Published online Oct 6, 2023. doi: 10.12998/wjcc.v11.i28.6707
Peer-review started: July 6, 2023
First decision: July 27, 2023
Revised: August 9, 2023
Accepted: September 5, 2023
Article in press: September 5, 2023
Published online: October 6, 2023
Processing time: 81 Days and 2.2 Hours
Childhood asthma is a common respiratory ailment that significantly affects preschool children. Effective asthma management in this population is particularly challenging due to limited communication skills in children and the necessity for consistent involvement of a caregiver. With the rise of digital healthcare and the need for innovative interventions, Internet-based models can potentially offer relatively more efficient and patient-tailored care, especially in children.
To explore the impact of an intelligent Internet care model based on the child respiratory and asthma control test (TRACK) on asthma management in preschool children.
The study group comprised preschoolers, aged 5 years or younger, that visited the hospital's pediatric outpatient and emergency departments between January 2021 and January 2022. Total of 200 children were evenly and randomly divided into the observation and control groups. The control group received standard treatment in accordance with the 2016 Guidelines for Pediatric Bronchial Asthma and the Global Initiative on Asthma. In addition to above treatment, the observation group was introduced to an intelligent internet nursing model, emphasizing the TRACK scale. Key measures monitored over a six-month period included the frequency of asthma attack, emergency visits, pulmonary function parameters (FEV1, FEV1/FVC, and PEF), monthly TRACK scores, and the SF-12 quality of life assessment. Post-intervention asthma control rates were assessed at six-month follow-up.
The observation group had fewer asthma attacks and emergency room visits than the control group (P < 0.05). After six months of treatment, the children in both groups had higher FEV1, FEV1/FVC, and PEF (P < 0.05). Statistically significant differences were observed between the two groups (P < 0.05). For six months, children in the observation group had a higher monthly TRACK score than those in the control group (P < 0.05). The PCS and MCSSF-12 quality of life scores were relatively higher than those before the nursing period (P < 0.05). Furthermore, the groups showed statistically significant differences (P < 0.05). The asthma control rate was higher in the observation group than in the control group (P < 0.05).
TRACK based Intelligent Internet nursing model may reduce asthma attacks and emergency visits in asthmatic children, improve lung function, quality of life, and the TRACK score and asthma control rate. The effect of nursing was significant, allowing for development of an asthma management model.
Core Tip: Childhood asthma is a common respiratory disease that affects preschoolers. Asthma management in this population can be challenging due to limited communication and the need for involvement of a caregiver. This study explored the impact of an intelligent Internet care model based on the child respiratory and asthma control test (TRACK) on asthma management in preschoolers. Two hundred preschoolers were randomly divided into observation and control groups. The observation group received an intelligent Internet nursing model based on the TRACK scale. The results showed that the observation group had fewer asthma attacks and emergency visits, higher lung function, and better quality of life scores than the control group. Asthma control rate was also higher in the observation group in comparison to the control group. The present study suggests that a TRACK based intelligent internet nursing model can be an effective approach for asthma management in preschoolers.
- Citation: Pei CF, Zhang L, Xu XY, Qin Z, Liang HM. Research on the intelligent internet nursing model based on the child respiratory and asthma control test scale for asthma management of preschool children. World J Clin Cases 2023; 11(28): 6707-6714
- URL: https://www.wjgnet.com/2307-8960/full/v11/i28/6707.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i28.6707
Childhood asthma is a chronic disease that affects many children. Its prevalence and associated mortality are increasing worldwide, making the disease a global public health problem. According to an epidemiological survey, childhood asthma in China has increased by 50% annually over the past 10 years, with an incidence rate of 3%[1].
Recurring asthma episodes are a common reason for emergency treatment in children. The disease affects their physical and mental health as well as reduces their quality of life. In addition, families and society bear a great financial burden[2]. Despite tremendous advances in research on the mechanisms and treatment of asthma, the overall asthma control rate in children remains low, mainly because of limited awareness of asthma in some parents and children and a lack of comprehensive asthma care. Irregular medication usage and non-compliance with medical advice combined with negative family, social and psychological factors may also significantly impact the health of children with asthma[3]. The test for respiratory and asthma control in children (TRACK) is currently the only tool used worldwide for assessing asthma control levels in children aged 5 years or younger. Since its publication by Murphy et al[4] in the early twentieth century, its efficacy and reliability have been well demonstrated. The present study was primarily aimed at preschoolers, aged 5 years or younger, that had at least two episodes of wheezing, shortness of breath, or cough lasting longer than a day and that had been diagnosed with bronchiectasis or asthma. Medical staff and pharmacists jointly developed a personalized asthma management plan by consulting outpatient doctors and establishing an intelligent Internet information platform. The team guided the child's guardian in planning treatment and provided a basis for the family to manage childhood asthma. The study explored the effectiveness of a TRACK-based intelligent Internet nursing model for asthma management in preschoolers and aimed to provide a novel method for clinical asthma management in children.
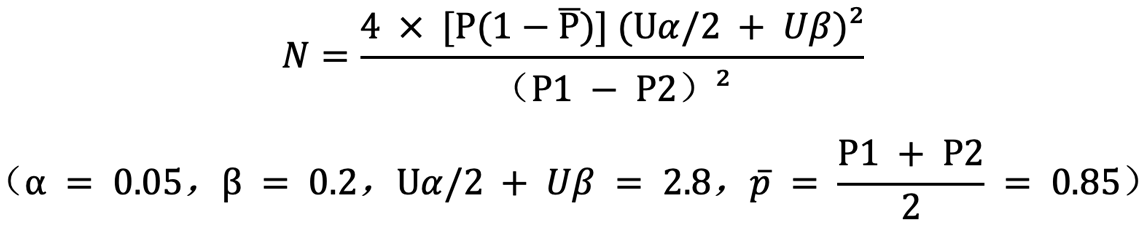
Preschoolers, aged 5 years or younger, that were treated in the hospital's pediatric outpatient clinics and emergency departments between January 2021 and January 2022 were selected as study participants. The inclusion criteria were: (1) The study participants that did not receive standardized family management and regular medication for treatment for asthma at the time of enrollment; (2) that could be prescribed with fluticasone propionate aerosol inhalation therapy; or (3) that had a guardian who could accompany them for the period of the research; or (4) that lived locally for a long time; or (5) that could be followed up for six months. The exclusion criteria were: (1) Children aged older than 5 years; (2) those that were allergic to therapeutic drugs or contraindications; (3) that had co-morbidities that affected the results of the pulmonary function test; or (4) that had guardians that were mentally or cognitively handicapped, therefore, showed poor compliance. The asthma control rates in domestic and tertiary hospitals are currently reported to be 80%. Therefore, a P1 of 80% (control rate of the control group) and P2 of 90% (control rate of the treatment group) were set. According to the formula for the total sample size, the random number table method was adopted as follows:
Control group: A dedicated WeChat account was established for the patient's family members. Treatment was performed according to the Guidelines for the Diagnosis and Prevention of Pediatric Bronchial Asthma, revised by the Respiratory Group of the Chinese Society of Pediatrics in 2016[5] and the Global Initiative on Asthma (GINA Program)[6]. The nurses explained the mechanism of the atomizer as well as the measures taken during inhalation. The pharmacists explained the proper usage of the drugs. Regular counseling and health education were provided. During the six months of the study, the TRACK scale was used to monthly assess and upload records. The nurses conducted telephone follow-ups, summarized the frequency of asthma attacks and emergency visits, and collected the results of pulmonary function tests before and after nursing.
Observation group: A dedicated asthma management WeChat account for each patient's family members was established. Based on the treatment of the control group, medical staff, and pharmacists provided online education and guidance, including knowledge related to childhood asthma, the importance of long-term family management, and methods for effectively controlling the family environment. The team assisted the family members in mastering medication, monitoring, and handling methods for acute attacks. In addition, the child was guided to breathe correctly and psychological comfort was provided. Similarly, the TRACK scale was used to evaluate and upload monthly records. Nurses conducted telephone follow-ups, summarized the frequency of asthma attacks and emergency visits, and collected the results of pulmonary function tests before and after nursing. The results were also observed for six months (Table 1).
| Group | Case | No. of asthma attacks (times) | No. of emergency visits (times) |
| Observation group | 100 | 2.85 ± 0.26 | 2.06 ± 0.27 |
| Control group | 100 | 3.62 ± 0.28 | 2.95 ± 0.34 |
| t value | 20.152 | 20.499 | |
| P value | 0.000 | 0.000 |
Various observational parameters analyzed in this study are as follows: (1) Total number of asthma attacks and emergency department visits for each child within six months in the two groups; (2) Forced expiratory volume in one second (FEV1) and the proportion of FEV1 to forced vital capacity (i.e., FEV1/FVC) and peak breath flow (PEF) before and after six months in both groups. These parameters were measured by using a pulmonary function instrument (Jaeger, Germany). Professional testing experts calibrated the parameters and assisted children with the recommended actions before each test. During testing, children were required to stand upright, keep their heads level, clamp their nose clips, and tightly wrap their lips to prevent air leakage. The collar was loosened to avoid interference with the test findings. The number of tests was determined based on the actual situation, with the best value as the final test result; (3) Within six months of care, a TRACK score was obtained for each child for each month and combined with clinical symptoms to determine the condition. The nurses followed up by telephone calls. The nurses were advised to seek medical attention promptly if any discomfort was observed. The TRACK scale is an evaluation tool for the control of childhood asthma developed by the American scholar Murphy[7]. It is currently the only tool to evaluate the level of asthma control in children aged less than five years as well as the first evaluation tool that includes damage and risk. The guardians were required to answer five questions on the questionnaire. Each question has five options, with scores of 20, 15, 10, 5, and 0, resulting in a total score of 100. A score of less than 80 after the addition of scores of the five options indicates that breathing problems may not be controlled, whereas a score greater than 80 indicates that respiratory problems are under control; (4) The SF-12 Life quality, which consists of 12 items and eight dimensions divided into two parts i.e., physical health (PCS) and mental health (MCS), was evaluated before and after six months of nursing[8]. PCS included physical role (RP), bodily pain (BP), and general health (GH) while MCS included vitality (VT), social functioning (SF), mental health (MH), and role-emotional (RE). Each dimension was converted according to the formula, with a total score of 0–100 with average normalized to 50 and a standard deviation of 10. BP, GH, VT, and MH were scored in reverse, with the total score being the sum of the scores for each dimension. Higher scores indicate better health; and (5) Six months after the intervention, children returned to the hospital to assess asthma control rates[9] (Table 2). No activity restrictions, asthma attacks, or the need for emergency medicine in the past four weeks was collectively designated as control. Partial control was defined as when activity was unrestricted, daytime asthma attacks were less than once per week with occasional attacks at night, and no emergency medication was used in the past four weeks while uncontrolled was defined as those who failed to meet the above standards. The control rate was calculated as given below: Control rate = (number of control cases/total number of cases) × 100.
| Group | Case | FEV1 (%) | FEV1/FVC (%) | PEF (L/s) | |||
| Before nursing | Nursing for six-month | Before nursing | Nursing for six-month | Before nursing | Nursing for six-month | ||
| Observation group | 100 | 97.03 ± 10.03 | 113.69 ± 11.14a | 86.22 ± 10.03 | 94.22 ± 11.37a | 3.62 ± 0.24 | 5.79 ± 0.24a |
| Control group | 100 | 97.12 ± 10.08 | 102.22 ± 12.14a | 86.13 ± 10.16 | 90.37 ± 11.18a | 3.63 ± 0.19 | 4.35 ± 0.28a |
| t value | 0.063 | 6.961 | 0.063 | 2.414 | 0.327 | 39.047 | |
| P value | 0.950 | 0.000 | 0.950 | 0.020 | 0.740 | 0.000 | |
Statistical analysis was performed using SPSS19.0 statistical software. First, the measured data were checked for normality. When variance was homogeneous and distribution was normal, data was expressed as mean ± SD, and within-group differences were compared with a t-test. When the data was non-normal and did not conform to the homogeneity of variance, data was expressed as median, and differences within groups were compared with a rank sum test. Counting data was described using the rate and chi-square test was performed, with a significance level of P < 0.05.
As shown in Table 1, the number of asthma attacks and emergency visits within six-month in the observation group was lower than that in the control group (P < 0.05).
As shown in Table 2, after six-month of nursing care, the levels of lung function indicators such as FEV1, FEV1/FVC, and PEF of children in both groups were higher than that before nursing care (P < 0.05). The difference is statistically significant (P < 0.05).
As shown in Table 3, the monthly TRACK scores of the observation group were higher than those of the control group for six-month.
| Group | Case | 1st month of nursing | 2nd month of nursing | 3rd month of nursing | 4th month of nursing | 5th month of nursing | 6th month of nursing |
| Observation group | 100 | 60.29 ± 8.22 | 66.18 ± 8.19 | 76.23 ± 9.12 | 78.19 ± 9.27 | 80.17 ± 9.06 | 82.29 ± 8.17 |
| Control group | 100 | 57.37 ± 7.27 | 60.27 ± 8.26 | 70.26 ± 9.07 | 75.37 ± 9.17 | 77.22 ± 9.12 | 79.07 ± 8.15 |
| t value | 2.661 | 5.081 | 4.641 | 51.521 | 2.295 | 2.790 | |
| P value | 0.010 | 0.000 | 0.000 | 0.000 | 0.020 | 0.010 |
As shown in Table 4, after six-month of nursing care, the life quality scores of PCS and MCSSF-12 of children in both groups were higher than that before nursing care (P < 0.05). The difference is statistically significant (P < 0.05).
As shown in Table 5, the asthma control rate of the observation group was higher than that of the control group (P < 0.05).
| Group | Case | Control (cases) | Partial control (cases) | Uncontrolled (cases) | Control rate (%) |
| Observation group | 100 | 39 | 58 | 3 | 39.00 |
| Control group | 100 | 25 | 56 | 19 | 25.00 |
| χ2 | 3.880 | ||||
| P value | 0.049 |
Asthma management in young children is relatively difficult because of their sensitivity to infection and other triggers such as poor treatment compliance, and limited lung function testing[10]. Studies have shown that the vast majority of asthma cases begin before the age of 3 years. Impaired lung function usually starts in children before the age of 6. Therefore, it is necessary to identify and effectively intervene for children, with asthma aged less than six years, who exhibit wheezing symptoms[11]. According to the “Global Initiative on Asthma”, managing asthma is difficult in the initial five years of life because diagnosing asthma in young children is challenging. Moreover, children's self-control is poor, and most asthma control level assessment tools are inappropriate for children under five, resulting in few clinical reports[12]. In this study, asthma was diagnosed based on observations, consultations, and related examination results. The children's caregivers were educated by nurses and pharmacists about their health and then advised by Internet Intelligence. Nurses advised parents to follow their WeChat account for asthma control i.e., scan the WeChat code, register a file, and record the results in Microsoft Excel. Follow-up through telephone as well as WeChat consultations were taken up for children in the control group. After obtaining the guardians' written consent, household atomizers were distributed and all children were followed up for six months.
This study compared the application of a TRACK-based intelligent Internet nursing model with a traditional nursing model in preschoolers. The number of asthma attacks and emergency visits decreased significantly after six months of asthma management in the observation group. This result suggests that the TRACK-based intelligent Internet nursing model helps control asthma, improve breathing, and reduce acute attacks in preschoolers. This may be owing to nurses using the Internet to remind children and caregivers to document their daily asthma, medication status, and need for emergency medications once preschoolers apply the TRACK-based smart nursing model via the Internet. To help children and their caregivers manage asthma more effectively and change treatment plans promptly, asthma-related knowledge and preventive measures were shared daily, children's condition was analyzed based on TRACK scores, and appropriate treatment plans were made[13]. After six months of intervention, preschoolers' PCSs and MCSs were higher for those that were cared for using the TRACK-based intelligent Internet care model in comparison to the traditional care model. An Internet-based intelligent nursing model, based on the TRACK scale, may help improve the quality of life of preschoolers suffering from asthma. Using the TRACK scale, the present study demonstrated better lung function and asthma control for the observation group in comparison to the control group after six months of Internet-based intelligent nursing. It has been proven TRACK based intelligent Internet nursing could improve the management of asthma, shorten the course of the disease, reduce attacks, and improve the quality of life. Children become extremely reliant on their caregivers after experiencing asthma. They require guardians to provide basic care and disease management. However, single management finds it difficult to successfully implement relevant medical orders. TRACK-based intelligent Internet nursing can incorporate doctors' advice into family chronic disease management using the Internet[14]. As for time, the scale TRACK has difficulty using systemic corticosteroids or high-dose inhaled corticosteroids within one year[15]. Although the other four items were all 100 points during the 6-month follow-up period, the TRACK score never reached 100 points. The TRACK scale scores were recorded once every month for six months to guide treatment. This implies that doctors and guardians need to pay particular attention to these children as they may be at risk of recurrent asthma attacks. The range of TRACK scores, obtained in this study, is helpful for quickly determining clinical conditions and asthma control levels. The current results show that the TRACK scores of the children in the observation group were higher than those of the control group within six months (P < 0.05). Intelligent Internet nursing based on the TRACK scale can better manage asthma in preschoolers. Therefore, it is difficult for guardians to judge the level of asthma control. While the TRACK score is used for family management, guardians can learn about the child's illness using real data. Objectively assessing the level of asthma control, assisting guardians in precisely understanding the disease, standardizing medications to control the condition, and increasing the implementation rate of household nebulization will consequently enhance the asthma control rate[16].
This study on a TRACK-based intelligent Internet nursing model for preschoolers with asthma has several limitations. First, it was limited to a single institution, limiting its generalization to other hospitals. Second, the reliance on guardians for accurately reporting on the TRACK scale might have introduced bias. Additionally, the six-month follow-up period did not reflect long-term study effects. Furthermore, the study did not consider factors such as asthma severity at baseline or exposure to environmental triggers. Also, the control group's use of a traditional nursing model without technological components may not represent current practices in many institutions, and further research in diverse settings and over extended periods is recommended to validate and expand our findings.
In conclusion, the TRACK-based intelligent Internet care model could reduce the number of asthma attacks and emergency visits in asthmatic preschoolers, improve lung function, quality of life, increase the TRACK score and asthma control rate, and have significant care effects. Therefore, it is worthwhile to develop and apply asthma management models.
Childhood asthma is a common respiratory illness that significantly affects preschoolers. Managing asthma in this demographic is challenging because of the limited communication abilities and the need for continuous caregiver involvement. The advent of digital healthcare tools has enabled the potential use of Internet-based models to deliver more efficient and personalized care to young patients with asthma.
Childhood asthma presents significant challenges for effective management, especially among preschoolers with limited communication skills and reliance on caregivers. With the advancement in digital healthcare tools and the need for innovative interventions, there is a motivation to explore Internet-based models for more efficient and personalized care of young patients with asthma.
This study explored the impact of an intelligent Internet care model, based on the child respiratory and asthma control test (TRACK), on asthma management in preschoolers. By leveraging Internet-based models and innovative interventions, tailored and efficient care may be provided to young patients with asthma.
This study enrolled preschoolers, below five years of age, that attended the pediatric outpatient and emergency departments of a hospital between January 2021 and January 2022. A total of 200 children were randomly divided into observation and control groups. The control group received standard treatment, whereas the observation group was introduced to an intelligent Internet nursing model that focused on the TRACK scale.
The results showed that the observation group, treated with the intelligent Internet nursing model, experienced fewer asthma attacks and emergency department visits than the control group. Moreover, both groups exhibited improved lung function after six months of treatment.
This study revealed a new finding: The TRACK-based intelligent Internet nursing model offers significant benefits in asthma management for preschoolers. This study provides an appropriate summary of current knowledge and offers implications for future clinical practice, highlighting that the use of this Internet-based model could enhance asthma management.
The experiences and lessons learned from this study indicate the potential of a TRACK-based intelligent Internet care model for asthma management in preschoolers. Future directions include conducting long-term follow-up studies to assess the sustainability and durability of the observed effects and exploring the cost-effectiveness and feasibility of implementing the model in various healthcare settings.
We express our sincere gratitude to all individuals and organizations that contributed to the successful completion of this research project. First, we extend our deepest appreciation to the preschoolers and their families that participated in the study. Their willingness to participate in this study was instrumental in advancing our understanding of asthma management among preschool-aged children. We thank the healthcare professionals and staff of (Shanghai Jiao Tong University School of Medicine Affiliated First People's Hospital) for their support and assistance throughout the data collection process. Their expertise and dedication significantly contributed to the accuracy and reliability of the findings. We are also grateful for the financial support provided by First People's Hospital Affiliated with the School of Medicine of Shanghai Jiao Tong University. Their investment in this study made it possible to collect, analyze, and disseminate the necessary data. Further, we acknowledge the valuable contributions of the members of our research team who worked tirelessly to ensure the smooth execution of this project. Their commitment, expertise, and collaborative spirit are invaluable. Finally, we express our deep appreciation to the authors of the studies and publications referenced in this research. Their groundbreaking work and findings served as the basis for our study and enriched our understanding of the treatment of asthma in children. Thank you for your contribution and support, which were vital for the successful completion of this research project.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Nursing
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Leung PCK, Canada; Mastoraki A, Greece S-Editor: Yan JP L-Editor: A P-Editor: Zhang XD
| 1. | Yildiz Y, Yavuz AY. Complementary and alternative medicine use in children with asthma. Complement Ther Clin Pract. 2021;43:101353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 2. | Ardura-Garcia C, Stolbrink M, Zaidi S, Cooper PJ, Blakey JD. Predictors of repeated acute hospital attendance for asthma in children: A systematic review and meta-analysis. Pediatr Pulmonol. 2018;53:1179-1192. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 36] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 3. | Shipp CL, Gergen PJ, Gern JE, Matsui EC, Guilbert TW. Asthma Management in Children. J Allergy Clin Immunol Pract. 2023;11:9-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 19] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 4. | Leiria-Pinto P, Marques J, Finelli E, Alves C, Alves M, Trincão D, Pinto N, Carreiro-Martins P, Papoila AL, Neuparth N. Cross-cultural validation of the Portuguese from Portugal version of the Test for Respiratory and Asthma Control in Kids (TRACK) questionnaire. Eur Ann Allergy Clin Immunol. 2021;53:214-220. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 5. | Subspecialty Group of Respiratory Diseases; Society of Pediatrics; Chinese Medical Association; Editorial Board, Chinese Journal of Pediatrics. [Guideline for the diagnosis and optimal management of asthma in children(2016)]. Zhonghua Er Ke Za Zhi. 2016;54:167-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 69] [Reference Citation Analysis (0)] |
| 6. | Boulet LP, Reddel HK, Bateman E, Pedersen S, FitzGerald JM, O'Byrne PM. The Global Initiative for Asthma (GINA): 25 years later. Eur Respir J. 2019;54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 165] [Article Influence: 27.5] [Reference Citation Analysis (0)] |
| 7. | Liu L, Zhang J, Zhang L, Yuan SH, Wu JH, Tang MY, Chen JD, Zhang F, Qi XY, Yin Y. The Relationship of the Test for Respiratory and Asthma Control in Kids Initial Score on the Prognosis of Pre-school Children With Asthma: A Prospective Cohort Study. Front Pediatr. 2021;9:690333. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 8. | Holder RL, Winter MA, Greenlee JL, Robinson A, Dempster KW, Everhart RS. Racial regard and physical health among low-income black caregivers of children with and without asthma. J Black Psychol. 2022;48:631-644. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Pennington AF, Hsu J, Sircar K, Mirabelli MC, Zahran HS. Daycare attendance and asthma control, Asthma Call-back Survey 2012-2014. J Asthma. 2021;58:1111-1117. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Pedersen SE, Hurd SS, Lemanske RF Jr, Becker A, Zar HJ, Sly PD, Soto-Quiroz M, Wong G, Bateman ED; Global Initiative for Asthma. Global strategy for the diagnosis and management of asthma in children 5 years and younger. Pediatr Pulmonol. 2011;46:1-17. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 166] [Cited by in RCA: 188] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 11. | Gaillard EA, Moeller A. Evidence-based European guidelines for the diagnosis of asthma in children aged 5-16 years. Lancet Respir Med. 2021;9:558-560. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Polavarapu M, Klonoff-Cohen H. Serum ECP as a diagnostic marker for asthma in children less than 5 years: A systematic review and meta-analysis. Pediatr Pulmonol. 2020;55:3243-3251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Kellerer C, Schultz K, Linde K, Kohler B, Hapfelmeier A, Schneider A. Implementation of an internet-based asthma patient education program in primary care: results of a single-arm trial. J Asthma. 2023;60:195-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 14. | Chan DS, Callahan CW, Hatch-Pigott VB, Lawless A, Proffitt HL, Manning NE, Schweikert M, Malone FJ. Internet-based home monitoring and education of children with asthma is comparable to ideal office-based care: results of a 1-year asthma in-home monitoring trial. Pediatrics. 2007;119:569-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 124] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 15. | Boulet LP, Gupta S, FitzGerald JM. Inhaled Glucocorticoids in Asthma. N Engl J Med. 2018;378:2050-2051. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Lu MA, Eckmann T, Ruvalcaba E, McQuaid EL, Rand CS, Riekert KA, Eakin MN. Family management of asthma in Head Start preschool children. Ann Allergy Asthma Immunol. 2022;128:178-183. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |








