the 1980s, both techniques (hand sewn and stapled anastomosis) have become available for the majority of surgeons. Several studies have compared these techniques[25]. A Cochrane review conducted by Choy et al[11] concluded that stapled functional end-to-end ileocolic anastomosis after right hemicolectomy is associated with fewer leaks as compared to hand-sewn anastomosis. However, the difference was not considered statistically significant when the clinically significant anastomotic leaks were used as the comparison endpoint[11]. In general, superiority of the stapled over the hand-sewn anastomosis has not been documented in the available literature[26].
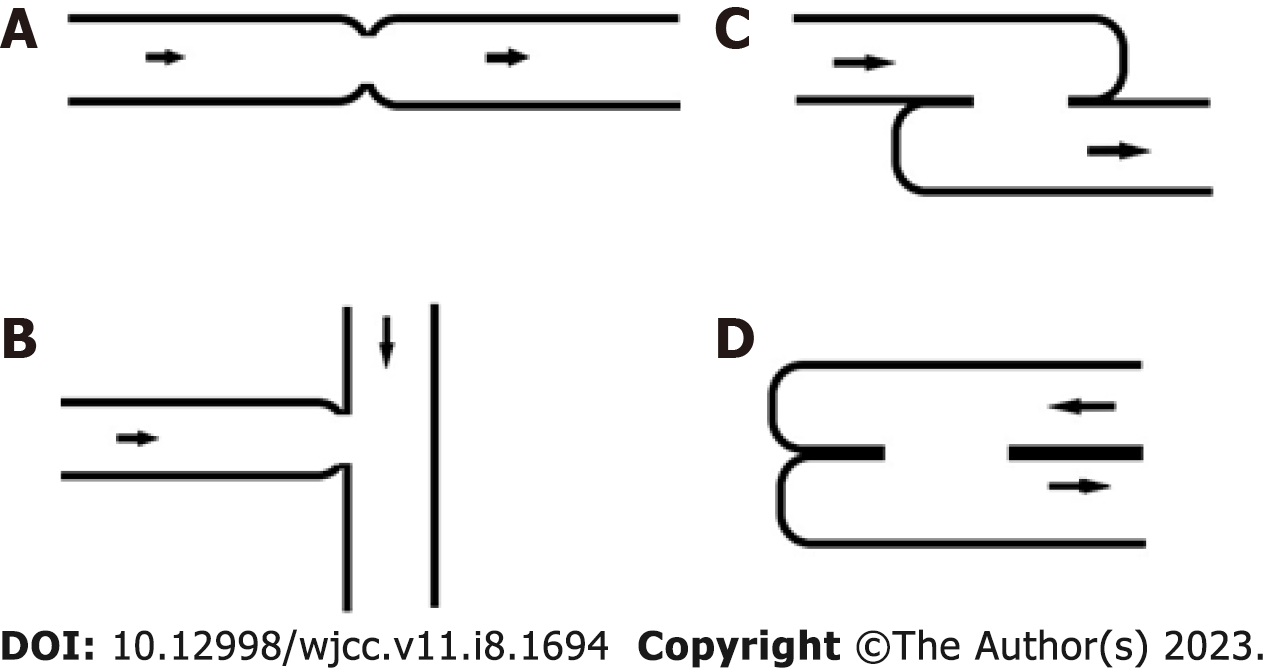
Irrespective of the use of sutures or stapling devices, anastomoses can be further classified based on the configuration of the two stumps, (i.e., end-to-end, end-to-side and side-to-side)[15] (Figure 1). Specifically for the side-to-side configuration, an additional distinction is made between isoperistaltic and antiperistaltic anastomoses, depending on the configuration and orientation of the two stumps. In the isoperistaltic variant, the peristaltic flow in both parts is towards the same normal, aboral direction (Figure 1).
Several technical parameters influence the final form of an intestinal anastomosis. In the case of a side-to-side anastomosis, one of these parameters is the configuration of the two bowel stumps as isoperistaltic or antiperistaltic. In attempt to identify the optimal configuration, interpretation of the reviewed studies is muddied by the modification of additional technical parameters in addition to the selection of an anastomotic configuration alone. The field becomes even more unclear with increased prevalence of laparoscopic surgery and incorporation of CME principles in colorectal cancer surgery, which have notably increased heterogeneity of the comparison groups[3,4,6]. Moreover, the endpoint of functional recovery following colonic resections, time to first flatus, which has been used to compare the two configurations, seems to be influenced by the presence of other confounding factors.
Generally, the ideal intestinal anastomosis is one that can be easily performed from a technical perspective, can be reproduced by surgeons without advanced surgical skills, is associated with low or no rate of complication due to leakage or stenosis, and is aligned with the physiological function of the gastrointestinal tract. To date, no single technique or anastomotic form can guarantee success with respect to these desired characteristics. Traditionally, a hand-sewn end-to-end anastomosis has been considered the standard approach for reestablishing gastrointestinal tract continuity after colonic resection[27]. However, this approach was associated with an increased incidence of anastomosis-related complications, mainly stenosis, particularly if a notable discrepancy occurred in the luminal diameter of the two stumps and in the setting of significant prolongation of operative time[27,28].
After the introduction of stapling devices, a shift in surgical trends was seen from the use of hand-sewn towards stapled anastomosis[29]. A side-to-side stapled anastomosis became the new standard as a rapid and easier alternative, and it allowed surgeons to overcome technical difficulties posed when a significant discrepancy in the luminal diameter of the two stumps was present[30]. Increased safety due to lower anastomotic failure rates was attributed to the stapled approach, at least in early comparative studies[28,29,31-35]. As more colorectal cancer resections are performed laparoscopically, another surgical dilemma has emerged; namely, whether to perform the anastomosis intra- or extracorporeally. In 2003, Casciola et al[36] reported the first intracorporeal ileocolic anastomosis after a laparoscopic right hemicolectomy. Generally, performing an intracorporeal anastomosis following laparoscopic right hemicolectomy appears to be associated with quicker recovery of postoperative bowel function, decreased infection rates, and overall postoperative complications when compared to the extracorporeal anastomotic approach[36-38].
Side-to-side anastomoses are considered to have certain advantages over end-to-end anastomoses, including better blood supply and wider diameter. In addition, the detrimental effect of increased intraluminal pressure on the healing process of an anastomosis seems to be more efficiently addressed by the side-to-side configuration[39,40]. A side-to-side ileocolic anastomosis appears to be the preferred anastomotic configuration by the majority of colorectal surgeons[41]. The end-to-side ileocolic configuration following right hemicolectomy has recently gained popularity due to the favorable results reported from retrospective cohort studies comparing end-to-side with side-to-side anastomosis[42-44]. Lower leakage rates and faster recovery at the expense of increased technical difficulty were reported after end-to-side anastomosis as compared to side-to-side anastomosis[42-44]. Several theoretical advantages have been attributed to the end-to-side configuration. This configuration resembles the physiological entry point of the ileum into the cecum lumen, results in less damage to luminal muscle fibers, and has been shown to withstand higher intraluminal pressures than end-to-end anastomosis[45,6]. However, these results were not confirmed in a study by Kim et al[47] which is the only available prospective randomized trial in the field, nor by any large retrospective cohort studies.
A side-to-side anastomosis can be performed either with an isoperistaltic or antiperistaltic orientation of the two stumps[48] (Figure 1). In 2005, Tewari et al[49] proposed the isoperistaltic, stapled, side-to-side ileocolic anastomosis after right hemicolectomy, rather than the antiperistaltic side-to-side anastomosis which was most common at the time. Despite being the most anatomical anastomotic configuration (as it is consistent with the physiological flow of the intestinal contents), a theoretical limitation of the isoperistaltic side-to-side configuration is that it requires additional mobilization to achieve adequate overlap of the two stumps. Therefore, challenges may arise in cases where the location of the anastomosis precludes such maneuvers, such as in low rectal anastomosis. However, as the isoperistaltic orientation has already proven valid in other anatomical locations such as the biliary tree, esophagus, and stomach, it could represent the optimal approach to reestablish gastrointestinal tract continuity following colonic resection[48].
Conversely, it has been postulated that the antiperistaltic orientation could reduce the incidence of postoperative ileus, since an ileocolic anastomosis could prevent the mesentery twist seen with the isoperistaltic variant[49]. After the resection of the ileocecal valve in right hemicolectomy, reflux of colonic contents in the terminal ileus may occur. The disruption of the physiological direction of colonic content flow may be associated with secondary bacterial overgrowth in the small bowel lumen[50]. The prolonged small bowel transit times attributable to this increasingly recognized syndrome appear to be more adequately prevented with antiperistaltic anastomosis[50]. This certain anastomotic orientation likely acts through a functional pseudovalvular mechanism, diminishing ileocecal reflux and postoperative ileus[49].
Few studies have directly compared the two anastomotic orientations. In 2003, Ibáñez et al[51] published a narrative review on intracorporeal anastomosis and analyzed the configuration as a possible risk factor for leakage. The authors concluded that there was no difference in anastomotic breakdown when isoperistaltic and antiperistaltic anastomoses were compared. Nevertheless, various studies have utilized different surgical techniques depending on the configuration type (i.e., the isoperistaltic orientation was achieved with stapled and hand-sewn intracorporeal anastomoses, while the antiperistaltic anastomoses were all stapled).
To our knowledge, only three studies have directly compared the isoperistaltic and antiperistaltic orientations for ileocolic anastomoses. The first was a study by Chander Roland et al[52] in which the authors conducted a randomized controlled trial comparing isoperistaltic vs antiperistaltic stapled side-to-side ileocolic and colocolic anastomoses in colon cancer patients. There were 20 elective resection patients in each study arm. While the antiperistaltic anastomoses were all stapled, the authors used a running suture to close the stapling device entry hole in the isoperistaltic anastomoses to prevent iatrogenic stenosis of the ileum stump. The primary endpoints were rates of anastomotic leakage, hemorrhage, and stenosis. Across all endpoints, no significant differences were observed between the two groups. Specifically, anastomotic leakage was seen in 2 patients from the isoperistaltic group, compared to none from the antiperistaltic group (P = 0.487). One patient from the antiperistaltic group had anastomotic stenosis, while there was no stenosis in the isoperistaltic group (P = 1.000). Median postoperative length of hospital stay was similar between the two groups (P = 0.313). However, the study was suspended due to excess morbidity detected in the isoperistaltic group. While the study did not show any short-term differences between the isoperistaltic and antiperistaltic side-to-side anastomoses, considering that anastomotic leakage occurred only in the isoperistaltic group, study authors suggested that additional modifications to the isoperistaltic technique may be justified. This study had several limitations that must be considered, including small sample size, the different anastomotic types included in the analysis (both ileocolic and colocolic anastomoses), the use of both open and laparoscopic approaches, and the dissimilar technical parameters used between the groups (i.e., the author used additional sutures to reinforce the antiperistaltic anastomosis).
The second study was the ISOVANTI trial published by Tewari et al[49]. This was a double-blind, randomized, prospective trial in colon cancer patients undergoing laparoscopic right hemicolectomy and isoperistaltic or antiperistaltic ileocolic anastomosis. A total of 108 patients were randomized either to isoperistaltic or antiperistaltic configuration groups. No differences in surgical time, anastomotic time, or postoperative complication rates (37.0% isoperistaltic vs 40.7% antiperistaltic, P = 0.693) were identified. In addition, there were no differences in postoperative ileus or anastomotic leakage rates (3.7% vs 5.56%, P = 1.00). However, the antiperistaltic configuration was associated with decreased "time to first flatus" and "time to first deposition" (P = 0.004 and P = 0.017, respectively). In the long-term, there were no differences between the groups at 1, 6 or 12 mo. There was also no difference in the rate of chronic diarrhea rate. The authors concluded that the isoperistaltic and antiperistaltic ileocolic anastomosis configurations present similar results in terms of performance, safety, and functionality.
The third study by Tarta et al[53] retrospectively reviewed 214 consecutive patients who underwent laparoscopic right colectomy with gastrointestinal tract continuity reestablished either by an isoperistaltic side-to-side anastomosis or an antiperistaltic side-to-side anastomosis. These anastomotic configurations proved similar in all short-term comparison categories, including operating time, intraoperative bleeding, length of resected intestine, number of harvested lymph nodes, length of incision, time to first flatus, time to first defecation, postoperative complications, and length of hospital stay. Similarly, at a median follow-up time of 35.6 mo, there were no differences in the long-term outcomes. The authors concluded that both configurations are safe, and are associated with similar short- and long-term outcomes. Despite the fact that this study has the larger sample size than the studies discussed above, it is limited by its retrospective nature. However, it is the only study that assessed oncological outcomes following the use of different anastomotic orientations.
Relevant, high-quality data are scarce, making it difficult to draw definite conclusions regarding optimal anastomotic configuration. None of the three aforementioned studies reported any significant differences between the configurations, including no differences in the incidences of anastomosis-related complications such as leakage, stenosis, and bleeding[49,52-55]. There may be a trend towards shorter intestinal function recovery time following antiperistaltic anastomosis; however, the small sample size and associated lack of statistical significance render any such conclusion unclear. High-quality, prospective randomized trials are needed to fully elucidate the optimal anastomotic configuration after a right hemicolectomy.
In conclusion, existing data are insufficient to favor either isoperistaltic or antiperistaltic anastomotic configuration. Thus, the most appropriate approach is to master both anastomotic techniques and select the appropriate configuration based on each individual case scenario.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C, C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Feng B, China; Gad EH, Egypt; Kurtcehajic A, Bosnia and Herzegovina; Luo W, China S-Editor: Wang LL L-Editor: Filipodia P-Editor: Wang LL
| 1. | Arnold M, Sierra MS, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global patterns and trends in colorectal cancer incidence and mortality. Gut. 2017;66:683-691. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3058] [Cited by in RCA: 3306] [Article Influence: 413.3] [Reference Citation Analysis (3)] |
| 2. | Baran B, Mert Ozupek N, Yerli Tetik N, Acar E, Bekcioglu O, Baskin Y. Difference Between Left-Sided and Right-Sided Colorectal Cancer: A Focused Review of Literature. Gastroenterology Res. 2018;11:264-273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 172] [Cited by in RCA: 338] [Article Influence: 48.3] [Reference Citation Analysis (1)] |
| 3. | Guillou PJ, Quirke P, Thorpe H, Walker J, Jayne DG, Smith AM, Heath RM, Brown JM; MRC CLASICC trial group. Short-term endpoints of conventional versus laparoscopic-assisted surgery in patients with colorectal cancer (MRC CLASICC trial): multicentre, randomised controlled trial. Lancet. 2005;365:1718-1726. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2360] [Cited by in RCA: 2298] [Article Influence: 114.9] [Reference Citation Analysis (0)] |
| 4. | Veldkamp R, Kuhry E, Hop WC, Jeekel J, Kazemier G, Bonjer HJ, Haglind E, Påhlman L, Cuesta MA, Msika S, Morino M, Lacy AM; COlon cancer Laparoscopic or Open Resection Study Group (COLOR). Laparoscopic surgery versus open surgery for colon cancer: short-term outcomes of a randomised trial. Lancet Oncol. 2005;6:477-484. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1691] [Cited by in RCA: 1680] [Article Influence: 84.0] [Reference Citation Analysis (0)] |
| 5. | Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S. Standardized surgery for colonic cancer: complete mesocolic excision and central ligation--technical notes and outcome. Colorectal Dis. 2009;11:354-64; discussion 364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 990] [Cited by in RCA: 1104] [Article Influence: 69.0] [Reference Citation Analysis (0)] |
| 6. | Anania G, Davies RJ, Bagolini F, Vettoretto N, Randolph J, Cirocchi R, Donini A. Right hemicolectomy with complete mesocolic excision is safe, leads to an increased lymph node yield and to increased survival: results of a systematic review and meta-analysis. Tech Coloproctol. 2021;25:1099-1113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 7. | Chen W, Zhou J, Chen M, Jiang C, Qian Q, Ding Z. Isoperistaltic side-to-side anastomosis for the surgical treatment of Crohn disease. Ann Surg Treat Res. 2022;103:53-61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 8. | Ng CH, Chin YH, Lin SY, Koh JWH, Lieske B, Koh FH, Chong CS, Foo FJ. Kono-S anastomosis for Crohn's disease: a systemic review, meta-analysis, and meta-regression. Surg Today. 2021;51:493-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 35] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 9. | Ricci C, Casadei R, Alagna V, Zani E, Taffurelli G, Pacilio CA, Minni F. A critical and comprehensive systematic review and meta-analysis of studies comparing intracorporeal and extracorporeal anastomosis in laparoscopic right hemicolectomy. Langenbecks Arch Surg. 2017;402:417-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 77] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 10. | Würtz HJ, Bundgaard L, Rahr HB, Frostberg E. Anastomosis technique and leakage rates in minimally invasive surgery for right-sided colon cancer. A retrospective national cohort study. Int J Colorectal Dis. 2022;37:701-708. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Choy PY, Bissett IP, Docherty JG, Parry BR, Merrie A, Fitzgerald A. Stapled versus handsewn methods for ileocolic anastomoses. Cochrane Database Syst Rev. 2011;CD004320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 110] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 12. | Sciuto A, Merola G, De Palma GD, Sodo M, Pirozzi F, Bracale UM, Bracale U. Predictive factors for anastomotic leakage after laparoscopic colorectal surgery. World J Gastroenterol. 2018;24:2247-2260. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 263] [Cited by in RCA: 224] [Article Influence: 32.0] [Reference Citation Analysis (2)] |
| 13. | McDermott FD, Heeney A, Kelly ME, Steele RJ, Carlson GL, Winter DC. Systematic review of preoperative, intraoperative and postoperative risk factors for colorectal anastomotic leaks. Br J Surg. 2015;102:462-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 427] [Cited by in RCA: 589] [Article Influence: 58.9] [Reference Citation Analysis (0)] |
| 14. | Kirk RM, Winslet M. Essential General Surgical Operations. Edinburgh: Churchill Livingstone, 2001. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | Goulder F. Bowel anastomoses: The theory, the practice and the evidence base. World J Gastrointest Surg. 2012;4:208-213. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 58] [Cited by in RCA: 59] [Article Influence: 4.5] [Reference Citation Analysis (1)] |
| 16. | Scott-Conner CEH. Chassin’s Operative Strategy in General Surgery. Heidelberg: Springer, 2002. |
| 17. | Slieker JC, Daams F, Mulder IM, Jeekel J, Lange JF. Systematic review of the technique of colorectal anastomosis. JAMA Surg. 2013;148:190-201. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 122] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 18. | Gambee LP. A single-layer open intestinal anastomosis applicable to the small as well as the large intestine. West J Surg Obstet Gynecol. 1951;59:1-514798834. |
| 19. | Gambee LP, Garnjobst W, Hardwick CE. Ten years' experience with a single layer anastomosis in colon surgery. Am J Surg. 1956;92:222-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 72] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 20. | Everett WG. A comparison of one layer and two layer techniques for colorectal anastomosis. Br J Surg. 1975;62:135-140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 80] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 21. | Ceraldi CM, Rypins EB, Monahan M, Chang B, Sarfeh IJ. Comparison of continuous single layer polypropylene anastomosis with double layer and stapled anastomoses in elective colon resections. Am Surg. 1993;59:168-171. [PubMed] |
| 22. | Burch JM, Franciose RJ, Moore EE, Biffl WL, Offner PJ. Single-layer continuous versus two-layer interrupted intestinal anastomosis: a prospective randomized trial. Ann Surg. 2000;231:832-837. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 84] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 23. | Deen KI, Smart PJ. Prospective evaluation of sutured, continuous, and interrupted single layer colonic anastomoses. Eur J Surg. 1995;161:751-753. [PubMed] |
| 24. | AhChong AK, Chiu KM, Law IC, Chu MK, Yip AW. Single-layer continuous anastomosis in gastrointestinal surgery: a prospective audit. Aust N Z J Surg. 1996;66:34-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | MacRae HM, McLeod RS. Handsewn vs. stapled anastomoses in colon and rectal surgery: a meta-analysis. Dis Colon Rectum. 1998;41:180-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 143] [Cited by in RCA: 129] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 26. | Steger J, Jell A, Ficht S, Ostler D, Eblenkamp M, Mela P, Wilhelm D. Systematic Review and Meta-Analysis on Colorectal Anastomotic Techniques. Ther Clin Risk Manag. 2022;18:523-539. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 27. | Ruggiero R, Sparavigna L, Docimo G, Gubitosi A, Agresti M, Procaccini E, Docimo L. Post-operative peritonitis due to anastomotic dehiscence after colonic resection. Multicentric experience, retrospective analysis of risk factors and review of the literature. Ann Ital Chir. 2011;82:369-375. [PubMed] |
| 28. | Golda T, Lazzara C, Zerpa C, Sobrino L, Fico V, Kreisler E, Biondo S. Risk factors for ileocolic anastomosis dehiscence; a cohort study. Am J Surg. 2020;220:170-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 29. | Kracht M, Hay JM, Fagniez PL, Fingerhut A. Ileocolonic anastomosis after right hemicolectomy for carcinoma: stapled or hand-sewn? Int J Colorectal Dis. 1993;8:29-33. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 68] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 30. | Kyzer S, Gordon PH. The stapled functional end-to-end anastomosis following colonic resection. Int J Colorectal Dis. 1992;7:125-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | Steichen FM. The use staplers in anatomical side-to-side and functional end-to-end enteroanastomosis. Surgery. 1968;64:948. |
| 32. | Hashemi M, Novell JR, Lewis AA. Side-to-side stapled anastomosis may delay recurrence in Crohn's disease. Dis Colon Rectum. 1998;41:1293-1296. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 65] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 33. | Muñoz-Juárez M, Yamamoto T, Wolff BG, Keighley MR. Wide-lumen stapled anastomosis vs. conventional end-to-end anastomosis in the treatment of Crohn's disease. Dis Colon Rectum. 2001;44:20-5; discussion 25. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 104] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 34. | Resegotti A, Astegiano M, Farina EC, Ciccone G, Avagnina G, Giustetto A, Campra D, Fronda GR. Side-to-side stapled anastomosis strongly reduces anastomotic leak rates in Crohn's disease surgery. Dis Colon Rectum. 2005;48:464-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 91] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 35. | Yamamoto T, Keighley MR. Stapled functional end-to-end anastomosis in Crohn's disease. Surg Today. 1999;29:679-681. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 36. | Casciola L, Ceccarelli G, Di Zitti L, Valeri R, Bellochi R, Bartoli A, Barbieri F, Spaziani A, D'Ajello M. [Laparoscopic right hemicolectomy with intracorporeal anastomosis. Technical aspects and personal experience]. Minerva Chir. 2003;58:621-627. [PubMed] [DOI] [Full Text] |
| 37. | Zhang H, Sun N, Fu Y, Zhao C. Intracorporeal versus extracorporeal anastomosis in laparoscopic right colectomy: updated meta-analysis of randomized controlled trials. BJS Open. 2021;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 38. | Cheek FE, Tomarchio T, Burtle V, Moss H, McConnell D. A behavior modification training program for staff working with drug addicts. Int J Addict. 1975;10:1073-1101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 36] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 39. | Małczak P, Wysocki M, Pisarska-Adamczyk M, Major P, Pędziwiatr M. Bowel function after laparoscopic right hemicolectomy: a randomized controlled trial comparing intracorporeal anastomosis and extracorporeal anastomosis. Surg Endosc. 2022;36:4977-4982. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 26] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 40. | Soluble CD4: another therapeutic option in HIV infection. Lancet. 1990;335:1128-1130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 41. | Hallböök O, Johansson K, Sjödahl R. Laser Doppler blood flow measurement in rectal resection for carcinoma--comparison between the straight and colonic J pouch reconstruction. Br J Surg. 1996;83:389-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 94] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 42. | Allaix ME, Degiuli M, Bonino MA, Arezzo A, Mistrangelo M, Passera R, Morino M. Intracorporeal or Extracorporeal Ileocolic Anastomosis After Laparoscopic Right Colectomy: A Double-blinded Randomized Controlled Trial. Ann Surg. 2019;270:762-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 138] [Article Influence: 27.6] [Reference Citation Analysis (0)] |
| 43. | Garofalo E, Selvaggi F, Spinelli A, Pellino G, Flashman K, Frasson M, Carvello M, de'Angelis N, Garcia-Granero A, Harper M, Warusavitarne J, Coleman M, Espin E, Celentano V. Surgical management of complex ileocolonic Crohn's disease: a survey of IBD colorectal surgeons to assess variability in operative strategy. Int J Colorectal Dis. 2021;36:1811-1815. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 44. | Puleo S, Sofia M, Trovato MA, Pesce A, Portale TR, Russello D, La Greca G. Ileocolonic anastomosis: preferred techniques in 999 patients. A multicentric study. Surg Today. 2013;43:1145-1149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 45. | Lee KH, Lee SM, Oh HK, Lee SY, Ihn MH, Kim DW, Kang SB. Comparison of anastomotic configuration after laparoscopic right hemicolectomy under enhanced recovery program: side-to-side versus end-to-side anastomosis. Surg Endosc. 2016;30:1952-1957. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (1)] |
| 46. | Liu Z, Wang G, Yang M, Chen Y, Miao D, Muhammad S, Wang X. Ileocolonic anastomosis after right hemicolectomy for colon cancer: functional end-to-end or end-to-side? World J Surg Oncol. 2014;12:306. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 23] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 47. | Kim MH, Kang SI, Cho JR, Lee J, Yang IJ, Suh JW, Oh HK, Kim DW, Kang SB. Objective recovery time with end-to-side versus side-to-side anastomosis after laparoscopic right hemicolectomy for colon cancer: a randomized controlled trial. Surg Endosc. 2022;36:2499-2506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 48. | Baqar AR, Wilkins S, Wang WC, Oliva K, Centauri S, Yap R, McMurrick P. A comparison of extracorporeal side to side or end to side anastomosis following a laparoscopic right hemicolectomy for colon cancer. ANZ J Surg. 2022;92:1472-1479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 49. | Tewari M, Shukla HS. Right colectomy with isoperistaltic side-to-side stapled ileocolic anastomosis. J Surg Oncol. 2005;89:99-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 50. | Matsumoto S, Wakatsuki K, Migita K, Ito M, Nakade H, Kunishige T, Kitano M, Nakatani M, Sho M. Predictive Factors for Delayed Gastric Emptying after Distal Gastrectomy with Roux-en-Y Reconstruction. Am Surg. 2018;84:1086-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 51. | Ibáñez N, Abrisqueta J, Luján J, Hernández Q, Rufete MD, Parrilla P. Isoperistaltic versus antiperistaltic ileocolic anastomosis. Does it really matter? Surg Endosc. 2019;33:2850-2857. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 52. | Chander Roland B, Mullin GE, Passi M, Zheng X, Salem A, Yolken R, Pasricha PJ. A Prospective Evaluation of Ileocecal Valve Dysfunction and Intestinal Motility Derangements in Small Intestinal Bacterial Overgrowth. Dig Dis Sci. 2017;62:3525-3535. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 53. | Tarta C, Bishawi M, Bergamaschi R. Intracorporeal ileocolic anastomosis: a review. Tech Coloproctol. 2013;17:479-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 42] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 54. | Matsuda A, Miyashita M, Matsumoto S, Sakurazawa N, Takahashi G, Yamada M, Uchida E. Isoperistaltic versus antiperistaltic stapled side-to-side anastomosis for colon cancer surgery: a randomized controlled trial. J Surg Res. 2015;196:107-112. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 55. | Zhang M, Lu Z, Hu X, Zhou H, Zheng Z, Liu Z, Wang X. Comparison of the short-term outcomes between intracorporeal isoperistaltic and antiperistaltic totally stapled side-to-side anastomosis for right colectomy: A retrospective study on 214 consecutive patients. Surg Open Sci. 2022;9:7-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |