Published online May 26, 2023. doi: 10.12998/wjcc.v11.i15.3612
Peer-review started: February 7, 2023
First decision: March 14, 2023
Revised: March 27, 2023
Accepted: April 13, 2023
Article in press: April 13, 2023
Published online: May 26, 2023
Processing time: 107 Days and 1.2 Hours
Radicular cysts are one of the most common odontogenic cystic lesions found in the jaw. Nonsurgical treatment of large radicular cysts is a topic of ongoing debate, and there is still no clear consensus on the most effective therapies. The apical negative pressure irrigation system aspirates the cystic fluid and releases the static pressure in the radicular cyst, representing a minimally invasive approach for decompression. In this case, the radicular cyst was in close proximity to the mandibular nerve canal. We used nonsurgical endodontic treatment with a homemade apical negative pressure irrigation system and the prognosis was good.
A 27-year-old male presented to our Department of General Dentistry with complaints of pain in the mandibular right molar when chewing. The patient had no history of drug allergies or systemic disease. A multidisciplinary management approach was designed and included root canal retreatment with a homemade apical negative pressure irrigation system, deep margin elevation and prosthodontic treatment. According to a 1-year follow-up period, the patient showed a favorable outcome.
This report reveals that nonsurgical treatment with an apical negative pressure irrigation system may provide new insights into the treatment of radicular cysts.
Core Tip: We present a case of a radicular cyst treated through root canal retreatment with a homemade apical negative pressure irrigation system, which had excellent therapeutic effects. This is a minimally invasive technique because it is carried out through root canal access without impinging on anatomic structures, bone, or soft tissues. This case report offers new insight into the treatment of patients with radicular cysts.
- Citation: Chen GP, Zhang YZ, Ling DH. Application of apical negative pressure irrigation in the nonsurgical treatment of radicular cysts: A case report. World J Clin Cases 2023; 11(15): 3612-3618
- URL: https://www.wjgnet.com/2307-8960/full/v11/i15/3612.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i15.3612
Radicular cysts are one of the most common odontogenic cystic lesions found in the jaw[1]. These cysts develop as a result of inflammation in the pulp and periodontium, originating from Malassez's epithelial remnants. They can grow to significant sizes and lead to extensive bone damage[2].
These cysts usually go unnoticed because of their painless nature and small size. Radicular cysts might expand significantly, leading to extensive damage to the surrounding bone and compromising the integrity of the relevant vital teeth. The surgical treatments for radicular cysts include total enucleation, marsupialization or decompression, or a combination of these techniques[3]. In recent years, an increasing number of publications have reported that radicular cysts can be healed by nonsurgical endodontic treatment[4,5]. However, it is controversial whether large radicular cystic lesions can be cured by nonsurgical endodontic treatment[6,7].
In this case report, the radicular cyst was in close proximity to the mandibular nerve canal, and there would be a high risk of damage to the mandibular nerve if surgical treatment was performed. Thus, we performed nonsurgical endodontic treatment with a homemade apical negative pressure irrigation system and achieved a good outcome. The cyst was reconstructed in three dimensions by 3D Slicer 5.0.3 software, and prognosis was evaluated by comparing changes in cyst volume. Nonsurgical treatment of large radicular cysts is a topic of ongoing debate, and there is still no clear consensus on the most effective therapies. This study provides new insight into the treatment and prognostic evaluation of radicular cysts.
A 27-year-old man visited the Department of General Dentistry, the Second Affiliated Hospital of Zhejiang University School of Medicine, and reported that his right mandibular molar was painful when chewing, which had been lasting for two weeks.
The patient experienced pain in the mandibular right molar when chewing for about two weeks.
The patient had undergone root canal treatment and inlay restoration in another hospital 5 years prior. He did not report any systemic illnesses or history of drug allergies, nor did he show any obvious contraindications to dental treatment.
There was no personal or family history reported by the patient.
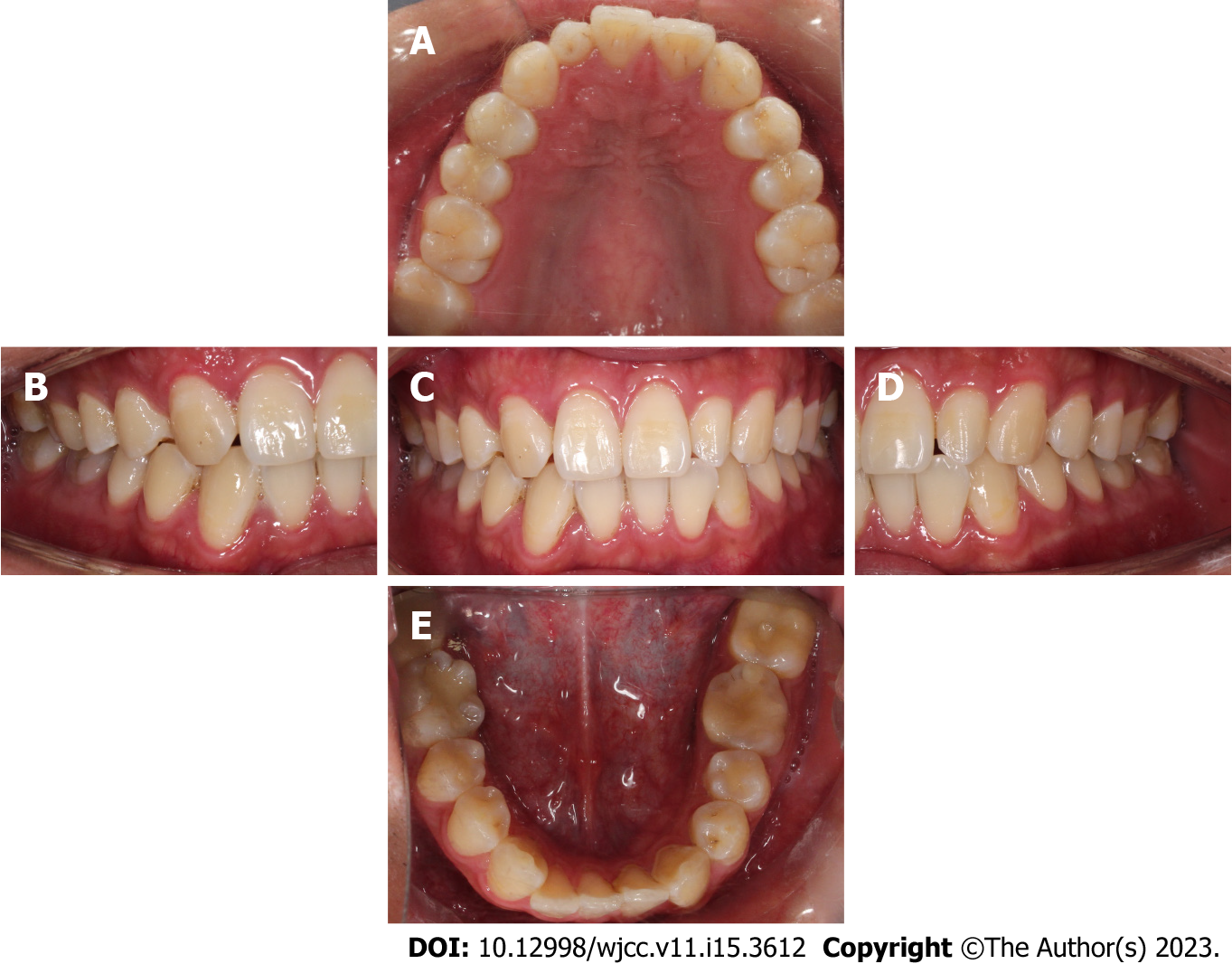
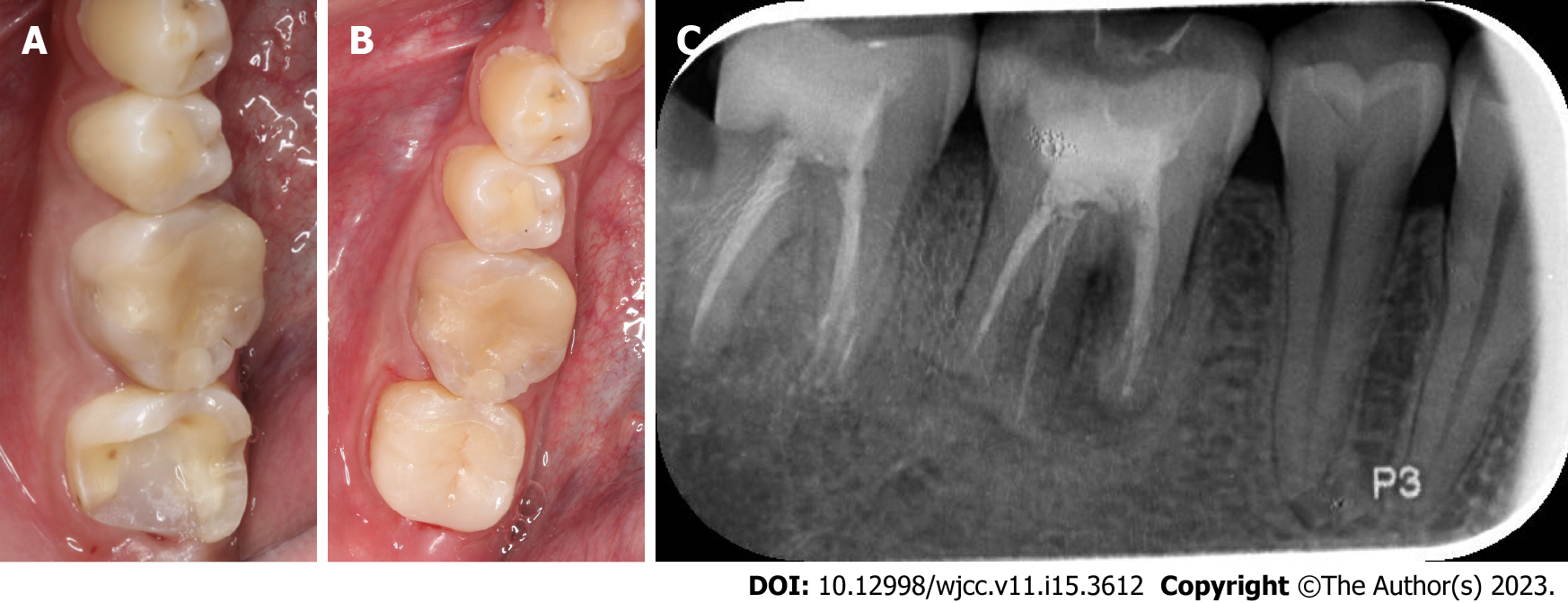
In the clinical examination, tooth 47 had an inlay restoration and showed a sensitive response to percussion. No mobility or swelling was evident. The periodontal probing depth of tooth 47 was < 3.0 mm (Figure 1).
This case did not involve any laboratory examinations.
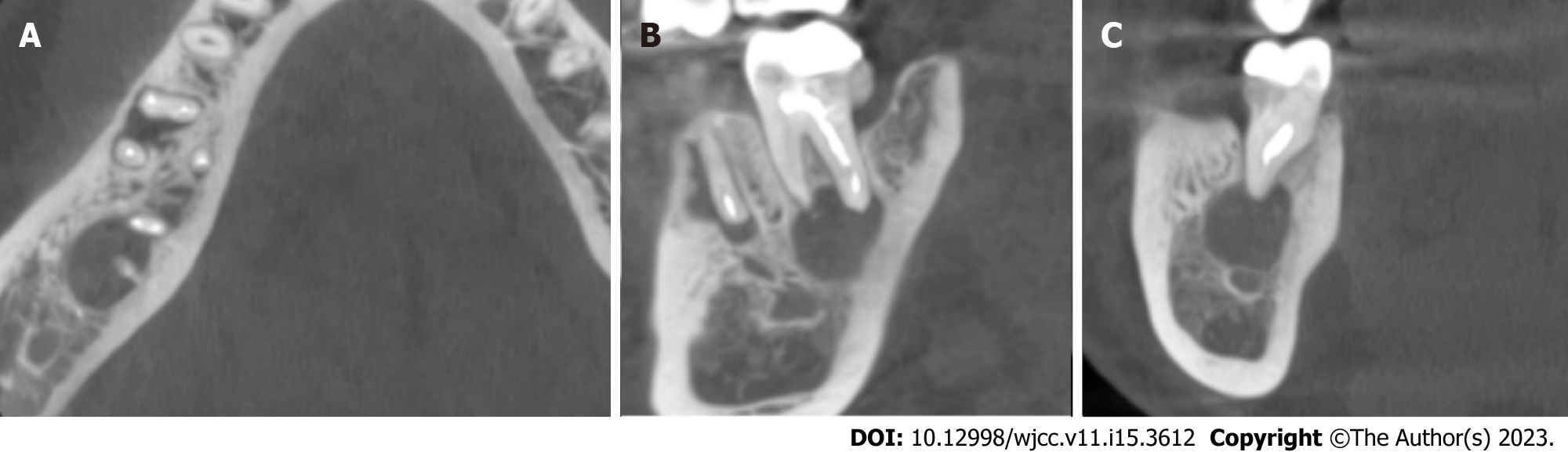
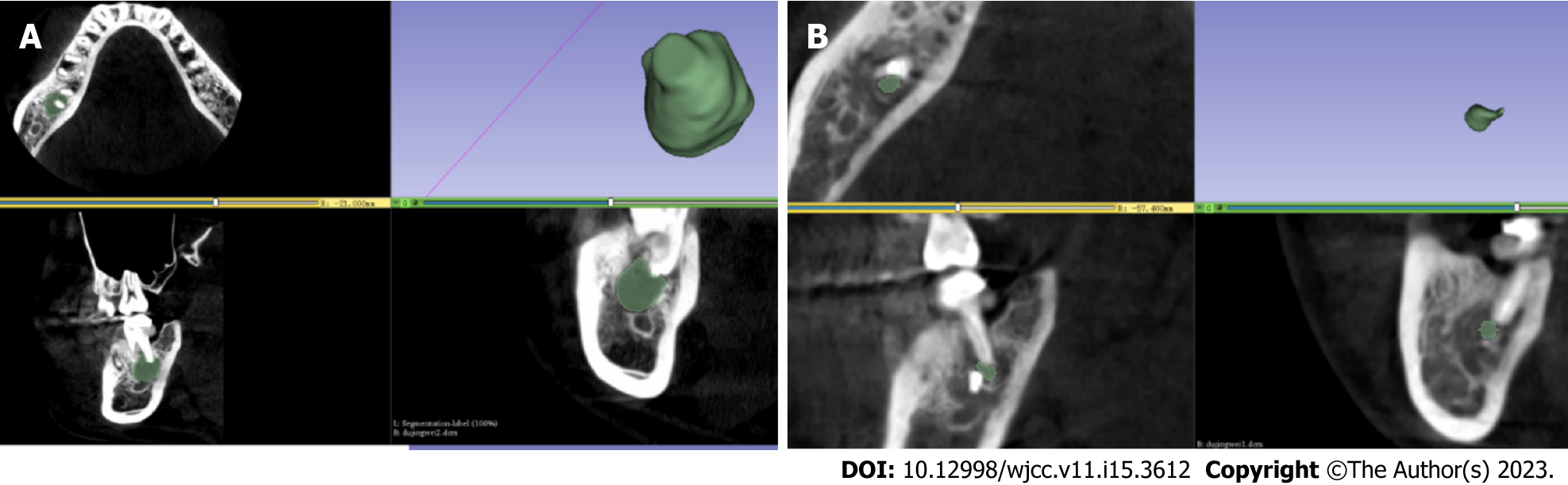
Cone-beam CT scan (Planmeca Romexis Viewer 4.5.0R, Planmeca Oy, Helsinki, Finland) showed a high-density shadow in the root canal of tooth 47 and a 13 mm × 9 mm × 10 mm low-density shadow in the apical region, with clear borders and bone white lines. The filling overhang was visible in the distal cervical region of the tooth (Figure 2).
The tooth was diagnosed with a radicular cyst based on the patient's history, as well as clinical and radiographic examination findings.
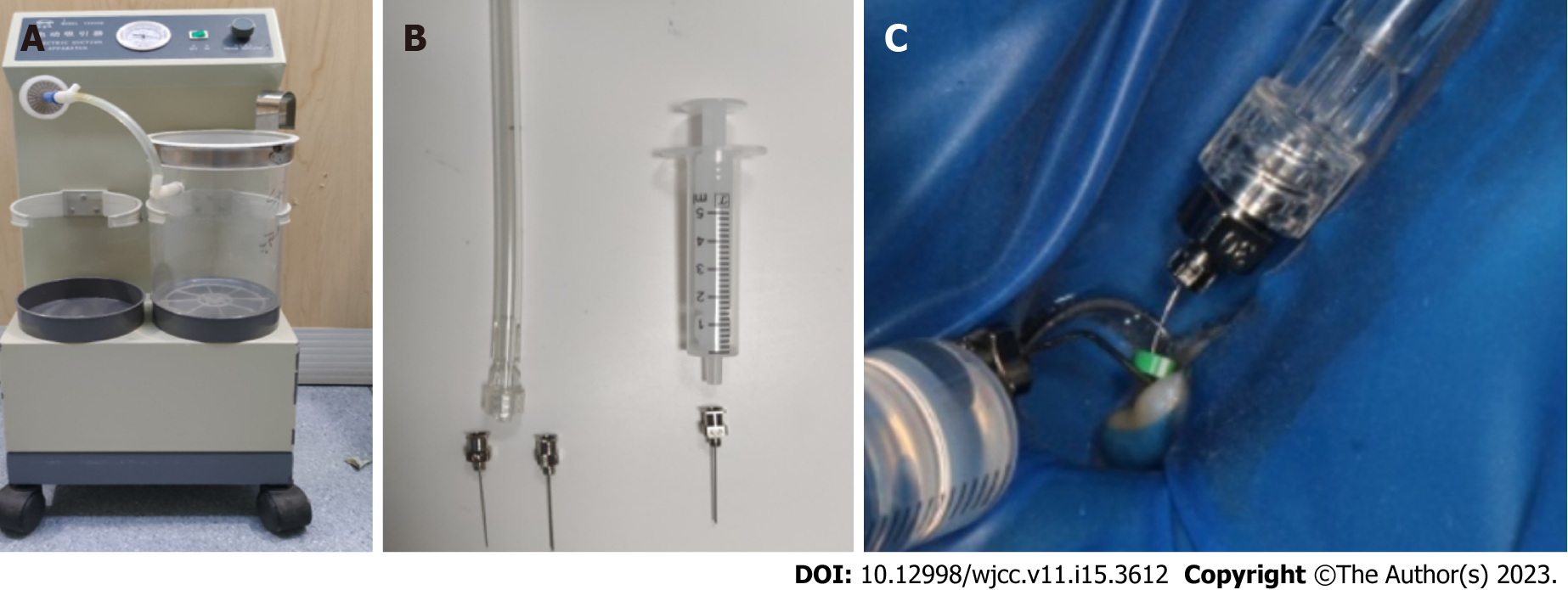
A multidisciplinary management plan was designed, which comprised root canal retreatment with a homemade apical negative pressure irrigation system (Figure 3), deep margin elevation and prosthodontic treatment. The patients were informed about the treatment plan and possible longer-term outcome for tooth 47 and signed an informed consent form.
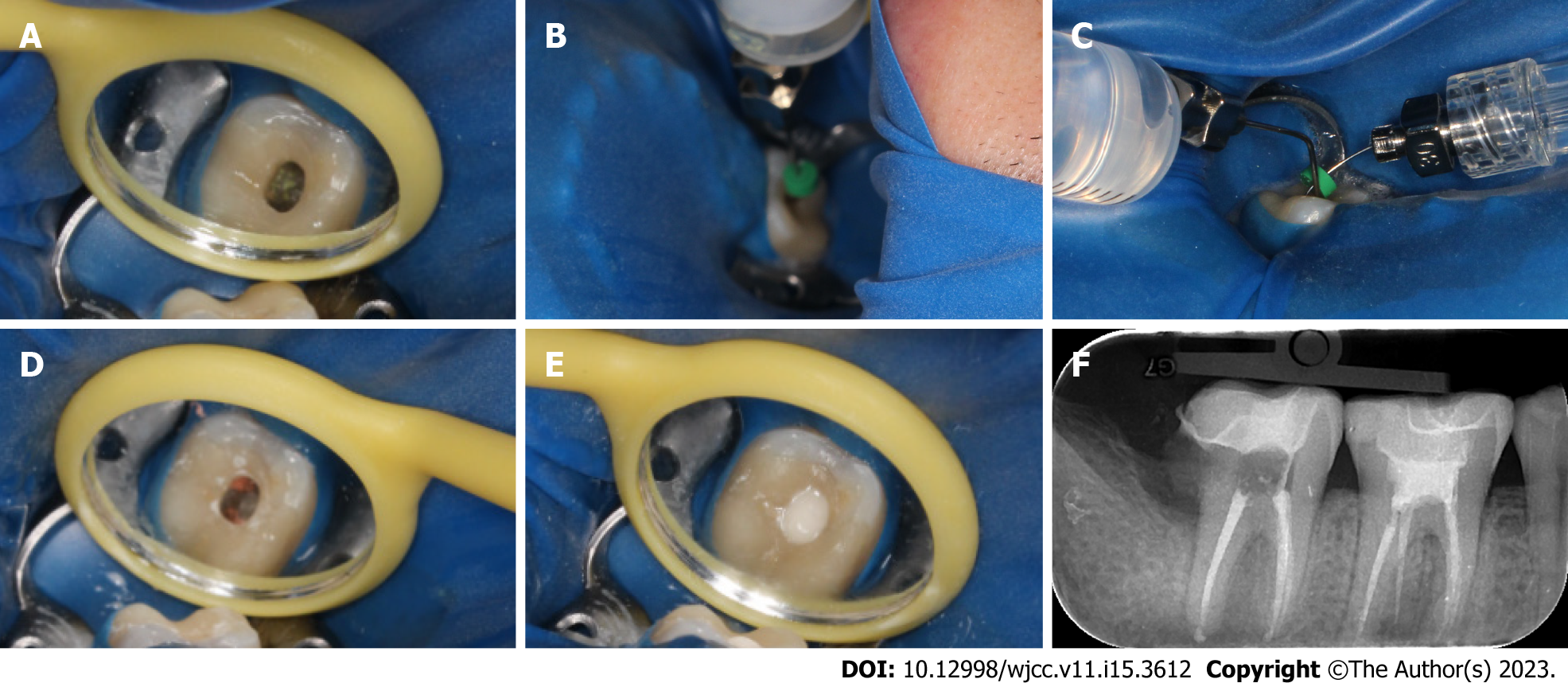
The first step was root canal retreatment. A rubber dam was properly positioned, the access cavity was opened directly on the inlay, and the original filling was removed under a microscope (Figure 4A). A G drill, a K file and Ni-Ti rotary instruments (Dentsply Sirona, Switzerland) were used to remove the root canal fillings. Using electronic apex locator and #8 file to determine the working length, and the canal was then prepareed until a #15 size was achieved. During this step, each K file size went beyond the apical foramen by 2 mm, and a homemade apical negative pressure irrigation system was used to drain the cystic fluid (Figure 4B). The Ni-Ti rotary instruments were selected for root canal preparation with the crown-down preparation method. During the preparation, 1% sodium hypochlorite and 0.9% normal saline were used together with the homemade apical negative pressure irrigation system for irrigation (Figure 4C). The canals were dehydrated using paper points, followed by the application of a paste made of calcium hydroxide [Ca(OH)2]. Finally, the access cavity was sealed with Cavit™.
At 2 wk postoperation, the patient experienced no pain upon percussion. The single cone technique was used to fill the canal with gutta-percha (Gapadent, Tianjin, China) and iRoot SP (Innovative BioCeramix, Vancouver, BC, Canada) (Figure 4D). The access cavity was then sealed by glass ionomer (GC- Fuji IX Japan) (Figure 4E). A final digital PAX was taken at this time, in which we could see that the canals were well obturated (Figure 4F).
During the 3-mo, 6-mo, and 12-mo follow-up periods, the patient did not report any symptoms. A cone-beam CT scan (Planmeca Romexis Viewer 4.5.0R, Planmeca Oy, Helsinki, Finland) was performed again after 6 months. After exporting the 3D CBCT data, 3D Slicer 5.0.3 software was applied to reconstruct a 3D model of the radicular cyst, which showed that the volume was reduced by approximately 80% (Figure 5). Then, the inlay and filling overhang in the distal cervical region of tooth 47 were removed. Deep margin elevation was performed with Smart Dentin Replacement (Dentsply Sirona, Switzerland) and repaired with lava ultimate high toughness porcelain inlay (3M Dental Products, MN, United States) (Figure 6).
Radicular cysts, as chronic apical periodontitis, are mostly caused by untreated pulpitis and apical periodontitis, incomplete root canal treatment or posttraumatic pulp necrosis without spontaneous symptoms that do not receive timely treatment[8,9]. Radicular cysts have a slow course, with no obvious clinical symptoms other than pain and swelling in some patients, and are closely associated with chronic periradicular granulomas and periradicular abscesses, which can transform into each other. The management of large periapical cyst-like lesions has been the subject of much debate. Treatment options may vary from nonsurgical root canal treatment, endodontic microsurgery, or tooth extraction[10]. The different treatment approaches mainly aimed at eliminating the cystic epithelium while minimizing the potential harm to vital structures. Surgical therapy often causes complications such as destruction of the adjacent teeth and important adjacent anatomical structures.
When managing inflammatory lesions associated with an intracanal infection, it is recommended to adopt a conservative approach. It has been suggested that the main reasons for the failure of root canal therapy to treat some of the larger diameter apical cysts are improper endodontic flushing methods during root preparation, failure to use pharmaceutical solvents, improper selection of endodontic sealants, or unclean root canals[11]. Currently, the most commonly used clinical method for root canal irrigation is syringe irrigation. However, syringe irrigation alone does not provide effective cleaning of the three-dimensional root canal system. From the perspective of hydrodynamics, the syringe can only effectively flush the area 1-2 mm beyond the tip of the needle, so it is not effective in cleaning anatomically restricted areas, especially the lateral root canals, accessory root canal, isthmus, and apical areas affected by the air-blocking phenomena[12]. Since Schoeffel[13] first proposed apical negative pressure irrigation in 2007, increasing attention has been given to the application of apical negative pressure irrigation in root canal therapy. Studies have shown that negative pressure irrigation can reduce the amount of irrigation liquid that spills over the root tip during irrigation, eliminate the apical airlock effect, improve the cleaning efficiency in the area of root canal stenosis and reduce the incidence of postoperative pain[13-15]. In addition, negative pressure in the root canal relieves the static pressure in the radicular cyst, allowing for adequate drainage of the cystic fluid and promoting healing of the cyst[15].
In this case, the radicular cyst was in close proximity to the mandibular nerve canal, and there was a greater risk of damage to the mandibular nerve if surgical treatment was performed. Therefore, this patient was treated with nonsurgical root canal retreatment in combination with a homemade apical negative pressure irrigation system. This conservative method has several advantages, such as less discomfort because no surgical flaps are necessary; In contrast to marsupialization or surgical decompression, it is a minimally invasive technique. The procedure is performed through the root canal access means that patient cooperation is not required, and there is no damage to surrounding anatomic structures, bone, or soft tissues.In addition, this technique also generates proper healing[16].
3D Slicer, a multiplatform software that runs on personal computers, can be extended to enable new algorithms and applications and permits multiple configuring, which range from simple 3D visibility of medical images to different reconstructed and generated images[17]. The patient’s 3D CBCT data were exported before treatment and at the postoperative follow-up, and 3D Slicer software was applied to reconstruct the 3D appearance of the cyst. The prognosis of the radicular cysts after nonsurgical treatment was observed by calculating the volume at different time periods.
We report a case of a radicular cyst that achieved a good prognosis through nonsurgical treatment with an apical negative pressure irrigation system. We utilized CBCT data to generate a 3D model of the radicular cyst with 3D Slicer, and this model enabled us to better evaluate prognosis. This case report offers new insight into the treatment of patients with radicular cysts. Future studies with large samples are needed to evaluate the efficacy of nonsurgical endodontic treatment with apical negative pressure irrigation in patient with radicular cysts.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Grawish ME, Egypt; Rakhshan V, Iran S-Editor: Liu JH L-Editor: A P-Editor: Yuan YY
| 1. | Ramachandran Nair PN, Pajarola G, Schroeder HE. Types and incidence of human periapical lesions obtained with extracted teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1996;81:93-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 219] [Cited by in RCA: 204] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 2. | Lin LM, Huang GT, Rosenberg PA. Proliferation of epithelial cell rests, formation of apical cysts, and regression of apical cysts after periapical wound healing. J Endod. 2007;33:908-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 109] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 3. | Gonzalez SM, Spalding PM, Payne JB, Giannini PJ. A dentigerous cyst associated with bilaterally impacted mandibular canines in a girl: a case report. J Med Case Rep. 2011;5:230. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 4. | Ghorbanzadeh S, Ashraf H, Hosseinpour S, Ghorbanzadeh F. Nonsurgical Management of a Large Periapical Lesion: A Case Report. Iran Endod J. 2017;12:253-256. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 5. | Fernandes M, de Ataide I. Nonsurgical management of periapical lesions. J Conserv Dent. 2010;13:240-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 6. | Lin LM, Ricucci D, Lin J, Rosenberg PA. Nonsurgical root canal therapy of large cyst-like inflammatory periapical lesions and inflammatory apical cysts. J Endod. 2009;35:607-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 89] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 7. | Talpos-Niculescu RM, Popa M, Rusu LC, Pricop MO, Nica LM, Talpos-Niculescu S. Conservative Approach in the Management of Large Periapical Cyst-Like Lesions. A Report of Two Cases. Medicina (Kaunas). 2021;57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 8. | Martins JN, Freitas F, Andre S, Moreira A, Carames J. Very Large Inflammatory Odontogenic Cyst with Origin on a Single Long Time Traumatized Lower Incisor. J Clin Diagn Res. 2015;9:ZD07-ZD10. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Karamifar K, Tondari A, Saghiri MA. Endodontic Periapical Lesion: An Overview on the Etiology, Diagnosis and Current Treatment Modalities. Eur Endod J. 2020;5:54-67. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 10. | Oztan MD. Endodontic treatment of teeth associated with a large periapical lesion. Int Endod J. 2002;35:73-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 11. | Ahmed HM, Al Rayes MH, Saini D. Management and prognosis of teeth with trauma induced crown fractures and large periapical cyst like lesions following apical surgery with and without retrograde filling. J Conserv Dent. 2012;15:77-79. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Tay FR, Gu LS, Schoeffel GJ, Wimmer C, Susin L, Zhang K, Arun SN, Kim J, Looney SW, Pashley DH. Effect of vapor lock on root canal debridement by using a side-vented needle for positive-pressure irrigant delivery. J Endod. 2010;36:745-750. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 269] [Cited by in RCA: 245] [Article Influence: 16.3] [Reference Citation Analysis (0)] |
| 13. | Miller TA, Baumgartner JC. Comparison of the antimicrobial efficacy of irrigation using the EndoVac to endodontic needle delivery. J Endod. 2010;36:509-511. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 30] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 14. | Chow TW. Mechanical effectiveness of root canal irrigation. J Endod. 1983;9:475-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 182] [Cited by in RCA: 182] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 15. | Nielsen BA, Craig Baumgartner J. Comparison of the EndoVac system to needle irrigation of root canals. J Endod. 2007;33:611-615. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 174] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 16. | Mejia JL, Donado JE, Basrani B. Active nonsurgical decompression of large periapical lesions--3 case reports. J Can Dent Assoc. 2004;70:691-694. [PubMed] |
| 17. | Gonzalo Domínguez M, Hernández C, Ruisoto P, Juanes JA, Prats A, Hernández T. Morphological and Volumetric Assessment of Cerebral Ventricular System with 3D Slicer Software. J Med Syst. 2016;40:154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |