Published online Oct 6, 2023. doi: 10.12998/wjcc.v11.i28.6857
Peer-review started: June 22, 2023
First decision: August 8, 2023
Revised: August 12, 2023
Accepted: September 4, 2023
Article in press: September 4, 2023
Published online: October 6, 2023
Processing time: 95 Days and 2.1 Hours
Neuropathy of the common peroneal nerve caused by compression by a fabella is an extremely rare form of compression neuropathy. Involving both the superficial and deep peroneal nerves, it usually manifests as either impaired sensation from the lower lateral leg to the top of the foot or drop foot, or as a combination of both.
We report the case of a 58-year-old Asian female who presented with inversion of the right foot during the stance phase of gait without sensory complaints related to the lower leg. Electrodiagnostic testing revealed the neuropathy of the common peroneal nerve at the level of the knee, exclusively affecting the muscular branch of the superficial peroneal nerve. A neuromuscular ultrasound disclosed swelling of the right common peroneal nerve just before it crossed over a large fabella as well as atrophy and fatty infiltration of the right peroneus longus and peroneus brevis muscles. Surgical excision of the fabella and neurolysis were performed. Subsequently, the strength of the right foot evertors improved, but the unsteady gait with occasional falls persisted for nine months after the surgery. Therefore, another procedure was performed to transfer the split posterior tibialis tendon to the peroneus brevis in order to correct the gait.
This is the first case of neuropathy of the common peroneal nerve caused by compression by a fabella affecting exclusively the muscular branch of the super
Core Tip: This is the first case of common peroneal nerve entrapment neuropathy caused by compression by a fabella affecting exclusively the muscular branch of the superficial peroneal nerve. Instead of features typically found in neuropathy of the common peroneal nerve, such as drop foot, steppage gait, and numbness in the anterolateral leg and the dorsum of the foot, the case reported here presented with inversion of the right foot during the stance phase of gait for every step taken without any sensory problems. Therefore, clinicians should be aware of this unusual peripheral neuropathy while evaluating and treating patients with gait disturbance.
- Citation: Lin JC, Tsai MH, Lin WP, Kuan TS, Lien WC. Entrapment neuropathy of common peroneal nerve by fabella: A case report. World J Clin Cases 2023; 11(28): 6857-6863
- URL: https://www.wjgnet.com/2307-8960/full/v11/i28/6857.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i28.6857
The most common type of peripheral neuropathy in the lower extremities is neuropathy of the common peroneal nerve[1,2]. The usual etiology includes compression due to either prolonged immobilization or a mass lesion like a ganglion cyst or a nerve sheath tumor, a repetitive strain injury, and a direct blow to the knee[1,2]. On the other hand, neuropathy of the common peroneal nerve caused by compression by a fabella is extremely rare[3]. Only 11 cases have been reported in the literature to date, all affecting either the superficial branch of the peroneal nerve alone or both its deep and superficial branches. We report the first case of neuropathy of the common peroneal nerve caused by compression by a fabella which preferentially affected the muscular branch of the superficial peroneal nerve.
A 58-year-old Asian female presented with a gait disturbance for six months.
The patient had progressive weakness in the eversion of the right foot and a gait disturbance which had lasted six months. There was no history of trauma. She denied having numbness, pain, or impaired sensation in the right lower extremity.
The patient had undergone pacemaker implantation surgery for sick sinus syndrome several years ago.
The patient denied any family history of peroneal neuropathy.
A physical examination disclosed severe atrophy of the lateral calf muscles and decreased evertor strength in the right foot, graded 1/5 on the Medical Research Council scale. It was noted that she walked with a wide-based gait and with inversion of the right foot during the stance phase of the gait cycle for every step taken. A sensory examination which tested for light touch, pinprick and proprioception sensation showed that sensation in the lower extremities was intact, and the patellar reflex and ankle jerk reflex tests for both legs were normal.
Routine blood analysis revealed the following: White blood cell count, 6.8 × 103/μL [reference range: (3.3-9.9) × 103/μL]; red blood cell count, 2.69 × 106/μL [reference range: (3.78-5.11) × 106/μL]; hemoglobin, 9.9 g/dL (reference range: 11.0-15.0 g/dL); and platelet count, 324 × 103/μL [reference range: (157-392) × 103/μL]. Liver function and kidney function were normal (serum creatinine, 0.77 mg/dL; epidermal growth factor receptor, 77; aspartate transaminase, 29 U/L; alanine aminotransferase, 26 U/L).
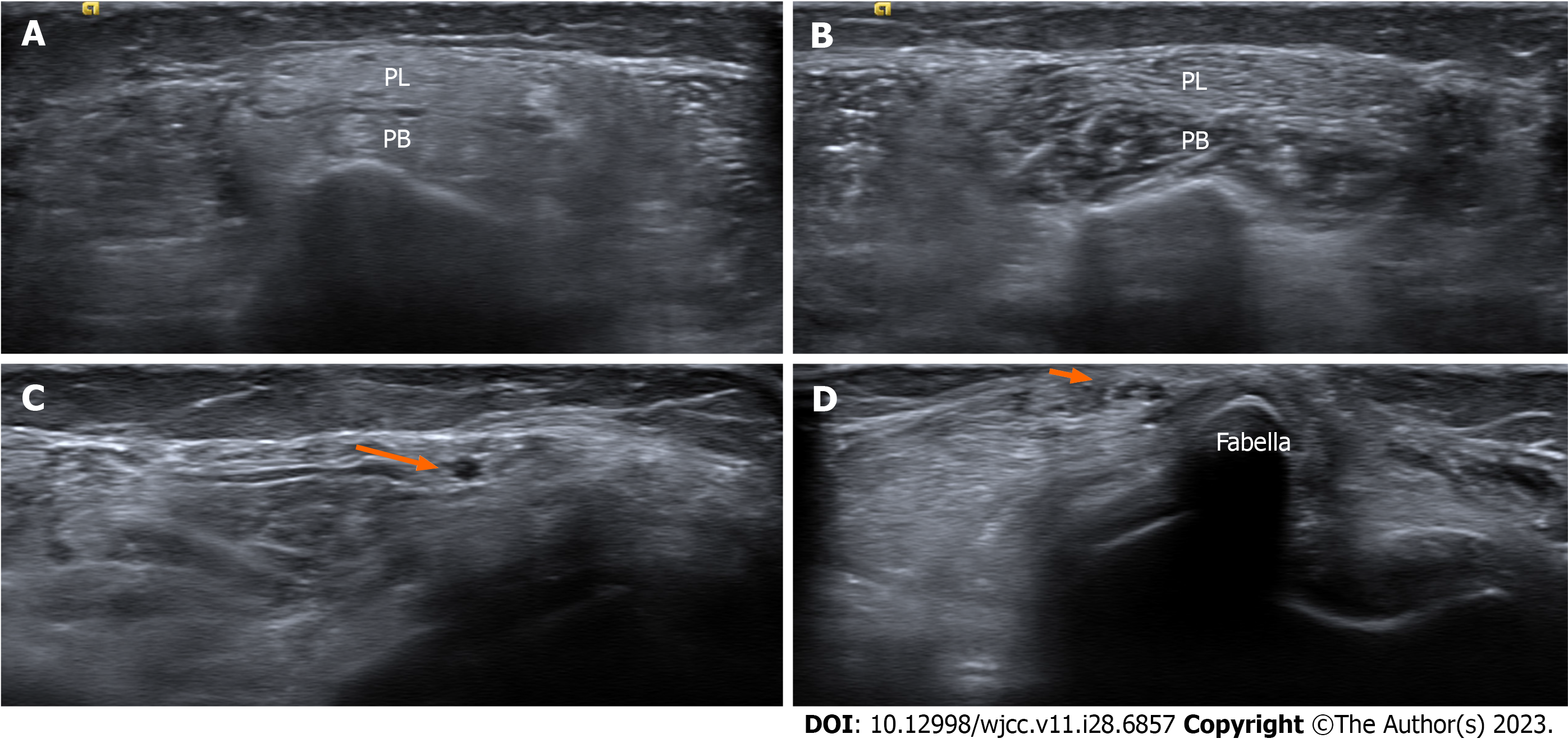
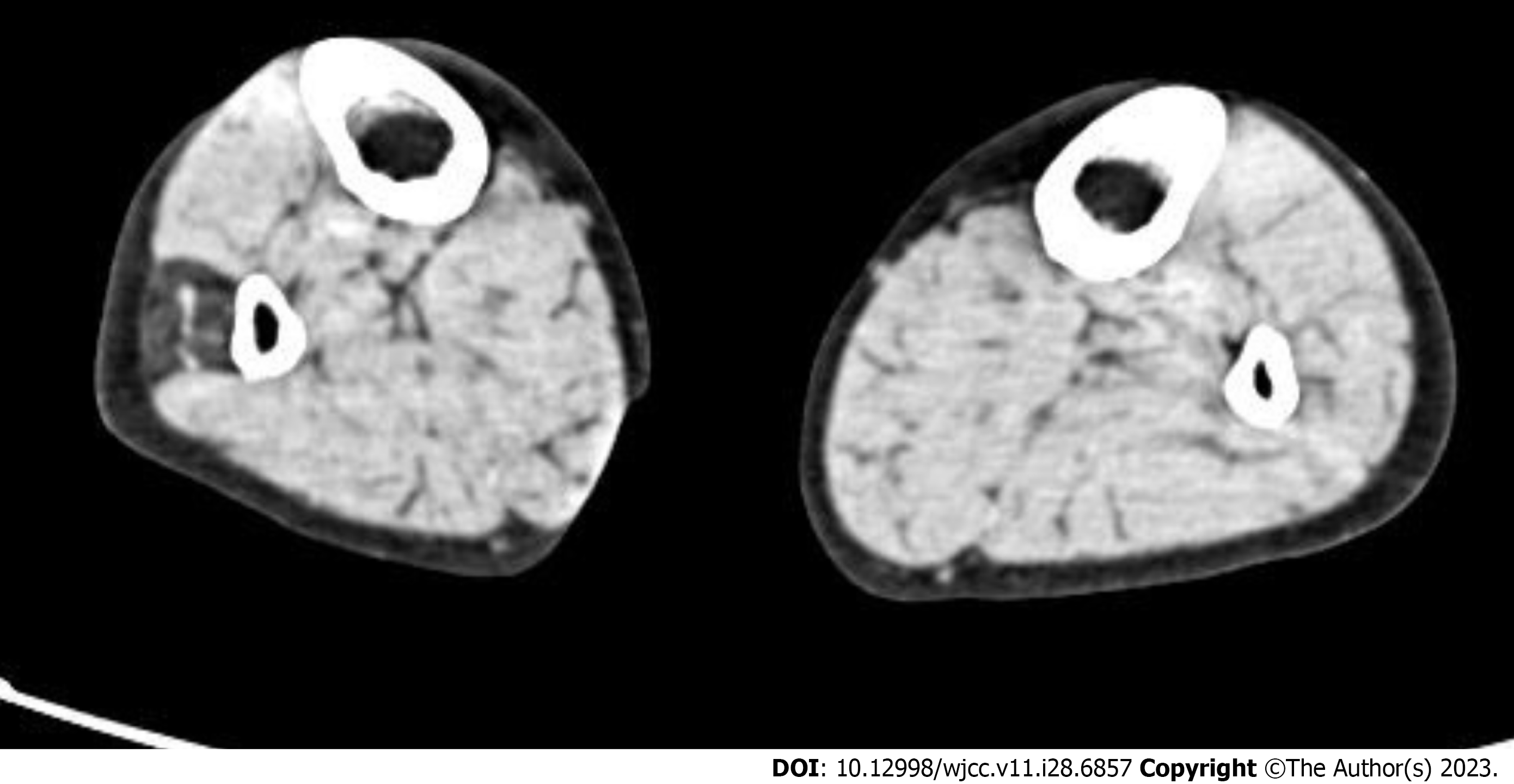
Electrodiagnostic (EDX) testing was performed with findings compatible with subacute neuropathy of the right common peroneal nerve at the level of the fibular head, preferentially affecting the muscular branch of the superficial peroneal nerve (Tables 1 and 2). A neuromuscular ultrasound revealed atrophy of the right peroneal longus and peroneal brevis muscles, graded 3/4 on the modified Heckmatt scale[4] (Figures 1A and B). Swelling of the right common peroneal nerve just proximal to an incidentally found fabella was also identified by means of ultrasound imaging (Figures 1C and D). Atrophy of the right peroneus longus and peroneus brevis muscles was also disclosed by means of a computed tomography scan of the lower extremities, with decreased muscle cross-sectional area and decreased radiodensity at the level of the mid-calf compared to the asymptomatic contralateral side (Figure 2).
| Nerve stimulated | Stimulation site | Recording site | Onset latency (ms) | Amplitude motor (mV), sensory (μV) | Velocity (m/s) | |||
| Right | Left | Right | Left | Right | Left | |||
| Motor studies | ||||||||
| Tibia | Ankle | AHB | 4.3 | 4.7 | 13.6 | 14.2 | ||
| Popliteal fossa | 12.7 | 13.6 | 8.9 | 9.4 | 47 | 44 | ||
| Peroneal | Ankle | EDB | 4.9 | 5.2 | 3.5 | 3.4 | ||
| Fibular head | 11.3 | 11.7 | 2.9 | 2.9 | 46 | 45 | ||
| Popliteal fossa | 13.4 | 13.8 | 2.4 | 2.7 | 49 | 47 | ||
| Peroneal | Fibular head | TA | 3.4 | 3.2 | 4.2 | 4.3 | ||
| Popliteal fossa | 4.6 | 4.5 | 4.0 | 3.9 | 54 | 50 | ||
| Peroneal | Fibular head | PL | 2.6 | 2.7 | 3.11 | 6.5 | ||
| Popliteal fossa | 6.3 | 4.4 | 1.11 | 5.9 | 221 | 47 | ||
| Sensory studies | ||||||||
| Sural | Calf | Posterior ankle | 3.4 | 3.5 | 14.7 | 15.6 | 42 | 40 |
| Superficial peroneal | Lateral calf | Ankle | 3.3 | 3.4 | 15.7 | 16.1 | 42 | 41 |
| Muscle | Spontaneous activity | Voluntary motor unit action potentials | ||||||
| Insertional activity | Fibrillation potentials | Positive sharp waves | Amplitude | Duration | Polyphasia | Recruitment | Interference pattern | |
| Right | ||||||||
| Vastus lateralis | NL | 0 | 0 | NL | NL | NL | NL | Full |
| Tibialis anterior | NL | 0 | 0 | NL | NL | NL | NL | Full |
| Peroneus longus | Increased | 2+ | 2+ | NL | NL | NL | Discrete | Incomplete |
| Peroneus brevis | Increased | 2+ | 2+ | NL | NL | NL | Discrete | Incomplete |
| Gastrocnemius | NL | 0 | 0 | NL | NL | NL | NL | Full |
| Left | ||||||||
| Tibialis anterior | NL | 0 | 0 | NL | NL | NL | NL | Full |
| Peroneus longus | NL | 0 | 0 | NL | NL | NL | NL | Full |
| Peroneus brevis | NL | 0 | 0 | NL | NL | NL | NL | Full |
Surgical excision of the fabella was performed through a dorsolateral incision between the biceps femoris muscle and the iliotibial band. The common peroneal nerve was isolated. The fabella was removed and measured 25 mm × 19 mm × 27 mm.
Combined with the patient’s medical history, the final diagnosis was common peroneal entrapment neuropathy by fabella which exclusively affects the muscular branch of superficial peroneal nerve.
Afterwards, a nine-month rehabilitation program was prescribed consisting of exercises for strengthening the right foot evertors and therapeutic electrical stimulation of the foot evertors. The evertor muscles in the right foot were partially strengthened, graded 3/5 on the Medical Research Council scale. However, the unsteady gait persisted with occasional falls while walking, presumably due to the inversion of the right ankle. Thus, another surgical procedure was carried out to transfer the split posterior tibialis tendon to the peroneus brevis.
Following a one-month postoperative rehabilitation program, the severity of the right ankle inversion while walking decreased, with no more falls reported on the last clinical visit two months after the surgery.
The fabella is a sesamoid bone or fibrocartilage embedded in the proximal tendon of the lateral head of the gastrocnemius muscle[5]. Although its actual function remains unclear, it has been suggested that it reinforces the structure of the posterior part of the knee, in particular the juncture of the fabellofibular ligament and oblique popliteal ligament, or that it lengthens the lever arm of the tendon of the lateral gastrocnemius muscle[3,5]. The fabella prevalence in humans is approximately 10%-30% with higher rates among Asian populations[6]. Overall, it occurs bilaterally in 70%-80% of cases[6].
Despite such a high prevalence, the presence of a fabella rarely causes compression neuropathy of the peroneal nerve[3]. In fact, with stringent diagnostic criteria which included EDX testing, only 11 cases have so far been reported in the literature (Table 3), with all cases accompanied by sensory impairment. Those whose motor functions were also affected had in common symptoms such as drop foot and active denervation potentials observed in the tibialis anterior by means of electromyography tests. Tinel’s sign could be elicited in around half of the cases. On the other hand, we report the first case of neuropathy of the common peroneal nerve caused by compression by a fabella which preferentially affected the muscular branch of superficial peroneal nerve.
| Ref. | Age | Gender | Symptom | Tinel sign | Fabella size | NCV | EMG | Treatment | Outcome |
| This case | 46 | Female | Inverted foot with evertors atrophy | + | 25 mm × 19 mm × 27 mm | Conduction block | AD and R-MUAP in PL, PB | Surgery | Partially resolved |
| Mangieri[7] | 46 | Female | Sensory impairment | + | 22 mm × 14 mm | Focal slowing | Normal | Surgery | Completely resolved |
| Takebe and Hirohata[6] | 49 | Male | Drop foot with sensory impairment | + | 9 mm × 7 mm × 6 mm | Focal slowing | AD and R-MUAP in TA, PL | Surgery | Slight functional disturbance |
| 34 | Male | Drop foot with sensory impairment | + | 11 mm × 9 mm × 7 mm | Focal slowing | AD and R-MUAP in TA, PL | Surgery | Completely resolved | |
| 36 | Male | Drop foot with sensory impairment | - | 10 mm × 10 mm × 8 mm | Focal slowing | AD, R-MUAP and polyphasia in TA, PL | Surgery | Completely resolved | |
| 53 | Male | Drop foot with sensory | - | 11 mm × 11 mm × 8 mm | Conduction block | R-MUAP in TA, PL | Conservative | Satisfactory improvement | |
| 40 | Male | Drop foot with sensory impairment | + | 8 mm × 8 mm × 6 mm | Focal slowing | AD in PL, R-MUAP in TA, PL | Conservative | Completely resolved | |
| 22 | Male | Drop foot with sensory impairment | - | 9 mm × 9 mm × 7 mm | Focal slowing | R-MUAP in TA, PL | Conservative | Completely resolved | |
| 25 | Male | Drop foot with sensory impairment | - | 7 mm × 5 mm × 4 mm | Focal slowing | AD in TA | Conservative | Satisfactory improvement | |
| Patel et al[3] | 67 | Male | Drop foot with sensory impairment | - | 23 mm × 20 mm | Focal slowing | Normal | Surgery | Completely resolved |
| Lee et al[8] | 79 | Female | Drop foot with sensory impairment | + | 16 mm × 20 mm × 15 mm | Conduction block | AD in TA | Surgery | Completely resolved |
| Kubota et al[9] | 50 | Female | Drop foot with sensory | - | 5 mm × 5 mm | Focal slowing | AD in TA, PL, EDL | Conservative | Partially resolved |
Our case had a unique clinical presentation. Instead of features typically found in neuropathy of the common peroneal nerve, such as drop foot, steppage gait, and numbness in the anterolateral leg and the dorsum of the foot, the case re
Previous studies have suggested such predisposing factors of peroneal neuropathy caused by a fabella as an enlarged fabella, a low body mass index, and an external force such as trauma[5,6]. Our case subject had a normal bodily shape without any history of trauma, but had a relatively large fabella (25 mm × 19 mm × 27 mm) compared with the average size reported in the literature (7.9 mm × 4.2 mm)[10]. It has been shown that the internal fascicular anatomy of the com
The treatment of choice for compression neuropathy by a fabella is surgical removal of the fabella and neurolysis[3]. In past research, the symptoms completely resolved in almost all of the cases who had undergone surgery, with a single exception which the author attributed to delayed surgical intervention (Table 3). For patients with results of EDX testing which are suggestive of neuropraxia, conservative treatment is an alternative approach which has also provided satis
Neuropathy of the common peroneal nerve caused by compression by a fabella is an extremely rare form of compression neuropathy. While drop foot and sensory impairment in the anterolateral lower leg and the dorsum of the foot are the most common clinical features, atypical presentations such as weakness of the lateral calf muscle are also possible. Cli
This research was supported in part by Higher Education Sprout Project, Ministry of Education to the Headquarters of University Advancement at National Cheng Kung University.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Papazafiropoulou A, Greece S-Editor: Wang JJ L-Editor: A P-Editor: Wang JJ
| 1. | Preston DC, Shapiro BE. Electromyography and Neuromuscular Disorders: Clinical-Electrophysiologic-Ultrasound Correlations. Philadelphia: Saunders, 2021. |
| 2. | Fortier LM, Markel M, Thomas BG, Sherman WF, Thomas BH, Kaye AD. An Update on Peroneal Nerve Entrapment and Neuropathy. Orthop Rev (Pavia). 2021;13:24937. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Patel A, Singh R, Johnson B, Smith A. Compression neuropathy of the common peroneal nerve by the fabella. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Moreta MC, Fleet A, Reebye R, McKernan G, Berger M, Farag J, Munin MC. Reliability and Validity of the Modified Heckmatt Scale in Evaluating Muscle Changes With Ultrasound in Spasticity. Arch Rehabil Res Clin Transl. 2020;2:100071. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Tabira Y, Saga T, Takahashi N, Watanabe K, Nakamura M, Yamaki K. Influence of a fabella in the gastrocnemius muscle on the common fibular nerve in Japanese subjects. Clin Anat. 2013;26:893-902. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Takebe K, Hirohata K. Peroneal nerve palsy due to fabella. Arch Orthop Trauma Surg (1978). 1981;99:91-95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Mangieri JV. Peroneal-nerve injury from an enlarged fabella. A case report. J Bone Joint Surg Am. 1973;55:395-397. [PubMed] |
| 8. | Lee YH, Wu CT, Wang YC, Chen IH. Common Peroneal Neuropathy Caused by the Fabella: Case Report and Literature Review. FJMD. 2019;10:74-78. [DOI] [Full Text] |
| 9. | Kubota Y, Toyoda Y, Kubota H, Kawai H, Yamamoto T. Common peroneal nerve palsy associated with the fabella syndrome. Anesthesiology. 1986;65:552-553. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Friedman AC, Naidich TP. The fabella sign: fabella displacement in synovial effusion and popliteal fossa masses. Normal and abnormal fabello-femoral and fabello-tibial distances. Radiology. 1978;127:113-121. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Lien WC, Ching CT, Lai ZW, Wang HD, Lin JS, Huang YC, Lin FH, Wang WF. Intelligent Fall-Risk Assessment Based on Gait Stability and Symmetry Among Older Adults Using Tri-Axial Accelerometry. Front Bioeng Biotechnol. 2022;10:887269. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 12. | Lien WC, Wang WM, Wang F, Wang JD. Savings of loss-of-life expectancy and lifetime medical costs from prevention of spinal cord injuries: analysis of nationwide data followed for 17 years. Inj Prev. 2021;27:567-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Lien WC, Chang JH, Guo NW, Lin YC, Hsieh PC, Kuan TS. Determinants of Perceived Physical Environment Barriers among Community-Dwelling Elderly in Taiwan. J Nutr Health Aging. 2015;19:575-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |