Published online Dec 26, 2023. doi: 10.12998/wjcc.v11.i36.8563
Peer-review started: October 16, 2023
First decision: November 1, 2023
Revised: November 11, 2023
Accepted: December 12, 2023
Article in press: December 12, 2023
Published online: December 26, 2023
Processing time: 67 Days and 5.3 Hours
Colonoscopy is widely used for examination, diagnosis, and treatment because of its low incidence of associated complications. Post-colonoscopy appendicitis (PCA) is very rare and is easily misdiagnosed as electrocoagulation syndrome or colon perforation. Therefore, clinicians should pay close attention to this complication.
A 47-year-old female patient underwent a colonoscopy for a systematic physical examination, and the procedure was uneventful with normal endoscopic and histologic findings. However, the bowel preparation was suboptimal (Boston 2-3-2). After the examination, the patient experienced pain in the lower abdomen, which progressively worsened. Computed tomography of the lower abdomen and pelvis revealed appendiceal calcular obstruction and appendicitis. As the patient refused surgery, she was managed with antibiotics and recovered well.
In the current literature, the definition of PCA remains unclear. However, abdominal pain after colonoscopy should be differentiated from acute appen
Core Tip: Abdominal pain is a common symptom after colonoscopy and is generally considered to be caused by perforation or electrocoagulation syndrome. Acute appendicitis is often ignored as a differential diagnosis. This case report aims to improve clinicians’ awareness of possible appendicitis after colonoscopy. The causal relationship between colonoscopy and acute appendicitis remains unclear. However, regardless of whether it is defined as a complication, it should be differentiated from colonoscopy-associated abdominal pain, particularly in the right lower abdomen.
- Citation: Song XL, Ma JY, Zhang ZG. Colonoscopy-induced acute appendicitis: A case report. World J Clin Cases 2023; 11(36): 8563-8567
- URL: https://www.wjgnet.com/2307-8960/full/v11/i36/8563.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i36.8563
Colonoscopy is a common clinical examination, involving an endoscopic analysis of the entire colon, which aids in diagnosis and treatment. Colonoscopy is widely used because of its safety. However, although rare, serious complications, such as pain, bleeding, inflammation, perforation, cardiopulmonary complications, and death, can occur after colonoscopy.
Abdominal pain is a common symptom of colonoscopy. Mild abdominal pain is considered normal, and acute appendicitis, a relatively rare condition, is often ignored as a possible cause. Indeed, a previous study reported that the incidence of acute appendicitis after colonoscopy was approximately 0.038%[1]. However, considering that non-specific abdominal pain symptoms and minor appendicitis are easily overlooked, the recorded incidence of acute appendicitis may have been underestimated.
The number of patients undergoing colonoscopy have recently been increasing, and more cases of appendicitis after colonoscopy have consequently been reported. Since the first reported case in 1988, over 50 cases have been reported in the literature[2,3]. Many cases of perforation or gangrene, for which surgery is the primary treatment, have been reported[4-7]. Herein, we report the case of a woman who developed non-perforated appendicitis 10 h after colonoscopy and was treated with antibiotics immediately after a definitive diagnosis. This treatment yielded satisfactory results. This article aims to attract clinical attention to appendicitis after colonoscopy. Early identification and timely treatment are of paramount importance to avoid serious consequences and improve prognosis.
The patient complained of abdominal pain after undergoing colonoscopy. Appendicitis was diagnosed 10 h later.
The patient underwent a colonoscopy for health management, and the procedure was uneventful without any pathological biopsy. However, the state of intestinal cleanliness was poor (Boston 2-3-2), and clumps were observed in the feces. Ten hours after the examination, the patient experienced progressive pain in the right lower abdomen and was admitted to the gastroenterology department.
The patient’s past medical history was unremarkable.
The patient denied any possibility of family history-related conditions.
Body temperature was 37.6 °C, blood pressure was 132/75 mmHg, and heart rate was 85 beats/min. Tenderness of the right lower abdomen was evident without total abdominal pain [Murphy (-), Mc (+)].
The white blood cell count, neutrophil count, and C-reactive protein level were 9.54 × 109 cells/L, 11.8 × 109 cells/L (N%: 90.4%), and 25.3 mg/L, respectively.
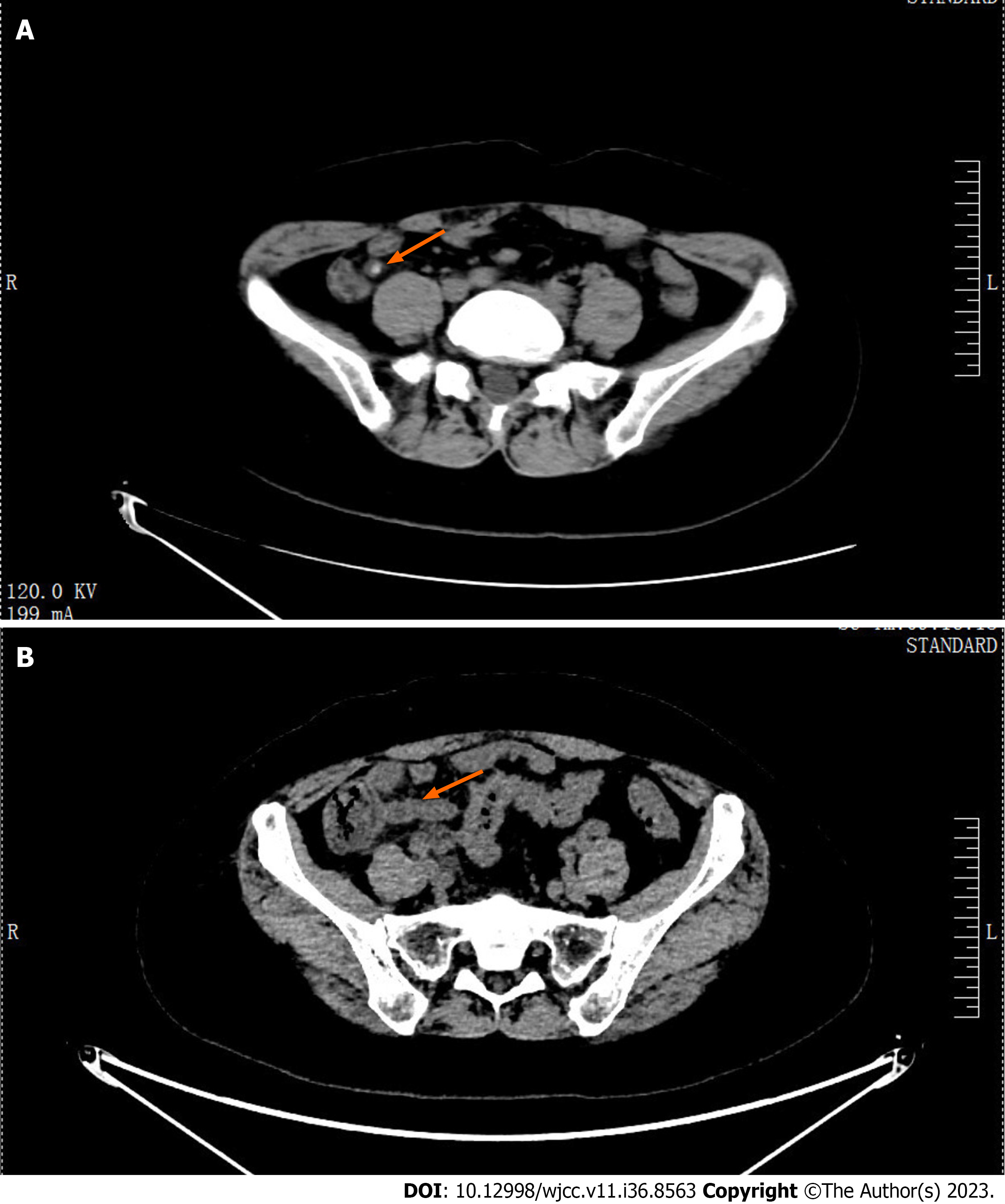
A computed tomography (CT) scan of the lower abdomen and pelvis revealed a dilated and inflamed appendix with fecoliths (Figure 1A).
Post-colonoscopy acute appendicitis.
The patient refused surgery and was administered antibiotics. After 3 d of treatment, the pelvic CT revealed inflammation in the appendix, and the appendicolith had disappeared (Figure 1B). Five days later, the patient was discharged in good physical condition.
The patient was followed up for 1 year and no symptoms of appendicitis recurred.
Colonoscopy is widely used to examine, diagnose, and treat intestinal diseases. It is associated with rare serious complications, of which bleeding and perforation are the most common. The incidence rate of complications ranges from 0.2% to 3%[8-10]. In recent years, more rare complications have been reported, including splenic and mesenteric vein embolisms. Post-colonoscopy appendicitis (PCA) is a rare complication.
Further, some scholars believe that PCA is a coincidence rather than a complication. Since the first reported case of PCA in 1988, the number of similar cases has increased over the past 20 years; to date, over 50 similar cases have been reported[2,3]. Interestingly, the number of cases reported in the past decade has increased fourfold compared to the previous decade[2], suggesting that this complication has gained increasing awareness among physicians.
Currently, no consensus on the definition, pathogenic factors, or pathogenesis of PCA have been established. Shaw et al[11] proposed that PCA should be defined as appendicitis occurring within 72 h of colonoscopy. Currently, there are several hypotheses regarding the pathogenesis of PCA: (1) Air pressure trauma caused by over-inflation[9]; (2) Obstruction and/or inflammation caused by stool pressing on the appendix[12]; (3) Direct trauma caused by unintentional intubation of the appendix tube[13]; (4) Exacerbation of existing subclinical diseases[14]; and (5) Stimulation of residual glutaraldehyde in the endoscope on the mucosa[13].
In the present case, appendicitis may not have been caused by a single factor. Owing to the impact of intestinal air pressure, fecal calculus in the intestinal cavity rushes into the appendix. Meanwhile, rising airway pressure makes it difficult for the airway to roll out, thereby causing appendicitis. In this case, this assumption was based on the fact that the patient’s intestinal cleanliness was unremarkable.
The diagnosis of PCA presents certain challenges, particularly because its initial clinical manifestations are generally nonspecific. Therefore, misdiagnosis of intestinal perforation or polypectomy syndrome is common. In the early stages of the disease, changes in biochemical examination results are not evident. However, CT can exclude lesions in other organs and intestinal perforations very early. CT scanning has high sensitivity and specificity for detecting acute appendicitis[15]. Plain abdominal film and ultrasound examinations may not be significantly useful in the early diagnosis and treatment of this disease[16-21]. Therefore, CT has become the primary diagnostic modality for PCA in clinical settings. The duration of PCA from symptom onset to diagnosis varied from several hours to 10 d. A recent study demonstrated that patients undergoing colonoscopy are prone to developing appendicitis within a week[22]. Therefore, patients experiencing abdominal pain after an examination should be cautious and skeptical of their diagnosis.
Based on previous treatment of PCA, laparoscopy is the first treatment choice. Over the past 15 years, the success rate of laparoscopy has reached approximately 89.5%[3]. However, when complicated with extensive peritonitis, open surgery remains a more safe, rapid, and effective treatment modality[23,24]. However, in recent years, nonsurgical treatments have received increasing attention. Furthermore, owing to an improved understanding of PCA, this disease can now commonly be diagnosed at an early stage. Non-surgical treatment is feasible for appendicitis without perforation, gangrene, or suppuration[3].
Although PCA is rare, the number of reported cases has increased in recent years. Owing to its nonspecific clinical symptoms and the fact that some mild inflammatory reactions may independently subside, the actual incidence of this disease may be underestimated. However, PCA should be considered in the differential diagnosis of patients with abdominal pain after colonoscopy, especially when intestinal cleanliness is poor.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Day AS, New Zealand S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Zhang XD
| 1. | Chae HS, Jeon SY, Nam WS, Kim HK, Kim JS, An CH. Acute appendicitis caused by colonoscopy. Korean J Intern Med. 2007;22:308-311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Ng ZQ, Elsabagh A, Wijesuriya R. Post-colonoscopy appendicitis: Systematic review of current evidence. J Gastroenterol Hepatol. 2020;35:2032-2040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Hamid HKS, Ahmed AY, Simmons JR. Postcolonoscopy Appendicitis: A Review of 57 Cases. Surg Laparosc Endosc Percutan Tech. 2019;29:328-334. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Gancayco J, Soulos PR, Khiani V, Cramer LD, Ross JS, Genao I, Tinetti M, Gross CP. Age-based and sex-based disparities in screening colonoscopy use among medicare beneficiaries. J Clin Gastroenterol. 2013;47:630-636. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Musielak M, Patel H, Fegelman E. Postcolonoscopy appendicitis: laparoscopy a viable option. Am Surg. 2012;78:1300-1303. [PubMed] |
| 6. | Lipton S, Estrin J. Postcolonoscopy appendicitis: a case report. J Clin Gastroenterol. 1999;28:255-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 8. | Kavic SM, Basson MD. Complications of endoscopy. Am J Surg. 2001;181:319-332. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 113] [Article Influence: 4.7] [Reference Citation Analysis (1)] |
| 9. | Basson MD, Etter L, Panzini LA. Rates of colonoscopic perforation in current practice. Gastroenterology. 1998;114:1115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 31] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Kim SY, Kim HS, Park HJ. Adverse events related to colonoscopy: Global trends and future challenges. World J Gastroenterol. 2019;25:190-204. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 91] [Cited by in RCA: 165] [Article Influence: 27.5] [Reference Citation Analysis (8)] |
| 11. | Shaw D, Gallardo G, Basson MD. Post-colonoscopy appendicitis: A case report and systematic review. World J Gastrointest Surg. 2013;5:259-263. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 21] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Gatto NM, Frucht H, Sundararajan V, Jacobson JS, Grann VR, Neugut AI. Risk of perforation after colonoscopy and sigmoidoscopy: a population-based study. J Natl Cancer Inst. 2003;95:230-236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 354] [Cited by in RCA: 338] [Article Influence: 15.4] [Reference Citation Analysis (0)] |
| 13. | Vender R, Larson J, Garcia J, Topazian M, Ephraim P. Appendicitis as a complication of colonoscopy. Gastrointest Endosc. 1995;41:514-516. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 29] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Doohen RR, Aanning HL. Appendiceal colic: A rare complication of colonoscopy. S D J Med. 2002;55:526-527. [PubMed] |
| 15. | Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ. Diagnostic performance of multidetector computed tomography for suspected acute appendicitis. Ann Intern Med. 2011;154:789-796, W. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 122] [Cited by in RCA: 126] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 16. | Wong J, Chang J, Alkidady W. Acute appendicitis post-colonoscopy. ANZ J Surg. 2016;86:309-310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Hirata K, Noguchi J, Yoshikawa I, Tabaru A, Nagata N, Murata I, Itoh H. Acute appendicitis immediately after colonoscopy. Am J Gastroenterol. 1996;91:2239-2240. [PubMed] |
| 18. | Srivastava V, Pink J, Swarnkar K, Feroz A, Stephenson BM. Colonoscopically induced appendicitis. Colorectal Dis. 2004;6:124-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Paramythiotis D, Kofina K, Papadopoulos V, Michalopoulos A. Diagnostic Colonoscopy Leading to Perforated Appendicitis: A Case Report and Systematic Literature Review. Case Rep Gastrointest Med. 2016;2016:1378046. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 20. | Kafadar MT, Bilgiç İ, Kartal S, Güliter S. An unusual cause of acute abdomen: Post-colonoscopy appendicitis. Turk J Surg. 2018;34:340-341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 21. | Zhou XC, Huang CW, Dai YY, Huang ZY, Lou Z. Perforated appendicitis after colonoscopy: cause or coincidence?: A rare case report and literature review. Medicine (Baltimore). 2017;96:e8747. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 22. | Basson MD, Persinger D, Newman WP. Association of Colonoscopy With Risk of Appendicitis. JAMA Surg. 2018;153:90-91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Ohtani H, Tamamori Y, Arimoto Y, Nishiguchi Y, Maeda K, Hirakawa K. Meta-analysis of the results of randomized controlled trials that compared laparoscopic and open surgery for acute appendicitis. J Gastrointest Surg. 2012;16:1929-1939. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 90] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 24. | Sohn M, Agha A, Bremer S, Lehmann KS, Bormann M, Hochrein A. Surgical management of acute appendicitis in adults: A review of current techniques. Int J Surg. 2017;48:232-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.9] [Reference Citation Analysis (0)] |