Published online Dec 6, 2023. doi: 10.12998/wjcc.v11.i34.8164
Peer-review started: September 1, 2023
First decision: October 17, 2023
Revised: October 30, 2023
Accepted: November 27, 2023
Article in press: November 27, 2023
Published online: December 6, 2023
Processing time: 96 Days and 7.4 Hours
Langerhans cell histiocytosis (LCH) is a rare clonal proliferative disease of Langerhans cells with unknown pathogenesis. An increasing number of clinicians recognize that LCH has a wide clinical spectrum and a highly varied course. Adults rarely develop LCH. Here, we report a case of adult localized LCH.
A 32-year-old woman presented with plaques and ulcers on the vulva and crissum, accompanied by pain that persisted for more than one year. Physical examination revealed a red-infiltrating plaque with ulcerations and exudates in the vulva and crissum. Pathological examination revealed a diffuse infiltration of lymphocytes, eosinophilic granulocytes, and histiocytoid cells in the superficial dermis. Proliferative histiocytoid cells showed mild atypia, partly with kidney-shaped nuclei. Immunohistochemical examination showed that the histiocytoid cells were positive for S100 protein and CD1 and weakly positive for CD68 (20% +), with a Ki-67 index of 30%. Laboratory tests did not reveal any other systemic damage. The patient was diagnosed with adult localized LCH and was prescribed oral prednisone (20 mg) once daily. The skin lesions gradually improved and are still being followed-up.
Adult localized LCH is rare and must be differentiated from other common conditions.
Core Tip: Langerhans cell histiocytosis (LCH) is a rare clonal proliferative disease of Langerhans cells that express an immunophenotype positive for S100 protein, CD1 (CD1a), and Langerin (CD207) and contain cytoplasmic Birbeck granules. Adult localized LCH presenting with plaques and ulcers on the vulva and crissum is rare and must be differentiated from other common conditions.
- Citation: Yang PP, Hu SY, Chai XY, Shi XM, Liu LX, Li LE. Adult localized Langerhans cell histiocytosis: A case report. World J Clin Cases 2023; 11(34): 8164-8169
- URL: https://www.wjgnet.com/2307-8960/full/v11/i34/8164.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i34.8164
Langerhans cell histiocytosis (LCH) is a disease characterized by the proliferation of Langerhans cells that express an immunophenotype positive for S100 protein, CD1 (CD1a), and Langerin (CD207) and contain cytoplasmic Birbeck granules[1]. Several organs are involved in this process. The childhood and adult forms of LCH should be considered separately. Two-thirds or more children under one year of age and those aging 1–4 years have multi-system diseases, including those of the liver, lungs, or bone marrow. In adults, the peak age of presentation is between 20 years and 35 years, with multi-system diseases occurring in one-third to two-thirds of adults with LCH. The bones are the most commonly involved organs. Skin and mucosal involvement are the second most common manifestations in adults[2]. Here, we report a case of adult LCH that presented solely with skin involvement, without systemic damage.
A 32-year-old woman presented with plaques and ulcers on the vulva and crissum, accompanied by pain and exudates on the surface of the ulcers.
The patient reported a rash on the vulva as the first manifestation, which gradually enlarged and extended to the perianal area. She did not complain of diarrhea, constipation, melena, hematochezia, diabetes insipidus, changes in appetite, or weight loss.
The patient denied any previous chronic diseases, hepatitis, tuberculosis, and any history of infectious disease and close contact with infected people. She also denied drug and food allergies. Her vaccination history was unknown.
The patient had no family history of cancer.
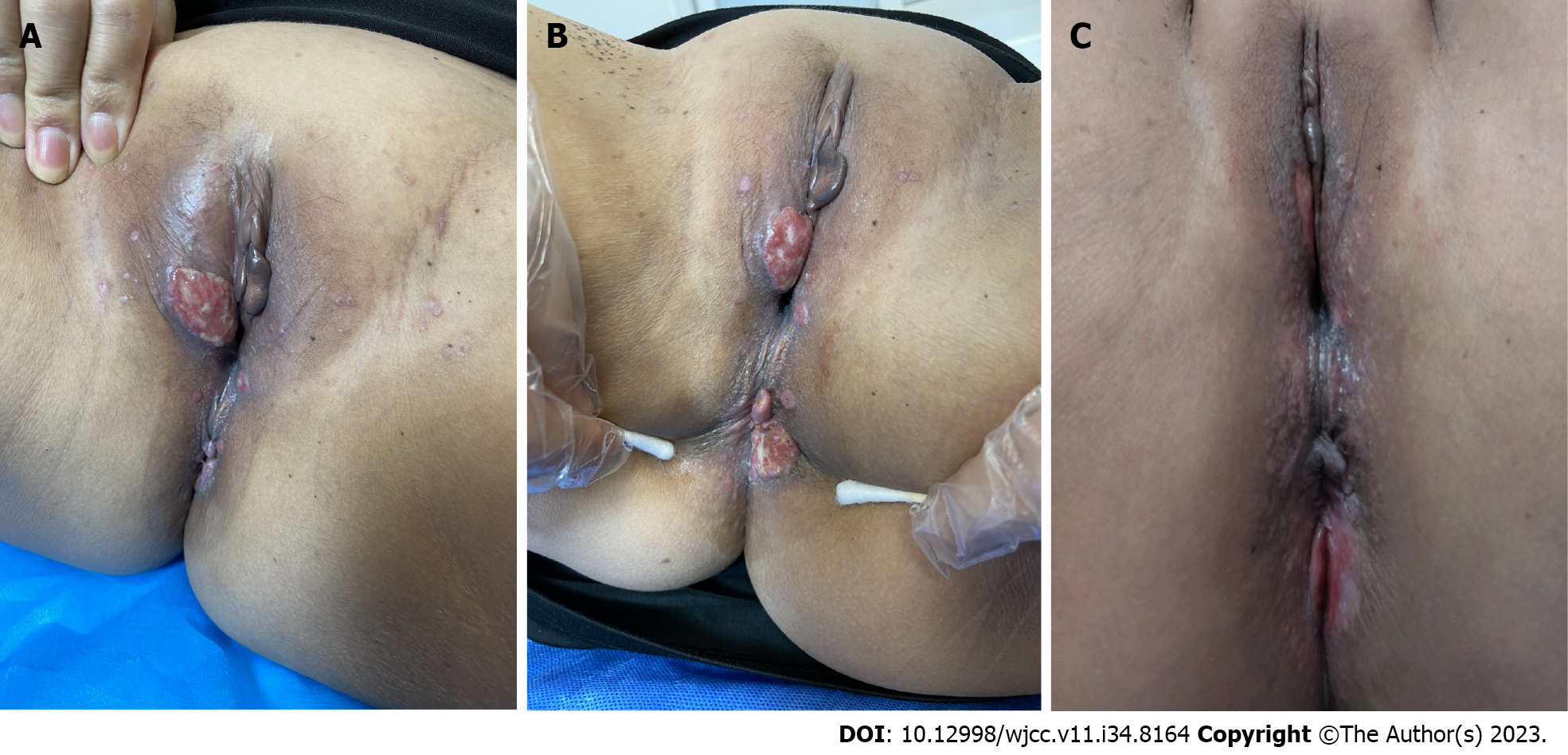
Physical examination revealed red erosive plaques and ulcers on the vulva and perianal areas, which were covered with exudates (Figure 1). No skull defects were observed.
A punch biopsy was performed at the intersection between the normal skin and vulvar rash during the initial visit. The tissue section was fixed in 10% neutral formalin, paraffin-embedded, sectioned, stained with hematoxylin and eosin, and subjected to direct immunohistochemistry before observation under light microscopy. Each immunohistochemistry test group included a negative self-control. All primary and secondary antibodies were purchased from ZSGB-BIO, Beijing, China. The primary antibody incubation lasted 50 min at 37 °C and 20 min at 37 °C for the secondary antibody. Visualization was performed using DAB (3,3'-diaminobiphenyl), and results were assessed by capturing images with a light microscope.
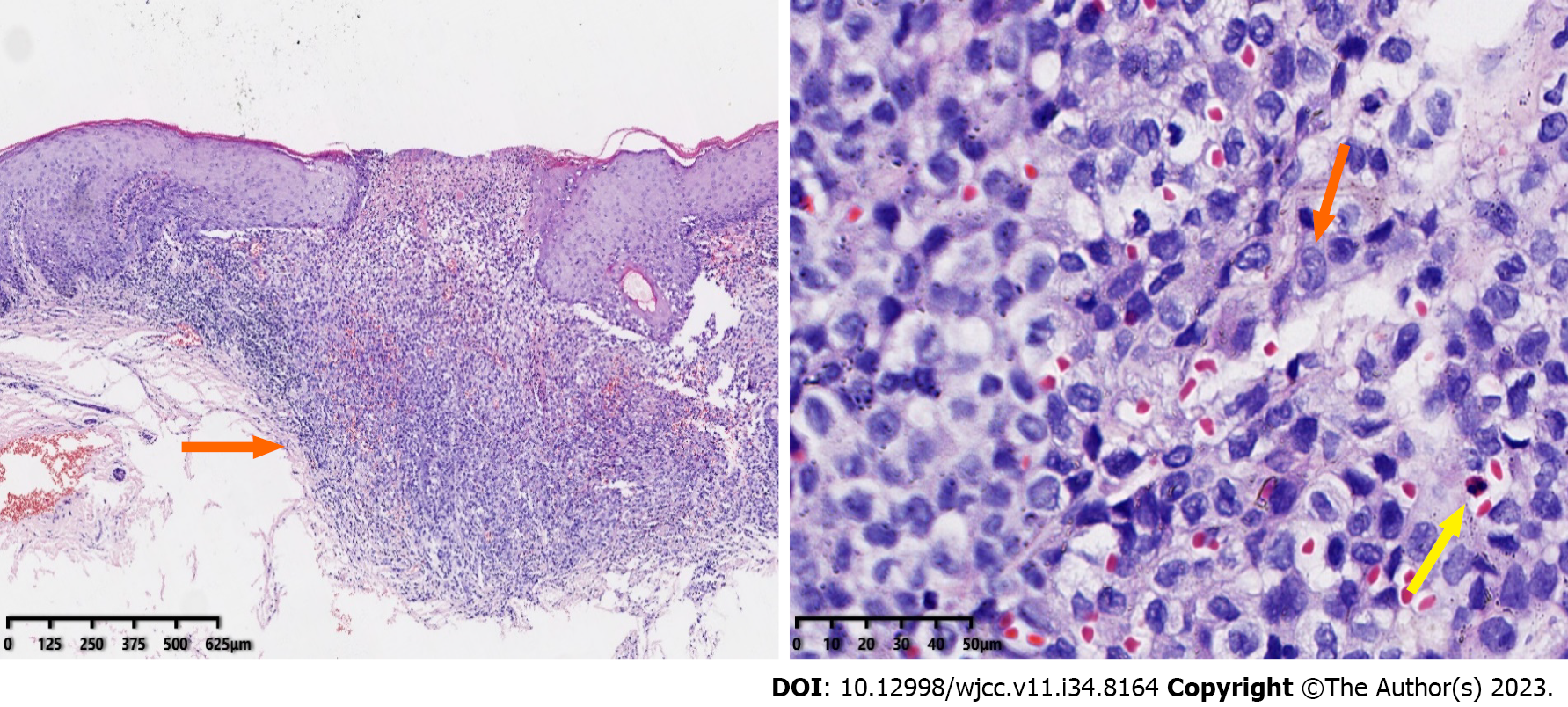
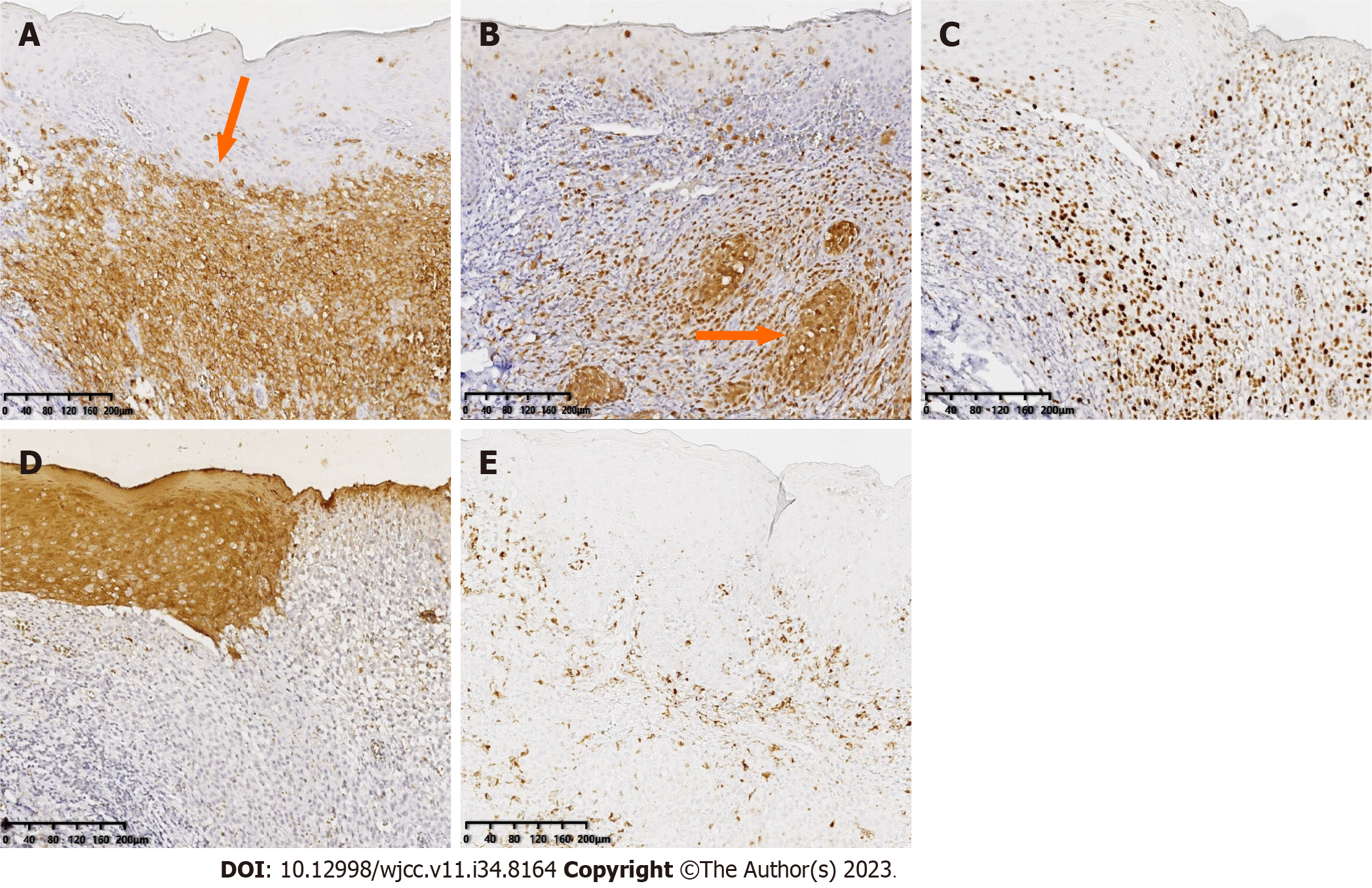
Pathology revealed histiocytoid cells in the superficial and middle dermal layers with mild nuclear atypia and a population of occasional eosinophils. The atypical histiocytoid cells were positive for S100 protein and CD1a, and weakly positive for CD68 (20% +), with a Ki-67 index of 30%. These cells were negative for creatine kinase (Figures 2 and 3).
Computed tomography of the sacroiliac joint showed that the cortical bone of the sacral surface of the right sacroiliac joint was discontinuous.
Based on these results, the patient was diagnosed with adult localized LCH.
The patient was prescribed thalidomide 0.1 g orally twice daily and methotrexate 7.5 mg once weekly.
Three months later, the patient reported a poor response and was prescribed prednisone 20 mg orally once daily; the lesions gradually improved and the patient is still being followed up (Figure 1).
LCH is a rare group of disorders in which mononuclear macrophages and dendritic cell systems proliferate, often affecting the skin and bones. It can also lead to multi-system diseases of the liver, spleen, lung, central nervous system, lymph nodes, thymus, gastrointestinal tract, and bone marrow[1-5]. Liver and spleen involvement causes abnormal liver function, hepatomegaly, and hypersplenism[6]. Involvement of the lungs may cause chest pain and dyspnea[7]. The pituitary gland may also be affected by LCH causing diabetes insipidus[8-10]. The bones of the skull are the most common sites affected by LCH, but other bones, such as the femur, scapula, rib, mandible, and vertebrae, can also be affected[11-13].
Depending on the number of systems involved in the patient, LCH is divided into single-system-LCH (SS-LCH) and multi-system-LCH (MS-LCH)[14]. SS-LCH is divided into SS-S (a single site involving the bone, skin, or lymph nodes) and SS-M (involving multiple parts of the bone or lymph nodes). Patients with SS-LCH have a good prognosis, whereas those with MS-LCH, especially those with liver and hematopoietic system involvement, have a poor prognosis and higher mortality rate[6,15]. Generally, patients with LCH in whom only the skin is affected have a good prognosis and about 50% of the patients can be in remission within a few months; however, disease progression and persistence are more common, and long-term follow-up is recommended[16].
The most common areas of skin involvement in LCH are the scalp, trunk, skin folds, and mucosa. Skin lesions vary and present as papules, blisters, pustules, purpura, plaques, or ulcers[2]. The most characteristic presentations of adult LCH are groin, perianal, and vulvar involvements. Chen et al[17] reported a case of adult LCH with an eczematoid lesion in the vulva as the initial manifestation, whereas Wu et al[18]reported a case of LCH with perianal skin lesions as the first presentation. In the present case, the skin lesions were located on both the vulvar and perianal regions. Computed tomography of the sacroiliac joint revealed discontinuity in the cortical bone of the right sacroiliac joint. Changes in the sacroiliac joint necessitated further follow-up and progressed slowly with no apparent systemic involvement. In conclusion, adult LCH is a rare disease that must be distinguished from other common diseases, including Paget’s disease, candidiasis, and malignant melanoma.
Treatment of LCH should be individualized according to the number and severity of organs involved. Therapeutic options should also prevent long-term side effects of medication. Topical and systemic corticosteroids, nitrogen mustard, methotrexate, psoralen plus ultraviolet-A radiation, narrow-band ultraviolet-B radiation (or excimer laser), thalidomide, interferon, and azathioprine can be considered for treatment depending on the extent of skin lesions[2]. Therefore, surgical resection of a single lesion should be considered. No single treatment has been effective in all patients.
The rarity of LCH in adults may have resulted in its overlooked diagnosis. Therefore, dermatologists should consider this disease, along with its varied presentation and treatment options.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Exbrayat JM, France S-Editor: Lin C L-Editor: Wang TQ P-Editor: Lin C
| 1. | Bolognia JL, Jorizzo JL, Rapini RP, Schaffer JV. Dermatology. 4th ed. Philadelphia: Elsevier, 2017: 1614-1620. |
| 2. | James WD, Elston D, Treat JR, Rosenbach MA. Andrews' Diseases of the Skin: Clinical Dermatology. 13th ed. Edinburgh: Elsevier, 2019: 726-729. |
| 3. | DiCaprio MR, Roberts TT. Diagnosis and management of langerhans cell histiocytosis. J Am Acad Orthop Surg. 2014;22:643-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Burns T, Breathnach S, Cox N, Griffiths C. Rook’s Textbook of Dermatology. 8th ed. Chichester: Blackwell Publishing Ltd, 2010. |
| 5. | Liu GQ, Liu T, Shen C, Zhou L, Ouyang RY. Adult Langerhans cell histiocytosis involving lung, pituitary, thyroid, liver, lymph nodes, and skin: a case report. Zhongnan Daxue Xuebao (Yixueban). 2020;45:96-101. |
| 6. | Ye YJ, Chen W, Liu B, Wang L. Adult hepatic Langerhans cell histiocytosis: a case report. Zhongguo Xiandai Yixue Zazhi. 2019;29:125-126. |
| 7. | Tazi A. Adult pulmonary Langerhans' cell histiocytosis. Eur Respir J. 2006;27:1272-1285. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 178] [Cited by in RCA: 149] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 8. | Choi JE, Lee HR, Ohn JH, Moon MK, Park J, Lee SJ, Choi MG, Yoo HJ, Kim JH, Hong EG. Adult multisystem langerhans cell histiocytosis presenting with central diabetes insipidus successfully treated with chemotherapy. Endocrinol Metab (Seoul). 2014;29:394-399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Liu K, Zeng M, Chen J, Hui Y, Kong Q, Duan Q, Sang H. Multisystem Langerhans cell histiocytosis with diabetes insipidus in an adult. Indian J Dermatol. 2022;67:184-186. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Lourenço J, Ferreira C, Marado D. Adult pulmonary Langerhans cell histiocytosis revealed by central diabetes insipidus: A case report and literature review. Mol Clin Oncol. 2020;13:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 11. | Angelini A, Mavrogenis AF, Rimondi E, Rossi G, Ruggieri P. Current concepts for the diagnosis and management of eosinophilic granuloma of bone. J Orthop Traumatol. 2017;18:83-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 12. | Simko SJ, Garmezy B, Abhyankar H, Lupo PJ, Chakraborty R, Lim KP, Shih A, Hicks MJ, Wright TS, Levy ML, McClain KL, Allen CE. Differentiating skin-limited and multisystem Langerhans cell histiocytosis. J Pediatr. 2014;165:990-996. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 13. | Sapkas G, Papadakis M. Vertebral Langerhans cell histiocytosis in an adult patient: case report and review of the literature. Acta Orthop Belg. 2011;77:260-264. [PubMed] |
| 14. | Hamdan M, Qiao JC, Fikfak V. Adult-onset perianal Langerhans cell histiocytosis presenting as pruritus ani: a case report and review of the literature. J Med Case Rep. 2021;15:357. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Gao Z, Yao X, Hu J. Bone marrow Langerhans cell histiocytosis: a case report. Guangdong Yixue. 2017;38:2597. [DOI] [Full Text] |
| 16. | Barkaoui MA, Queheille E, Aladjidi N, Plat G, Jeziorski E, Moshous D, Lambilliotte A, Kebaili K, Pacquement H, Leverger G, Mansuy L, Entz-Werlé N, Bodet D, Schneider P, Pagnier A, Lutun A, Gillibert-Yvert M, Millot F, Toutain F, Reguerre Y, Thomas C, Tazi A, Emile JF, Donadieu J, Héritier S. Long-term follow-up of children with risk organ-negative Langerhans cell histiocytosis after 2-chlorodeoxyadenosine treatment. Br J Haematol. 2020;191:825-834. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Chen Y, Yu XH, Yang GL. Genital eczema-like lesions as the first manifestation of adult Langerhans cell histiocytosis. Linchuang Pifuke Zazhi. 2018;47:25-28. [DOI] [Full Text] |
| 18. | Wu HJ, Yang S, Zhou CL, Wang S, Yang X, Xie JY, Zhang HY, Song C, Dong Q, Sun C, Li M. A case of Langerhans Cell Histiocytosis with perianal lesion as the first manifestation and literature review. Zhongguo Pifuxingbingxue Zazhi. 2020;34:1056-1058. [DOI] [Full Text] |