Published online Dec 26, 2023. doi: 10.12998/wjcc.v11.i36.8568
Peer-review started: October 16, 2023
First decision: November 21, 2023
Revised: November 24, 2023
Accepted: December 13, 2023
Article in press: December 13, 2023
Published online: December 26, 2023
Processing time: 67 Days and 0 Hours
Heterotopic ossification (HO) represents all types of extraskeletal ossification in the body. It occurs in various areas, including the skin, subcutaneous tissue, muscle, and joints. Surgical excision is recommended for symptomatic HO. Postoperative radiotherapy, oral nonsteroidal anti-inflammatory drugs, and topical sealants, such as bone wax, have been recommended as preventive measures. As HO is rare in occurrence, these recommendations are based on personal experiences, and there is a lack of information on individualized treatments depending on its location.
A 62-year-old male was admitted for symptomatic HO along a laparotomy scar. Surgical excision was performed for an 11 cm-sized ossification originating from the xiphoid process, and bone wax was applied to the excisional margin. However, the surgical wound failed to heal. After several weeks of saline-soaked gauze dressing, delayed wound closure was performed. The patient was finally discharged eight weeks after the excision. Because HO can occur in various areas of the body, a treatment strategy that may be effective for some may not be for others. Bone wax has been used as a topical sealant over excisional margins in the shoulder, elbow, and temporomandibular joints. However, in our case, its application on an abdominal surgical wound delayed its primary healing intention. The valuable lesson was that, when choosing a treatment method for HO based on available research data, its location must be considered.
Complete excision should be the priority treatment option for symptomatic HO along the laparotomy scar. Bone wax application is not recommended.
Core Tip: Heterotopic ossification (HO) represents all types of extraskeletal ossification, and occurs in various areas, including the skin, muscle, and joints. There are some suggested treatment and preventive approaches for symptomatic HO, which include surgical excision and preventive measures such as postoperative radiotherapy, oral nonsteroidal anti-inflammatory drugs, and topical sealants (bone wax). However, these recommendations are based on personal experiences limited to HO in certain locations. It is important to individualize our treatment approaches depending on its location. For symptomatic HO along the laparotomy scar, complete surgical excision should be the priority treatment option, and bone wax application is not recommended.
- Citation: Lee SS. Post-laparotomy heterotopic ossification of the xiphoid process: A case report. World J Clin Cases 2023; 11(36): 8568-8573
- URL: https://www.wjgnet.com/2307-8960/full/v11/i36/8568.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i36.8568
Heterotopic ossification (HO) refers to the formation of trabecular bone outside the usual skeletal system[1,2]. Therefore, all extraskeletal bone formation in various areas of the body, including the skin, subcutaneous tissue, muscle, joints, and mesentery are included in this uncommon clinical entity[3,4]. As much as it covers all extraskeletal bone formation throughout the body, a wide range of factors contribute to each occurrence. Some of the most mentioned associated factors are trauma, burns, arthroplasty, and abdominal surgery[1,5]. As HO is highly associated with an external insult, the concern is higher in military settings where a high incidence of HO in combat-injured patients has been reported[2].
HO has been reported in various sites of the human body, and some hypotheses have been presented for its pathogenesis[6]. The generally recommended treatment for symptomatic HO has been selective surgical excision[2,7]. Some cases have been treated with open resection[8,9], and others, especially cases of HO in the joints, have been treated with arthroscopy[1]. Regardless of the HO site, recurrence has always been a concern for surgeons, and some preventive measures, such as postoperative radiotherapy[10], oral nonsteroidal anti-inflammatory drugs (NSAIDs)[11], and topical sealant (bone wax) over the osteotomy plane[1,7,12], have been recommended.
We experienced a case of symptomatic HO along a laparotomy scar following gastrectomy for gastric cancer. To search for the best treatment options, we vigorously reviewed the previous reports that were available at the time. While realizing that HO is a collective term representing all types of extraskeletal ossifications, we found a lack of information stating the need for individualizing our treatment efforts depending on the HO location. Our choice of treatment, which was a combination of surgical excision and the application of bone wax, did not turn out to be the best option.
A 62-year-old Asian man complained of persistent difficulties in bending his waist forward for six months.
The patient underwent a curative surgery for gastric cancer about a year earlier and had been making routine visits to our outpatient department for regular surveillance. After the gastrectomy, he continued to display a tendency toward excessive anxiety about his health. He kept complaining about memory loss, hair loss, and constipation, which were somewhat different from the usual postgastrectomy complaints, such as diarrhea, nausea, vomiting, and other gastrointestinal symptoms. Four months after the gastrectomy, he started complaining of stiffness along the surgical scar but received little medical attention at the time. The symptoms worsened over the next two months, and the patient started experiencing difficulties in bending his waist forward. The patient had a normal weight (62.7 kg) and body mass index (20.9 kg/m2). Postgastrectomy weight loss was minimal (weight loss of 1.3 kg). There were no signs of cancer recurrence.
The patient underwent distal subtotal gastrectomy, D2 lymphadenectomy, and Billroth II anastomosis for gastric cancer a year earlier. He did not undergo adjuvant chemotherapy as the surgical specimen confirmed stage I cancer according to the 8th edition of the Union for International Cancer Control classification. The patient had no history of smoking, alcohol abuse, or previous illnesses except for well-controlled hypertension and type 2 diabetes.
The patient had no significant personal or family history.
The vital signs were unremarkable. Abdominal physical examination revealed no distension or rigidity. Bowel sound was normal. There was a firm, fixed palpable mass along the surgical incision that was about 10 cm in size. There was no pain or tenderness.
Routine blood and urine analysis results were normal. Serum tumor markers including carcinoembryonic antigen and carbohydrate antigen 19-9 were normal with 3.4 ng/mL and 21.4 U/mL, respectively.
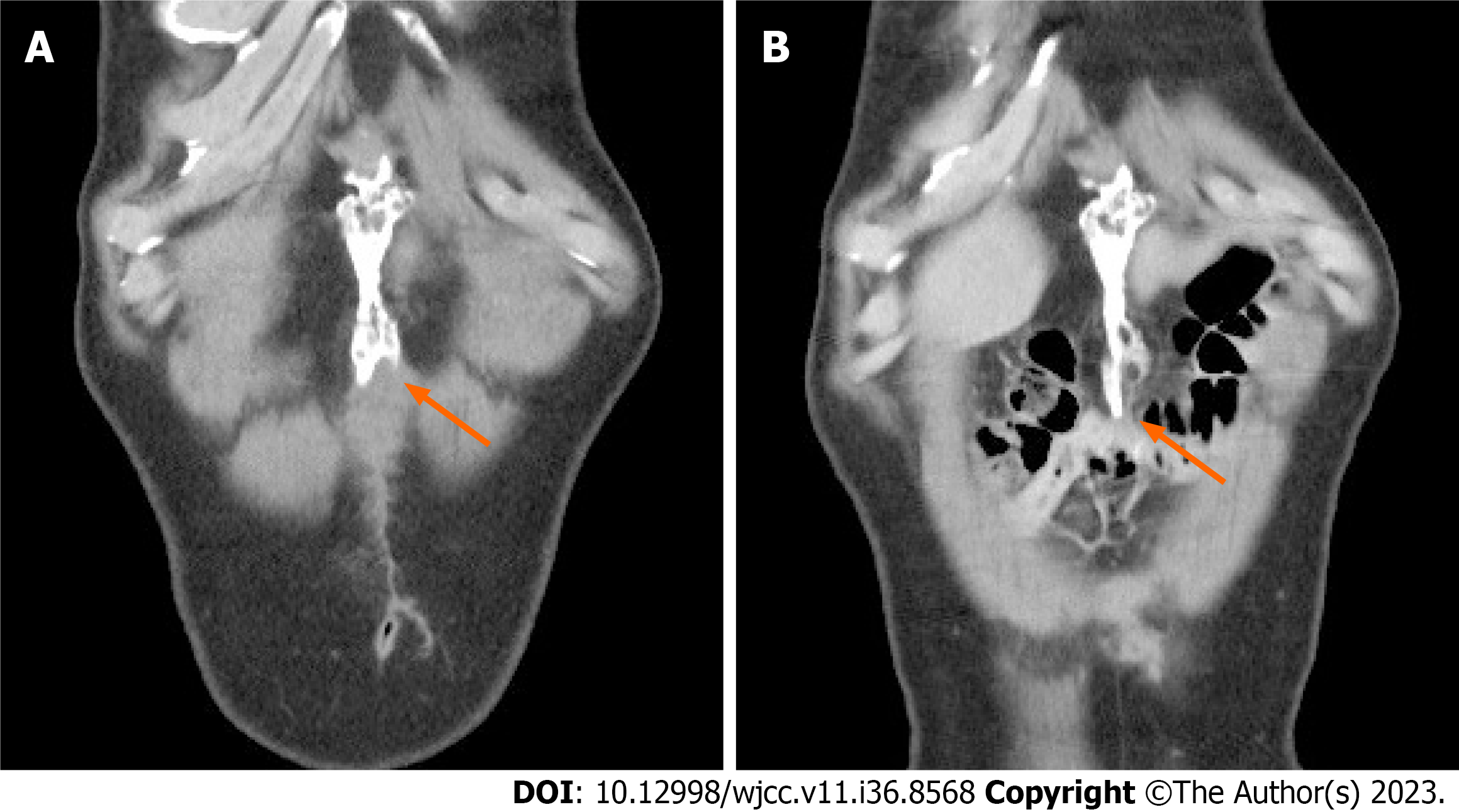
An abdominal computerized tomography (CT), taken for 6-mo postgastrectomy surveillance, revealed a 10 cm-sized ossification along the surgical incision (Figure 1). The latest CT, taken for 1-year postgastrectomy surveillance just before the admission, confirmed an 11 cm-sized ossification along the surgical incision.
Based on the patient’s medical history, physical examination, and CT findings, the final diagnosis was HO, originating from the xiphoid process.
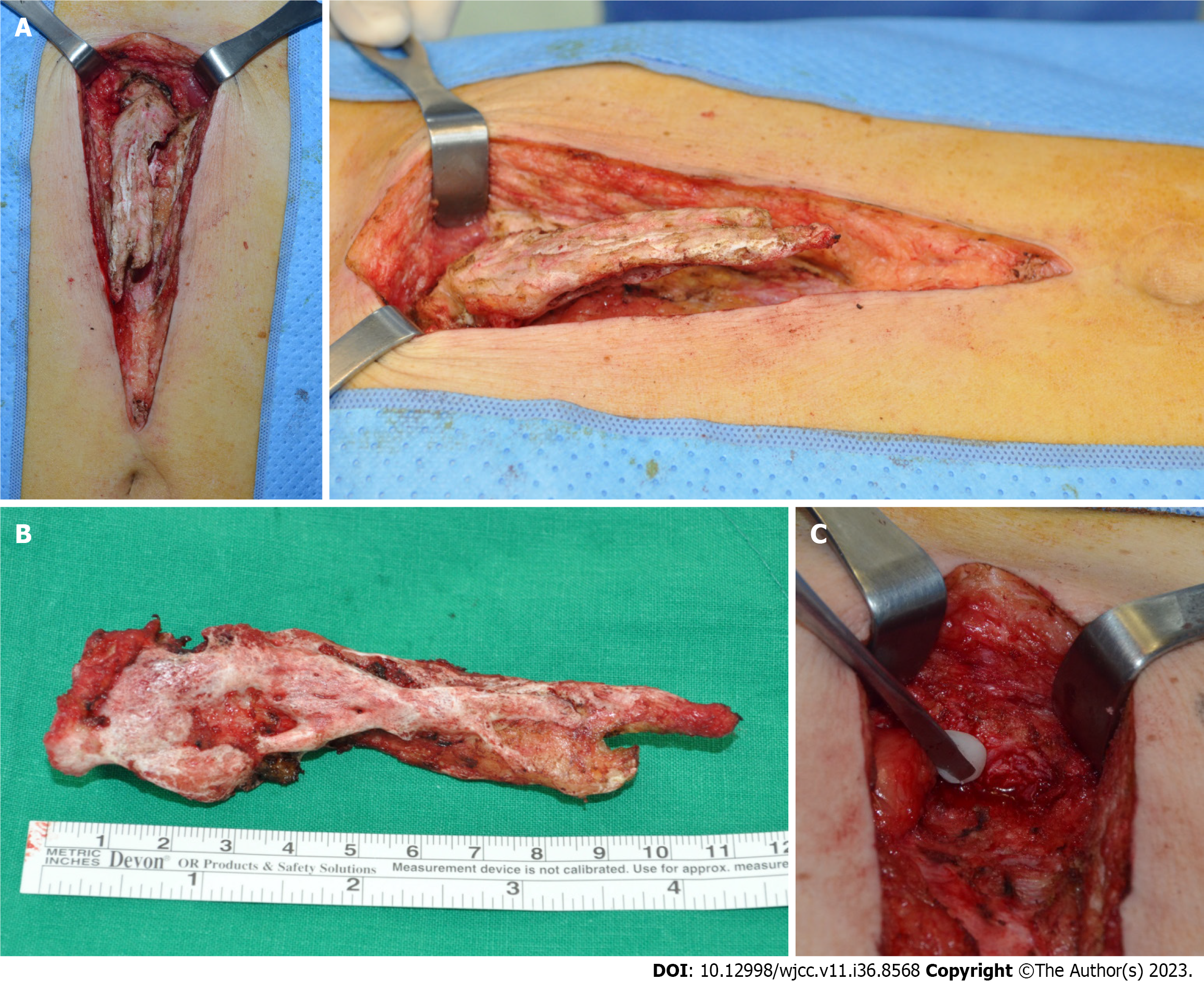
Surgery for symptomatic HO was performed under general anesthesia. At laparotomy, an 11 cm-sized ossification, originating from the xiphoid process, was noticed between the linea alba and preperitoneal adipose layer (Figure 2). The structure was densely adhered to the surrounding tissue. After careful dissection of the adhered tissue and separation of the bony attachment at the xiphoidal end, we completely removed the structure. As an extra precaution for bone hemostasis and HO recurrence, bone wax was applied to the excisional margin. The surgical wound was closed layer by layer.
Histological examination of the surgical specimen confirmed HO. However, there was extensive discharge from the surgical wound over the following two weeks. The nature of the discharge slowly changed from serous to turbid, and we decided to open the surgical wound. The wound was somewhat waxy, and massive wound irrigation was performed. After three weeks of applying saline-soaked gauze dressings, delayed wound closure was performed, and the patient was finally discharged eight weeks after the HO excision. He underwent a follow-up CT two years postgastrectomy, which was about a year after the HO excision, and there were no signs of recurrence (Figure 3).
HO is rare and, yet, broad in that it represents all types of extraskeletal ossifications in the body. Therefore, depending on its location, a treatment strategy that may be effective for some may not be for others. An extensive literature search led us to the application of bone wax along the laparotomy scar following surgical HO excision. However, this turned out to be a grave misapplication of our treatment efforts.
Two pathogenesis hypotheses for the HO of abdominal scar tissue have been suggested[6]. The first and more favored hypothesis is an aberrant inflammatory process in wound healing, leading to the differentiation of mesenchymal stromal cells into osteoblasts. This is highly favored in those with HO located at a distance from the adjacent bone. The second hypothesis emphasizes the iatrogenic spillage of periosteal cells from the adjacent bone during surgery. In our case, HO was connected with the xiphoid process, and we could not exclude the possibility of the iatrogenic spillage of periosteal cells from the xiphoid process.
Whatever the pathogenesis hypothesis, surgical excision has been recommended for symptomatic HO. Our literature search delved deeper into HO prevention. The search returned some recommendations for preventing HO recurrence, and bone wax was one of them. Bone wax is a nonabsorbable substance composed of beeswax and petroleum jelly, and has been used to achieve hemostasis after bone resection[13]. While it functions as a mechanical barrier to stop bleeding, using it to suppress bone formation in the resection surface has also been reported[14]. Despite concerns about a chronic inflammatory reaction following the intraarticular use of bone wax[15], bone wax has been used as a topical sealant to prevent HO in shoulders[1], temporomandibular joints[7], and elbows[12].
Besides bone wax, postoperative radiotherapy and oral NSAIDs have been recommended as feasible preventive measures for HO[10,11]. However, we chose none of these because they are highly associated with gastrointestinal symptoms[16,17]. Gastric cancer survivors are known to experience gastrointestinal symptoms for years after surgery[18]. Our patient underwent distal subtotal gastrectomy a year earlier and was not free of gastrointestinal symptoms. Therefore, the clinical application of either radiotherapy or oral NSAIDs would have exacerbated postgastrectomy symptoms.
After much deliberation, we decided to use bone wax. Unfortunately, the outcome was an eight-week-long hospital stay and additional surgery for delayed wound closure. The application of bone wax on the abdominal surgical wound delayed its primary healing intention. A previous study reported the clinical use of bone wax in dermatologic surgery by exploiting such a distinguishing trait[19]. Bone wax has been used to cover deep tissue defects and create an ideal occlusive environment for secondary healing intention. In our case, our efforts to prevent HO recurrence left the surgical wound in a condition that was suitable only for secondary healing intention.
Complete excision may be a sufficient management strategy for HO along a laparotomy scar. We eventually made huge efforts to remove the bone wax as much as possible by massive wound irrigation and repeated cleansing with wet gauze, and there was no sign of recurrence after a year. Nevertheless, uncertainty regarding the remaining bone wax and its implication on HO prevention is a limitation of this finding. The strength would be sharing the valuable lesson that we need to be very careful about choosing a treatment method for HO using available research data and treatment should be individualized depending on the HO location. Previous reports suggesting the beneficial effect of bone wax against HO recurrence have focused on HO in joints[1,7,12]. Our effort of applying bone wax to an abdominal wound could have failed because we did not realize the distinction in treatment between different areas.
In conclusion, HO represents all types of extraskeletal ossifications in the body, and treatment approaches must be individualized depending on the surroundings. Complete surgical excision should be the priority treatment option for HO along a laparotomy scar, and the application of bone wax is not recommended.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Augustin G, Croatia S-Editor: Wang JJ L-Editor: A P-Editor: Zhao S
| 1. | Hallock J, Field LD. Surgical Management of Shoulder Heterotopic Ossification. Arthrosc Tech. 2019;8:e1057-e1062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Edwards DS, Kuhn KM, Potter BK, Forsberg JA. Heterotopic Ossification: A Review of Current Understanding, Treatment, and Future. J Orthop Trauma. 2016;30 Suppl 3:S27-S30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 3. | Hogan NM, Caffrey E, Curran S, Sheehan M, Joyce MR. Heterotopic ossification of the abdominal wall. Int J Surg Case Rep. 2012;3:489-491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Hakim M, McCarthy EF. Heterotopic mesenteric ossification. AJR Am J Roentgenol. 2001;176:260-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Brady RD, Shultz SR, McDonald SJ, O'Brien TJ. Neurological heterotopic ossification: Current understanding and future directions. Bone. 2018;109:35-42. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 55] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 6. | Fennema EM, de Boer J, Mastboom WJ. Ossification of abdominal scar tissue: a case series with a translational review on its development. Hernia. 2014;18:825-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Ding R, Lu C, Zhao J, He D. Heterotopic ossification after alloplastic temporomandibular joint replacement: a case cohort study. BMC Musculoskelet Disord. 2022;23:638. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 8. | Hong SP, Lee JB, Bae CH. Heterotopic Ossification of the Xiphoid Process after Abdominal Surgery for Traumatic Hemoperitoneum. J Korean Med Sci. 2018;33:e62. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Tytherleigh-Strong G, Gill J, Sforza G, Copeland S, Levy O. Reossification and fusion across the acromioclavicular joint after arthroscopic acromioplasty and distal clavicle resection. Arthroscopy. 2001;17:E36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Jensen AW, Viozzi CF, Foote RL. Long-term results of radiation prophylaxis for heterotopic ossification in the temporomandibular joint. J Oral Maxillofac Surg. 2010;68:1100-1105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 11. | Naylor BH, Iturriaga CR, Bisen YB, Caid MJ, Reinhardt KR. Heterotopic Ossification Following Direct Anterior Total Hip Arthroplasty With and Without Postoperative Analgesic Nonsteroidal Anti-inflammatories. J Arthroplasty. 2021;36:3471-3477. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Kamineni S, Maritz NG, Morrey BF. Proximal radial resection for posttraumatic radioulnar synostosis: a new technique to improve forearm rotation. J Bone Joint Surg Am. 2002;84:745-751. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 38] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Schonauer C, Tessitore E, Barbagallo G, Albanese V, Moraci A. The use of local agents: bone wax, gelatin, collagen, oxidized cellulose. Eur Spine J. 2004;13 Suppl 1:S89-S96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 235] [Cited by in RCA: 203] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 14. | Krueger A, Leunig M, Siebenrock KA, Beck M. Hip arthroscopy after previous surgical hip dislocation for femoroacetabular impingement. Arthroscopy. 2007;23:1285-1289.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 38] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 15. | Solomon LB, Guevara C, Büchler L, Howie DW, Byard RW, Beck M. Does bone wax induce a chronic inflammatory articular reaction? Clin Orthop Relat Res. 2012;470:3207-3212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Dennis K, Poon M, Chow E. Nausea and vomiting induced by gastrointestinal radiation therapy: current status and future directions. Curr Opin Support Palliat Care. 2015;9:182-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 17. | Koch M, Dezi A, Ferrario F, Capurso I. Prevention of nonsteroidal anti-inflammatory drug-induced gastrointestinal mucosal injury. A meta-analysis of randomized controlled clinical trials. Arch Intern Med. 1996;156:2321-2332. [PubMed] |
| 18. | Samrat R, Naimish M, Samiran N. Post-Gastrectomy Complications - An Overview. Chirurgia (Bucur). 2020;115:423-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Alegre M, Garcés JR, Puig L. Bone wax in dermatologic surgery. Actas Dermosifiliogr. 2013;104:299-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |