Published online Nov 16, 2023. doi: 10.12998/wjcc.v11.i32.7858
Peer-review started: September 21, 2023
First decision: October 9, 2023
Revised: October 17, 2023
Accepted: November 3, 2023
Article in press: November 3, 2023
Published online: November 16, 2023
Processing time: 55 Days and 10.6 Hours
Persistent left superior vena cava (PLSVC), a relatively rare thoracic vascular malformation, can inconvenience perfusionists and operators when encountered during deep hypothermic circulatory arrest (DHCA).
Herein, we describe the case of a patient with concurrent giant aortic arch aneurysm, aortic stenosis, and PLSVC. To treat these conditions, we performed right hemiarch and aortic valve replacements under DHCA. Notably, we applied “bilateral superior vena cava retrograde cerebral perfusion (RCP)” for cerebral protection, which significantly optimized the surgical procedure and reduced the risk of postoperative complications. The patient was discharged 14 d after surgery with no complications.
Surgical intervention for PLSVC under DHCA can be performed using the bilateral superior vena cava RCP approach.
Core Tip: Persistent left superior vena cava (PLSVC) is a malformation that can coexist with the right superior vena cava without causing an imbalance in the hemodynamics, thereby concealing its detection during clinical consultation. We describe the case of a patient with an aortic arch aneurysm who also had PLSVC. When replacing the right hemiarch under deep hypothermic circulatory arrest, we utilized a “bilateral superior vena cava retrograde cerebral perfusion (RCP)” approach to PLSVC. The patient was discharged 14 d postoperatively without any complications. To the best of our knowledge, RCP via the bilateral superior vena cava has not previously been reported.
- Citation: Mi ZY, He G, Gao HL, Li C. Persistent left superior vena cava in right hemiarch replacement under deep hypothermic circulatory arrest: A case report. World J Clin Cases 2023; 11(32): 7858-7864
- URL: https://www.wjgnet.com/2307-8960/full/v11/i32/7858.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i32.7858
Persistent left superior vena cava (PLSVC) is one of the most prevalent venous malformations of the superior vena cava vessels, occurring in approximately 0.3%-0.5% of individuals[1]. PLSVC with agenesis of the right superior vena cava (RSVC) is also known as isolated PLSVC[2]. In approximately 80%-90% of cases, PLSVC returns to the right atrium (RA) via the coronary sinus (CS), coexisting with the RSVC without causing an imbalance in the hemodynamics, thereby making detection difficult during clinical consultation[3]. PLSVC is usually detected incidentally during cardiovascular surgery[4]. However, PLSVC can cause extracorporeal circulation drainage, retrograde cerebral perfusion (RCP), and retrograde arrest fluid perfusion failure, presenting challenges during cardiac surgery.
Herein, we present the case of a patient with an aortic arch aneurysm combined with PLSVC who required a right hemiarch replacement under deep hypothermic circulatory arrest (DHCA). Cerebral protection was achieved by DHCA and RCP. To the best of our knowledge, this is the first report of RCP via the bilateral superior vena cava in the literature.
On June 20, 2022, a 55-year-old male patient presented with cough and shortness of breath that had persisted for 3 mo.
Three months prior to admission, the patient had presented with cough and shortness of breath without any obvious trigger, accompanied by the coughing up of white foamy sputum. These symptoms were aggravated by activity and could be relieved by rest. There was no diagnosis nor treatment at that time.
Prior to this visit, the patient had been in good health with no underlying diseases.
The patient had no history of familial hereditary diseases.
At the time of admission, the patient's blood pressure was 90/64 mmHg, there was no cyanosis in the lips, there was no protuberance in the precordial area, the apical beat point was located 0.5 cm medial to the intersection of the left fifth intercostal space and the midclavicular line, there was no pericardial friction, the heart rhythm was neat, a systolic ejective murmur was heard at the auscultation area of the aortic valve, and there was no abnormal murmur at the other auscultation areas of the heart valves.
The results of all of biochemical tests were within normal limits.
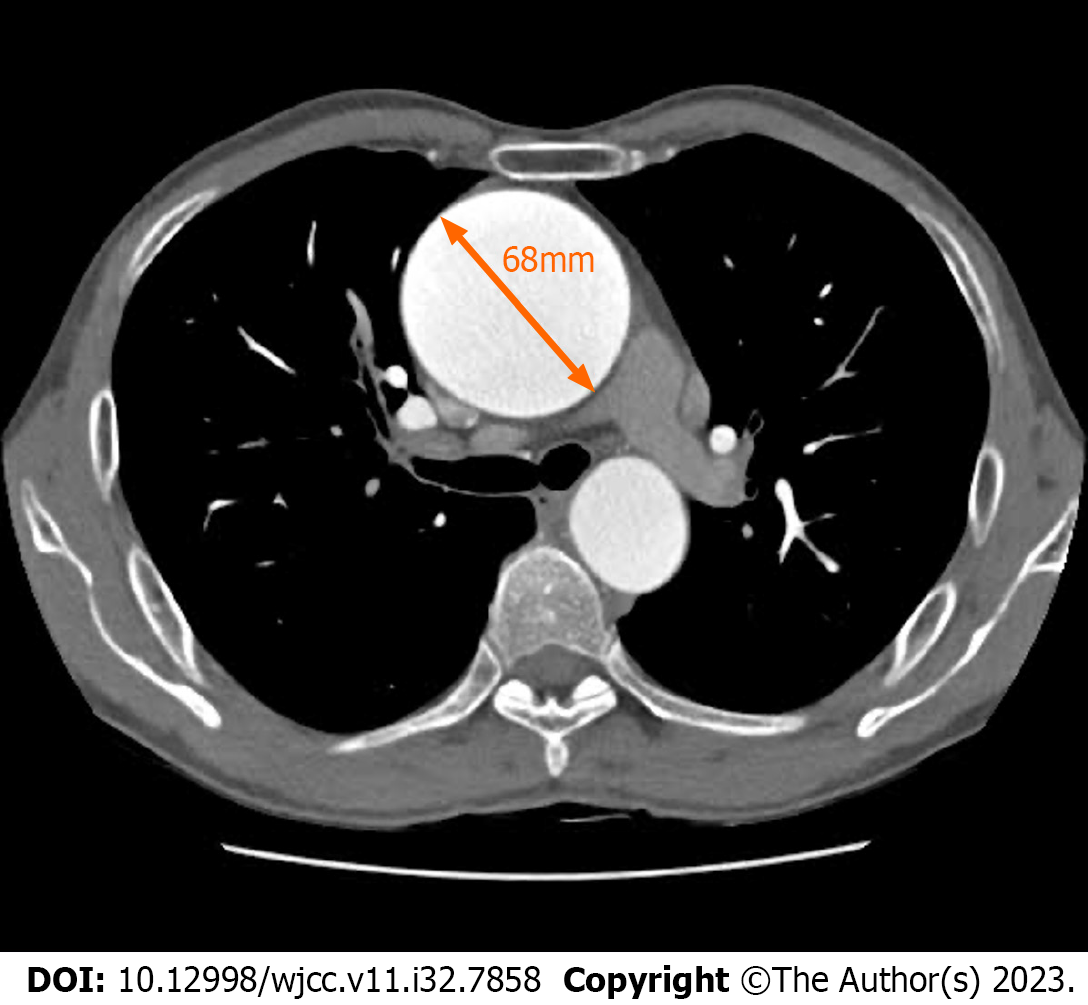
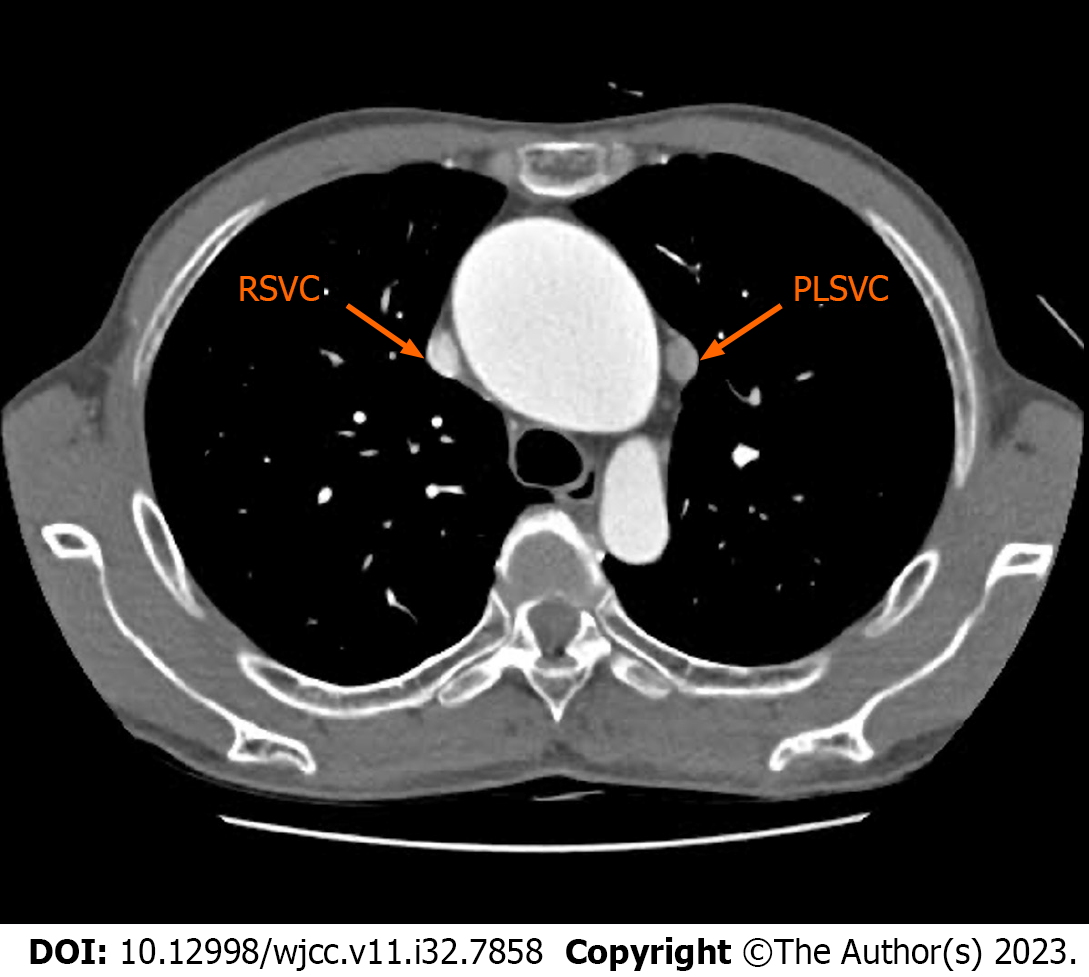
Multislice computed tomography revealed a significant aortic arch aneurysm with a maximum diameter of approximately 68 mm (Figure 1). The PLSVC returned to the CS and collected venous flow from the left internal jugular, left subclavian, and azygos veins (Figure 2). The diameter of the PLSVC was 11 mm (Figure 3). Echocardiography revealed severe aortic stenosis (AS) with an aortic annular diameter of 21.8 mm, annular area of 6.16 cm2, maximum aortic antegrade flow velocity of 4.83 m/s, and mean pressure difference of 41 mmHg. The patient’s left ventricular ejection fraction was 70%, and the atrial and ventricular sizes were within the normal range. Notably, we observed enlargement of the CS on echocardiography to approximately 2.5 times the normal size.
We further performed saline-contrast echocardiography. Saline contrast was injected through the left arm vein, and the order of contrast injection was the PLSVC, CS, and RA; no contrast was present in the RSVC. Upon injection of saline contrast through the right arm vein, in the order of the RSVC and RA, we noted the absence of a bridging vein (BV) connected between the PLSVC and RSVC[5].
Bicuspid aortic valve, severe AS, aortic arch aneurysm, PLSVC, and New York Heart Association Class IV status.
We performed aortic valve replacement and right hemiarch replacement under DHCA after diagnosis, and the procedure was as follows. While sawing through the sternum to expose the heart and right aortic arch, our surgical exploration revealed the absence of the innominate vein, and a giant aneurysm in the right aortic arch. The heart was lifted to expose the PLSVC crossing the anterior aspect of the left pulmonary artery and flowing downward into the CS (Figure 4).
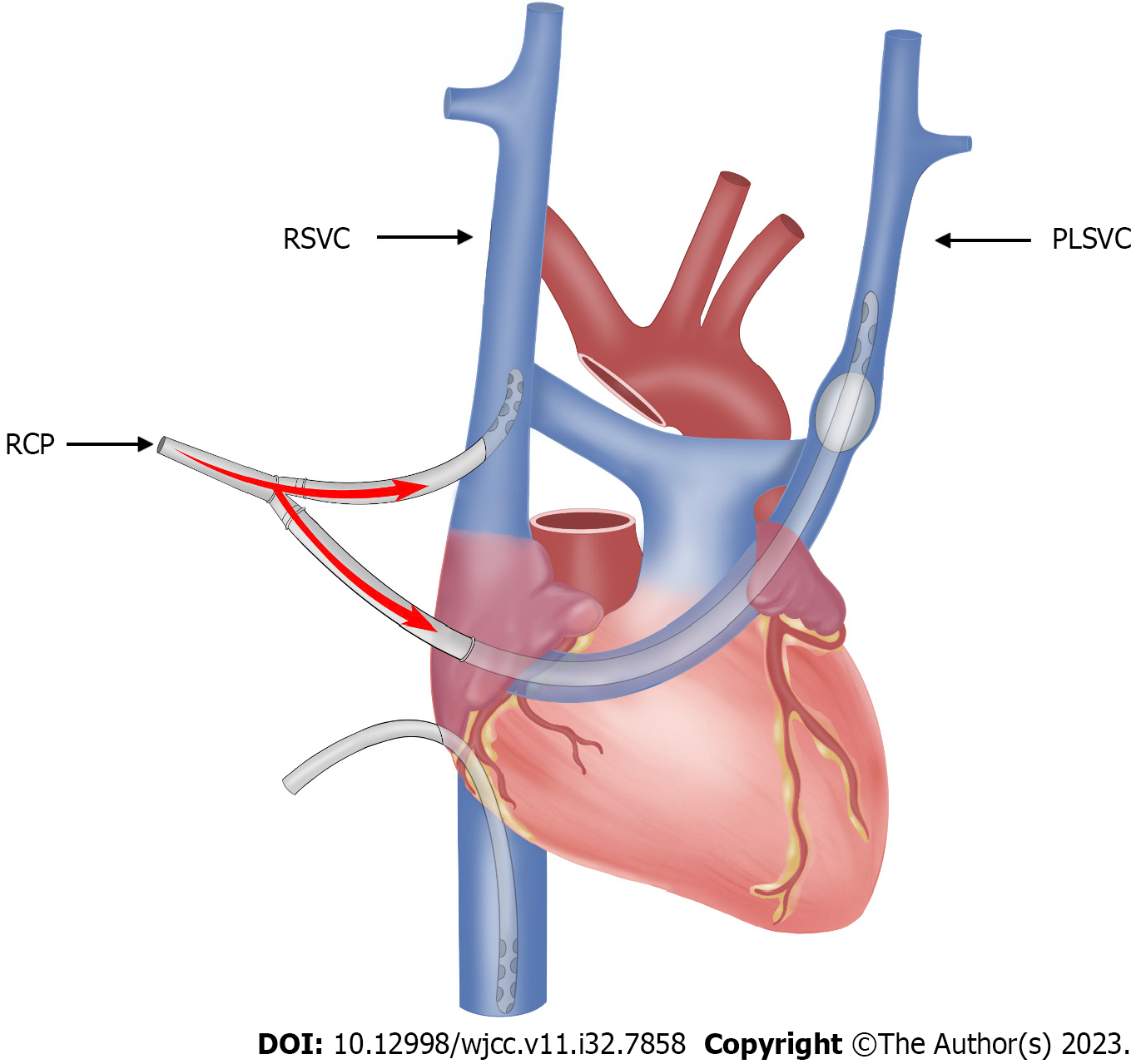
The right femoral artery was cannulated and connected to an arterial perfusion tube, and venous drains were inserted in the superior and inferior vena cava lumens. A 1.5 cm incision was made on the surface of the RA, an inflatable balloon cannula was inserted into the PLSVC via the CS, and the left and RSVC drains were connected to the superior vena cava drains of the extracorporeal circulation machine via a T-tie to initiate extracorporeal circulation.
After gradual lowering of the circulatory temperature (Figure 5), we clamped the distal ascending aorta with a blocking clamp, and the ascending aorta was transected at 1 cm above the sinotubular junction. Myocardial protection was achieved by cascade perfusion and aortic valve replacement. We continued to lower the circulatory temperature to 20 ℃, at which point the extracorporeal circulation was stopped, the ascending aortic blocking clamp was opened, and RCP was performed via the bilateral superior vena cava, with the perfusion pressure maintained at 20-25 mmHg (Figure 5). We subsequently excised the aortic arch aneurysm and anastomosed the artificial vessel with the distal aorta. The proximal artificial vessel was clipped after completion of the anastomosis, and the side of the head was lowered to remove residual gas from the blood vessels. Extracorporeal circulation was restarted, and the circulatory temperature was gradually restored to 30 ℃, while anastomosing the proximal end of the ascending aorta with the artificial vessel. Subsequently, we opened the artificial vessel blocking clamps, and the heart resumed beating by itself. Then strict hemostasis and suturing of the surgical incision were performed.
After the operation, the patient was sent to the intensive care unit for continued treatment, with 800 mL of intraoperative bleeding. The DHCA duration was 16 min. The duration of the aortic block was 90 min. Postoperatively, the patient was mechanically ventilated for 7 h without complications and was discharged after 12 d.
PLSVC is caused by the degenerative failure of the left anterior cardinal vein that forms the Marshall ligament[1]. Its incidence is relatively rare in the general population. As PLSVC usually has no hemodynamically significant con
With the increased awareness of PLSVC and the continuous development of imaging techniques in medicine, the diagnosis of PLSVC is becoming increasingly common. Experienced imaging physicians can now identify the presence of a PLSVC using multilayer spiral computed tomography of the chest, which can show the drainage pathway of the PLSVC in its entirety. The detection of a dilated CS upon echocardiography suggests the presence of PLSVC[9]. Saline contrast echocardiography can confirm the diagnosis of PLSVC and the BV connection between PLSVC and RSVC[10]. In addition, widening of the left upper mediastinum on chest radiography and leftward deviation of the electrocardiographic electrical axis are indicators of PLSVC[11]. It has further been suggested that an enlarged CS can compress the atrioventricular node and hippocampus, leading to arrhythmias, which can also indicate a diagnosis of PLSVC[12].
DHCA and RCP can be used for cerebral protection during aortic arch surgery. RCP is one of the key factors affecting clinical outcomes. Ensuring a moderate perfusion pressure (20-25 mmHg) during RCP can prevent the development of postoperative cerebral edema[12]. Several reports have confirmed that PLSVC occurrence in general cardiac surgery leads to retrograde arrest fluid perfusion failure[13]. However, no incidences of PLSVC encountered during DHCA surgery have been reported to date. Previous studies have shown that a DHCA duration of > 25 min is a risk factor for transient neurological deficits, and that the duration of DHCA correlates linearly with the incidence of transient neurological deficits, which significantly increase when the duration of ischemia exceeds 50 min[14]. Therefore, in this case, we used a single pump and two tubes to perform “bilateral superior vena cava RCP”, which prevented the prolongation of DHCA time due to RCP failure. In cases with an abundant BV connection between the PLSVC and RSVC, surgeons may also block the PLSVC with an intravenous sleeve and perform RCP using the RSVC. Preoperative verification of BV connections between the PLSVC and the RSVC can be performed using saline-contrast echocardiography[10].
In conclusion, when PLSVC is encountered during the DHCA procedure, the bilateral superior vena cava RCP technique ensures stable perfusion pressure and adequate perfusion flow and is safe and effective. The preoperative identification of PLSVC is particularly critical in DHCA surgery. Further, preoperative planning of the surgery involving a reasonable RCP approach can shorten DHCA time, allowing optimization of the surgical procedure. With this approach, major complications can be prevented, and a satisfactory clinical outcome can be achieved.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Vyshka G, Albania S-Editor: Qu XL L-Editor: Wang TQ P-Editor: Zhang XD
| 1. | Tak T, Crouch E, Drake GB. Persistent left superior vena cava: incidence, significance and clinical correlates. Int J Cardiol. 2002;82:91-93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 53] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 2. | Teklehaimanot A, Nguyen-Dinh P, Collins WE, Barber AM, Campbell CC. Evaluation of sporontocidal compounds using Plasmodium falciparum gametocytes produced in vitro. Am J Trop Med Hyg. 1985;34:429-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 50] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 3. | Mantini E, Grondin CM, Lillehei CW, Edwards JE. Congenital anomalies involving the coronary sinus. Circulation. 1966;33:317-327. [PubMed] |
| 4. | Elhamamsy M, Aldemerdash A, Zahran F, Bakir BM, Alanazi NA, Awadallah YA, Haggag SI, Alshiekh MS. Persistent left superior vena cava in patient with right atrial myxoma undergoing open heart surgery. A case report and review of literature. Saudi J Anaesth. 2020;14:217-220. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 5. | Cherian SB, Ramesh BR, Madhyastha S. Persistent left superior vena cava. Clin Anat. 2006;19:561-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Cha EM, Khoury GH. Persistent left superior vena cava. Radiologic and clinical significance. Radiology. 1972;103:375-381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 101] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Gao M, Bian Y, Huang L, Zhang J, Li C, Liu N, Liu X, Zuo S, Guo X, Wang W, Zhao X, Long D, Sang C, Tang R, Li S, Dong J, Ma C. Catheter ablation for atrial fibrillation in patients with persistent left superior vena cava: Case series and systematic review. Front Cardiovasc Med. 2022;9:1015540. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 8. | Totorean IC, Vacarescu C, Cozma D, Luca CT, Feier H, Lazăr MA, Deme MA, Stoica S, Arnautu DA, Gaiță D. Pacemaker Implantation in a Patient with Isolated Persistent Left Superior Vena Cava Draining into the Left Atrium: A Case Report and Brief Literature Review. Diagnostics (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Lentini S, Recupero A. Recognition of persistent left superior vena cava in non-congenital patients undergoing cardiac surgery. Perfusion. 2011;26:347-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Recupero A, Pugliatti P, Rizzo F, Carerj S, Cavalli G, de Gregorio C, Di Bella G, Minutoli F, Arrigo F, Oreto G, Coglitore S. Persistent left-sided superior vena cava: integrated noninvasive diagnosis. Echocardiography. 2007;24:982-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 26] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 11. | Yuce M, Kizilkan N, Kus E, Davutoglu V, Sari I. Giant coronary sinus and absent right superior vena cava. Vasa. 2011;40:65-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Hsu LF, Jaïs P, Keane D, Wharton JM, Deisenhofer I, Hocini M, Shah DC, Sanders P, Scavée C, Weerasooriya R, Clémenty J, Haïssaguerre M. Atrial fibrillation originating from persistent left superior vena cava. Circulation. 2004;109:828-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 149] [Cited by in RCA: 157] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 13. | Oosawa M, Sakai A, Abe M, Hanayama N, Lin ZB, Kodera K. [Repeat open heart surgery in a case associated with persistent left superior vena cava: a method of simple occlusion of L-SVC using an alternative extra-pericardial approach and retrograde cardioplegia]. Kyobu Geka. 1995;48:741-744. [PubMed] |
| 14. | Ergin MA, Griepp EB, Lansman SL, Galla JD, Levy M, Griepp RB. Hypothermic circulatory arrest and other methods of cerebral protection during operations on the thoracic aorta. J Card Surg. 1994;9:525-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 107] [Cited by in RCA: 105] [Article Influence: 3.4] [Reference Citation Analysis (0)] |