Published online Jun 6, 2023. doi: 10.12998/wjcc.v11.i16.3870
Peer-review started: February 24, 2023
First decision: March 24, 2023
Revised: April 14, 2023
Accepted: May 4, 2023
Article in press: May 4, 2023
Published online: June 6, 2023
Processing time: 98 Days and 3.7 Hours
Dextromethorphan is a prevalent antitussive agent that can be easily obtained as an over-the-counter medication. There has been a growing number of reported cases of toxicity in recent years. Generally, there are numerous instances of mild symptoms, with only a limited number of reports of severe cases necessitating intensive care. We presented the case of a female who ingested 111 tablets of dextromethorphan, leading to shock and convulsions and requiring intensive care that ultimately saved her life.
A 19-year-old female was admitted to our hospital via ambulance, having overdosed on 111 tablets of dextromethorphan (15 mg) obtained through an online importer in a suicide attempt. The patient had a history of drug abuse and multiple self-inflicted injuries. At the time of admission, she exhibited symptoms of shock and altered consciousness. However, upon arrival at the hospital, the patient experienced recurrent generalized clonic convulsions and status epilepticus, necessitating tracheal intubation. The convulsions were determined to have been caused by decreased cerebral perfusion pressure secondary to shock, and noradrenaline was administered as a vasopressor. Gastric lavage and activated charcoal were also administered after intubation. Through systemic management in the intensive care unit, the patient’s condition stabilized, and the need for vasopressors ceased. The patient regained consciousness and was extubated. The patient was subsequently transferred to a psychiatric facility, as suicidal ideation persisted.
We report the first case of shock caused by an overdose of dextromethorphan.
Core Tip: Prior studies have posited that dextromethorphan acts as a voltage-gated calcium channel inhibitor, one of its mechanisms of action. It is possible that the high dose in the present case amplified this effect. Previous reports attributed fatalities to central nervous system and respiratory depression, yet shock may also be a contributing factor, as evidenced by this case. This may be a rare occurrence, as it was only observed in the emergency room. We reported the first case of shock caused by an overdose of dextromethorphan. We were able to save the patient’s life in intensive care.
- Citation: Shimozawa S, Usuda D, Sasaki T, Tsuge S, Sakurai R, Kawai K, Matsubara S, Tanaka R, Suzuki M, Hotchi Y, Tokunaga S, Osugi I, Katou R, Ito S, Asako S, Mishima K, Kondo A, Mizuno K, Takami H, Komatsu T, Oba J, Nomura T, Sugita M. High doses of dextromethorphan induced shock and convulsions in a 19-year-old female: A case report. World J Clin Cases 2023; 11(16): 3870-3876
- URL: https://www.wjgnet.com/2307-8960/full/v11/i16/3870.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i16.3870
Dextromethorphan is a readily obtainable and broadly used over-the-counter antitussive drug, and recent years have seen more and more poisoning cases related to dextromethorphan consumption[1-5]. Recreational dextromethorphan consumption in the United States is prevalent among younger generations. Each year, roughly a million individuals aged 12-25 years abuse it non-medicinally[6]. As a result, there are over 6000 emergency department visits in the United States each year caused by dextromethorphan abuse, and half of all dextromethorphan-toxicity-caused emergency department visits occurred in patients aged 12-20 years[7]. Other countries, including Canada, Germany, Thailand, South Korea, and Japan, have also documented similar increases in dextromethorphan abuse cases[8-12].
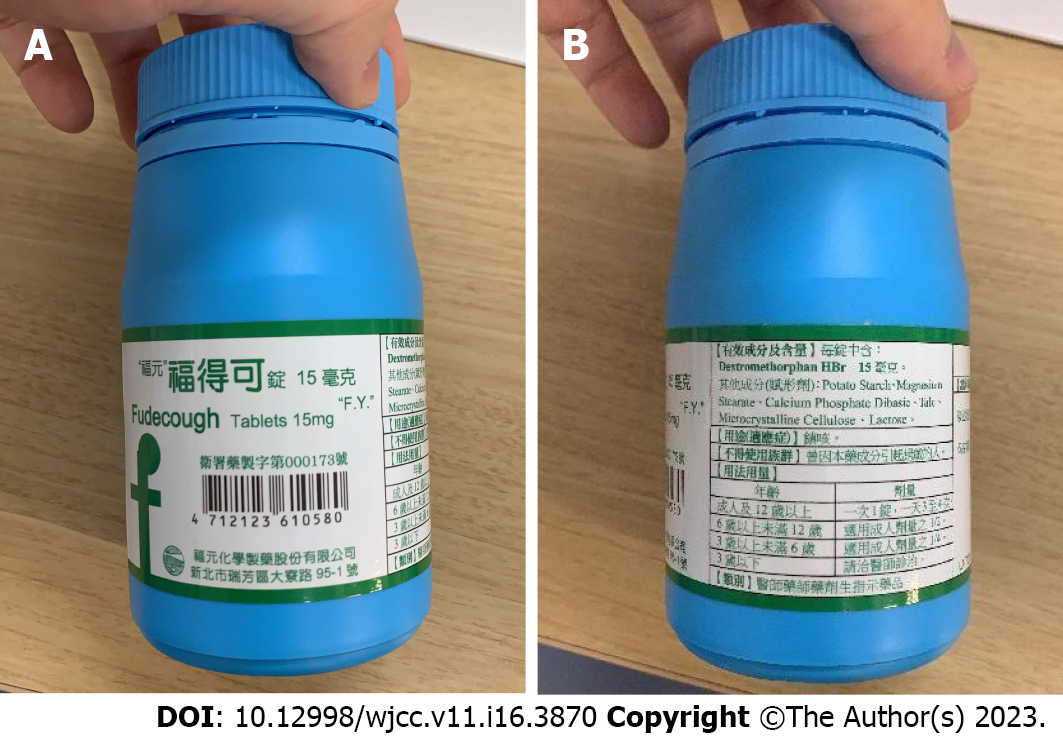
More broadly, there have been many instances involving mild symptoms; only a small fraction of these reports are for severe cases that necessitated intensive care[13]. We presented the case of a female who ingested 111 tablets of dextromethorphan of Chinese origin, leading to shock and convulsions. She was transported to the emergency room (ER) and requiring intensive care, which ultimately saved her life. We also reported the first case of shock caused by an overdose of dextromethorphan (Figure 1).
A 19-year-old Japanese female presented to the ER with a complaint of disturbance of consciousness.
The symptoms started 2 h before presentation.
The patient ingested 111 tablets of dextromethorphan (15 mg) of Chinese origin, obtained through an online importer, in a suicide attempt approximately 2 h prior to presentation. The patient’s boyfriend discovered that she was lethargic. Once he saw an empty medication bottle, the patient was promptly transported to our hospital via ambulance.
The patient had a history of previous drug overdose and multiple self-inflicted injuries resulting from jumping.
Upon physical examination, vital signs were as follows: body temperature of 37.7 °C; blood pressure of 82/44 mmHg; heart rate of 120 beats per minute; respiratory rate of 16 breaths per minute; E4V2M4/GCS10; and oxygen saturation of 96% on room air. The radial artery was barely perceptible upon palpation; nonetheless, the extremities were warm.
Her skin was dry, and her pupils were 6 mm/6 mm and reactive. She was drowsy and had difficulty conversing. The muscle tone in her limbs was normal, with no stiffness.
Serum creatine phosphokinase was 106 U/L, and white blood count was 10100/mm3. The remainder of the complete blood count, prothrombin time, liver function tests, electrolytes, blood urea nitrogen and creatinine were all within normal limits.
Findings from venous blood gas analysis indicated lactic acidosis, likely correlated with shock or seizures (pH 7.114, pCO2 46.1 mmHg, HCO3- 14.8 mmol/L, Glu 65 mg/dL, Lac 12.4 mmol/L). A basic drug screen (SIGNIFY ER) was negative for all drugs. No increase in anion gap or osmotic pressure gap was observed.
Echocardiography in the ER demonstrated adequate cardiac contractility (ejection fraction) of 50% or above and an inferior vena cava diameter of 10/6 mm. On a body computed tomography (CT) scan about 2 h after taking the pills, a hyper-dense area in her stomach that was thought to be a drug clot was found. On a brain CT scan, there were no significant findings. An electrocardiogram showed sinus tachycardia, with a QRS of 119 ms and a QTc of 426 ms, without ischemic changes.
Acute drug intoxication with dextromethorphan.
Upon arrival, the patient presented with symptoms of shock and altered consciousness; a significant infusion of extracellular fluid was swiftly initiated. The patient later developed recurrent generalized convulsions and status epilepticus, necessitating endotracheal intubation. We initiated the administration of noradrenaline as a vasopressor. Continuous administration of noradrenaline (maximum 0.2 μg/kg/min) increased blood pressure and halted the convulsions. A plain CT scan revealed a hyper-dense area in the patient’s stomach, thought to be a drug clot, approximately 2 h post-ingestion. Subsequently, gastric lavage was performed, and activated charcoal was administered.
After admission to the intensive care unit and comprehensive management, we reduced the dose of vasopressors while confirming that mean arterial pressure was maintained at 65 mmHg or higher. On the 2nd hospital day, vasopressors were discontinued, and the patient was extubated because she was alert. Despite her overall stable condition, the patient was transferred to a psychiatric facility on the 3rd hospital day due to persistent suicidal ideation.
Dextromethorphan has long been utilized as an over-the-counter cough suppressant, available in various forms, including oral strips, lozenges, liquids and liquid-filled capsules, and in various formulations. The precise mechanism by which it suppresses coughing remains unclear. Despite structural similarities to opioid agonists, dextromethorphan does not exhibit significant activity at opioid receptors. Dextromethorphan acts on agonism at Sigma-1 receptors and is efficacious as an antitussive to an extent comparable to codeine but without the analgesic or habit-forming characteristics of codeine[14]. Dextromethorphan is a medication with a well-established safety profile when used in therapeutic doses[15].
In humans, dextromethorphan distribution volume is believed to be 5.0-6.7 L/kg[7]. Its protein binding rate is 65%[16]. The serum concentration of dextromethorphan peaks 2.5 h post-ingestion. The primary metabolite of dextromethorphan, dextrorphan, reaches peak plasma concentrations between 1.6-1.7 h after oral administration. The elimination half-life of the parent compound is approximately 2-4 h in individuals with typical metabolic function. Dextromethorphan and its metabolites are primarily excreted through renal elimination, with only very small amounts of fecal excretion[15].
Approximately 90% of individuals, classified as extensive metabolizers, experience rapid and extensive first-pass metabolism of dextromethorphan, resulting in the formation of the major O-demethylated metabolite dextrorphan, mediated by the enzyme CYP2D6. It is vital to note that the enzyme CYP2D6 is polymorphically expressed; some individuals lack activity (known as poor metabolizers), and others express enzyme activity at varying levels[15,17].
The dissociative properties of dextromethorphan are similar to those of ketamine and phencyclidine, owing to the cyclohexane ring and alkylated amine (features common in dissociative agents) found in its structure[18,19]. Dextromethorphan, in higher doses, has a mechanism of action similar to those of phencyclidine and ketamine, in that it antagonizes N-methyl-D-aspartic acid receptors by binding to the calcium ion channel. Blocking the N-methyl-D-aspartic acid receptors modulates excitatory neurotransmission, which brings about hallucinations, euphoria, dissociation, agitation, coma, “out-of-body” experiences and other neurobehavioral effects[1,7,20-22]. Additionally, dextromethorphan inhibits peripheral and central uptake of catecholamine, leading to adrenergic effects such as hypertension, tachycardia and diaphoresis[23]. The life-threatening toxicity associated with dextromethorphan abuse is caused by serotonin syndrome. Because of its serotonin reuptake inhibition properties, dextromethorphan can potentiate excessive body serotonin levels when used along with common prescription selective serotonin reuptake inhibitors or monoamine oxidase inhibitors, which can cause serotonin syndrome to develop[24-26].
Additionally, studies have identified various sites of action at which dextromethorphan and its metabolite dextrorphan interact, including antagonism at nicotinic receptors (a3b4, a4b2, a7), inhibiting serotonin and norepinephrine transporters and inhibiting voltage-gated calcium channels[24]. Other research has found that distinct symptoms occur within specific dosage ranges, which are known as plateaus[18]. Plateau 1 (100–250 mg) elicits a mild stimulant effect similar to that of methylenedioxyamphetamine. Plateau 2 (250–400 mg) is characterized by effects similar to concurrent ethanol and marijuana use, with some individuals experiencing hallucinations. Plateau 3 (450–800 mg) is associated with a dissociative “out-of-body” state akin to that produced by low recreational doses of ketamine. Plateau 4 (> 800 mg) produces a fully dissociative condition similar to ketamine intoxication. Dosages above 1800 mg have been associated with death. A unique study, based on comments left on YouTube videos, also lends credence to these findings[6].
The altered cognitive state brought about by dextromethorphan can lead to injuries. Therefore, a comprehensive assessment for indications of trauma should be a part of examinations[27]. Furthermore, the dissociative and hallucinogenic effects have been reported to potentially lead to suicide, assault and homicide among individuals who are addicted to the drug[28,29]. There are no definitive diagnostic tests for dextromethorphan poisoning, despite its widespread use and potential for abuse. As such, determining diagnoses may be difficult for patients with uncertain medical histories[30,31].
For most patients, dextromethorphan toxicity can be effectively managed through supportive care, including monitoring of the airway, breathing and circulation, and hemodynamic monitoring. In some cases, airway protection may necessitate intubation with ventilator support, and sedation using medication and physical restraints may prove necessary in order to control agitation, violent behavior, and psychosis[32]. When administered within an hour of ingestion, gastrointestinal decontamination with activated charcoal is the most effective treatment for dextromethorphan overdose. Naloxone may serve as a treatment for respiratory depression and central nervous system depression, but reports on its efficacy remain controversial[33]. Due to the large volume of distribution and high protein binding rate of dextromethorphan, blood purification therapy is considered to be less effective for dextromethorphan toxicity.
In this instance, the convulsions were believed to have transpired as a result of a decline in cerebral perfusion pressure owing to shock. The possibility of distributive shock was considered, based on physical and echocardiographic findings. No elevation in blood pressure was detected, despite the administration of a significant volume of extracellular fluid. However, the infusion of noradrenaline raised the patient’s blood pressure and terminated the convulsive activity. Without appropriate treatment, the patient would have likely suffered cardiac arrest.
Although the possibility of symptoms arising from other drugs or additives cannot be ruled out, there have been no documented cases thus far (to the best of our knowledge) of shock resulting from dextromethorphan poisoning. Previous research has proposed that dextromethorphan functions as a voltage-gated calcium channel inhibitor among its potential sites of action. To date, no studies have shown sufficient evidence that these receptors are meaningfully activated by therapeutic doses[34]. However, in this particular case, it is feasible that the high dose of 1665 mg, administered orally, augmented the calcium channel inhibitory effect. Blood purification was not deemed necessary, as the convulsions were swiftly mitigated through hemodynamic stabilization. However, it may prove efficacious in the event of severe symptoms.
Given that the patient in question was a petite woman, it is plausible that the dose of dextromethorphan in this scenario could have been lethal. Previous reports have attributed deaths to central nervous system depression and respiratory depression; however, shock may have been the causative factor in this particular instance. It is possible that we were merely fortuitous witnesses in the ER.
We reported the first case of shock caused by an overdose of dextromethorphan. Proper monitoring must be instituted when administrating high doses of dextromethorphan, regardless of stable blood pressure, in anticipation of potential hemodynamic disturbances.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Substance abuse
Country/Territory of origin: Japan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Agrawal A, India; Moldovan CA, Romania S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Burns JM, Boyer EW. Antitussives and substance abuse. Subst Abuse Rehabil. 2013;4:75-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 2. | Bates MLS, Trujillo KA. Use and abuse of dissociative and psychedelic drugs in adolescence. Pharmacol Biochem Behav. 2021;203:173129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 3. | Bryner JK, Wang UK, Hui JW, Bedodo M, MacDougall C, Anderson IB. Dextromethorphan abuse in adolescence: an increasing trend: 1999-2004. Arch Pediatr Adolesc Med. 2006;160:1217-1222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 84] [Cited by in RCA: 73] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Forrester MB. Dextromethorphan abuse in Texas, 2000-2009. J Addict Dis. 2011;30:243-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Banken JA, Foster H. Dextromethorphan. Ann N Y Acad Sci. 2008;1139:402-411. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 41] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Chary M, Park EH, McKenzie A, Sun J, Manini AF, Genes N. Signs & symptoms of Dextromethorphan exposure from YouTube. PLoS One. 2014;9:e82452. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Brown GR, McLaughlin K, Vaughn K. Identifying and treating patients with synthetic psychoactive drug intoxication. JAAPA. 2018;31:1-5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Mutschler J, Koopmann A, Grosshans M, Hermann D, Mann K, Kiefer F. Dextromethorphan withdrawal and dependence syndrome. Dtsch Arztebl Int. 2010;107:537-540. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Armstrong C, Kapolowicz MR. Interventional Study of Dextromethorphan Abuse Within the U.S. Military Community in Okinawa, Japan. Mil Med. 2020;185:e926-e929. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 10. | Manaboriboon B, Chomchai C. Dextromethorphan abuse in Thai adolescents: A report of two cases and review of literature. J Med Assoc Thai. 2005;88 Suppl 8:S242-S245. [PubMed] |
| 11. | Chung H, Park M, Hahn E, Choi H, Lim M. Recent trends of drug abuse and drug-associated deaths in Korea. Ann N Y Acad Sci. 2004;1025:458-464. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 12. | Leos-Toro C, Hammond D, Manske S. A cross-sectional examination of medicinal substance abuse and use of nonmedicinal substances among Canadian youth: findings from the 2012-2013 Youth Smoking Survey. CMAJ Open. 2015;3:E387-E394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Seltzer JA, Sheth SK, Friedland S, Foreman E, Toney C, Raviendran R, McDaniel MA, Lasoff DR. Life-threatening pediatric dextromethorphan polistirex overdose. Am J Emerg Med. 2022;61:233.e1-233.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Carr BC. Efficacy, abuse, and toxicity of over-the-counter cough and cold medicines in the pediatric population. Curr Opin Pediatr. 2006;18:184-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 15. | Taylor CP, Traynelis SF, Siffert J, Pope LE, Matsumoto RR. Pharmacology of dextromethorphan: Relevance to dextromethorphan/quinidine (Nuedexta®) clinical use. Pharmacol Ther. 2016;164:170-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 124] [Article Influence: 13.8] [Reference Citation Analysis (0)] |
| 16. | Pope LE, Khalil MH, Berg JE, Stiles M, Yakatan GJ, Sellers EM. Pharmacokinetics of dextromethorphan after single or multiple dosing in combination with quinidine in extensive and poor metabolizers. J Clin Pharmacol. 2004;44:1132-1142. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 82] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 17. | Silva AR, Dinis-Oliveira RJ. Pharmacokinetics and pharmacodynamics of dextromethorphan: clinical and forensic aspects. Drug Metab Rev. 2020;52:258-282. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 18. | Boyer EW. Dextromethorphan abuse. Pediatr Emerg Care. 2004;20:858-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 55] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 19. | Antoniou T, Juurlink DN. Dextromethorphan abuse. CMAJ. 2014;186:E631. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 20. | Stanciu CN, Penders TM, Rouse EM. Recreational use of dextromethorphan, "Robotripping"-A brief review. Am J Addict. 2016;25:374-377. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Eggleston W, Stork C. Generation Z: Adolescent Xenobiotic Abuse in the 21st Century. Adolesc Med State Art Rev. 2015;26:570-588. [PubMed] |
| 22. | Reissig CJ, Carter LP, Johnson MW, Mintzer MZ, Klinedinst MA, Griffiths RR. High doses of dextromethorphan, an NMDA antagonist, produce effects similar to classic hallucinogens. Psychopharmacology (Berl). 2012;223:1-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 62] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 23. | Ahmed G, Saleem MD, Naim H. How many deaths before we put cough syrups behind the counter? Perspect Public Health. 2014;134:309. [PubMed] |
| 24. | Oh S, Agrawal S, Sabir S, Taylor A. Dextromethorphan. 2022 May 29. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. [PubMed] |
| 25. | Dy P, Arcega V, Ghali W, Wolfe W. Serotonin syndrome caused by drug to drug interaction between escitalopram and dextromethorphan. BMJ Case Rep. 2017;2017. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 26. | Monte AA, Chuang R, Bodmer M. Dextromethorphan, chlorphenamine and serotonin toxicity: case report and systematic literature review. Br J Clin Pharmacol. 2010;70:794-798. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 44] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 27. | Windhab LG, Gastberger S, Hulka LM, Baumgartner MR, Soyka M, Müller TJ, Seifritz E, Mutschler J. Dextromethorphan Abuse Among Opioid-Dependent Patients. Clin Neuropharmacol. 2020;43:127-133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 28. | Logan BK, Yeakel JK, Goldfogel G, Frost MP, Sandstrom G, Wickham DJ. Dextromethorphan abuse leading to assault, suicide, or homicide. J Forensic Sci. 2012;57:1388-1394. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 29. | Modi D, Bhalavat R, Patterson JC 2nd. Suicidal and homicidal behaviors related to dextromethorphan abuse in a middle-aged woman. J Addict Med. 2013;7:143-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 30. | Majlesi N, Lee DC, Ali SS. Dextromethorphan abuse masquerading as a recurrent seizure disorder. Pediatr Emerg Care. 2011;27:210-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 31. | Amaladoss A, O'Brien S. Cough syrup psychosis. CJEM. 2011;13:53-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Chyka PA, Erdman AR, Manoguerra AS, Christianson G, Booze LL, Nelson LS, Woolf AD, Cobaugh DJ, Caravati EM, Scharman EJ, Troutman WG; American Assiciation of Poison Control Centers. Dextromethorphan poisoning: an evidence-based consensus guideline for out-of-hospital management. Clin Toxicol (Phila). 2007;45:662-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 48] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 33. | Romanelli F, Smith KM. Dextromethorphan abuse: clinical effects and management. J Am Pharm Assoc (2003). 2009;49:e20-5; quiz e26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 34. | Kazis A, Kimiskidis V, Niopas I. Pharmacokinetics of dextromethorphan and dextrorphan in epileptic patients. Acta Neurol Scand. 1996;93:94-98. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |