Published online Nov 16, 2023. doi: 10.12998/wjcc.v11.i32.7778
Peer-review started: September 29, 2023
First decision: October 9, 2023
Revised: October 18, 2023
Accepted: November 2, 2023
Article in press: November 2, 2023
Published online: November 16, 2023
Processing time: 47 Days and 15.9 Hours
Tongue abscess (TA) is a very rare clinical condition and its treatment is very important. Surgical drainage is at the forefront in the treatment. Our study includes patients with tongue and tongue base abscesses.
To discuss the clinical and laboratory findings of these patients emphasizing the underlying causes and treatment options with the largest patient series in the English literature.
We included patients with isolated TA who applied to our clinic between January 1, 2020 and January 1, 2023. Those who lack the recorded data, those who are not between the ages of 18-66, those who have not undergone surgery-interventional procedure, and those who have infection and/or abscess in another place were excluded from the study.
There were two female (18%) and nine male (82%) patients in our series consisting of 11 patients. Their ages ranged from 18 to 66, and the mean ± SD was 48.63 ± 16.3. Considering the localization of the abscess, three anterior abscesses (27%), two lateral abscesses (18%), and six abscesses at the base of the tongue (54%) were detected.
Tongue abscesses can cause acute upper airway obstruction and respiratory collapse. It may be necessary to act quickly for the tracheotomy procedure and this procedure can usually be performed under local anesthesia as intubation cannot be achieved. When we encounter an abscess in an unexpected organ, difficulties may be encountered in the management of the patient.
Core Tip: Tongue abscess is a very rare disease due to the anatomical and physiological structure of the tongue. The rarity of the disease can make it difficult to diagnose. Particular attention should be paid to airway obstruction, sepsis, and mediastinitis. Surgical drainage should be performed in abscesses larger than one centimeter.
- Citation: Bal KK, Gür H, Demir I, Ismi O, Vayisoglu Y, Gorur K, Ozcan C, Unal M. Mortal condition in an unusual localization, analysis of isolated tongue and tongue base abscesses. World J Clin Cases 2023; 11(32): 7778-7784
- URL: https://www.wjgnet.com/2307-8960/full/v11/i32/7778.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i32.7778
Tongue abscess (TA) is a very rare disease, potentially dangerous due to possible airway obstruction. The anatomical, vascular and muscular structure of the tongue and the unique antibacterial properties of saliva promote prevention of infection. Foreign bodies and immunosuppression may predispose to infection. TA may show symptoms such as dysphagia, dyspnea, pain, referred pain, fever. Especially tongue base abscesses should be taken into consideration as they can cause sudden respiratory collapse. Drainage should be applied in the treatment of tongue abscesses[1]. Most tongue abscesses are unifocal and located in the anterior two-thirds of the tongue. Abscesses in the posterior part of the tongue (including the tongue base) mostly occur as diseases involving the lingual tonsil, infected thyroglossal duct cysts extending to the base of the tongue, ectopic thyroid gland, or dissemination of apical infections of the first or second molar teeth[2]. Most of the articles on the subject remained as case reports, and the patient series found in the literature are limited in number. A maximum of six patient series have been reported[3].
There are authors in the literature reporting that the ratios of neutrophil (NEU) and lymphocyte (LYMPH) values to each other are useful in predicting cardiac diseases, cancer, infective diseases and length of hospital stay[4-6]. There are also studies on infectious diseases involving the ratio of platelets (PLTs) and LYMPHs to each other, diseases with ischemic neuropathy hypothesis, allergic rhinitis and asthma, neonatal sepsis, congenital branchial cysts[7-10]. We aimed to discuss this article with up-to-date information, which includes the largest patient series and allows to look at the disease with different laboratory parameters.
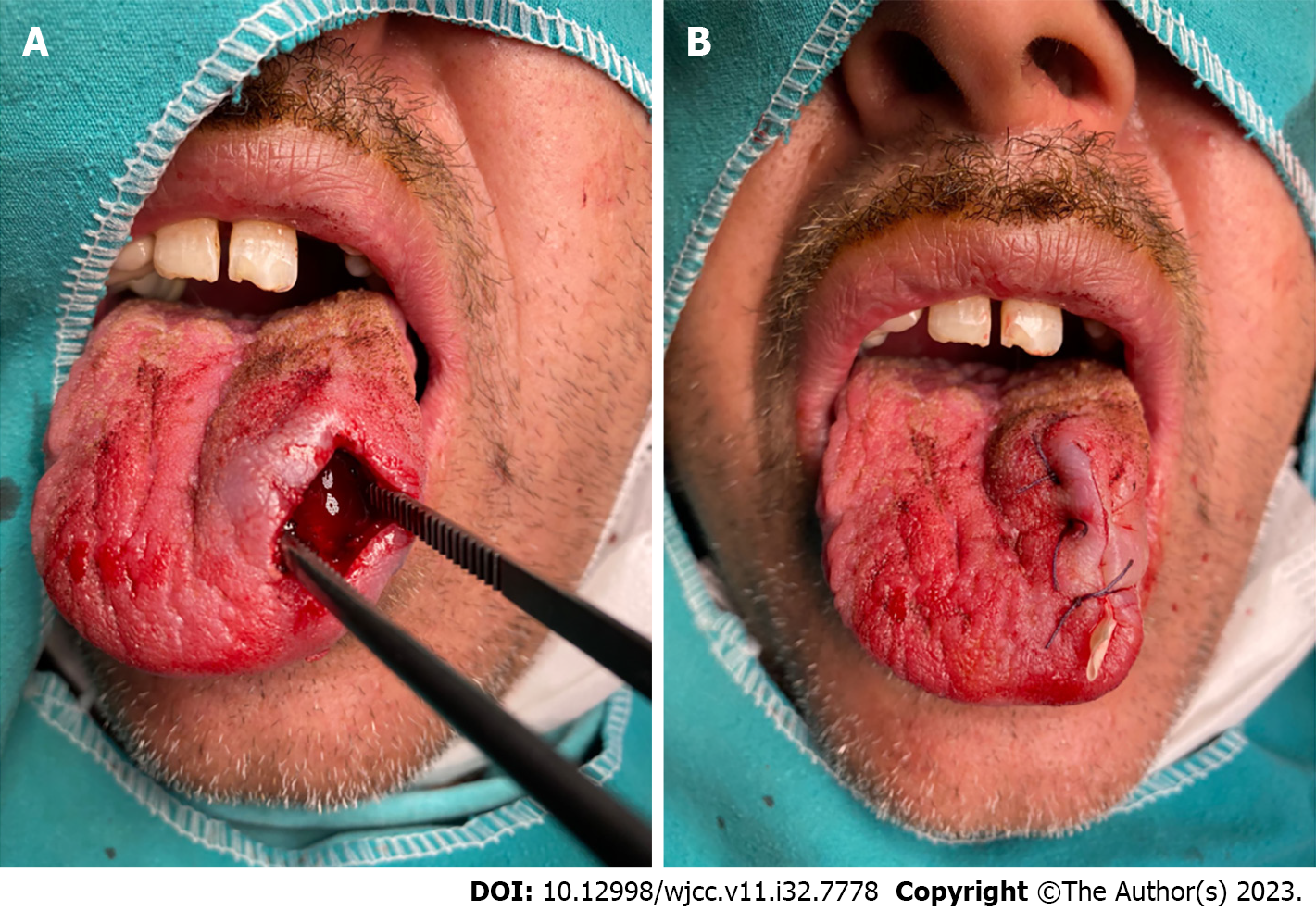
We included patients with isolated TA who applied to our clinic between January 1, 2020 and January 1, 2023. The patients were divided into two groups. Anterior and lateral tongue abscesses were named as group 1 (anterolateral) and tongue base abscesses were named as group 2. Patients’ age, gender, location of the abscess, contrast-enhanced computed tomography (CT) results (Figures 1A and B), white blood cell (WBC, μL) count, NEU (μL) count, LYMPH (μL) count, PLT (μL) number, NEU/LYMPH ratio (NLR), PLT/LYMPH ratio (PLR), C-reactive protein (CRP, m/L) value, erythrocyte sedimentation rate (ESR, m/h) value, abscess culture results, surgeries and interventional procedures (Figures 2A and B), underlying causes, additional systemic diseases, smoking history, length of hospital stay, antibiotics used, antibiotics used before admission, pathology results were recorded. A retrospective archive search was conducted for the study. Those who lack the recorded data, those who are not between the ages of 18-66, those who have not undergone surgery-interventional procedure, and those who have infection and/or abscess in another place were excluded from the study. Pediatric patients were excluded from the study. None of the patients had a history of foreign body or piercing. TA drainage and tracheotomy surgical procedures were performed under local anesthesia, and penrose drains were placed in all patients who underwent surgical drainage. In patients with tongue base abscess, the operation was started with tracheotomy under local anesthesia, followed by external drainage of the abscess with a transhyoidal approach under general anesthesia. Transoral tongue base abscess drainage; it has not been tried because the abscesses are closer to the hyoid bone and in deeper localizations, the external method is preferred (Table 1). All of our patients were decannulated (postoperative 10th d) after treatment. All of our patients were given intravenous treatment for 14 d as standard, and 600 m of oral cefdinir was given daily for 14 d at discharge. Ethics committee approval was obtained for our study (09/286). Written and verbal consent was obtained from all patients participating in the study.
| Patient | Surgery/puncture | Incision-drainage/incision-drainage and tracheotomy | Hospitalization time (d) |
| 1 | Surgery | Incision-drainage | 6 |
| 2 (HIV positive) | Surgery | Incision-drainage | 4 |
| 3 | Surgery | Incision-drainage | 9 |
| 4 | Surgery | Incision-drainage | 8 |
| 5 | Surgery | Incision-drainage and tracheotomy | 11 |
| 6 | Surgery | Incision-drainage and tracheotomy | 9 |
| 7 | Surgery | Incision-drainage and tracheotomy | 8 |
| 8 (diabetes mellitus) | Puncture | 6 | |
| 9 (hypothyroidism) | Surgery | Incision-drainage | 7 |
| 10 | Surgery | Incision-drainage and tracheotomy | 10 |
| 11 (intravenous heroin addict) | Surgery | Incision-drainage | 4 |
There were 2 female (18%) and 9 male (82%) patients in our series consisting of 11 patients. Their ages ranged from 18 to 66, and the mean ± SD was 48.63 ± 16.3. Considering the localization of the abscess, three anterior abscesses (27%), two lateral abscesses (18%) in group 1, six abscesses at the base of the tongue (54%) in group 2 were detected. Contrast-enhanced CT was performed in all abscess patients, and abscess sizes ranged from 10 to 45 mm, the mean ± SD was 22.9 ± 10.79 mm. Four of the patients (36%) had additional disease; acquired immune deficiency syndrome was found in one patient, diabetes mellitus (DM) in one patient, hypothyroidism in one patient, and intravenous heroin addiction in one patient. WBC ranged from 4240 to 20470, the mean ± SD was 11330 ± 4079. NEU ranged from 220 to 17870 and the mean ± SD was 8282 ± 3839. LYMPH ranged from 1020 to 3740, the mean ± SD was 2018 ± 872. PLT ranged from 172000 to 457000, the mean ± SD was 274818 ± 94437. The NLR ranged from 1.65 to 17.51, and the mean ± SD was 5.05 ± 4.43. The PLR ranged from 60.9 to 304.41, and the mean ± SD was 159.67 ± 81.27. CRP ranged from 4.9 to 178.6 and the mean ± SD was 43.59 ± 54.34. ESR ranged from 11 to 62, the mean ± SD was 35.81 ± 16.88. Bacterial growth was observed as a result of abscess culture in 82% of patients (9 patients). Streptococcus viridans was detected in two patients, Streptococcus pneumoniae in two patients, Streptococcus spp. in two patients, Methicillin-sensitive coagulase negative staphylococci in one patient, Candida krusei in one patient, Bacteroides spp. in one patient. Abscesses of all patients were drained, incision-drainage was preferred in 10 patients, and needle aspiration was preferred in one patient. Tracheotomy was preferred in four (36%) patients to secure the airway. Five of the patients are smokers and have poor oral hygiene (45%). Etiology could be detected in four (36%) of the patients. Extension of the infected thyroglossal duct cyst to the base of the tongue in two of the patients, abscess formation 24 h after the coronavirus disease 2019 mRNA vaccine in one patient, and intravenous heroin addiction in one patient were detected. Hospitalization time ranged from 4 to 11 d, and the mean ± SD was 7.45 ± 2.29. Ampicillin-Sulbactam was given to 10 of our patients and Piperacillin-Tazobactam was given to 1 of our patients. No antibiotic revision was required in any of our patients. Antifungal treatment was also given to our patient who overgrown Candida krusei. Six of our patients (54%) used Amoxicillin-clavulanate before applying to the hospital. Pathology was sent to 10 of our patients, and cytology (a patient with needle aspiration) was sent in one of our patients. In all of the pathology results, an appearance compatible with chronic active inflammation and abscess was detected. In addition, dense actinomyces colonies were detected in one patient.
Three patients in group 1 had a history of additional diseases, one patient in group 2. There is no statistically significant difference between groups regarding the frequency of additional diseases (P = 0.545). There was no statistically significant difference between the groups in terms of WBC, NEU, LYMPH, PLT, NLR, PLR, CRP, ESR, and hospitalization time (P > 0.05 for all, respectively 0.361, 0.465, 0.584, 0.361, 0.855, 0.584, 0.273, 0.201, 0.08).
TA is a disease that is usually seen in immunocompromised people and is very rare in healthy individuals. TA is a rare clinical condition that is seen much less frequently than deep neck infections (DNIs), which are common diseases in otorhinolaryngology clinics.
Therefore, we believe that it is not correct to state the incidence for the disease. The tongue is resistant to infection with additional antimicrobial effect of the saliva. The differential diagnosis of tongue abscesses includes tumor, cyst, hematoma, hyperpituitarism, hypothyroidism, lingual thyroid, and ectopic lymphoid tissues. Generally, abscesses are unilateral and located in the anterior 2/3 of the tongue. Painful swelling, dysphagia, odynophagia, speech disorder, tongue pain - headache, high fever, dyspnea are among the symptoms[1,11]. There are 2 types of abscesses, superficial and deep. Deep abscesses of the tongue are observed in cases that go down to the muscle tissue planes. Patients present with more severe symptoms and a toxic appearance. Tracheotomy may be considered for patients with dyspnea CT, magnetic resonance imaging can be used in the diagnosis of patients. After the correct diagnosis, the safety of the airway, incision-drainage is important. Antibiotics treatments should cover streptococci, staphylococci and anaerobes. Since aspiration alone is an inadequate treatment method, it should not be preferred over drainage[2]. We preferred it in one of our patients because the abscess was located anteriorly and was small in size. To prevent complications, it is important for the clinician to take a decisive stance and act quickly if drainage and elective local tracheotomy are indicated.
In the literature, comorbidity was not observed in most patients, and the most common symptoms are painful tongue, odynophagia, and tongue swelling. Tracheotomy is performed in approximately one third of the patients[3]. Antoniades et al[12] reported two immunocompromised patients presenting with severe respiratory distress. And in two patients with severe immune problems, the predisposing factors were dental intervention and odontogenic infection. Palpation can be a valuable diagnostic tool in posterior lingual abscesses. Isolated medical treatment may be sufficient for abscesses < 1 cm. Only medical treatment works for subcentimetric abscess. Posterior lingual abscesses may result in sepsis, mediastinitis, and fatal airway obstruction[13]. Although rates for airway obstruction, sepsis, and mediastinitis are given for DNIs in the literature[11], unfortunately these cannot be stated clearly for TA. We think that airway obstruction and sepsis may be a bigger problem for TA. Because the tongue is a muscular organ, it does not have potential spaces and fascias like the neck, and therefore the increased abscess size will directly cause collapse in the upper airway. Another important situation is that the tongue base is one of the most important anatomical formations of swallowing and upper airway breathing. The size of the abscess between the vallecula and tongue base may cause direct passage collapse and make possible elective or semi-elective intubations impossible. It should not be forgotten that there is always the possibility of emergency tracheotomy in this patient group, and if the indication occurs, this situation can be dramatic for the patient and the doctor. We think that due to the high blood supply and arterial network of the tongue, it is more susceptible to septic microemboli and the rate and probability of leading to sepsis may be higher than DNIs. Our study, which included 11 consecutive patients, is the largest series in the literature. Contrary to the literature, posterior lingual abscess (54%) was observed more frequently in our study and appeared as swelling at the base of the tongue. It should not be forgotten that there may be tumoral lesions that occupy space in the differential diagnosis of the disease and contrast-enhanced imaging methods can always be preferred. Contrast-enhanced CT was performed in all of our abscess patients. Abscess sizes were found to be 22.9 mm on average. All patients had odynophagia and dysphagia. Additional disease was detected in four of our patients (36%). Incision-drainage was applied to all of our patients except one. In one of our patients, only puncture was performed. Tracheotomy was performed in 36% of our patients. Five of our patients were smokers and had poor oral hygiene. Human immunodeficiency virus (HIV) infection was present in one of our patients, DM in one, and intravenous heroin use in one caused immunosuppression. Although we cannot provide sufficient data on isolated medical treatment since we do not have an abscess < 1 cm, we think that incision-drainage would be appropriate because the tongue contains dense muscle tissue and may obstruct the airway. It is necessary not to be very conservative about tracheotomy in patients with tongue base localization, because sudden collapse will result in death. Poor oral hygiene and smoking were observed as a remarkable factor in tongue abscesses. Since it is an atypical disease, an infectious disease specialist should be asked about empirical antibiotics within the framework of a multidisciplinary approach and revised antibiotics based on the bacteriological result of the abscess content.
NLR was found useful in comparing two conditions that regressed with medical treatment, such as abscess requiring incision-drainage and microabscess-cellulitis[4]. NLR has been identified as a variable predicting hospitalization time in odontogenic head and neck infections[5]. CRP is elevated in case of infection and the half-life is between 5 and 7 h. WBC determines total WBC count, values > 10000 suggest infection. In inflammatory conditions, neutrophils usually increase while LYMPHs decrease. Therefore, NLR is a more reliable marker than the total leukocyte count in the evaluation of inflammation. NLR is a good marker especially in odontogenic infections[6]. PLR is a new inflammatory marker. In a study conducted with patients with DNI, NEU and PLR values differed between patient groups requiring and not requiring airway management. NEU and PLR were found to be statistically significantly higher in patients requiring airway management[7]. It has been stated that PLR is a parameter that can also be used in neonatal sepsis[8]. NLR, PLR are important biochemical markers shown to be increased in bacterial inflammation. NLR and PLR averages of group 1 were higher than group 2. The remarkable point in our study is that patients with intravenous heroin addiction (highest) and hypothyroidism had the highest values in terms of PLR. These two patients were ranked 2nd (hypothyroidism) and 3rd (intravenous heroin addict) in terms of NLR. In patients with TA, we may encounter low immune system and/or additional disease status with high PLR, NLR values. NLR and PLR are among the recent trending fields of study in otorhinolaryngology and are thought to be useful in predicting hospitalization time and bacterial inflammation status, especially in DNIs patients. In particular, the fact that NLR is a significant marker in odontogenic DNIs may be the subject of a new and original study with a large case series in the group of patients with TA who have predisposing factors of poor oral hygiene. Systemic additional diseases that cause immunosuppression and diseases that create an insidious clinical course, such as HIV, can cause serious problems in cases of TA. We routinely monitor hemogram, biochemical parameters and CRP in all our patients to whom we perform drainage and puncture, and request a preoperative serological marker for viral diseases such as hepatitis B, C and HIV, which are transmitted through blood and contact. Depending on the status of additional diseases, we take the advice of the relevant branch and treat this serious illness with a multidisciplinary approach.
TA is a very rare disease due to the anatomical and physiological structure of the tongue. The rarity of the disease can make it difficult to diagnose. Particular attention should be paid to airway obstruction, sepsis, and mediastinitis. Surgical drainage should be performed in abscesses larger than one centimeter.
Discussing the treatment methods and complications of this rare disease will contribute to science. Its rarity may make the disease difficult to diagnose and cause increased mortality.
The fact that our patient series has the highest number of patients in the English literature makes our study very valuable.
We aimed to discuss this very rare disease, which can be fatal, within the literature information. Because there is no algorithm or general information about its treatment.
We have eleven patients in our approximately three-year study, where patient data is complete.
Three anterior abscesses (27%), two lateral abscesses (18%) in group 1, six abscesses at the base of the tongue (54%) in group 2 were detected.
Surgical drainage of abscesses larger than one centimeter is inevitable and the clinician should be hurried as soon as the need for a tracheotomy occurs.
Poor oral hygiene and prevention of odontogenic diseases can prevent this fatal disease.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aseni P, Italy S-Editor: Wang JJ L-Editor: A P-Editor: Yu HG
| 1. | Mesfin T, Debele G, Seyoum K, Dadi S, Tsegaye M, Gomora D, Kene C, Tolosa G. Tongue Abscess: A Case Report. Int Med Case Rep J. 2022;15:769-772. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Mesolella M, Allosso S, Iorio B, Motta G. Clinical and Diagnostic Aspect of Tongue Abscess. Ear Nose Throat J. 2021;100:1012S-1014S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 3. | Srivanitchapoom C, Yata K. Lingual Abscess: Predisposing Factors, Pathophysiology, Clinical Manifestations, Diagnosis, and Management. Int J Otolaryngol. 2018;2018:4504270. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 4. | Ban MJ, Jung JY, Kim JW, Park KN, Lee SW, Koh YW, Park JH. A clinical prediction score to determine surgical drainage of deep neck infection: A retrospective case-control study. Int J Surg. 2018;52:131-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 5. | Słotwińska-Pawlaczyk A, Orzechowska-Wylęgała B, Latusek K, Roszkowska AM. Analysis of the Clinical Status and Treatment of Facial Cellulitis of Odontogenic Origin in Pediatric Patients. Int J Environ Res Public Health. 2023;20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 6. | Słotwińska-Pawlaczyk A, Orzechowska-Wylęgała B, Latusek K, Roszkowska AM. Analysis of Clinical Symptoms and Biochemical Parameters in Odontogenic Cellulitis of the Head and Neck Region in Children. Children (Basel). 2023;10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Lin Y, Gao W, Yue H, Chen W, Liu T, Ye J, Cai Q, Ye F, He L, Xie X, Xiong G, Wang B, Pang F, Li P, Wu J, Huang J, Wen W, Lei W. A novel risk score for the prediction of airway management in patients with deep neck space abscess: a multicenter retrospective cohort study. J Intensive Care. 2021;9:41. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Cansever M, Sari N. The association of allergic rhinitis severity with neutrophil-lymphocyte and platelet-lymphocyte ratio in children. North Clin Istanb. 2022;9:602-609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 9. | Oya R, Takenaka Y, Imai T, Sato T, Oshima K, Ohta Y, Inohara H. Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio as Prognostic Hematologic Markers of Bell's Palsy: A Meta-analysis. Otol Neurotol. 2019;40:681-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 10. | Durgut O, Gökgün ÖF, Gencay S. Evaluation of Neutrophil-to-Lymphocyte Ratio, Platelet-to-Lymphocyte Ratio and Mean Platelet Volume in Patients with Branchial Cleft Cyst. Indian J Otolaryngol Head Neck Surg. 2022;74:5465-5468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 11. | Bal KK, Unal M, Delialioglu N, Oztornaci RO, Ismi O, Vayisoglu Y. Diagnostic and therapeutic approaches in deep neck infections: an analysis of 74 consecutive patients. Braz J Otorhinolaryngol. 2022;88:511-522. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 12. | Antoniades K, Hadjipetrou L, Antoniades V, Antoniades D. Acute tongue abscess. Report of three cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;97:570-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |