Published online Sep 6, 2023. doi: 10.12998/wjcc.v11.i25.5941
Peer-review started: May 2, 2023
First decision: July 3, 2023
Revised: July 14, 2023
Accepted: August 9, 2023
Article in press: August 9, 2023
Published online: September 6, 2023
Processing time: 121 Days and 19.5 Hours
Neuropathy may occur at some sites after catheterization for close examination of cardiac disease. Although the radial artery is considered a relatively uncom-plicated site for catheterization, the radial artery and median nerve are in relatively close proximity, with the risk of median nerve injury depending on the angle of puncture. The purpose of this study was to report the outcomes of surgery performed for conservative therapy-resistant median neuropathy following forearm catheterization.
A 50-year-old woman experienced palsy from the right thumb to the radial side of the ring finger after catheterization from the radial artery of the right forearm. Paresthesia developed at the same site and a positive tinel-like sign was seen for the median nerve area at the high level of the puncture site. Nerve conduction study showed reduced compound muscle action potentials and loss of sensory nerve action potentials. Symptoms did not improve despite pharmacotherapy and the patient gradually developed flexion restrictions of the index and middle fingers. Median nerve injury and associated flexor tendon adhesion was diagnosed, and the patient was referred for surgery at 3 mo after injury. When the same area was opened, no injury to the median nerve epithelium was obvious, but the area of the positive tinel-like sign was highly adherent to surrounding tissue and to the flexor digitorum superficialis of the index and middle fingers. The surgery was terminated with adequate adhesion release. Rehabilitation was initiated postoperatively, improving neurological symptoms and range of motion of the fingers. Six months after surgery, the patient returned to daily activities without discomfort.
This case provides the appropriate diagnosis and treatment for a suspected peripheral nerve injury.
Core Tip: Median neuropathy during forearm puncture is unlikely but possible given the anatomic location. In general, peripheral neuropathy of the upper extremity causes difficulty in performing hand-operated tasks and daily living, leading to a decreased quality of life, so surgery is aggressively considered in cases that are resistant to conservative treatment. Even in examinations where the risk of complications is considered low, accurate diagnosis based on clinical symptoms is important to provide appropriate treatment.
- Citation: Suzuki T, Matsui Y, Momma D, Endo T, Iwasaki N. Median neuropathy after multiple punctures of the forearm for catheterization: A case report. World J Clin Cases 2023; 11(25): 5941-5946
- URL: https://www.wjgnet.com/2307-8960/full/v11/i25/5941.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i25.5941
The radial artery is the most common site for arterial catheters, and radial artery catheters are considered relatively safe. The incidence of serious complications of radial artery catheterization is less than 0.2%[1]. One potential complication is nerve injury[2], most often in the form of median neuropathy at the forearm level. Median nerve injury related to radial artery catheterization has been reported to be caused by prolonged dorsiflexion of the wrist joint[3] and increased intra-carpal pressure due to hematoma formation[4,5], but the possibility of direct injury cannot be ruled out. We report a case of median nerve injury diagnosed and operated on after radial artery catheterization.
A 50-year-old woman underwent coronary angiography from the radial artery of the right forearm. When the artery was punctured with a 22-G needle, the patient reported a burning sensation in the right hand, and multiple punctures were made without injecting any drug. Coronary artery bypass grafting was performed the same day under a diagnosis of unstable angina pectoris.
After the patient noticed a burning sensation in the right hand during the initial forearm puncture, anesthesia was induced in emergency surgery. After waking from anesthesia, she perceived paresthesia from the thumb to the radial side of the ring finger and difficulty moving the right hand. Medical treatment with drugs was started but obtained little improvement in symptoms, and the difficulty in bending the index finger gradually worsened.
Unstable angina pectoris.
Non-contributory.
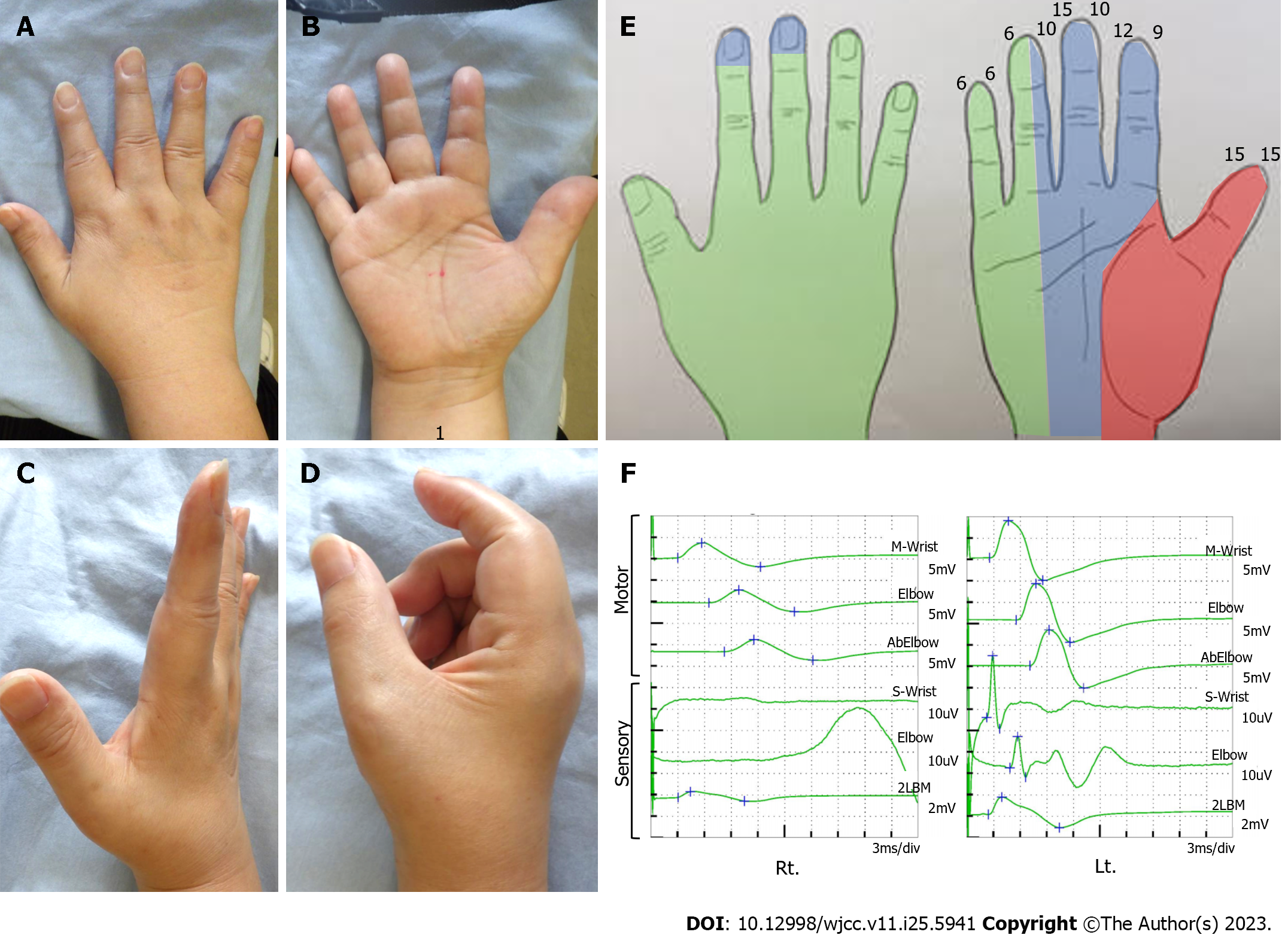
There was decreased perception of the phalanx and from the thumb to radial side of the ring finger as compared to the other side. Manual muscle testing of the abductor pollicis brevis (APB) had dropped to 4. Range of motion of the wrist joint was preserved, but flexion of the metacarpophalangeal and proximal interphalangeal joints of the index and middle fingers was limited (Figure 1), and a complete O could not be made. A positive tinel-like sign was seen for the two proximal lateral digits from the wrist crease and negative at the carpal tunnel. In peripheral nerve conduction studies (NCS), motor and sensory latencies at the wrists did not differ between left and right. Compound muscle action potential (CMAP) of the APB was reduced and no waveform was recorded for sensory nerve action potential (SNAP) of the right second finger (Figure 1). Ultrasonography and magnetic resonance imaging did not show any median nerve swelling or hematoma formation.
No special abnormal findings.
No special abnormal findings.
The patient was finally diagnosed with median nerve injury and flexor digitorum superficialis (FDS) adhesion of the index and middle fingers.
Three months of conservative treatment with medication failed to improve the condition, so surgery was performed.
A skin incision was made from the proximal median of the palm to the distal median forearm. The median nerve was dissected circumferentially at the proximal level of the second transverse digit of the wrist crease, with erythema of the epineurium and adhesions to fatty tissue and tendons (palmaris longus and FDS for the second and third digits). The carpal tunnel was also released. The wound was closed under microscopy to ensure that there was no obvious injury or defect in the epineural membrane (Figure 2). No external fixation was performed and rehabilitation for hand exercises and prevention of adhesions was started on the third postoperative day.
Improvement of palsy was observed from the day after surgery. Hand movement improved gradually, with full grip possible 2 wk after surgery. The NCS waveform of SNAP (3.3 μV), which could not be confirmed preoperatively, was confirmed at 3 mo postoperatively (Figure 3). By 6 mo postoperatively, decreased perception was localized only to the phalanges of the index and middle fingers and disability of arm, shoulder and hand score had improved from 62.1 preoperatively to 15.5.
A detailed history and thorough clinical examination are the foundations of diagnosing nerve injuries. Electrodiagnostic studies are also commonly performed as an aid to diagnosis. This modality provides important information for identifying the site of compression and neuropathy, determining severity and prognosis, and allowing the identification of relevant phenomena such as denervation, reinnervation, abnormal reinnervation, and motor plate lesions[6,7]. In nerve palsy, stimulation of the nerve proximal to the lesion with distal recording results in loss of CMAP amplitude, partial or complete conduction block, and reduced conduction velocity across the lesion. SNAP is also lost or reduced in amplitude with proximal stimulation, with a 50%-70% reduction in amplitude suggesting conduction block[8]. These changes show complete or partial resolution once remyelination has been completed[9]. The present case showed reduced CMAP amplitude and loss of SNAP, suggesting conduction block due to axonal injury or nerve adhesions. Intraoperative findings were anatomically consistent with the predominance of dysesthesia in this case, since the sensory fibers in the distal forearm run mainly on the radial side of the median nerve[10,11].
Several peripheral neuropathies have been associated with vascular punctures related to venipuncture, with frequencies below 0.0001%[12-15]. Of particular significance is that half of the nerve injuries related to venipuncture improved within 5 wk, and all injuries improved within 18 wk[12]. The lack of spontaneous improvement in this case may have been related to the size of the puncture needle and the surface area of the injured nerve. External denervation has been reported to be effective for peripheral nerve injuries resistant to conservative therapy[16-18], and the same principle was applied in this case. The preoperative findings led to a diagnosis of median nerve injury, and the median nerve did in fact show marked adhesions at the site of the positive tinel-like sign. The coexisting flexion limitations of the index and middle fingers in this patient also completely resolved with adhesion release and postoperative rehabilitation. As of 6 mo postoperatively, neurological symptoms remained mild, but the patient had full use of the hand without any problems in daily life, much to her satisfaction.
This case provides insights into the appropriate diagnosis and treatment of suspected peripheral nerve injury. A thorough understanding of the nerve, tendon, and vascular anatomies is important and aggressive performance of surgery may be warranted for neuropathies that prove resistant to conservative therapy.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bernardes A, Portugal; Papazafiropoulou A, Greece S-Editor: Qu XL L-Editor: A P-Editor: Chen YX
| 1. | Wallach SG. Cannulation injury of the radial artery: diagnosis and treatment algorithm. Am J Crit Care. 2004;13:315-319. [PubMed] |
| 2. | Brzezinski M, Luisetti T, London MJ. Radial artery cannulation: a comprehensive review of recent anatomic and physiologic investigations. Anesth Analg. 2009;109:1763-1781. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 202] [Cited by in RCA: 221] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 3. | Chowet AL, Lopez JR, Brock-Utne JG, Jaffe RA. Wrist hyperextension leads to median nerve conduction block: implications for intra-arterial catheter placement. Anesthesiology. 2004;100:287-291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Kokosis G, Blueschke G, Blanton M, Levinson H, Erdmann D. Acute carpal tunnel syndrome secondary to iatrogenic hemorrhage. A case report. Hand (N Y). 2011;6:206-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Lazaro RP. Complex regional pain syndrome and acute carpal tunnel syndrome following radial artery cannulation: a neurological perspective and review of the literature. Medicine (Baltimore). 2015;94:e422. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Domkundwar S, Autkar G, Khadilkar SV, Virarkar M. Ultrasound and EMG-NCV study (electromyography and nerve conduction velocity) correlation in diagnosis of nerve pathologies. J Ultrasound. 2017;20:111-122. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | Aminoff MJ. Electrophysiologic testing for the diagnosis of peripheral nerve injuries. Anesthesiology. 2004;100:1298-1303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Kimura J, Machida M, Ishida T, Yamada T, Rodnitzky RL, Kudo Y, Suzuki S. Relation between size of compound sensory or muscle action potentials, and length of nerve segment. Neurology. 1986;36:647-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 77] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 9. | Campbell WW. Evaluation and management of peripheral nerve injury. Clin Neurophysiol. 2008;119:1951-1965. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 431] [Cited by in RCA: 472] [Article Influence: 27.8] [Reference Citation Analysis (0)] |
| 10. | Tamura K. The funicular pattern of Japanese peripheral nerves. Nihon Geka Hokan. 1969;38:35-58. [PubMed] |
| 11. | Delgado-Martínez I, Badia J, Pascual-Font A, Rodríguez-Baeza A, Navarro X. Fascicular Topography of the Human Median Nerve for Neuroprosthetic Surgery. Front Neurosci. 2016;10:286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 47] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 12. | Tsukuda Y, Funakoshi T, Nasuhara Y, Nagano Y, Shimizu C, Iwasaki N. Venipuncture Nerve Injuries in the Upper Extremity From More Than 1 Million Procedures. J Patient Saf. 2019;15:299-301. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 13. | Newman BH, Waxman DA. Blood donation-related neurologic needle injury: evaluation of 2 years' worth of data from a large blood center. Transfusion. 1996;36:213-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 14. | Newman B. Venipuncture nerve injuries after whole-blood donation. Transfusion. 2001;41:571-572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 15. | Berry PR, Wallis WE. Venepuncture nerve injuries. Lancet. 1977;1:1236-1237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 44] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Kuncoro J, Deapsari F, Suroto H. Clinical and functional outcome after different surgical approaches for brachial plexus injuries: Cohort study. Ann Med Surg (Lond). 2022;78:103714. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 17. | Temiz Ç, Yaşar S, Kırık A. Surgical treatment of peripheral nerve injuries: Better outcomes with intraoperative NAP recordings. Ulus Travma Acil Cerrahi Derg. 2021;27:510-515. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Desai K, Warade AC, Jha AK, Pattankar S. Injection-related iatrogenic peripheral nerve injuries: Surgical experience of 354 operated cases. Neurol India. 2019;67:S82-S91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |