Published online Feb 16, 2023. doi: 10.12998/wjcc.v11.i5.1129
Peer-review started: October 25, 2022
First decision: December 13, 2022
Revised: December 24, 2022
Accepted: January 20, 2023
Article in press: January 20, 2023
Published online: February 16, 2023
Processing time: 111 Days and 14.3 Hours
Hemorrhagic chronic radiation proctitis (CRP) is a common late complication of irradiation of the pelvis and seriously impairs life quality. There is no standard treatment for hemorrhagic CRP. Medical treatment, interventional treatment, and surgery are available, but they are limited in their applications due to nondefinite efficacy or side effects. Chinese herbal medicine (CHM), as a complementary or alternative therapy, may provide another option for hemorrhagic CRP treatment.
A 51-year-old woman with cervical cancer received intensity-modulated radiation therapy and brachytherapy with a total dose of 93 Gy fifteen days after hysterectomy and bilateral adnexectomy. She received six additional cycles of chemotherapy with carboplatin and paclitaxel. Nine months after radiotherapy treatment, she mainly complained of 5-6 times diarrhea daily and bloody purulent stools for over 10 d. After colonoscopy examinations, she was diagnosed with hemorrhagic CRP with a giant ulcer. After assessment, she received CHM treatment. The specific regimen was 150 mL of modified Gegen Qinlian decoction (GQD) used as a retention enema for 1 mo, followed by replacement with oral administration of 150 mL of modified GQD three times per day for 5 mo. After the whole treatment, her diarrhea reduced to 1-2 times a day. Her rectal tenesmus and mild pain in lower abdomen disappeared. Both colonoscopy and magnetic resonance imaging confirmed its significant improvement. During treatment, there were no side effects, such as liver and renal function damage.
Modified GQD may be another effective and safe option for hemorrhagic CRP patients with giant ulcers.
Core Tip: We report a case of hemorrhagic chronic radiation proctitis (CRP) in a patient with a giant rectal ulcer who achieved significant remission via retention enema and oral administration of modified Gegen Qinlian decoction (GQD). As an alternative and complementary medicine, modified GQD may be another effective and safe option for hemorrhagic CRP patients with giant ulcers in the absence of standard treatments.
- Citation: Liu SY, Hu LL, Wang SJ, Liao ZL. Administration of modified Gegen Qinlian decoction for hemorrhagic chronic radiation proctitis: A case report and review of literature. World J Clin Cases 2023; 11(5): 1129-1136
- URL: https://www.wjgnet.com/2307-8960/full/v11/i5/1129.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i5.1129
In the case of pelvic cancer, radiation therapy is often used[1]. As a complication of radiation therapy, radiation proctitis frequently occurs. Acute radiation proctitis often occurs in the first 6 wk of radiation treatment; however, it usually subsides on its own. For chronic radiation proctitis (CRP), 5%-20% of patients with pelvic malignancies experience CRP after radiotherapy[2,3]. It can continue from the acute phase or occur after an asymptomatic period of 3 to 6 mo or even years after pelvic radiotherapy[4]. The most common symptoms of CRP are rectal bleeding, also called hemorrhagic CRP, due to neoang
Although the Clinical Practice Guidelines Committee of The American Society of Colon and Rectal Surgeons issued Clinical Practice Guidelines for the Treatment of CRP in 2018, there are currently no standard treatment for hemorrhagic CRP[9,10]. Current treatments for hemorrhagic CRP mainly include conventional medical therapies (e.g., anti-inflammatory medications, antioxidants, and formalin), endoscopic therapy, and surgery[3]. Due to their side effects and costs, as well as associated high recurrence rates, the above mentioned therapies are selected with caution[11]. In addition, accomp
CHMs have been widely applied to treat ulcerative colitis[11,12]. Increasing evidence has demonstrated that CHMs have potentially positive effects on the relief of intestinal inflammation. Some clinical trials explored the efficacy of CHMs for acute radiation proctitis following oral administration or enema[13,14], but no reports were found on CRP or hemorrhagic CRP in the clinical setting. Here, we report a hemorrhagic CRP patient with a giant ulcer treated using CHM by means of retention enema and oral administration.
A 51-year-old female patient first visited the Traditional Chinese Medicine Cancer Treatment Center in our hospital on September 13, 2021. She mainly complained of frequent diarrhea (5-6 times per day) and bloody purulent stools for over 10 d.
The patient presented mainly with frequent diarrhea (5-6 times a day), loose stool with blood and mucus accompanied by tenesmus and pain, and mild pain in the lower abdomen. We observed that her tongue was thin and red, with a thin, yellowish, and greasy coating. Her pulse was rapid and thready.
In her past medical history, she was diagnosed with cervical cancer and received intensity-modulated radiation therapy and brachytherapy with a total dose of 93 Gy 15 d after hysterectomy and bilateral adnexectomy from October 30, 2020, to November 23, 2020. Due to the presence of residual disease, she received six additional cycles of chemotherapy with carboplatin and paclitaxel on November 14, 21, and 28 and December 5, 12, and 19, 2020. Two-dimensional conventional radiotherapy was performed 5 times from December 4 to 30, 2020.
The patient had no significant personal or family history.
On admission, the patient’s temperature was 36.2 °C, heart rate was 86 bpm, respiratory rate was 18 breaths per minute, blood pressure was 108/65 mm Hg and body mass index was 20.5 kg/m2. The patient presented with a soft abdomen, and no mass was palpated. There was no tenderness in the abdomen and no rebound pain. Bowel sounds occurred 4 times/minute.
A routine fecal occult blood test yielded positive results. No abnormalities were found in tests for cytomegalovirus antibody, Clostridium difficile antigen, or coagulation function or in the tuberculous infection of T cell spot test (T-SPOT.TB) test for tuberculosis. The routine blood examination showed a minimum hemoglobin concentration of 121 g/L.
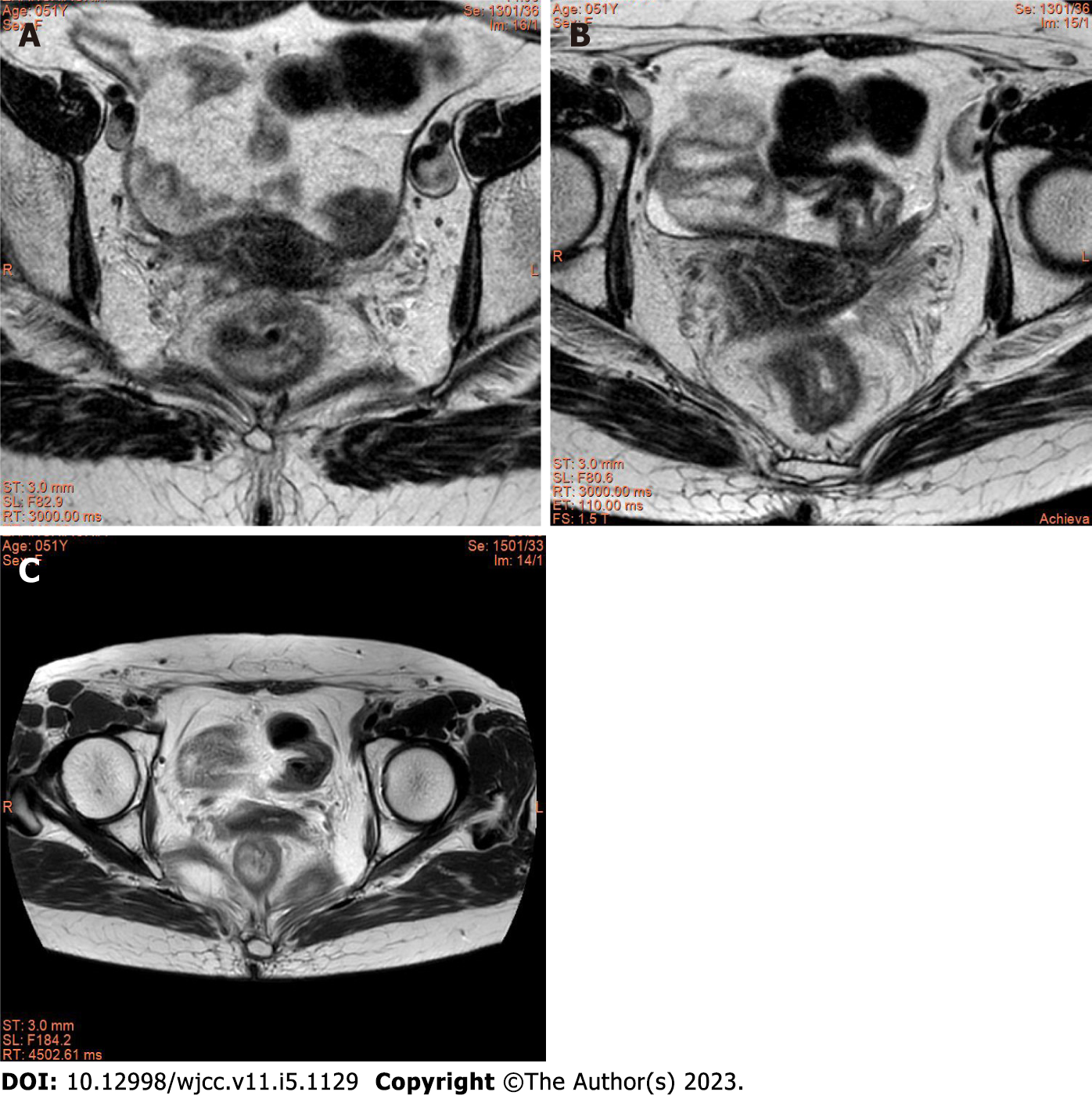
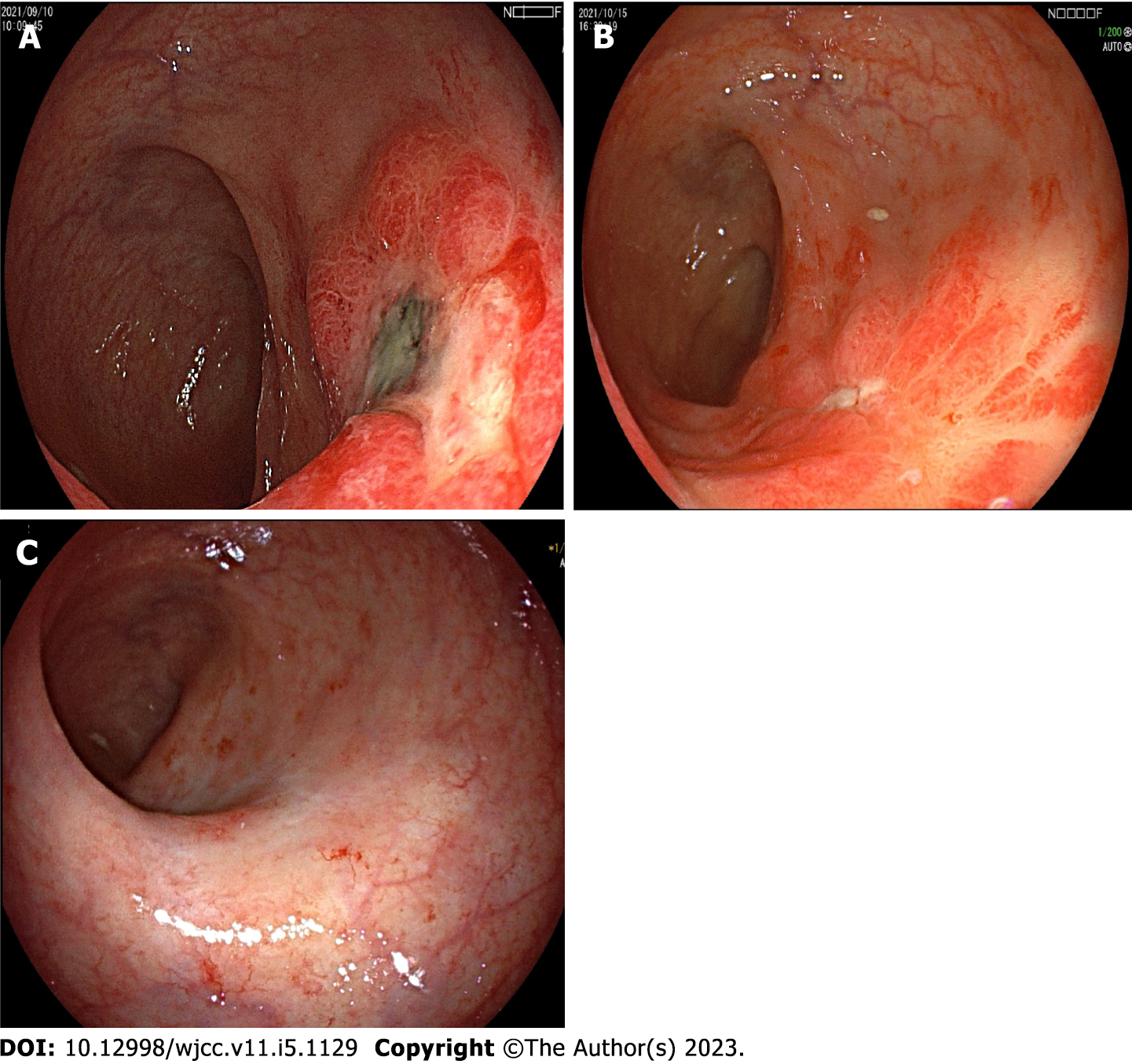
The magnetic resonance imaging (MRI) examination of the pelvic cavity showed no obvious tumor recurrence or metastasis. The walls of the rectum were significantly thickened and swollen, which was considered to have occurred after radiotherapy (Figure 1A). A colonoscopy was also performed and revealed a giant ulcer (ulceration area > 2.0 cm2) covered with necrotic tissue and patchy telangiectasias in the rectum (Figure 2A). The colonoscopy diagnosis was radiation proctitis. Biopsies also confirmed changes consistent with radiation-induced proctitis and ruled out malignant lesions.
Based on the above examination results and after the exclusion of diseases, the patient was diagnosed with hemorrhagic CRP. According to the toxicity grade of the Radiation Therapy Oncology Group and the European Organization for Research and Treatment of Cancer[15], the patient experienced grade 2 radiation proctitis. Regarding the specific Vienna rectoscopy score criteria[16], the patient had grade 3 congested mucosa, grade 3 telangiectasia, grade 3 ulcerations, no stricture, and no necrosis.
After performing a comprehensive assessment and obtaining the patient’s willingness, she underwent a conservative CHM regimen. A volume of 150 mL of modified Gegen Qinlian decoction (GQD) (Table 1) was used as a retention enema by injection into the rectum in the evening each day for 1 mo.
| Ingredients | Family | Batch number | Dose |
| Huangqin (Radix Scutellariae) | Labiatae | 220606 | 10 g |
| Huanglian (Rhizoma Coptidis) | Ranunculaceae | 21110106 | 10 g |
| Gegen (Radix Puerariae) | Fabaceae | 22050102 | 30 g |
| Baitouweng (Radix Pulsatillae) | Ranunculaceae | 22040102 | 15 g |
| Diyu (Radix Sanguisorbae, charred) | Rosaceae | 220304 | 10 g |
| Oujie (Nodus Nelumbinis Rhizomatis, charred) | Nymphaeaceae | 220221 | 10 g |
| Paojiang (Rhizoma Zingiberis, prepared) | Zingiberaceae | 200308 | 10 g |
| Huangqi (Radix Astragali) | Fabaceae | 220510 | 30 g |
| Egg yolk oil | NA | 20270314 | 6 mL |
One week after she received retention enema treatment, the frequency of her diarrhea reduced to 2-3 times a day. Her symptoms of rectal tenesmus gradually subsided. On follow-up colonoscopy 1 mo later, the rectal mucosal ulcer had healed, but patchy telangiectasias still existed (Figure 2B). However, due to the inconvenience of retention enema every day, the patient was thereafter prescribed oral administration of modified GQD instead of enema (Table 2). The decoction was administered at a dose of 150 mL each time, 3 times per day for 5 mo. On follow-up colonoscopy in April 2022, the rectal mucosal ulcer and patchy telangiectasias were almost healed, with an almost normal vascular pattern (Figure 2C). The MRI examination showed that the thickening and swelling of the intestinal wall were markedly improved (Figure 1B and C). The frequency of her diarrhea reduced to 1-2 times a day. Her symptoms of rectal tenesmus and signs of mild pain in her lower abdomen disappeared. Her tongue was thin and light red, with thin and white coating. Her pulse was thready and moderate. During the period of treatment, no adverse reactions were reported, such as liver or renal function injury. A timeline with relevant data from the treatment period is shown in Supplementary Table 1.
| Ingredients | Family | Batch number | Dose |
| Huangqin (Radix Scutellariae) | Labiatae | 220606 | 10 g |
| Huanglian (Rhizoma Coptidis) | Ranunculaceae | 21110106 | 10 g |
| Baitouweng (Radix Pulsatillae) | Ranunculaceae | 22040102 | 10 g |
| Diyu (Radix Sanguisorbae, charred) | Rosaceae | 220304 | 10 g |
| Oujie (Nodus Nelumbinis Rhizomatis, charred) | Nymphaeaceae | 220221 | 10 g |
| Paojiang (Rhizoma Zingiberis, prepared) | Zingiberaceae | 200308 | 10 g |
| Huangqi (Radix Astragali) | Fabaceae | 220510 | 30 g |
| Baizhu (Rhizoma Atractylodis Macrocephalae, prepared) | Asteraceae | 220207 | 10 g |
| Danggui (Radix Angelicae Sinensis) | Apiaceae | 22050201 | 10 g |
| Baishao (Radix Paeoniae Alba) | Ranunculaceae | 220401861 | 15 g |
| Dangshen (Radix Codonopsis) | Campanulaceae | 220301511 | 15 g |
| Egg yolk oil | NA | 20270314 | 6 mL |
Treatment of CRP mainly consists of medical treatment, interventional treatment, and surgical treatment[8]. Endoscopy with ablation remains the preferred interventional treatment for CRP. Among the available medical treatments, sucralfate enemas are the most popular option. Other medical treatments include antibiotics, 5-aminosalicylic acid derivatives, probiotics, antioxidants, short-chain fatty acids, formalin instillation, and hyperbaric oxygen therapy. Unfortunately, there are no large, multicenter, randomized clinical trials evaluating the treatment options for CRP. Currently, clinical data on available treatment strategies are mostly from case reports or small studies[10,17]. According to the severity of disease, medical therapies are often used for mild diarrhea, cramping, or bleeding; endoscopic therapy for rectal bleeding; and surgical therapy for more severe cases, such as refractory bleeding and pain, strictures leading to intestinal obstruction, extremely deep ulcer, and fistulas.
Sucralfate retention enemas have been reported to be effective in the treatment of hemorrhagic CRP[18,19]. Other enemas, such as aminosalicylate, steroid, and short-chain fatty acid enemas, have not been shown to yield a sustainable effect on hemorrhagic proctitis[20]. Formalin (formaldehyde 4%-10%) can chemically cauterize telangiectasias and ulcerations and is often considered the most effective topical treatment of hemorrhagic proctitis. However, because of its corrosive nature, local morbidity was not negligible, particularly with respect to anal incontinence[21].
Argon plasma coagulation (APC) plays the most important role in the endoscopic treatment of hemorrhagic CRP[22]. Similar to formalin, it may require more than one treatment course. The associated prognostic factors were endoscopic features prior to APC, including the presence of telangiectasias on more than 50% of the surface area and ulcerations greater than 1 cm2. Zhong et al[23] demonstrated that APC may be risky, with 13.3% of patients developing rectal fistulas. The only risk factor identified was an ulceration area greater than 1 cm2[23].
Our patient’s first colonoscopy showed a very deep ulcer (ulceration area > 2 cm2) covered with necrotic tissue and patchy telangiectasias in the rectum. Based on her endoscopic characteristics and chief complaints, we diagnosed her with qi deficiency and damp heat syndrome and prescribed her with the CHM formula. The CHM formula was modified from GQD, which is a traditional Chinese herbal formula used to treat acute enteritis, chronic diarrhea, and bacterial dysentery[24,25]. It has been reported that GQD can alleviate dextran sulfate sodium-induced ulcerative colitis by suppressing IL-6/JAK2/STAT3 signaling to restore Treg and Th17-cell homeostasis in colonic tissue[26].
Considering the presence of telangiectasias and ulceration, we added charcoal medicines, such as Diyu (Radix Sanguisorbae, charred), Oujie (Nodus Nelumbinis Rhizomatis, charred), and egg yolk oil, to control hemorrhagic proctitis. Charcoal medicines refer to a type of medicine carbonized under the guidance of traditional Chinese medicine theory with some unique clinical effects[27]. In ancient times, charcoal medicines were used for the clinical treatment of hemoptysis, hematemesis, and hemorrhage[28]. In recent years, researchers have found that carbon dots are the material basis for the activity of charcoal-processed drugs[29]. They may exert different effects on stanching bleeding by stimulating the extrinsic blood coagulation pathway, activating the fibrinogen system and mitigating inflammatory responses by reducing the serum concentrations of tumor necrosis factor-α, interleukin-6, and interleukin-1β in hemorrhagic or infectious diseases[30,31].
In the first month of treatment, modified GQD was used for retention enema. In the second stage of treatment, given the patient’s compliance, we changed our treatment strategy to using modified GQD as an oral administration, which was more convenient. Eventually, the patient achieved remarkable remission in both her clinical symptoms and imaging examinations. During the 3-mo follow-up visits, the patient felt well.
Modified GQD may be an effective, safe, and applicable approach to treat hemorrhagic CRP patients with giant ulcers. Further well-designed, high-quality clinical studies, such as randomized controlled trials, are needed to investigate the role of modified GQD in hemorrhagic CRP patients with giant ulcers.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Meng S, China S-Editor: Li L L-Editor: A P-Editor: Li L
| 1. | van de Wetering FT, Verleye L, Andreyev HJ, Maher J, Vlayen J, Pieters BR, van Tienhoven G, Scholten RJ. Non-surgical interventions for late rectal problems (proctopathy) of radiotherapy in people who have received radiotherapy to the pelvis. Cochrane Database Syst Rev. 2016;4:CD003455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Yuan ZX, Ma TH, Wang HM, Zhong QH, Yu XH, Qin QY, Wang JP, Wang L. Colostomy is a simple and effective procedure for severe chronic radiation proctitis. World J Gastroenterol. 2016;22:5598-5608. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 16] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Nelamangala Ramakrishnaiah VP, Krishnamachari S. Chronic haemorrhagic radiation proctitis: A review. World J Gastrointest Surg. 2016;8:483-491. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Hanson B, MacDonald R, Shaukat A. Endoscopic and medical therapy for chronic radiation proctopathy: a systematic review. Dis Colon Rectum. 2012;55:1081-1095. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Kuku S, Fragkos C, McCormack M, Forbes A. Radiation-induced bowel injury: the impact of radiotherapy on survivorship after treatment for gynaecological cancers. Br J Cancer. 2013;109:1504-1512. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 60] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 6. | Krol R, Smeenk RJ, van Lin EN, Yeoh EE, Hopman WP. Systematic review: anal and rectal changes after radiotherapy for prostate cancer. Int J Colorectal Dis. 2014;29:273-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 7. | Wu C, Guan L, Yao L, Huang J. Mesalazine suppository for the treatment of refractory ulcerative chronic radiation proctitis. Exp Ther Med. 2018;16:2319-2324. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Vanneste BG, Van De Voorde L, de Ridder RJ, Van Limbergen EJ, Lambin P, van Lin EN. Chronic radiation proctitis: tricks to prevent and treat. Int J Colorectal Dis. 2015;30:1293-1303. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 78] [Cited by in RCA: 77] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 9. | Paquette IM, Vogel JD, Abbas MA, Feingold DL, Steele SR; Clinical Practice Guidelines Committee of The American Society of Colon and Rectal Surgeons. The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Treatment of Chronic Radiation Proctitis. Dis Colon Rectum. 2018;61:1135-1140. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 57] [Article Influence: 8.1] [Reference Citation Analysis (0)] |
| 10. | Mahmood S, Bollipo S, Steele S, Bristow RG, Choudhury A, Oakland K, Martin J. It's All the RAVE: Time to Give up on the "Chronic Radiation Proctitis" Misnomer. Gastroenterology. 2021;160:635-638. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 11. | Zhang C, Jiang M, Lu A. Considerations of traditional Chinese medicine as adjunct therapy in the management of ulcerative colitis. Clin Rev Allergy Immunol. 2013;44:274-283. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 12. | Zhang X, Zhang L, Chan JCP, Wang X, Zhao C, Xu Y, Xiong W, Chung WC, Liang F, Miao J, Bian Z. Chinese herbal medicines in the treatment of ulcerative colitis: a review. Chin Med. 2022;17:43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 28] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 13. | Wang L, Zhang ZZ, Tu XH, Zou ZD, Liu JH, Wang Y. Safety and efficacy of Qingre Buyi Decoction in the treatment of acute radiation proctitis: a prospective, randomized and controlled trial. Chin J Integr Med. 2009;15:272-278. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Tang Y, Huang Y, Mo X, Yi G, Wen H, Guo Z, Feng K, Liu Y, Bu Q, JiAng W. Efficacy and safety of Yunxiangjing derived from Chinese herbal medicine administered as an enema in the management of acute radiation-induced proctitis in patients with pelvic malignancy. J Tradit Chin Med. 2016;36:45-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Herrmann T, Knorr A, Dörner K. [The RTOG/EORTC classification criteria for early and late radiation reactions]. Radiobiol Radiother (Berl). 1987;28:519-528. [PubMed] |
| 16. | Lee J, Han HJ, Min BS, Hong SP, Shin SJ, Yoon HI, Park SJ, Koom WS. The role of endoscopic evaluation for radiation proctitis in patients receiving intermediate-dose postoperative radiotherapy for rectal cancer. Jpn J Clin Oncol. 2018;48:988-994. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Dahiya DS, Kichloo A, Tuma F, Albosta M, Wani F. Radiation Proctitis and Management Strategies. Clin Endosc. 2022;55:22-32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 18. | Kochhar R, Patel F, Dhar A, Sharma SC, Ayyagari S, Aggarwal R, Goenka MK, Gupta BD, Mehta SK. Radiation-induced proctosigmoiditis. Prospective, randomized, double-blind controlled trial of oral sulfasalazine plus rectal steroids versus rectal sucralfate. Dig Dis Sci. 1991;36:103-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 177] [Cited by in RCA: 156] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 19. | Gul YA, Prasannan S, Jabar FM, Shaker AR, Moissinac K. Pharmacotherapy for chronic hemorrhagic radiation proctitis. World J Surg. 2002;26:1499-1502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 20. | Denton AS, Andreyev HJ, Forbes A, Maher EJ. Systematic review for non-surgical interventions for the management of late radiation proctitis. Br J Cancer. 2002;87:134-143. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 107] [Cited by in RCA: 98] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 21. | de Parades V, Etienney I, Bauer P, Bourguignon J, Meary N, Mory B, Sultan S, Taouk M, Thomas C, Atienza P. Formalin application in the treatment of chronic radiation-induced hemorrhagic proctitis--an effective but not risk-free procedure: a prospective study of 33 patients. Dis Colon Rectum. 2005;48:1535-1541. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 68] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 22. | Weiner JP, Wong AT, Schwartz D, Martinez M, Aytaman A, Schreiber D. Endoscopic and non-endoscopic approaches for the management of radiation-induced rectal bleeding. World J Gastroenterol. 2016;22:6972-6986. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 34] [Cited by in RCA: 28] [Article Influence: 3.1] [Reference Citation Analysis (1)] |
| 23. | Zhong QH, Liu ZZ, Yuan ZX, Ma TH, Huang XY, Wang HM, Chen DC, Wang JP, Wang L. Efficacy and complications of argon plasma coagulation for hemorrhagic chronic radiation proctitis. World J Gastroenterol. 2019;25:1618-1627. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 24. | Liu X, Fan Y, Du L, Mei Z, Fu Y. In Silico and In Vivo Studies on the Mechanisms of Chinese Medicine Formula (Gegen Qinlian Decoction) in the Treatment of Ulcerative Colitis. Front Pharmacol. 2021;12:665102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 25. | Lu JZ, Ye D, Ma BL. Constituents, Pharmacokinetics, and Pharmacology of Gegen-Qinlian Decoction. Front Pharmacol. 2021;12:668418. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 40] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 26. | Zhao Y, Luan H, Jiang H, Xu Y, Wu X, Zhang Y, Li R. Gegen Qinlian decoction relieved DSS-induced ulcerative colitis in mice by modulating Th17/Treg cell homeostasis via suppressing IL-6/JAK2/STAT3 signaling. Phytomedicine. 2021;84:153519. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 94] [Article Influence: 23.5] [Reference Citation Analysis (0)] |
| 27. | Gao M, Lan J, Bao B, Yao W, Cao Y, Shan M, Cheng F, Chen P, Zhang L. Effects of carbonized process on quality control, chemical composition and pharmacology of Typhae Pollen: A review. J Ethnopharmacol. 2021;270:113774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 19] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 28. | Chen Z, Ye SY, Yang Y, Li ZY. A review on charred traditional Chinese herbs: carbonization to yield a haemostatic effect. Pharm Biol. 2019;57:498-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 29. | Zhao Y, Zhang Y, Liu X, Kong H, Wang Y, Qin G, Cao P, Song X, Yan X, Wang Q, Qu H. Novel carbon quantum dots from egg yolk oil and their haemostatic effects. Sci Rep. 2017;7:4452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 35] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 30. | Luo J, Zhang M, Cheng J, Wu S, Xiong W, Kong H, Zhao Y, Qu H. Hemostatic effect of novel carbon dots derived from Cirsium setosum Carbonisata. RSC Adv. 2018;8:37707-37714. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 31. | Wu J, Zhang M, Cheng J, Zhang Y, Luo J, Liu Y, Kong H, Qu H, Zhao Y. Effect of Lonicerae japonicae Flos Carbonisata-Derived Carbon Dots on Rat Models of Fever and Hypothermia Induced by Lipopolysaccharide. Int J Nanomedicine. 2020;15:4139-4149. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |