Published online Jul 26, 2023. doi: 10.12998/wjcc.v11.i21.5187
Peer-review started: May 24, 2023
First decision: June 13, 2023
Revised: June 26, 2023
Accepted: July 7, 2023
Article in press: July 7, 2023
Published online: July 26, 2023
Processing time: 63 Days and 18.1 Hours
Brucellosis is one of the most common zoonotic infectious diseases in the world, with approximately 500000 new cases of human brucellosis diagnosed each year. Brucellosis can simulate various multi-system diseases, presenting atypical symptoms. Very few brucellosis cases with pancytopenia accompanied by a se
A 64-year-old woman presented with dizziness and fatigue, accompanied by pancytopenia and severe hearing loss. Brucella melitensis was identified on blood culture. Anti-infective therapy with rifampicin (900 mg/d) and doxycycline (100 mg twice a day) was prescribed for 4 mo along with ceftriaxone 2 g/d for 1 mo. The patient showed a good response to antibiotic therapy. Her blood counts re
Brucellosis should be considered in the differential diagnosis of patients pre
Core Tip: Brucellosis is a zoonotic disease that has recently shown a resurgence across the world. Brucellosis can affect multiple systems in the human body and the clinical manifestations may be atypical, making the diagnosis more difficult. In this article, we report a rare case of brucellosis presenting with pancytopenia and severe hearing loss. A series of tests ruled out a blood disorder, Brucella melitensis was identified on blood culture. The patient recovered well without sequelae after receiving anti-infective medication with rifampicin, doxycycline, and ceftriaxone. This report may help improve the understanding of brucellosis among clinicians in non-endemic areas.
- Citation: Chen X, Yang FB, Liang JY. Brucellosis presenting with pancytopenia and hearing loss: A case report. World J Clin Cases 2023; 11(21): 5187-5192
- URL: https://www.wjgnet.com/2307-8960/full/v11/i21/5187.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i21.5187
Brucellosis is a zoonotic disease that has recently shown a resurgence across the world[1]. The main geographical areas affected by brucellosis are the Mediterranean basin, South and Central America, Asia, Africa, the Caribbean, and the Near East countries. In China, the disease is more common in the northwest and Inner Mongolia pastoral areas. The incidence of human brucellosis in China has increased over the past 10 years and it has spread from north to south and from pastoral to non-pastoral areas[2]. Brucellosis is caused by a Gram-negative coccus. Sheep, pigs, and cattle are susceptible animals. Humans are usually infected through direct contact with infected animals, by consumption of contaminated milk and unsterilized food, and through inhalation of contaminated aerosols. Laboratory personnel are also susceptible to brucellosis, and human-to-human transmission is relatively rare. Brucella has 6 species and 20 biological types; currently, the most common strain infecting humans is Brucella melitensis.
The clinical manifestations of brucellosis may be atypical, mainly characterized by symptoms of respiratory infection, such as fever, sweating, headache, and cough; these may be accompanied by atypical fatigue and loss of appetite. Brucella can be found in every system of the human body; the most common site of damage is the bone and joint system; other systems affected include the blood system, cardiovascular system, and reproductive system. Nervous system involve
A 64-year-old woman living in the western Chinese city of Nanchong was hospitalized, because of dizziness and fatigue for 2 mo and hearing loss for the last 15 d.
About two months before admission, she developed dizziness and fatigue which was relieved after rest. There was no headache, nausea, vomiting, ataxia, nystagmus, palpitation, or other discomfort. Approximately 15 d before admission, her symptoms aggravated, accompanied by slight headache, and bilateral intermittent tinnitus with high frequency tone. Tinnitus did not interfere with sleep. She also developed bilateral progressive hearing loss, but there was no vertigo. There was no clear history of fever before admission. She was admitted to the Department of Hematology at our hospital.
She had no history of chronic diseases or infectious diseases.
She had no family history of genetically related diseases.
At admission, her vital parameters were: Temperature 36.5°C; pulse rate 98 per minute; respiration rate 20 per minute; blood pressure 116/68 mmHg. She appeared cachectic and pale. She had splenomegaly, but there was no hepatomegaly or mucosal petechiae. No abnormalities were detected on cardiopulmonary. On neurological examination, she was conscious, cooperative, and well-oriented with normal mental faculties. Her limb muscle strength and muscle tension were normal. There was no neck stiffness, Kerning sign and Brudzinski sign were negative. There was no papilledema. On ear examination, the bilateral auriculae were normal, the external ear canal was unobstructed, the tympanic membrane was intact, and the Politzcr cone was normal. She developed fever on the night of admission. Double sets of blood culture were obtained during the fever episode.
Blood counts showed pancytopenia (platelets: 95 × 109/L; hemoglobin 5.6 g/dL; white blood cell (WBC) count 2.97 × 109/L). Her biochemical parameters were: Aspartate aminotransferase 83 U/L; lactate dehydrogenase 503 U/L; alanine aminotransferase 42 U/L; C-reactive protein 26.38 mg/L; procalcitonin 0.172 ng/mL. Coomb's test was negative. Routine urine and fecal examination showed no signs of infection. She tested negative for antibodies against Hepatitis B, C, and human immunodeficiency virus. Bone marrow smear showed a reactionary marrow. Lumbar puncture revealed colorless and clear cerebrospinal fluid (CSF); the CSF pressure was 101 mmH2O, white blood cell count was 7 × 106/L; there were no leaf cells or lymphocytes; other CSF parameters were: microalbumin 0.373 g/L, lactate dehydrogenase 29.3 U/L, glucose 3.33 mmol/L, chlorine 125.4 mmol/L. Gram-stain negative, ink-stain negative, acid-fast bacilli negative. CSF cultures were negative.
Head computed tomography showed possible bilateral paraventricular lacunar infarction and intracranial arteriosclerosis. Abdominal ultrasound showed splenomegaly. Echocardiography showed mild mitral and tricuspid regurgitation.
Due to the lack of positive results and the persistence of clinical symptoms, marked anemia, and hearing loss, detailed epidemiological history of the patient was obtained. She stated that she had consumed contaminated mutton. Therefore, brucella infection was suspected. Subsequently, the blood culture suggested Brucella melitensis. The tiger red plate agglutination test (RBPT) and the standard test tube agglutination test (SAT) were positive (1:800). Brucellosis was determined
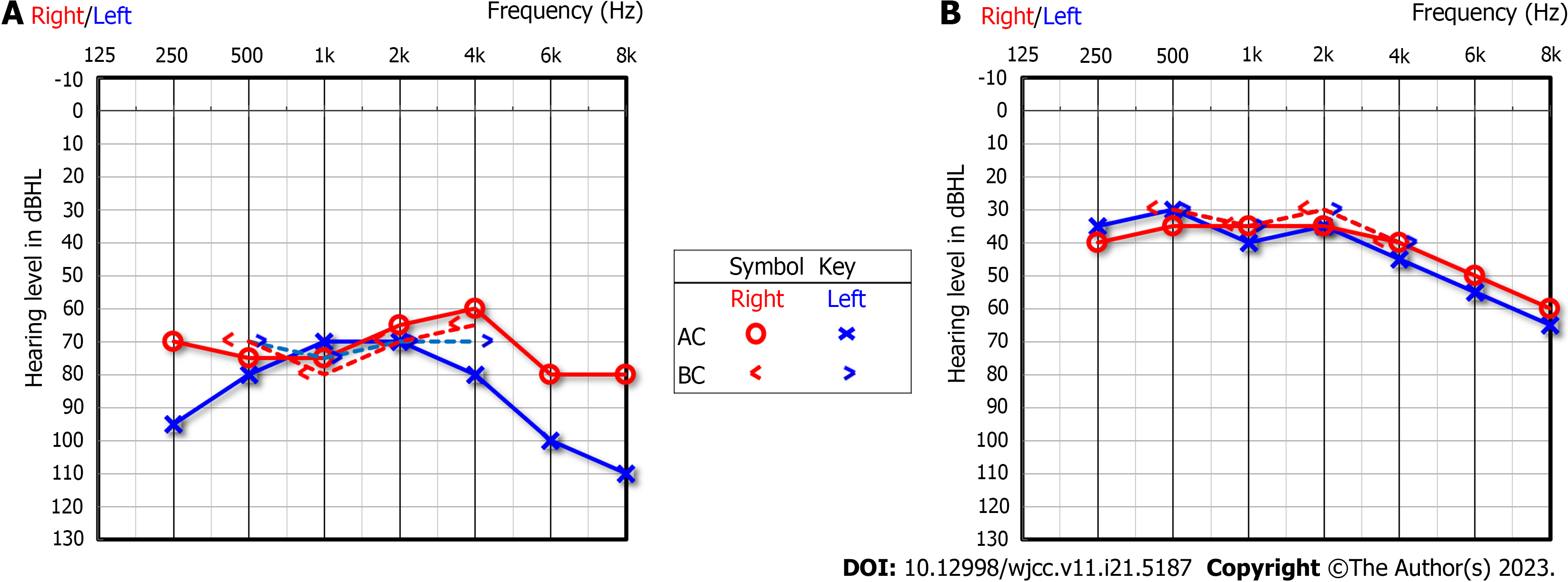
The patient was transferred to the Department of infectious diseases for further treatment. Pure-tone audiometry showed bilateral sensorineural hearing loss (Figure 1A). Due to the neurological complications, anti-infective therapy with rifampicin (900 mg/d) and doxycycline (100 mg twice a day) was prescribed for 4 mo, and ceftriaxone 2 g/d was prescribed for 1 mo.
The laboratory results and clinical symptoms indicated a good response. Her blood counts returned to normal in 90 days (Hb: 10.1 g/dL; platelets: 244 × 109/L; WBC: 4.84 × 109/L) (Table 1). Subsequently, the hearing improved as well (Figure 1B).
| Admission day | Day 7 | Day 90 | |
| WBC (109/L) | 2.97 | 3.77 | 4.84 |
| Hb (g/dL) | 5.6 | 9.5 | 10.1 |
| PLT (109/L) | 95 | 214 | 244 |
| CRP (mg/L) | 26.38 | 4.23 | 3.15 |
| PCT | 0.172 | 0.05 | 0.02 |
| D-dimer | 5890 | ||
| Serum ATL (U/L) | 42 | 6.4 | 16 |
| Serum AST (U/L) | 83 | 18.8 | 33 |
| Serum LDH (U/L) | 503 | 223.5 | 223 |
Brucellosis is an anthropozoonosis which is mainly transmitted through consumption of food contaminated with brucella, unpasteurized milk, contact with animals infected by brucella, or aerosol inhalation[3]. The organism can affect various organs and systems of the body, leading to a variety of complications, including spondylitis, meningitis, and endocarditis[4]. The condition is liable to be missed or misdiagnosed, leading to severe consequences.
Hematological disorders are often reflected in anemia and leukopenia. The occurrence of pancytopenia is extremely rare, and therefore, it can lead to a high suspicion of hematologic malignancy. Myelogram often shows reactionary marrow images, and hemophagocytosis can be seen in a few cases. The positive rate of bone marrow culture is higher than that of blood culture[5]. In a study, hematological disturbances and pancytopenia were detected in 28.6% and 7.7% of children affected by brucellosis[6]. In a study of Turkish adults affected by brucellosis, the percentage of patients having pancytopenia was approximately 5.8%, and those having thrombocytopenia, leukopenia, and erythrocytopenia was 18.8%, 14.6%, and 21.5%, respectively[7]. Our patient had pancytopenia, and Brucella melitensis was confirmed by blood culture. The pathophysiological basis of pancytopenia in brucellosis is not clear. It is believed that the hematological abnormalities caused by brucellosis may be attributable to various factors, such as hypersplenism, haemophagocytosis, maturation disorders of megakaryocytes, medullary hypoplasia, and production of autoimmune antibodies[8]. According to a study conducted in Turkey, WBC and platelet counts returns to normal approximately within 1 wk, and hemoglobin recovers in 3-4 wk after initiation of treatment[9]. Our patient was initially admitted to the Department of Hematology and was administered red blood cell transfusion to improve anemia. The hematological disturbances recovered well by the third month after standard antibiotic therapy.
Neurobrucellosis is a severe form of brucellosis occurring in approximately 5%-10% of all brucellosis patients[10]. Neurobrucellosis can present as meningoencephalitis, meningitis, polyradiculoneuropathy, papilledema, and optic neuritis. Previous case reports of brucellosis have also described the occurrence of brain abscess, cerebrovascular disease, and subarachnoid hemorrhage[11-13]. The chief complaints of the patients were headache, fever, defecation disorders, limb weakness, and a few patients manifested hearing loss. Thomas was one of the first scholars to report chronic sensorineural hearing loss caused by Brucella[14]. Subsequent reports have shown that patients with acute neurobrucellosis can also show hearing loss, and most of these patients manifest high-frequency hearing loss; the hearing loss is typically temporary, and the hearing threshold can be restored after antibiotic therapy. Kaygusuz et al[15] suggested that patients with chronic neurobrucellosis are prone to have neurological sequelae, such as permanent hearing loss. However, according to a literature review, timely antibiotic therapy can avoid permanent hearing impairment[16]. Our patient was diagnosed within 15 d of development of hearing loss, and pure-tone audiometry also suggested bilateral hearing loss (Figure 1A). Her hearing recovered well after 3 mo of standard antibiotic therapy (Figure 1B). It is generally agreed that hearing loss in neurobrucellosis may be related to the following factors: endotoxin-induced vascular spasm leading to nerve tissue ischemia, auditory pathway damage caused by inflammatory response, and auditory nerve fibrosis[17,18]. CSF examination in neurobrucellosis yields non-specific findings such as increased WBC count and protein level, and decreased glucose level, which are similar to the findings in tuberculous meningitis and neurosyphilis[19]. Brain imaging manifestations are also diverse and non-specific, including normal findings, inflammatory changes, white matter involvement, and cerebrovascular involvement[20]. Therefore, it is difficult to identify and diagnose neurobrucellosis based solely on physicochemical indices, CSF culture, and cranial imaging. The diagnosis rates can be greatly improved by collecting epidemiological history, serological tests, and nucleic acid amplification test[21]. Our patient had a history of consuming mutton and had abnormal blood indices and hearing loss at admission. Clinicians need to consider the possibility of brucella infection in such cases and conduct relevant investigations in time. Timely anti-brucella treatment can effectively restore hearing and avoid permanent hearing loss caused by chronic disease.
Brucella is a small, fastidious Gram-negative coccobacilli, which is an intracellular parasite. Conventional anti-infective treatment is not effective and it is easy to relapse.
As per the World Health Organization treatment guidelines, we prescribed triplet combination therapy of rifampicin plus doxycycline for 4 mo and ceftriaxone for 1 month. This case was admitted to our department in the second month of the onset, and was diagnosed as brucellosis according to the blood culture. With hematological and neurological abnormalities, she was administered red blood cell transfusion to correct anemia and treated with triplet combination antibiotic therapy. On the 7th day of the treatment course, the blood counts returned to normal, and on the 90th day, the pure-tone audiometry findings were significantly better than that at admission. There are still some areas for improvement in our case. The epidemiological history of the patient could have been more carefully evaluated at admission. Head magnetic resonance imaging examination could have helped evaluate the intracranial situation in more detail. Moreover, CSF examination with RBPT and SAT could have been performed. Lastly, otoscopy should have been performed for evaluation of hearing loss.
This case suggests that timely and effective antibiotic therapy can lead to a good prognosis of the patient. The clinical manifestations of brucellosis are often non-specific and atypical. For patients with unexplained pancytopenia, especially those with hearing loss, a detailed epidemiological history, and timely and standardized blood, bone marrow, ce
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Infectious diseases
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Koleci X, Albania; Mirsalehi M, Iran S-Editor: Liu JH L-Editor: A P-Editor: Cai YX
| 1. | Pappas G, Memish ZA. Brucellosis in the middle East: a persistent medical, socioeconomic and political issue. J Chemother. 2007;19:243-248. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 46] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 2. | Jiang H, O'Callaghan D, Ding JB. Brucellosis in China: history, progress and challenge. Infect Dis Poverty. 2020;9:55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 57] [Article Influence: 11.4] [Reference Citation Analysis (0)] |
| 3. | Jiao LD, Chu CB, Kumar CJ, Cui J, Wang XL, Wu LY, Li CJ, Wang XB. Clinical and Laboratory Findings of Nonacute Neurobrucellosis. Chin Med J (Engl). 2015;128:1831-1833. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Medical Microbiology. Galveston (TX): University of Texas Medical Branch at Galveston; 1996-. [PubMed] |
| 5. | Queipo-Ortuño MI, Morata P, Ocón P, Manchado P, Colmenero JD. Rapid diagnosis of human brucellosis by peripheral-blood PCR assay. J Clin Microbiol. 1997;35:2927-2930. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 90] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Karaman K, Akbayram S, Bayhan GI, Dogan M, Parlak M, Akbayram HT, Geylan H, Garipardic M, Oner AF. Hematologic Findings in Children With Brucellosis: Experiences of 622 Patients in Eastern Turkey. J Pediatr Hematol Oncol. 2016;38:463-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 7. | Kaya S, Elaldi N, Deveci O, Eskazan AE, Bekcibasi M, Hosoglu S. Cytopenia in adult brucellosis patients. Indian J Med Res. 2018;147:73-80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Pappas G. Treatment of brucellosis. BMJ. 2008;336:678-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Dilek I, Durmus A, Karahocagil MK, Akdeniz H, Karsen H, Baran AI. Hematological complications in 787 cases of acute brucellosis in Eastern Turkey. Turk J Med Sci. 2008;38:421-424. |
| 10. | Gul HC, Erdem H, Gorenek L, Ozdag MF, Kalpakci Y, Avci IY, Besirbellioglu BA, Eyigun CP. Management of neurobrucellosis: an assessment of 11 cases. Intern Med. 2008;47:995-1001. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 28] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Nas K, Tasdemir N, Cakmak E, Kemaloglu MS, Bukte Y, Geyik MF. Cervical intramedullary granuloma of Brucella: a case report and review of the literature. Eur Spine J. 2007;16 Suppl 3:255-259. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Adaletli I, Albayram S, Gurses B, Ozer H, Yilmaz MH, Gulsen F, Sirikci A. Vasculopathic changes in the cerebral arterial system with neurobrucellosis. AJNR Am J Neuroradiol. 2006;27:384-386. [PubMed] |
| 13. | Karakurum Goksel B, Yerdelen D, Karatas M, Pelit A, Demiroglu YZ, Kizilkilic O, Tan M, Toygar O. Abducens nerve palsy and optic neuritis as initial manifestation in brucellosis. Scand J Infect Dis. 2006;38:721-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Thomas R, Kameswaran M, Murugan V, Okafor BC. Sensorineural hearing loss in neurobrucellosis. J Laryngol Otol. 1993;107:1034-1036. [RCA] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 15. | Kaygusuz TO, Kaygusuz I, Kilic SS, Yalcin S, Felek S. Investigation of hearing loss in patients with acute brucellosis by standard and high-frequency audiometry. Clin Microbiol Infect. 2005;11:559-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Gul HC, Erdem H, Bek S. Overview of neurobrucellosis: a pooled analysis of 187 cases. Int J Infect Dis. 2009;13:e339-e343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 96] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 17. | Rodríguez AM, Delpino MV, Miraglia MC, Giambartolomei GH. Immune Mediators of Pathology in Neurobrucellosis: From Blood to Central Nervous System. Neuroscience. 2019;410:264-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 18. | Malhi AB, Ridal M, Bouchal S, Belahsen MF, El Alami MN. Neurobrucellosis: a treatable cause of sensorineural hearing loss not to ignore. Pan Afr Med J. 2015;22:122. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 19. | Erdem H, Ulu-Kilic A, Kilic S, Karahocagil M, Shehata G, Eren-Tulek N, Yetkin F, Celen MK, Ceran N, Gul HC, Mert G, Tekin-Koruk S, Dizbay M, Inal AS, Nayman-Alpat S, Bosilkovski M, Inan D, Saltoglu N, Abdel-Baky L, Adeva-Bartolome MT, Ceylan B, Sacar S, Turhan V, Yilmaz E, Elaldi N, Kocak-Tufan Z, Ugurlu K, Dokuzoguz B, Yilmaz H, Gundes S, Guner R, Ozgunes N, Ulcay A, Unal S, Dayan S, Gorenek L, Karakas A, Tasova Y, Usluer G, Bayindir Y, Kurtaran B, Sipahi OR, Leblebicioglu H. Efficacy and tolerability of antibiotic combinations in neurobrucellosis: results of the Istanbul study. Antimicrob Agents Chemother. 2012;56:1523-1528. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 20. | Rajan R, Khurana D, Kesav P. Deep gray matter involvement in neurobrucellosis. Neurology. 2013;80:e28-e29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |