Published online Jul 16, 2023. doi: 10.12998/wjcc.v11.i20.4752
Peer-review started: May 4, 2023
First decision: June 1, 2023
Revised: June 11, 2023
Accepted: June 19, 2023
Article in press: June 19, 2023
Published online: July 16, 2023
Processing time: 68 Days and 18.9 Hours
Coronary artery disease (CAD), a primary component of cardiovascular diseases, is one of the top contributors to mortality rates worldwide. In 2021, dietary risk was estimated to be attributed to 6.58 million cardiovascular deaths. Plant-based diets (PBDs), which encourage higher consumption of plant foods and lower intake of animal-based foods, have been shown to reduce the risk of CAD by up to 29% when compared to non-vegetarian diets in a meta-analysis. This article aims to summarize the array of PBDs and compare them with conventional Western diets that include meat. We review the various proposed mechanisms for how the bioactive nutrients of PBDs aid in preventing atherosclerosis and CAD events, as well as other cardiac diseases. We conducted a detailed search of PubMed using our exclusive search strategy using the keywords plant-based diet, vegan diet, phytosterols, CAD, myocardial ischemia, and atherosclerosis. A total of 162 pertinent articles published within the past decade were identified for qualitative synthesis. To ensure the accuracy and reliability of our review, we included a total of 55 full-text, peer-reviewed articles that demonstrated the effects of plant-based diets on CAD and were written in English. We excluded animal studies, in vitro or molecular studies, and non-original data like editorials, letters, protocols, and conference abstracts. In this article, we emphasize the importance of dietary interventions, such as PBDs, to prevent CAD and their benefits on environmental sustainability. Integrating plant foods and whole grains into one's daily eating habits leads to an increase in the intake of nutrient-rich foods while reducing the consumption of processed food could not only prevent millions of premature deaths but also provide prevention against many chronic gastrointestinal and metabolic diseases.
Core Tip: The prevailing fund of knowledge depicts that a high salt diet or a Western diet that contains excessive saturated fats, and meat augments inflammation, oxidation, and atherogenic activity in our body. The American Heart Association and European Atherosclerotic Society both recommend consuming more fruits, vegetables, dietary fibers, and nuts that are all integral to plant-based diets in order to prevent the progression of coronary artery disease (CAD). However, we could not find an article that provided a comprehensive review of a variety of bioactive nutrients in these diets, comparing several types of diets and their effects on diverse metabolic conditions like diabetes, hyperlipidemia, and atrial fibrillation, amongst others. We, thus, author a narrative review to compile the proposed effect of each nutrient, antioxidant as well as various diets on CAD in adults.
- Citation: Mehta P, Tawfeeq S, Padte S, Sunasra R, Desai H, Surani S, Kashyap R. Plant-based diet and its effect on coronary artery disease: A narrative review. World J Clin Cases 2023; 11(20): 4752-4762
- URL: https://www.wjgnet.com/2307-8960/full/v11/i20/4752.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i20.4752
Cardiovascular deaths are the primary cause of death worldwide. By 2035, 45.1% of American deaths will be attributed to cardiovascular diseases (CVD), resulting in approximately 130 million deaths, with a total estimated financial burden of $1.1 trillion. A decrease in these risk factors has the potential to increase global life expectancy by up to five years[1]. The categorization of coronary artery disease (CAD), a primary component of CVD, encompasses Stable Ischemic Heart Disease and Acute Coronary Syndrome, which includes ST-Elevation MI (STEMI), Non-STEMI (NSTEMI), and Unstable Angina[2]. The likelihood of suffering CVD can be exacerbated by risk factors such as excessive body weight, obesity, hypertension, smoking, stress, and a sedentary lifestyle[3]. However, an unhealthy diet, which is a significant modifiable risk factor for CVD, is often neglected[4]. In 2021, dietary risk was estimated to be attributed to 6.58 million cardiovascular deaths[5]. Typically, the detrimental effects of these risk factors on lipid profiles directly mediate CAD. Therefore, various interventions that restore a healthy lipid profile are crucial, as they significantly reduce the risk of developing atherosclerotic CVD[3].
Plant-based diets (PBDs), which encourage higher consumption of plant foods and a lower intake of animal-based foods, have been linked to improved cardiovascular health, lower cardiac mortality, and all-cause mortality[6]. The Nurses’ Health Study revealed that for each serving of leafy green vegetables consumed per day, the risk of CAD decreased by 11%[7]. Prompting patients to augment their intake of soluble fibers and phytosterols may also assist them in realizing their therapeutic goals for even obesity, dyslipidemia, Type 2 diabetes mellitus (T2DM), hypertension, and chronic kidney disease[3,7]. PBDs have also been shown to reduce the risk of CAD by up to 29% compared to non-vegetarian diets in a meta-analysis[3].
PBDs have gained popularity due to concerns about environmental welfare, as well as their perceived health benefits[4,7]. Adopting sustainable diets is essential to address environmental degradation, particularly climate change, as global livestock is responsible for 18% of anthropogenic greenhouse gas emissions[7]. During the coronavirus disease pandemic, PBDs have been proposed as a possible means of preventing and mitigating the future transmission of viruses between different species and humans[7].
This review aims to explore the gamut of PBDs, reassess clear definitions and categorizations, and contrast them with conventional Western non-vegetarian diets. Additionally, we examine the proposed mechanisms that explain the cardiovascular advantages of PBDs, with specific attention to how dietary adjustments affect the interaction between gut microbiota and the host and the resulting impact on inflammation at both the local and systemic levels. The current body of literature pertaining to the influence of PBDs on CAD is appraised, and the obstacles and constraints related to dietary interventions are examined.
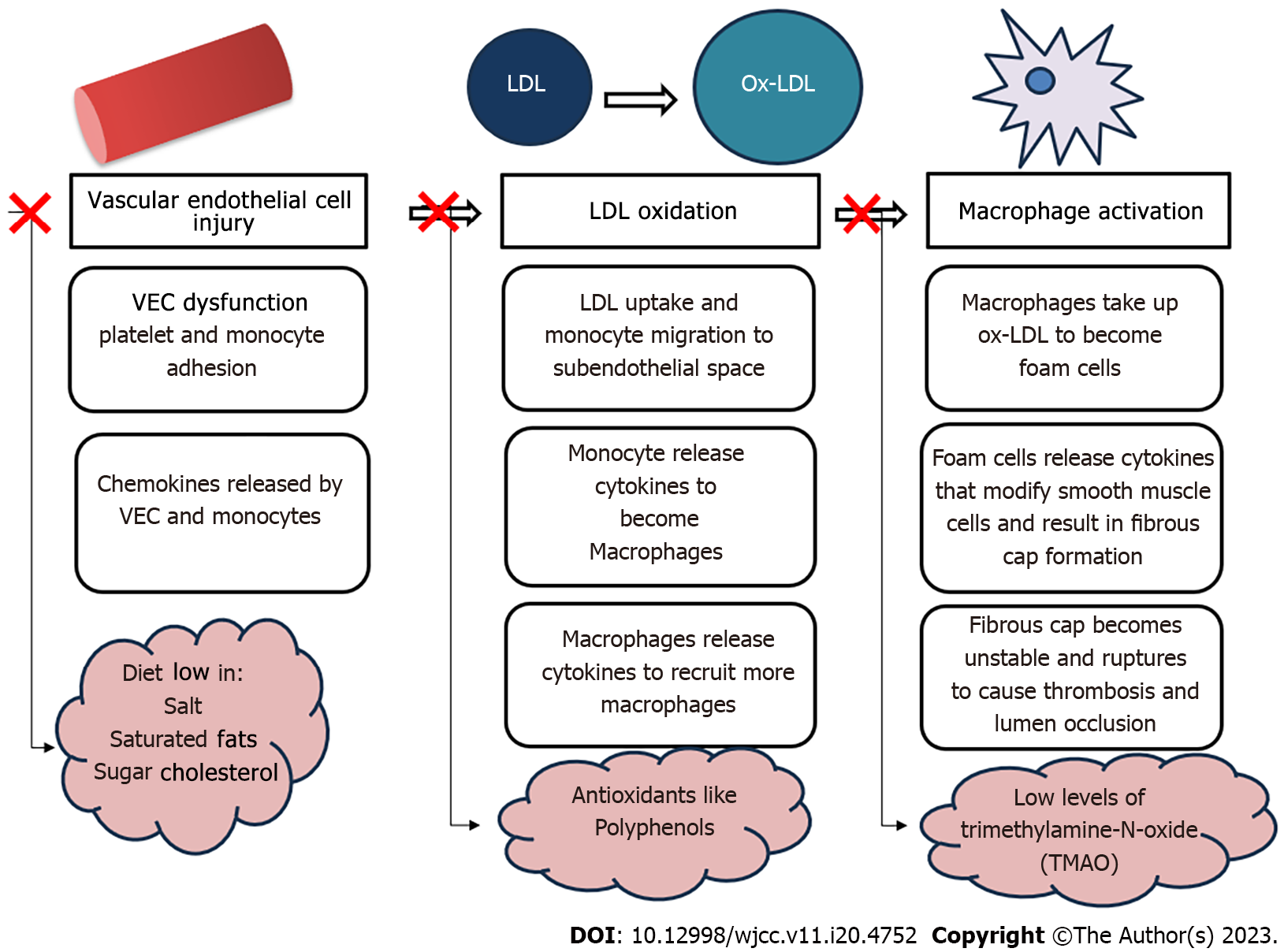
Atherosclerosis is a complex disorder that develops in response to numerous insults to the endothelial lining of arteries, resulting in an excessive inflammatory-fibro-proliferative response. Vascular endothelial cells (VECs) are essentially required to function properly to achieve vascular homeostasis because abnormalities may culminate as a clinical manifestation of CAD. VECs also modulate platelet, leukocyte adhesion, and leukocyte (macrophage) transmigration[7]. When VECs endure damage, they become dysfunctional and lose their ability to regulate nitric oxide production and prevent pro-inflammatory factors' expression[7,8]. Low-density lipoprotein (LDL) oxidation occurs in the subendothelial space, transforming monocytes into macrophages, which promotes plaque formation and destabilization. Oxidized LDL (ox-LDL) is currently considered a major contributor to atherosclerosis and endothelial and smooth muscle cell damage[7,9]. Unlike normal LDL receptors, ox-LDL is easily recognized and quickly engulfed by macrophages, leading to the formation of foam cells[8,10]. This contributes to the atherosclerotic plaque formation and stenosis of the arteries. These plaques can ultimately rupture, causing complete occlusion of the artery, ensuing ischemia, and potentially death. Furthermore, investigations have verified that a high level of reactive oxygen species can promote the activity of superoxide dismutase (SOD), which subsequently may initiate atherosclerosis by compromising the antioxidant capacity of cells, prompting lipid peroxidation alongside damaging DNA, and enabling vascular endothelial dysfunction. In contrast, high-density lipoprotein (HDL) removes cholesterol from arterial walls through cholesterol reverse transport, preventing atherosclerosis. HDL also has antioxidant effects, preventing LDL oxidation and competitively inhibiting LDL and endothelial cell receptors[9,11].
Plant-based nutrition encompasses predominantly consuming whole foods derived from plants to obtain essential macronutrients (carbohydrates, proteins, and fats), micronutrients (such as vitamins and minerals), and bioactive components (such as flavonoids, plant sterols, and polyphenols) that optimize our fettle and form[7,12]. The mechanism of various components of PBDs and their impact on atherogenesis is portrayed in Figure 1.
Phytosterols: Phytosterols are physiologically active molecules derived from plants that structurally analogize cholesterol[11]. While phytosterols cannot be synthesized in the human body, they are present in all plant-based food[13]. Vegetable oils, spreads, margarine, bread, cereals, and vegetables are the main food sources of plant sterols and account for 50%–80% of daily intake, with fruits contributing another 12%. Vegetarians may consume as much as 600 mg of plant sterols daily, which is higher than the average Western diet's 300 mg[14].
Cholesterol and phytosterols are both triterpenes, which have a tetracyclic ring and a carbon-linked side chain[15]. However, plant sterols differ from cholesterol in their side chain structure at position C24. Campesterol and β-sitosterol are the two most ubiquitous plant sterols comprising about 65% and 30% of the total, respectively. In contrast, plant stanols are typically found in very low amounts in plants, and the most common type of stanol is the 5α-saturated stanol. Plant stanols are sterols that are saturated and have a double bond located at the C5-atom in the B-ring[13].
In addition to competing with cholesterol for solubilization in mixed micelles in the intestinal lumen, phytosterols also transmogrify the expression of genes that encode for proteins that mediate cholesterol uptake into enterocytes, such as Niemann-Pick C1-like protein 1 and transport back into the gut lumen via the ABCG5/ABCG8 transporters. Alternate hypothesized mechanisms include a diminution in cholesterol esterification within intestinal cells with an escalation in the body's ability to excrete cholesterol via transintestinal cholesterol excretion[13]. Despite the intensification of synthesized cholesterol as a consequence of decreased dietary cholesterol absorption, the amount generated by the liver is insufficient to atone for the dwindled dietary cholesterol absorption. When contrasted with cholesterol (approximately 50%), the absorption of plant sterols (< 2%) and stanols (< 0.2%) is much lower. Owing to their efficient biliary excretion, circulating levels of phytosterols are generally quite low, ranging from 0.3 to 1.0 mg/dL for plant sterols and 0.002 to 0.012 mg/dL for plant stanols[16]. Treatment with plant sterols reduced plasma endothelin-1 Levels by 11%, regardless of any changes in LDL levels in the bloodstream[17].
In 2010, the United States Food and Drug Administration authorized a health claim for phytosterols, which indicated that consuming a minimum of 1.3 g of plant sterols and 3.4 g of plant stanols each day as part of a diet low in saturated fat and cholesterol can potentially lower the risk of heart disease[18].
Cholesterol Oxidation Products: Cholesterol oxidation products (COPs) are oxysterols, and oxy-phytosterols are phytosterol oxidation products (POPs). Oxy-Phytosterols are easily absorbed, are toxic, and can cross the blood-brain barrier. These POPs, like COPs, are linked to inflammation and atherosclerosis[16,19,20]. High blood levels of oxysterols have been observed in patients with > 75% coronary artery stenosis[21].
Campesterol: Campesterol is a crucial CAD marker. A previous study discovered a direct relationship between CAD and elevated levels of oxidized campesterol in the tissue that makes up the aortic valve[22,23].
Omega-3-Fatty acids: Omega-3 fatty acids (Omega-3-FA) are polyunsaturated fatty acids (PUFAs), with docosahexaenoic acid (DHA) and eicosapentaenoic acid (EPA) being the two most important types. These are abundant in fish, shellfish, and certain algae. The beneficial role of Omega-3-FA in CAD has been implicated in several research studies[11,24]. These include slowing the furtherance of atherosclerosis, ebbing inflammation, enhancing plaque stability, and inhibiting platelets[11]. Nevertheless, a different study reported no significant difference in LDL levels following Omega-3 supplementation[24].
Dietary Fibers: Dietary fibers, which are abounding in PBDs, eminently provide a palisade against colon cancer, notwithstanding some notable beneficial effects on cardiac health as well. A combined analysis of 18 cohort studies[1] examined the association between dietary fiber intake and CAD risk and inferred that a higher intake of fibers was significantly associated with a reduced risk of CAD incidence (by 7%) and mortality (by 17%). The analysis further demonstrated that for each additional 10 g/day of dietary fiber intake, there was an associated 8% decrease in the likelihood of any coronary events and a 24% reduction in the risk of mortality[1].
Polyphenols: Polyphenols, such as the arubigins in black tea, possess various salubrious benefits, especially for cardiac health[1]. Polyphenols delay the onset as well as the progression of CAD per their manifold protective effects. It acts as a hypolipidemic, antioxidative, antiproliferative, and anti-inflammatory agent[25]. They also act as an anti-atherogenic substance by elevating HDL levels and have a favorable impact on the endothelium[26].
Resveratrol is a type of polyphenol that is present in the skin of grapes, berries, and peanuts. It exhibits antioxidant properties, enhances the production of nitric oxide synthase, and improves mitochondrial function. Resveratrol supplementation improves hemoglobin A1c (HbA1c) concentrations, total cholesterol, LDL, and systolic blood pressure levels in people with T2DM[1]. Resveratrol can boost serum sirtuin 1 concentration, which impedes the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-kB) signaling pathway, causing the suppression of pro-inflammatory cytokines such as tumor necrosis factor-alpha, interleukin (IL)-1b, IL-6, and monocyte chemoattractant protein-1. Resveratrol also expresses antiplatelet activity by inhibiting cyclo-oxygenase 1, leading to reduced synthesis of thromboxane A2, which triggers platelet aggregation[11].
Studies have exhibited that consuming extra virgin olive oil can mitigate the incidence of several health conditions, including atherosclerosis, hypertension, thrombotic risk, hypercholesterolemia, and oxidative stress[1]. The prevention of atherosclerosis ontogenesis can be attributed to hydroxytyrosol, oleuropein, and tyrosol. These compounds can alleviate endothelial dysfunction, curtail the concentration and atherogenicity of LDL, ameliorate antioxidant effects and HDL function, and hamper platelet aggregation[11].
Flavonoids: Foods such as cocoa and green tea contain flavanols, epicatechin, catechin, and proanthocyanidins that have been studied for their potential utility in cardiovascular health[27]. Reviews and meta-analyses have examined the association between cacao consumption and various cardiovascular risk factors such as blood pressure, endothelial function, blood lipids, and platelet function[1]. Green tea catechins could be rapidly incorporated into LDL particles and significantly reduce LDL oxidation, thereby reducing the risk of atherosclerosis associated with oxidative stress[1,28].
Quercetin, one of the vital flavonoids of the human diet, can be found in plentitude in a variety of fruits and vegetables, including apples, onions, cherries, and grapes[1]. Quercetin has been found to have anti-obesity properties. Consequently, quercetin may help to reduce the development of atherosclerosis related to endothelial dysfunction[11].
Anthocyanins, which are abundant in blueberries, cranberries, bilberries, chokeberries, and elderberries, have been documented to enhance coronary wellness by minimizing pro-inflammatory markers in addition to their antioxidant capabilities. It has been discovered that drinking beverages high in anthocyanins augments plasma levels of the antioxidant enzymes catalase and SOD while decreasing levels of malondialdehyde which is a marker of lipid peroxidation. Research suggests that anthocyanins could be effective in preventing atherosclerosis by targeting platelet chemokines[1].
Isoflavones, present in soy and soy products, have been known to possess a positive influence on cardiovascular health. Their beneficial effects can be accredited to a reduction in cholesterol levels as well as a decrease in oxidative stress-mediated by isoflavones[1].
An additional benefit of a PBD is the number of micronutrients exposed to the body. Vitamin D, B12, K, and other micronutrients like calcium and selenium have been found to benefit cardiovascular health[10,29].
Whole food PBD: A whole food, plant-based (WFPB) diet includes whole grains, fruits, vegetables, legumes, nuts, seeds, herbs, and spices. For adequate nutrient consumption, the United States Department of Agriculture and American Heart Association (AHA) recommend half of the plate constitute vegetables and fruits[30].
Fiber and phytonutrients are the essential components of plant food. These promote health by reducing inflammation and oxidation and providing powerful protection through disease prevention and progression[30]. This is proven by a recent study where the WFPB diet was associated with reducing cardiometabolic disorders such as obesity, hyperlipidemia, hypertension, and diabetes and diminishing the need for medications for such conditions[31]. As a result, this diet has proven to reduce mortality from CVD and even reverse CAD[32].
Vegan diet: A vegan diet is entirely devoid of all animal products. Among the limited studies on the significance of veganism on cardiovascular health, a study conducted by Vinagre et al[33] stands out. He ascertained that vegans consume high PUFAs, fiber, and low saturated fats, cholesterol, and proteins. This reduces cardiometabolic risk factors such as body mass index (BMI), blood pressure, serum glucose, serum LDL and inflammation[34]. Compared to other food groups, the vegan diet has the least risk of CVD and can even reverse CAD to some extent[35]. Other studies have not found any compelling relevance to cardiovascular outcomes. Despite a better lipid profile, the mean carotid intima-media thickness was high amongst vegans[36,37]. Additionally, vascular studies revealed unfavorable atherosclerotic surrogates, endothelial impairment, as well as the slower transfer of cholesterol esters in vegans[37]. A strict vegan diet lacks certain cardioprotective nutrients such as vitamin B12 and certain Omega-3-FA: EPA and DHA. This may have an adverse outcome on atherosclerosis and can be ameliorated by vitamin B12 supplementation[26,34].
Nuts: Regular consumption of nuts positively directs the body's constitution. The bioactive substances present in nuts are unsaturated fatty acids, phytosterols, phenolic antioxidants, fiber, vitamins, and minerals[4].
Evidence from two large cohort studies showed that dietary intake of nuts five times per week was associated with a 48% decrease in the risk of mortality from coronary heart disease and a 25% reduction in the risk of cardiovascular death. Additionally, daily consumption of nuts was associated with a reduced risk of metabolic syndrome and a 20% reduction in all-cause death[38]. Therefore, the addition of nuts to the WFPB, vegan, or Mediterranean diet is recommended as it is well-recognized that it can reverse atherosclerosis and CAD due to its low saturated fat content[35].
Brazilian nuts, produced in South America, are rich in PUFAs (60%-70%), protein, fibers, selenium, arginine, vitamin B, vitamin E, phytosterols, and polyphenols. Brazilian nuts have been established to reduce vascular inflammation, oxidative stress, platelet aggregation, total cholesterol, triglyceride, and blood glucose levels. It emends HDL levels and arterial stiffness[38].
Wild Rice: Wild rice is grown mostly in North America and East Asia. It is a rich source of protein and antioxidant Vitamin E, as well as has a low-fat content. Several studies have demonstrated that the nutritional phytochemicals of wild rice exhibit the following beneficial effects: Preventing atherogenesis, extenuating cardiovascular risk factors such as lowering blood cholesterol levels, improving insulin resistance, and attenuating hypertension[39].
Tomatoes: Tomatoes contain phytonutrients such as carotenoids, phytosterols, and tocopherols. Evidence suggests regular tomato consumption reduces oxidized LDL levels, triglycerides, glucose, and insulin, which renders protection against atherosclerosis[40].
Traditional diet: Evidence suggests Panax ginseng, a component of traditional Chinese medicine, has cardioprotective effects as well as therapeutic effects on myocardial ischemic-reperfusion injury[41].
The population of Okinawa, Japan, boasts one of the highest numbers of centenarians and a low incidence of age-related illnesses[30]. This is, for the most part, due to their traditional diet, which is rich in nutrients, low in calories, and very low in fat, particularly saturated fat. However, as their dietary habits move away from the traditional Okinawan PBD and more towards a Western diet, their life expectancy is decreasing[30].
The practice of veganism, in particular, prohibits the intake of any animal-derived product, such as meat, seafood, eggs, and even dairy[33]. On the other hand, vegetarians are individuals who consume dairy, eggs, or both but do not consume seafood or animal meat[42]. Lastly, omnivores eat all the aforementioned foods, including animal meat. In recognition of the lower ingestion of saturated fats and larger quantities of nutritional fibers in vegetarian and vegan diets, omnivore subjects are more likely to develop CVD than their counterparts[42].
Research corroborates that a vegan diet ameliorates cardiovascular health by curtailing the BMI, inflammation, cholesterol, and glucose levels in contrast to omnivorous diets, which often lack substantial quantities of whole grains, fruits, vegetables, and nuts[36]. The concentration of LDL in omnivores supersedes that of vegetarians[33,43,44]; nonetheless, studies are yet to consistently estimate any remarkable difference in the levels of HDL and triglycerides (TG) betwixt the two groups[45]. However, Bhupathiraju et al[46] reported a strong, positive correlation between a Western or non-vegetarian diet with TG, insulin resistance, liver-to-spleen attenuation ratio, and markers of glycemia. Notably, an intake of more than four servings of dark fish in a week was ratiocinated to be associated with greater odds of developing atrial fibrillation[47]. Atrial fibrillation is postulated to be consecutive to oxidative stress, disturbed calcium homeostasis, and cardiomyocyte death, amongst other pathological events[47]. Over time, it has been deciphered that PBDs cause a considerable reduction in the risk of developing atrial fibrillation owing to their high anti-inflammatory and antioxidant nutrients[48].
A study by Bhupathiraju et al[49] assessed the quality of the PBD using 3 established indices: Overall PBD index (PDI); healthy PDI (hPDI), which encompasses whole grains, vegetables, fruits, legumes, nuts, herbs, and spices; and unhealthy PDI (uPDI) which includes refined grains, potatoes, deep fried food, coconut, sugar, sweetened beverages, and dessert. The results showed higher PDI and hPDI were associated with lower LDL, insulin resistance, and BMI[12,49]. Higher hPDI resulted in a lower likelihood of HbA1c, fatty liver, obesity, and incidence of type 2 diabetes. Surprisingly, this study reported no association between uPDI and cardiometabolic risk factors.
Another research article studied an additional PDI called the pro-vegetarian index with a more simplistic score that does not assess the refined carbohydrate group[6,50]. A higher pro-vegetarian index and PDI were found to significantly reduce the incidence of CVD, CVD mortality, and overall mortality, according to the study's findings. An inverse association between hPDI and CVD mortality and all-cause mortality was also reported[6,50].
The gut microbiota is a complex and diverse community of microorganisms that inhabits the gastrointestinal tract and plays a crucial role in regulating metabolism, immunity, and inflammatory processes. Additionally, recent research has revealed that the bacteria in atherosclerotic plaques are analogous to those that colonize the gut[51]. One of the metabolites produced by the gut microbiota is trimethylamine-N-oxide (TMAO)[4], which is derived from dietary sources such as choline, betaine, and L-carnitine. TMAO has been linked to the development and progression of CAD due to its pro-inflammatory effects and its inhibition of reverse cholesterol transport[51]. With their higher intake of red meat, Omnivores are significantly more susceptible to CVD than those who consume PBDs. This was disclosed in a study[4] conducted on over 4000 patients undergoing elective coronary angiography. Thereafter, augmented production of TMAO has deemed an independent risk factor for CAD. Nonetheless, switching to a PBD may offer protection against CAD by promoting endothelial protective mechanisms and lowering the pro-atherosclerotic metabolites, such as TMAO. A PBD microbiota would prevent the conversion of phosphatidylcholine or L-carnitine to TMAO[37]. A study of individuals with metabolic syndrome who received fecal microbiota transplant (FMT) from a single vegan donor had changes in the composition of their intestinal microbiota but not in the level of TMAO generation or an atherogenic proinflammatory state[45]. Although this study had its limitations, further research targeting the gut microbiota through therapies such as FMT and probiotic supplementation may provide better insight into CAD treatment[42].
Sitosterolemia, also known as phytosterolemia, is an inherited disorder that affects lipid metabolism and results in elevated levels of plant sterols in the blood. The condition is caused by specific genetic variations in ABCG5 or ABCG8, with the resultant accumulation of plant sterols in the body due to diminished elimination by the liver and upheaved absorption by the intestines[52]. In terms of clinical presentation, infants who are heterozygous for phytosterolemia do not show any symptoms, whereas homozygous infants may develop xanthomas in various areas of the body, including the patella and Achilles' tendons, extensor tendons of the hand, and pressure-bearing areas like the elbows. With dietary adjustments and, if necessary, medical treatment, these xanthomas may eventually disappear. Children between the ages of five and adolescents may have both life-threatening and non-fatal cardiac events as well as aortic stenosis[53]. The primary treatment for sitosterolemia is a combination of a diet that is low in plant sterols and the use of the medication ezetimibe, which inhibits cholesterol absorption in the intestines. This treatment is highly effective in reducing the levels of plant sterols in the blood and is considered the first-line therapy for this condition[51].
Inculcating lifestyle modifications can significantly improve cholesterol levels and reduce the risk of heart disease. An increased intake of fruits, vegetables, seafood, vegetable oils, yogurt, and entire grains, as well as a reduction in the consumption of animal meats, sodium-rich foods, and meals with substantially refined sugars, pertains to an estimated decrease in the incidence of CVD cases. Moreover, it indicates that the replacement of animal fats, including dairy fat, with vegetable sources of fats and PUFAs may check the risk of CVD. For the best outcomes, it is advised to work with a healthcare professional to develop a personalized diet plan[3,54,55].
A healthy nutrition pattern should aim at amplifying the consumption of vegetables, fruits, legumes, nuts, and whole grains. Additionally, it's critical to replace saturated oils in the diet with dietary monounsaturated and polyunsaturated fats. To achieve this, it is recommended to reduce the amount of cholesterol and sodium in the diet and incorporate PBDs. As part of a nutritious diet, it is also reasonable to curb your intake of processed animal products, refined starches, and sweetened beverages. Trans fats should be completely avoided since their ingestion is linked with negative health effects. Overall, a healthful diet should be surplus in whole, nutrient-dense foods and limit processed and high-calorie foods. The effect of a vegan versus AHA DiEt in CAD trial even portrayed that the patients with CAD who followed a vegan diet had significantly lower high-sensitivity C-reactive protein levels (32% lower) than those who followed the AHA diet[3,54-56].
Paring down the serum LDL levels can abate the likelihood of cardiovascular events in patients with CAD[54-56]. Statins are the first-line treatment, but some patients may not reach their target LDL values. Combining statins with other drugs or implementing dietary modifications, such as nuts, plant sterols, less digestible carbohydrates, and indigestible fiber, can also help in waning LDL levels[57].
Evidence suggests that supplementary plant sterols/stanols at a dose of approximately 2 g/d leads to a 10% decrement in serum LDL concentrations, which persists even when combined with statin therapy[14,56]. Similar results were reaffirmed by other studies. A clinical trial with 190 adults compared the effects of different treatments on reducing LDL[57]. Rosuvastatin showed the highest reduction at 38%, while plant sterols only showed a 4.4% reduction[57]. While there is limited data available, evidence also suggests that plant sterols/stanols may have an additive effect when combined with ezetimibe and fibrates[14,56]. In contrast, a well-designed study involving healthy individuals found that both low and high intake of plant sterols did not have a significant impact on plasma LDL concentrations[14].
There is insufficient data on the efficacy of combining bile acid sequestrants and dietary plant sterols/stanols for lowering lipids. Bile acid sequestrants could hinder the absorption of sterols/stanols, while the consumption of plant sterols may reduce bile acid synthesis, potentially impacting the effectiveness of bile acid sequestrants[14]. The replacement of at least 5% of saturated fatty acids by comparable amounts of PUFAs is the most effective dietary alteration that is consistently possible within usual patterns of eating. This could result in a 10% or more reduction in LDL[57]. Researchers have shifted their focus to discover combinations of natural food, specific nutrients, and other supplements that will decrease LDL concentrations by about 20% and make them affordable to compete with the equally efficacious and cheaper pharmacological interventions that include the use of statins and ezetimibe.
A considerable attrition in blood pressure was observed following an intensive cardiac rehabilitation program[58] that was supplemented by a PBD and psychosocial management. As evinced in this study, a 9%, 14%, and 7% decrease in CAD, stroke, and all-cause mortality could be predicted in response to a decline in systolic blood pressure of 5 mmHg.
In recent times, several ethical, environmental, and health issues have fuelled awareness regarding PBDs on an international scale[57]. A global survey in 2019 reported that 40% of consumers are trying to reduce their consumption of animal proteins, while 10% avoided red meat completely[59]. Table 1 represents the market trends of various countries worldwide. The predilection of meat-loving consumers for products that expressly resemble the taste and texture of real meat has inspirited the transformation of plant-based meat substitutes and the corresponding production technologies, including electro-spinning, high-moisture extrusion cooking, and shear cell technology with the extrusion method, known for their ability to create fibrous structures reminiscent of meat[60]. Plant-based proteins are the most frequently employed elements in replacement meats. Mushrooms, soy, and wheat gluten are the primary ingredients[59]. Cultured meat, a sustainable substitute with mitigated land utilization and an opportunity to expiate nutrient content through amendments in the growth medium, constitutes a single instance of a breakthrough advancement in the domain of PBDs. The global revenue for vegetarian meat substitutes is reckoned to pullulate from United States Dollar 1.6 billion in 2019 to United States Dollar 3.5 billion by 2026[59]. Similar plant-derived proteins are employed to devise seafood alternatives as well as milk substitutes. The Plant-Based Foods Association reports that the demand for plant-based yogurts, cheeses, and creamers has increased by 55%, 43%, and 131%, respectively, in the United States[59]. Another fascinating emergence is microalgae, which are prolific in almost every essential amino acid. Some species even contain an amino acid content strikingly equivalent to the amount found in eggs[59]. Nevertheless, factors like digestibility and bioavailability have an enormous influence on how proficiently these nutrients are adopted. The findings of a study conducted by Jakše et al[32] demonstrate that, even when consumed arbitrarily, transitioning from a modern western-style diet to a low-fat, unrefined whole food PBD supplemented with plant-based meal replacement conduces substantial noteworthy diminution in cardiovascular risk factors. We anticipate continuing to enjoy flavourful food while also expecting future developments in food to be more considerate of the environment. Therefore, we must manufacture the sustenance deploying "precision processing." These are inventive techniques that conform to the available resources at disposal whilst optimizing their quality and function[61].
| Country | Data |
| Germany | Vegetarians increased from 1% in 2005 to 7% in 2018 |
| Italy | The meat-free population has increased by 94.4% from 2011 to 2016 |
| Spain | Flexitarians (vegetarians who occasionally eat food from animals) increased by 25% between 2017-2019 |
| United Kingdom | Twenty-one percent of the population consider themselves flexitarian and 1 in 8 declared being vegetarian or vegan |
| United States | In United States, vegans increased by 500%, from nearly four million in 2014 to 19.6 million in 2017. A national United States survey published in 2018 found that two-thirds of participants had reduced meat consumption between 2015-2018 |
The choice to adopt a PBD is a deliberate and informed decision aimed at maximizing the health benefits per calorie while minimizing potential exposure to harmful substances. The PBD is cardioprotective. A Western diet, however the other hand, is high in sugar, salt, cholesterol, and fat, which can lead to several health problems, including diabetes mellitus, hypertension, high cholesterol levels, obesity, and CAD. The main goal of a PBD is to include more nutrient-dense plant-based foods while consuming less processed food, sugar-added items, fat, and animal products. We examine several speculated mechanisms by which a PBD could help prevent atherosclerosis and CAD incidents.
This includes three factors:
(1) Avoiding VEC injury by consuming foods that are low in sugar, salt, and fat;
(2) In order to reduce the risk of LDL oxidation, boost the consumption of freshly picked produce that is high in antioxidants, including flavonoids and polyphenols;
(3) Reducing macrophage activation by lowering the intake of red meat and preserving a vegan gut microbiome.
Moreover, the effects of PBDs are comparable with pharmacological measures on lipid profiles. This underscores the need to emphasize the importance of dietary interventions, such as PBDs, to prevent CAD and their benefits on economic and environmental sustainability. However, appropriate guidelines are required to clarify ongoing debates as to which is the best among the varied PBDs or whether omnivorous subjects could shift to vegetarianism and experience the health benefits with the same efficacy.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American College of Chest Physician; Society of Critical Care Medicine.
Specialty type: Medicine, research and experimental
Country/Territory of origin: United States
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Jian ZY, China; Lakusic N, Croatia S-Editor: Li L L-Editor: A P-Editor: Li L
| 1. | Casas R, Estruch R, Sacanella E. Influence of Bioactive Nutrients on the Atherosclerotic Process: A Review. Nutrients. 2018;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 2. | Shahjehan RD, Bhutta BS. Coronary Artery Disease. 2023 Feb 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. [PubMed] |
| 3. | Wojda A, Janczy A, Małgorzewicz S. Mediterranean, vegetarian and vegan diets as practical outtakes of EAS and ACC/AHA recommendations for lowering lipid profile. Acta Biochim Pol. 2021;68:41-48. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Kumar A, Chidambaram V, Mehta JL. Vegetarianism, microbiota, and cardiovascular health: looking back, and forward. Eur J Prev Cardiol. 2022;29:1895-1910. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 5. | Vaduganathan M, Mensah GA, Turco JV, Fuster V, Roth GA. The Global Burden of Cardiovascular Diseases and Risk: A Compass for Future Health. J Am Coll Cardiol. 2022;80:2361-2371. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 959] [Reference Citation Analysis (0)] |
| 6. | Kim H, Caulfield LE, Garcia-Larsen V, Steffen LM, Coresh J, Rebholz CM. Plant-Based Diets Are Associated With a Lower Risk of Incident Cardiovascular Disease, Cardiovascular Disease Mortality, and All-Cause Mortality in a General Population of Middle-Aged Adults. J Am Heart Assoc. 2019;8:e012865. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 132] [Cited by in RCA: 261] [Article Influence: 43.5] [Reference Citation Analysis (1)] |
| 7. | Tuso P, Stoll SR, Li WW. A plant-based diet, atherogenesis, and coronary artery disease prevention. Perm J. 2015;19:62-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 96] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 8. | Hansson GK. Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685-1695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6103] [Cited by in RCA: 6340] [Article Influence: 317.0] [Reference Citation Analysis (0)] |
| 9. | Nabel EG, Braunwald E. A tale of coronary artery disease and myocardial infarction. N Engl J Med. 2012;366:54-63. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 661] [Cited by in RCA: 697] [Article Influence: 53.6] [Reference Citation Analysis (0)] |
| 10. | Soltani S, Boozari M, Cicero AFG, Jamialahmadi T, Sahebkar A. Effects of phytochemicals on macrophage cholesterol efflux capacity: Impact on atherosclerosis. Phytother Res. 2021;35:2854-2878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 47] [Article Influence: 11.8] [Reference Citation Analysis (0)] |
| 11. | Wei T, Liu J, Zhang D, Wang X, Li G, Ma R, Chen G, Lin X, Guo X. The Relationship Between Nutrition and Atherosclerosis. Front Bioeng Biotechnol. 2021;9:635504. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 12. | Quek J, Lim G, Lim WH, Ng CH, So WZ, Toh J, Pan XH, Chin YH, Muthiah MD, Chan SP, Foo RSY, Yip J, Neelakantan N, Chong MFF, Loh PH, Chew NWS. The Association of Plant-Based Diet With Cardiovascular Disease and Mortality: A Meta-Analysis and Systematic Review of Prospect Cohort Studies. Front Cardiovasc Med. 2021;8:756810. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 68] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 13. | Makhmudova U, Schulze PC, Lütjohann D, Weingärtner O. Phytosterols and Cardiovascular Disease. Curr Atheroscler Rep. 2021;23:68. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 37] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 14. | Gylling H, Plat J, Turley S, Ginsberg HN, Ellegård L, Jessup W, Jones PJ, Lütjohann D, Maerz W, Masana L, Silbernagel G, Staels B, Borén J, Catapano AL, De Backer G, Deanfield J, Descamps OS, Kovanen PT, Riccardi G, Tokgözoglu L, Chapman MJ; European Atherosclerosis Society Consensus Panel on Phytosterols. Plant sterols and plant stanols in the management of dyslipidaemia and prevention of cardiovascular disease. Atherosclerosis. 2014;232:346-360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 331] [Cited by in RCA: 354] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 15. | Pereira TS, Fonseca FAH, Fonseca MIH, Martins CM, Fonseca HAR, Fonzar WT, Goulart AC, Bensenor IM, Lotufo PA, Izar MC. Phytosterol consumption and markers of subclinical atherosclerosis: Cross-sectional results from ELSA-Brasil. Nutr Metab Cardiovasc Dis. 2021;31:1756-1766. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Cabral CE, Klein MRST. Phytosterols in the Treatment of Hypercholesterolemia and Prevention of Cardiovascular Diseases. Arq Bras Cardiol. 2017;109:475-482. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 38] [Cited by in RCA: 61] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 17. | Oliveira Godoy Ilha A, Sutti Nunes V, Silva Afonso M, Regina Nakandakare E, da Silva Ferreira G, de Paula Assis Bombo R, Rodrigues Giorgi R, Marcondes Machado R, Carlos Rocha Quintão E, Lottenberg AM. Phytosterols Supplementation Reduces Endothelin-1 Plasma Concentration in Moderately Hypercholesterolemic Individuals Independently of Their Cholesterol-Lowering Properties. Nutrients. 2020;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 14] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Kaur R, Myrie SB. Association of Dietary Phytosterols with Cardiovascular Disease Biomarkers in Humans. Lipids. 2020;55:569-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 19. | Brzeska M, Szymczyk K, Szterk A. Current Knowledge about Oxysterols: A Review. J Food Sci. 2016;81:R2299-R2308. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 56] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 20. | O'Callaghan Y, McCarthy FO, O'Brien NM. Recent advances in Phytosterol Oxidation Products. Biochem Biophys Res Commun. 2014;446:786-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 56] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 21. | Brown RB. Phospholipid packing defects and oxysterols in atherosclerosis: Dietary prevention and the French paradox. Biochimie. 2019;167:145-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 22. | Luister A, Schött HF, Husche C, Schäfers HJ, Böhm M, Plat J, Gräber S, Lütjohann D, Laufs U, Weingärtner O. Increased plant sterol deposition in vascular tissue characterizes patients with severe aortic stenosis and concomitant coronary artery disease. Steroids. 2015;99:272-280. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 23. | Nunes VS, de Campos EVS, Baracat J, França V, Gomes ÉIL, Coelho RP, Nakandakare ER, Zago VHS, de Faria EC, Quintão ECR. Plasma Campesterol Is Positively Associated with Carotid Plaques in Asymptomatic Subjects. Int J Mol Sci. 2022;23. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 24. | Padro T, Vilahur G, Sánchez-Hernández J, Hernández M, Antonijoan RM, Perez A, Badimon L. Lipidomic changes of LDL in overweight and moderately hypercholesterolemic subjects taking phytosterol- and omega-3-supplemented milk. J Lipid Res. 2015;56:1043-1056. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 25. | Upadhyay S, Dixit M. Role of Polyphenols and Other Phytochemicals on Molecular Signaling. Oxid Med Cell Longev. 2015;2015:504253. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 207] [Cited by in RCA: 227] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 26. | Kuchta A, Lebiedzińska A, Fijałkowski M, Gałąska R, Kreft E, Totoń M, Czaja K, Kozłowska A, Ćwiklińska A, Kortas-Stempak B, Strzelecki A, Gliwińska A, Dąbkowski K, Jankowski M. Impact of plant-based diet on lipid risk factors for atherosclerosis. Cardiol J. 2016;23:141-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 27. | Rosa Cde O, Dos Santos CA, Leite JI, Caldas AP, Bressan J. Impact of nutrients and food components on dyslipidemias: what is the evidence? Adv Nutr. 2015;6:703-711. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 30] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 28. | Mooradian AD, Haas MJ. The effect of nutritional supplements on serum high-density lipoprotein cholesterol and apolipoprotein A-I. Am J Cardiovasc Drugs. 2014;14:253-274. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 29. | Salehin S, Rasmussen P, Mai S, Mushtaq M, Agarwal M, Hasan SM, Salehin S, Raja M, Gilani S, Khalife WI. Plant Based Diet and Its Effect on Cardiovascular Disease. Int J Environ Res Public Health. 2023;20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 32] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 30. | Hever J, Cronise RJ. Plant-based nutrition for healthcare professionals: implementing diet as a primary modality in the prevention and treatment of chronic disease. J Geriatr Cardiol. 2017;14:355-368. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 37] [Reference Citation Analysis (0)] |
| 31. | Ganguli SC, Russell LA, Tsoi KS. Implementation of a Whole Food Plant Based Diet in a Food as Prevention Program in a Resource Constrained Environment. J Lifestyle Med. 2022;12:148-152. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 32. | Jakše B, Jakše B, Pajek J, Pajek M. Effects of ad libitum consumed, low-fat, high-fiber plant-based diet supplemented with plant-based meal replacements on cardiovascular risk factors. Food Nutr Res. 2019;63. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 33. | Vinagre JC, Vinagre CG, Pozzi FS, Slywitch E, Maranhão RC. Metabolism of triglyceride-rich lipoproteins and transfer of lipids to high-density lipoproteins (HDL) in vegan and omnivore subjects. Nutr Metab Cardiovasc Dis. 2013;23:61-67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 34. | Kaiser J, van Daalen KR, Thayyil A, Cocco MTARR, Caputo D, Oliver-Williams C. A Systematic Review of the Association Between Vegan Diets and Risk of Cardiovascular Disease. J Nutr. 2021;151:1539-1552. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 24] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 35. | Sanchez A, Mejia A, Sanchez J, Runte E, Brown-Fraser S, Bivens RL. Diets with customary levels of fat from plant origin may reverse coronary artery disease. Med Hypotheses. 2019;122:103-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 36. | Gogga P, Sliwińska A, Aleksandrowicz-Wrona E, Malgorzewicz S. Lipid profile in Polish women following lacto-ovo-vegetarian and vegan diets - preliminary study. Acta Biochim Pol. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 37. | Woo KS, Kwok TC, Celermajer DS. Vegan diet, subnormal vitamin B-12 status and cardiovascular health. Nutrients. 2014;6:3259-3273. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 38. | Ferrari CKB. Anti-atherosclerotic and cardiovascular protective benefits of Brazilian nuts. Front Biosci (Schol Ed). 2020;12:38-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 39. | Yu X, Chu M, Chu C, Du Y, Shi J, Liu X, Liu Y, Zhang H, Zhang Z, Yan N. Wild rice (Zizania spp.): A review of its nutritional constituents, phytochemicals, antioxidant activities, and health-promoting effects. Food Chem. 2020;331:127293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 32] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 40. | Deplanque X, Muscente-Paque D, Chappuis E. Proprietary tomato extract improves metabolic response to high-fat meal in healthy normal weight subjects. Food Nutr Res. 2016;60:32537. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 41. | Chen J, Huang Q, Li J, Yao Y, Sun W, Zhang Z, Qi H, Chen Z, Liu J, Zhao D, Mi J, Li X. Panax ginseng against myocardial ischemia/reperfusion injury: A review of preclinical evidence and potential mechanisms. J Ethnopharmacol. 2023;300:115715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 21] [Article Influence: 10.5] [Reference Citation Analysis (1)] |
| 42. | Vinagre JC, Vinagre CC, Pozzi FS, Zácari CZ, Maranhão RC. Plasma kinetics of chylomicron-like emulsion and lipid transfers to high-density lipoprotein (HDL) in lacto-ovo vegetarian and in omnivorous subjects. Eur J Nutr. 2014;53:981-987. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 43. | Koch CA, Kjeldsen EW, Frikke-Schmidt R. Vegetarian or vegan diets and blood lipids: a meta-analysis of randomized trials. Eur Heart J. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 51] [Reference Citation Analysis (0)] |
| 44. | Craddock JC, Probst YC, Neale EP, Geraghty N, Peoples GE. A comparison of diet quality and cardiovascular and inflammatory responses between aerobically trained male adults following either a long-term vegan or omnivorous dietary pattern. Nutr Bull. 2023;48:227-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 45. | Smits LP, Kootte RS, Levin E, Prodan A, Fuentes S, Zoetendal EG, Wang Z, Levison BS, Cleophas MCP, Kemper EM, Dallinga-Thie GM, Groen AK, Joosten LAB, Netea MG, Stroes ESG, de Vos WM, Hazen SL, Nieuwdorp M. Effect of Vegan Fecal Microbiota Transplantation on Carnitine- and Choline-Derived Trimethylamine-N-Oxide Production and Vascular Inflammation in Patients With Metabolic Syndrome. J Am Heart Assoc. 2018;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 156] [Cited by in RCA: 173] [Article Influence: 24.7] [Reference Citation Analysis (0)] |
| 46. | Bhupathiraju SN, Guasch-Ferré M, Gadgil MD, Newgard CB, Bain JR, Muehlbauer MJ, Ilkayeva OR, Scholtens DM, Hu FB, Kanaya AM, Kandula NR. Dietary Patterns among Asian Indians Living in the United States Have Distinct Metabolomic Profiles That Are Associated with Cardiometabolic Risk. J Nutr. 2018;148:1150-1159. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 47. | Storz MA, Helle P. Atrial fibrillation risk factor management with a plant-based diet: A review. J Arrhythm. 2019;35:781-788. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 48. | Penson PE, Banach M. Natural compounds as anti-atherogenic agents: Clinical evidence for improved cardiovascular outcomes. Atherosclerosis. 2021;316:58-65. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 49. | Bhupathiraju SN, Sawicki CM, Goon S, Gujral UP, Hu FB, Kandula NR, Kanaya AM. A healthy plant-based diet is favorably associated with cardiometabolic risk factors among participants of South Asian ancestry. Am J Clin Nutr. 2022;116:1078-1090. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 35] [Article Influence: 11.7] [Reference Citation Analysis (0)] |
| 50. | Kim H, Rebholz CM, Garcia-Larsen V, Steffen LM, Coresh J, Caulfield LE. Operational Differences in Plant-Based Diet Indices Affect the Ability to Detect Associations with Incident Hypertension in Middle-Aged US Adults. J Nutr. 2020;150:842-850. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 47] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 51. | Wang D, Chen X, Li Z, Luo Y. Association of the gut microbiota with coronary artery disease and myocardial infarction: A Mendelian randomization study. Front Genet. 2023;14:1158293. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 52. | Rocha VZ, Ras RT, Gagliardi AC, Mangili LC, Trautwein EA, Santos RD. Effects of phytosterols on markers of inflammation: A systematic review and meta-analysis. Atherosclerosis. 2016;248:76-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 70] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 53. | Windler E, Beil FU, Berthold HK, Gouni-Berthold I, Kassner U, Klose G, Lorkowski S, März W, Parhofer KG, Plat J, Silbernagel G, Steinhagen-Thiessen E, Weingärtner O, Zyriax BC, Lütjohann D. Phytosterols and Cardiovascular Risk Evaluated against the Background of Phytosterolemia Cases-A German Expert Panel Statement. Nutrients. 2023;15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 54. | Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella-Tommasino J, Forman DE, Goldberg R, Heidenreich PA, Hlatky MA, Jones DW, Lloyd-Jones D, Lopez-Pajares N, Ndumele CE, Orringer CE, Peralta CA, Saseen JJ, Smith SC Jr, Sperling L, Virani SS, Yeboah J. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082-e1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 678] [Cited by in RCA: 1456] [Article Influence: 242.7] [Reference Citation Analysis (1)] |
| 55. | Mach F, Baigent C, Catapano AL, Koskinas KC, Casula M, Badimon L, Chapman MJ, De Backer GG, Delgado V, Ference BA, Graham IM, Halliday A, Landmesser U, Mihaylova B, Pedersen TR, Riccardi G, Richter DJ, Sabatine MS, Taskinen MR, Tokgozoglu L, Wiklund O; ESC Scientific Document Group. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: lipid modification to reduce cardiovascular risk. Eur Heart J. 2020;41:111-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6024] [Cited by in RCA: 5357] [Article Influence: 1071.4] [Reference Citation Analysis (0)] |
| 56. | Gomes GB, Zazula AD, Shigueoka LS, Fedato RA, da Costa AB, Guarita-Souza LC, Baena CP, Olandoski M, Faria-Neto JR. A Randomized Open-Label Trial to Assess the Effect of Plant Sterols Associated with Ezetimibe in Low-Density Lipoprotein Levels in Patients with Coronary Artery Disease on Statin Therapy. J Med Food. 2017;20:30-36. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 57. | Nestel PJ, Mori TA. A Review of Low-Density Lipoprotein-Lowering Diets in the Age of Anti-Sense Technology. Nutrients. 2023;15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (1)] |
| 58. | Świątkiewicz I, Di Somma S, De Fazio L, Mazzilli V, Taub PR. Effectiveness of Intensive Cardiac Rehabilitation in High-Risk Patients with Cardiovascular Disease in Real-World Practice. Nutrients. 2021;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 28] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 59. | Alcorta A, Porta A, Tárrega A, Alvarez MD, Vaquero MP. Foods for Plant-Based Diets: Challenges and Innovations. Foods. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 314] [Cited by in RCA: 227] [Article Influence: 56.8] [Reference Citation Analysis (1)] |
| 60. | Arwanto V, Buschle-Diller G, Mukti YP, Dewi ADR, Mumpuni C, Purwanto MGM, Sukweenadhi J. The state of plant-based food development and its prospects in the Indonesia market. Heliyon. 2022;8:e11062. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 61. | Menta R, Rosso G, Canzoneri F. Plant-Based: A Perspective on Nutritional and Technological Issues. Are We Ready for "Precision Processing"? Front Nutr. 2022;9:878926. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 5] [Article Influence: 1.7] [Reference Citation Analysis (0)] |