Published online May 26, 2023. doi: 10.12998/wjcc.v11.i15.3599
Peer-review started: January 28, 2023
First decision: February 28, 2023
Revised: March 7, 2023
Accepted: April 18, 2023
Article in press: April 18, 2023
Published online: May 26, 2023
Processing time: 117 Days and 14.5 Hours
Temporomandibular joint (TMJ) disorders are closely related to high-angle and skeletal Class II malocclusion. Sometimes pathological changes in the mandibular condyle can cause open bite to occur after growth is complete.
This article is about the treatment of an adult male patient with a severe hyperdivergent skeletal Class II base, an unusual and gradually occurring open bite and an abnormal mandibular condyle anterior displacement. Because the patient refused surgery, four second molars with cavities and root canal therapy were extracted, and four mini-screws were used for intrusion of the posterior teeth. The treatment duration was 22 mo, and after the treatment, the open bite was corrected and the displaced mandibular condyles were seated back to the articular fossa as shown by cone-beam computed tomography (CBCT). Based on the patient’s open bite history, the result of clinical examinations and CBCT comparisons, we believe it is possible that the occlusion interference was eliminated after the four second molars were extracted and the posterior teeth were intruded, and the patient's condyle spontaneously returned to its physio
This case report suggested that identifying the cause of open bite is essential, and the TMJ factors for hyperdivergent skeletal Class II cases should be particularly examined. For these cases, intruding posterior teeth may place the condyle in a more appropriate position and provide an environment suitable for TMJ recovery.
Core Tip: This article is about the treatment of an adult male patient with a severe hyperdivergent skeletal Class II base, an unusual and gradually occurring open bite and an abnormal mandibular condyle anterior displacement. This case report suggested that identifying the cause of open bite is essential, and the temporomandibular joint (TMJ) factors for hyperdivergent skeletal Class II cases should be particularly examined. For these cases, intruding posterior teeth may place the condyle in a more appropriate position and provide an environment suitable for TMJ recovery.
- Citation: Huang ZW, Yang R, Gong C, Zhang CX, Wen J, Li H. Treatment of severe open bite and mandibular condyle anterior displacement by mini-screws and four second molars extraction: A case report. World J Clin Cases 2023; 11(15): 3599-3611
- URL: https://www.wjgnet.com/2307-8960/full/v11/i15/3599.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i15.3599
Anterior open bite has various causes, including genetic backgrounds, oral dysfunction, bad oral habits and abnormal skeletal or alveolar bone development[1-5]. Finding the aetiology is important because it affects the stability after the treatment[3,6]. The relationship between anterior open bite and the temporomandibular joint (TMJ) has received increasing attention.
Although we cannot determine the causal relation, we found that TMJ disorders (TMDs) are closely related to open bite. Pathological changes in the condyle can cause anterior open bite. There were 2 case reports about idiopathic condylar resorption-caused anterior open bite published in the American Journal of Orthodontics and Dentofacial Orthopedics in 2019[7,8]. Condylar resorption caused mandibular clockwise rotation, and all patients presented a gradually increased anterior open bite. On the other hand, high-angle patients were reported to have an increased risk of TMJ disc displacement and TMJ degenerative bony changes[9-11].
Here, we report an unusual anterior open bite case with TMD treated by 4-second molar extractions and posterior teeth intrusion with mini-screws. The total treatment time is 22 mo.
A 26-year-old man complained of a progressively aggravated open bite for the duration of 1 year.
The patient had a long history of TMJ clicking but no pain. He also had a tongue-thrusting habit.
The patient denied any history of previous disease.
The patient denied any family history of present illness.
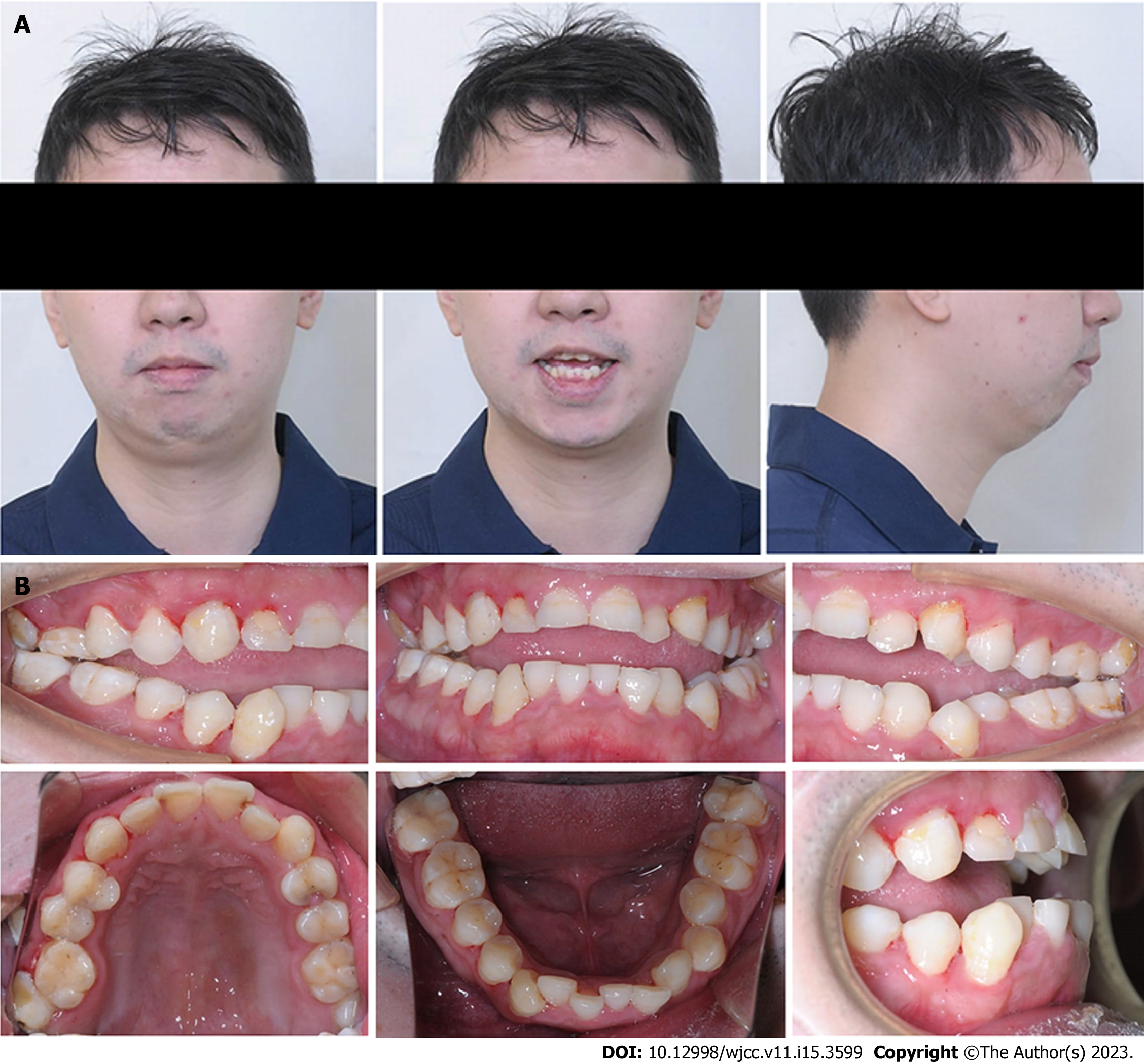
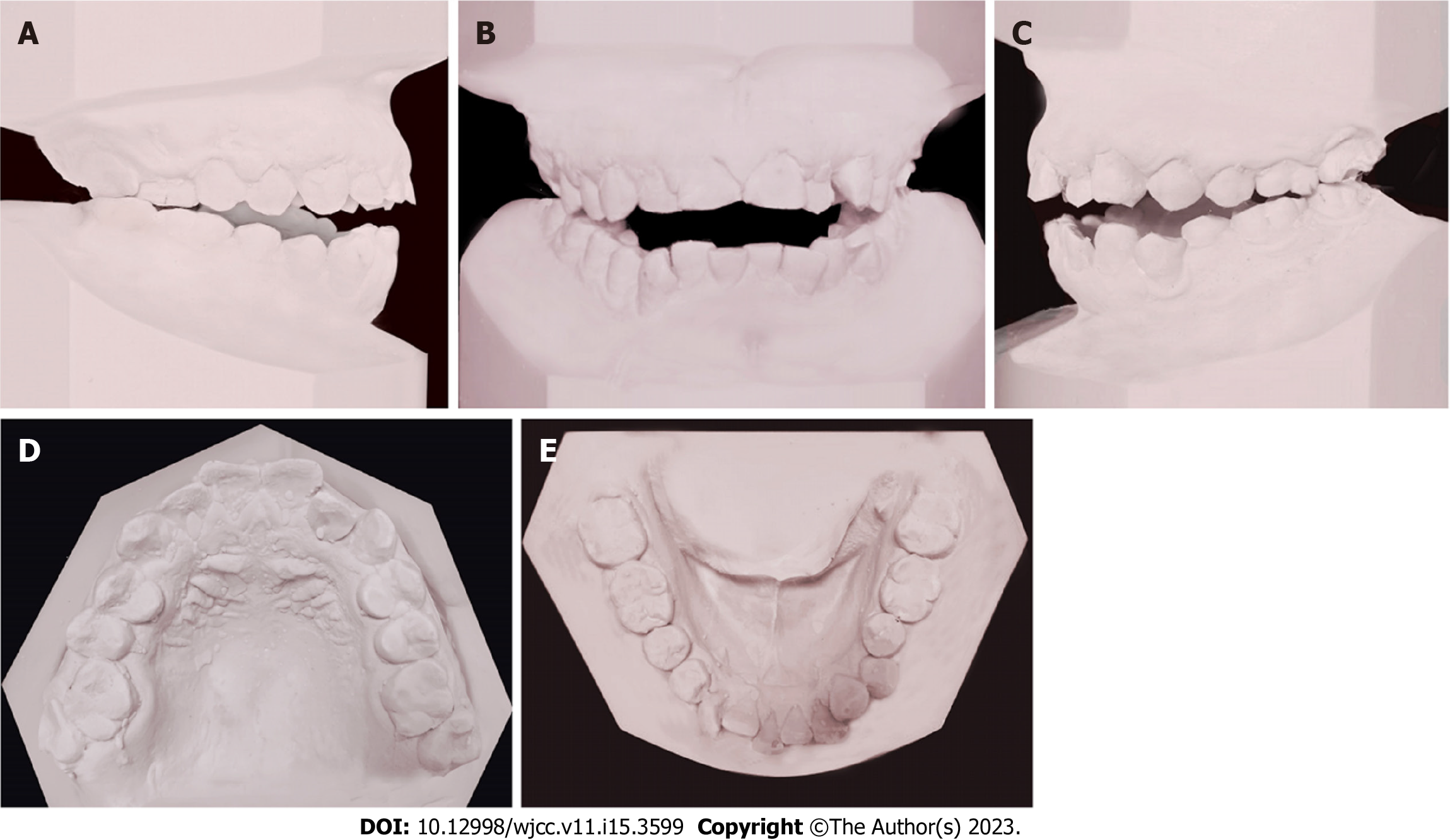
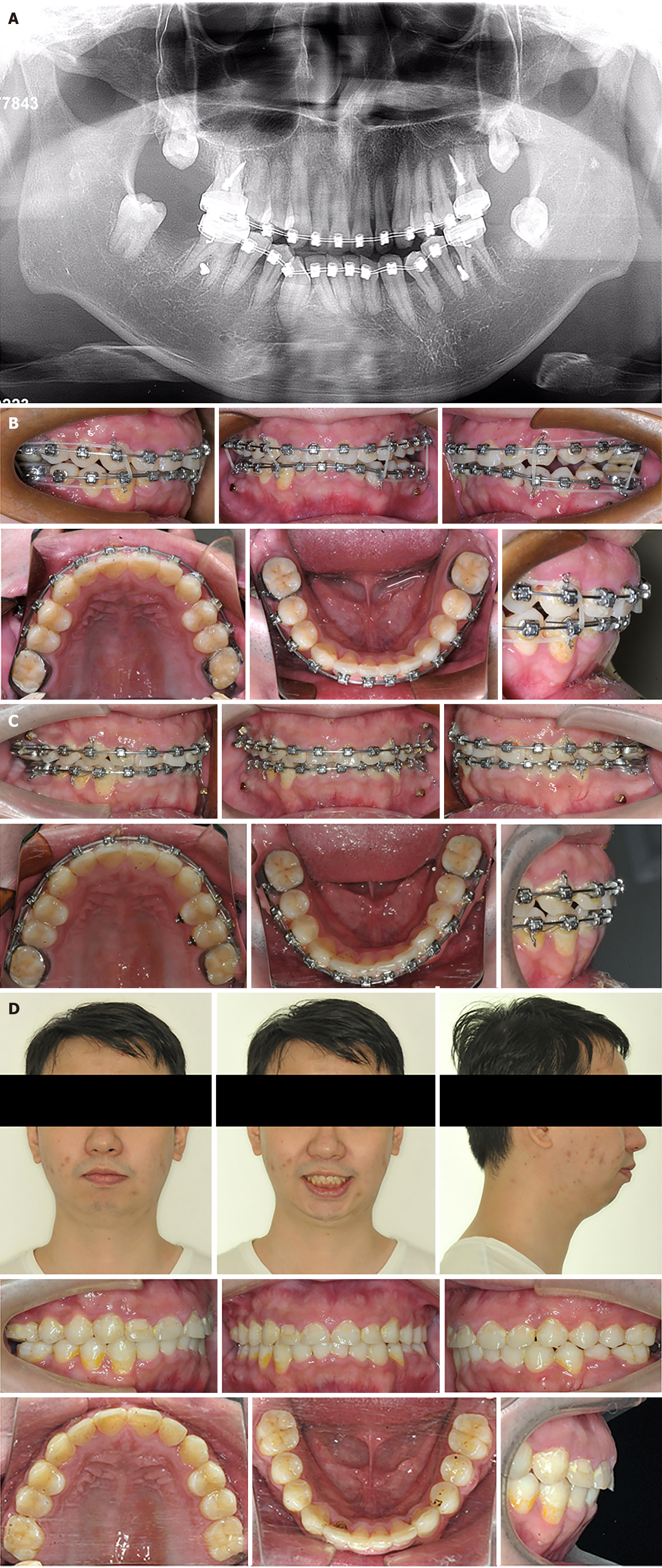
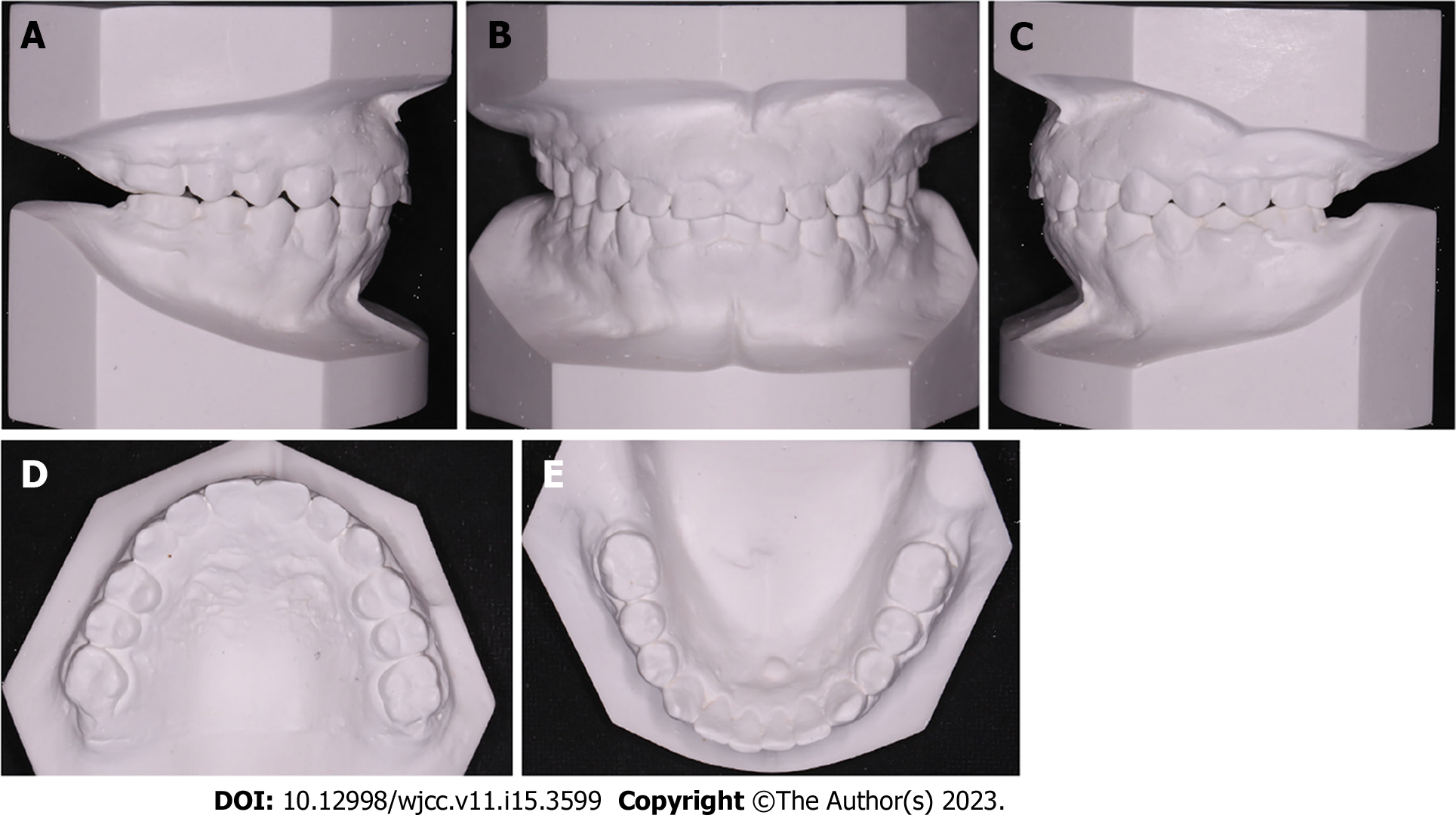
The facial analysis indicated that the patient’s lip sealing was inadequate and he had an increased lower facial third. A convex profile with a retrognathic mandible and mentum was also noted. Abrasion was apparent on the bimaxillary anterior teeth, indicating that the open bite had been a recent occurrence. The dental midline was coincident with the facial midline (Figure 1). The patient had a Class III molar relationship and posterior crossbite. Occlusal contact was only observed for the second molars (Figure 2), and dual bite was not observed.
None.
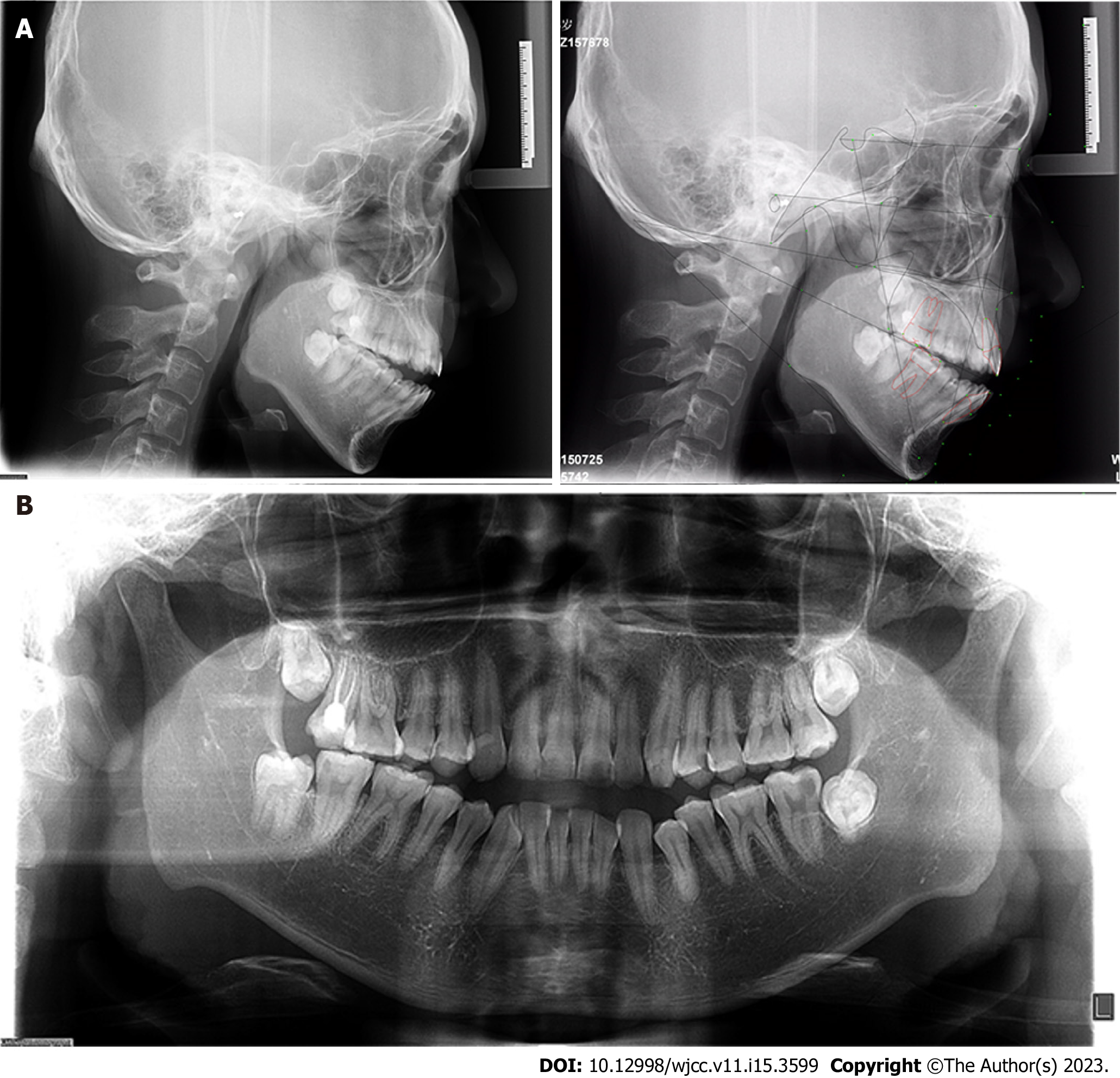
The cephalometric results revealed skeletal Class II malocclusion (SNA, 84.2°; SNB, 77.8°; ANB, 6.4°) and a high mandibular plane (SN-MP, 39.6°; FMA, 33.5°; Figure 3), and the mandibular incisors were proclined (Table 1). The panoramic radiograph showed caries in 15, 14, 11, 21, 24, and 37, 47 and 17 received root canal therapy. All four third molars were impacted (Figure 3).
| Variables | Norm | SD | Pretreatment | Posttreatment |
| SNA (°) | 83.8 | 2.8 | 84.2 | 83.4 |
| SNB (°) | 80 | 3 | 77.8 | 75.5 |
| ANB (°) | 3.8 | 1.9 | 6.4 | 8 |
| Wits | -1 | 1 | -3 | 0.3 |
| SN-MP (°) | 34.8 | 4.1 | 39.6 | 39.7 |
| Y-axis (°) | 65 | 3.9 | 76.3 | 77.4 |
| N-ANS (mm) | 55.9 | 3.1 | 54.4 | 55 |
| ANS-Me (mm) | 63.2 | 4.5 | 72.9 | 67.4 |
| S-Go (mm) | 79.8 | 6.2 | 89.7 | 85.7 |
| S-Go/N-Me (%) | 67 | 4 | 67.7 | 66.4 |
| ANS-Me/N-Me (%) | 53 | 1.8 | 57.1 | 55 |
| U1-L1 (°) | 120.6 | 9.1 | 111 | 114.8 |
| U1-SN (°) | 107.5 | 5.9 | 106.9 | 101.8 |
| U1-NA (mm) | 4.4 | 2.4 | 3.4 | 2.4 |
| U1-NA (°) | 23.7 | 5.7 | 22.7 | 18.3 |
| L1-NB (mm) | 6.8 | 2.7 | 12 | 11.6 |
| L1-NB (°) | 31.1 | 6.1 | 40 | 38.9 |
| FMIA (°) | 51.8 | 7.3 | 43.9 | 43.1 |
| IMPA (°) | 93.9 | 6.2 | 102.6 | 103.7 |
| FMA (°) | 31.3 | 5 | 33.5 | 33.2 |
| UL-EP (mm) | 2.2 | 2 | 0.5 | 2.8 |
| LL-EP (mm) | 3.2 | 2.7 | 3.5 | 6 |
| Z-Angle (°) | 69.5 | 4.8 | 57.3 | 50.7 |
| U6 - PP (UPDH) (mm) | 24.6 | 2 | 24.4 | 23.8 |
| L6 - MP (LPDH) (mm) | 32.9 | 2.5 | 39.8 | 38.3 |
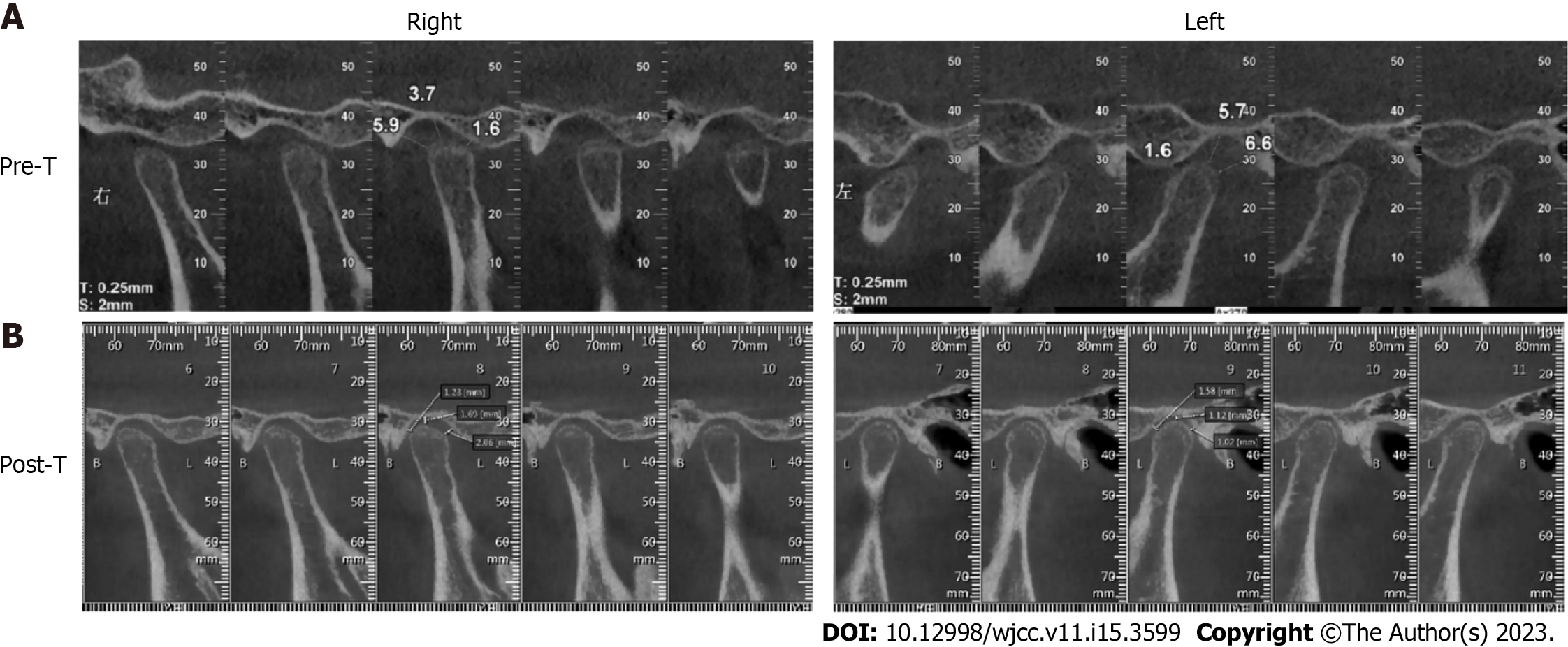
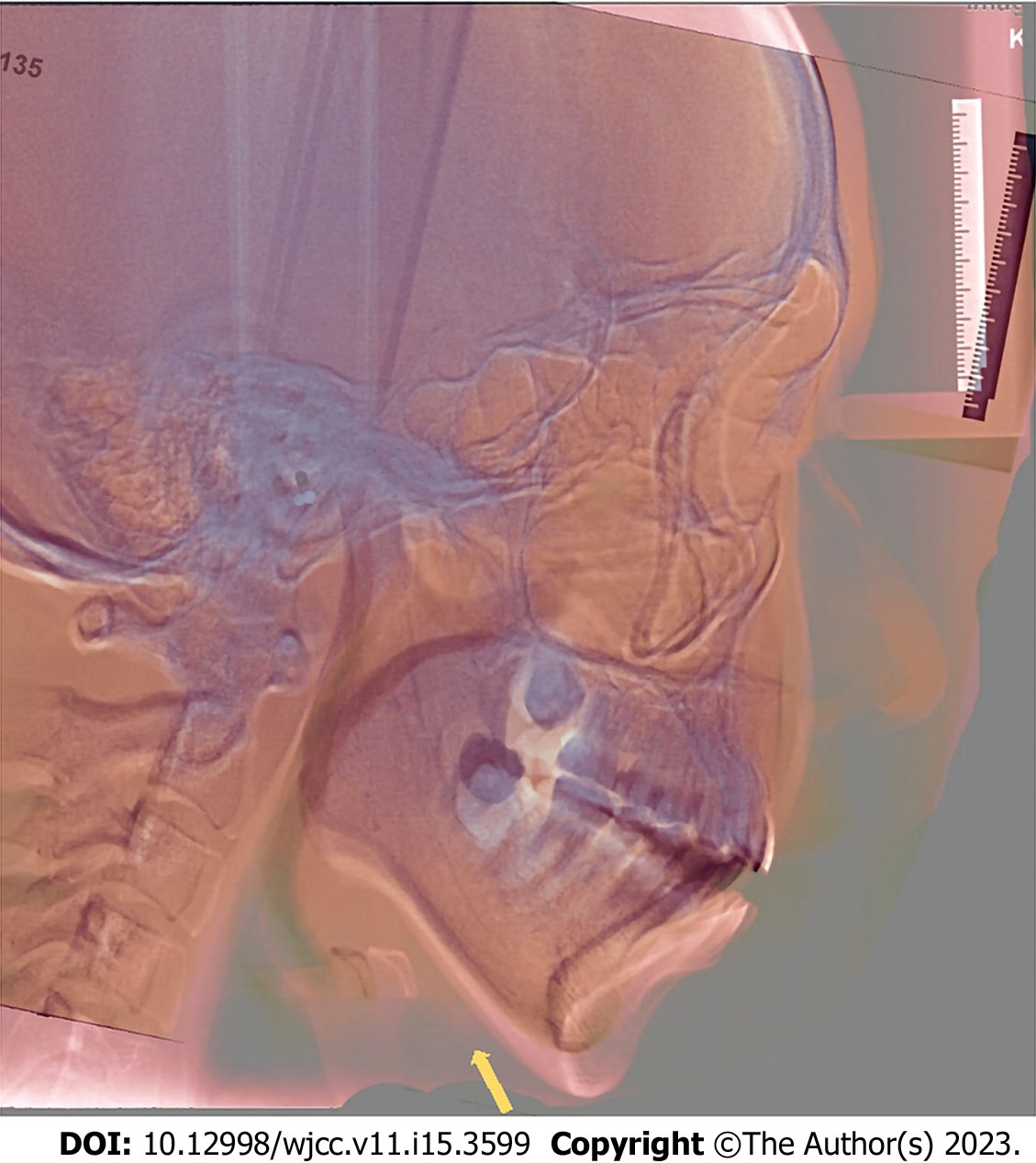
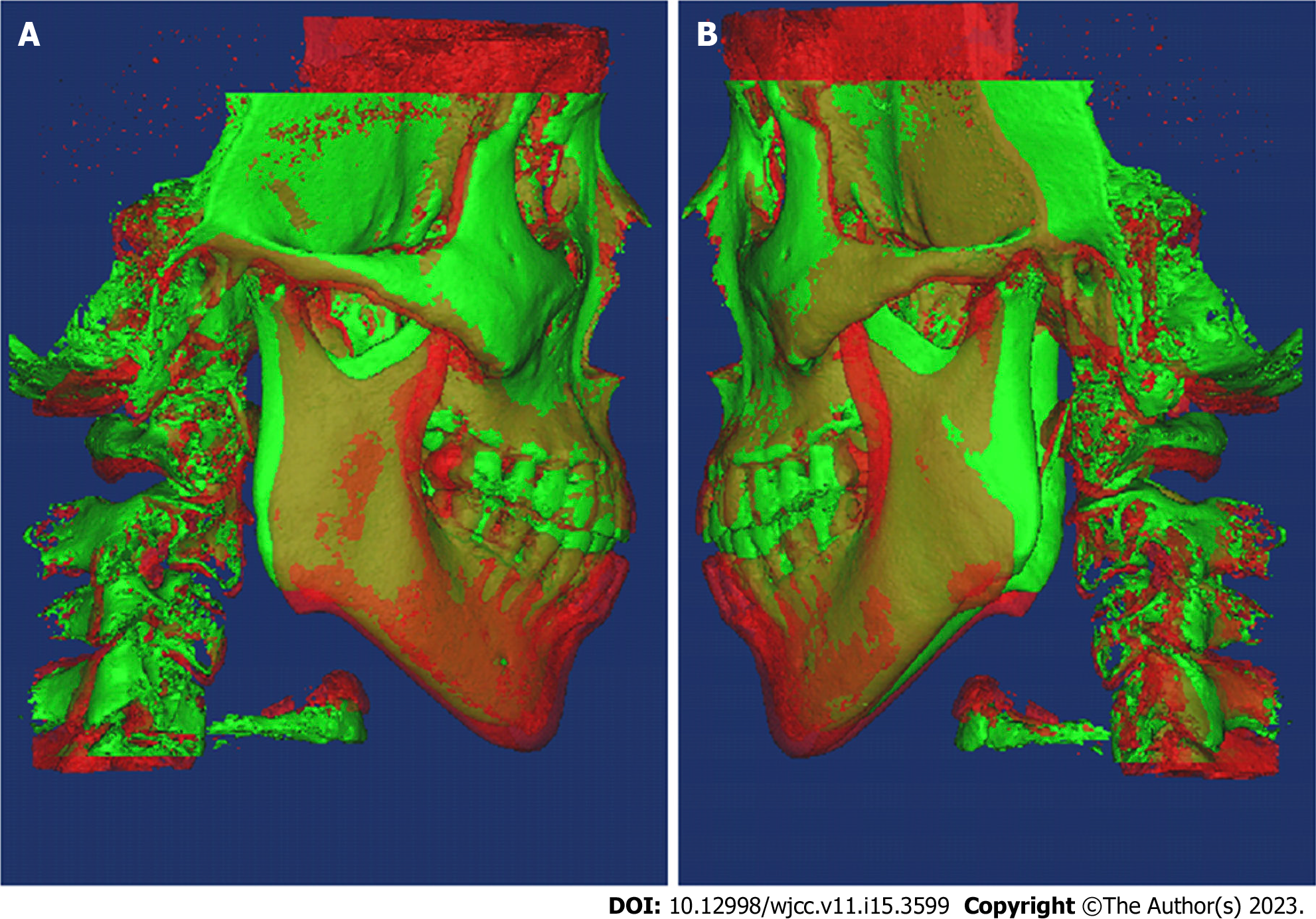
Cone-beam computed tomography (CBCT) revealed crescent-shaped changes on the posterior surface and flattening of the anterior surface of the bilateral TMJ condyles. The large superior and posterior joint space indicated condylar anterior displacement (Figure 4). The patient was diagnosed with anterior disc displacement with reduction on the right side and inside disc displacement on the left side based on magnetic resonance imaging from Shanghai Ninth People’s Hospital.
This patient was diagnosed with a skeletal Class II profile, a high mandibular plane angle, Angle Class III malocclusion and a severe open bite with TMD.
The treatment objectives were: (1) To correct the anterior open bite; (2) to achieve a Class I canine and molar relationship; (3) to relieve crowding; and (4) to improve facial aesthetics.
We proposed three treatment alternatives. The first was a combined orthodontic and orthognathic treatment, which included a Le Fort I osteotomy, a bilateral sagittal split ramus osteotomy and genioplasty. In consideration of the TMJ abnormality, we also referred the patient to the department of TMJ, who recommended TMJ disc repositioning[12,13]. However, he refused orthognathic and TMJ surgery due to safety risks.
The second alternative was camouflage treatment that would involve extracting the four first premolars and intruding the posterior teeth with mini-screws. Based on the pendulum effect and wedge effect, his open bite could be reduced.
The third alternative was also camouflage treatment. Because the second molars provided the only occlusal contact and three second molars were defective, we planned to extract four second molars and use 4 mini-screws to intrude the posterior teeth. We hope that the mandibular counterclockwise rotation could reduce the skeletal discrepancies. However, there were still some unpredictable problems, such as the periodontal risks due to posterior teeth intrusion, the TMD progression, the normal eruption of 4 third molars and the inferior alveolar nerve injury risks due to second molars extraction[14]. In addition, compared to the orthognathic surgery plan and premolar extraction plan, the ability to improve his profile and occlusion with this method was potentially more limited.
After discussion, the patient accepted the risk and selected the third treatment plan.
We taught the patient a tongue muscle training procedure to correct his tongue-thrusting habit. One week after the extraction of four second molars, a preadjusted appliance with 0.022-in slots was bonded. A sequence of continuous 0.012-in, 0.014-in, 0.016-in, 0.016-in × 0.022-in, 0.018-in × 0.025-in nickel-titanium and 0.019-in × 0.025-in stainless-steel archwires was used to align and level both arches for 8 mo. In the second month, four 8 mm mini-screws were implanted bilaterally between the second premolar and first molar. Power chains were used to load intrusive force on the posterior teeth in the third month (Figure 5A).
Surprisingly, the open bite was corrected after only 5 mo, which was very quick, and it was accompanied by an improvement in the sagittal molar relationship (Figure 5B). However, bilateral posterior open bite occurred because we only performed the intrusive force buccally on the nickel-titanium archwires, which caused buccal tipping of the posterior teeth. With the use of vertical elastics and stainless-steel wires, posterior occlusion was rebuilt (Figure 5C). The eruption of the third molars will need further observation during the retention phase, which may need extra treatment. The treatment duration was 22 mo. After removing all appliances, we used removable soft retainers for retention.
The ideal anterior overjet and overbite, Class I molar relationship and improved facial and dental aesthetics were achieved (Figures 5D and 6).
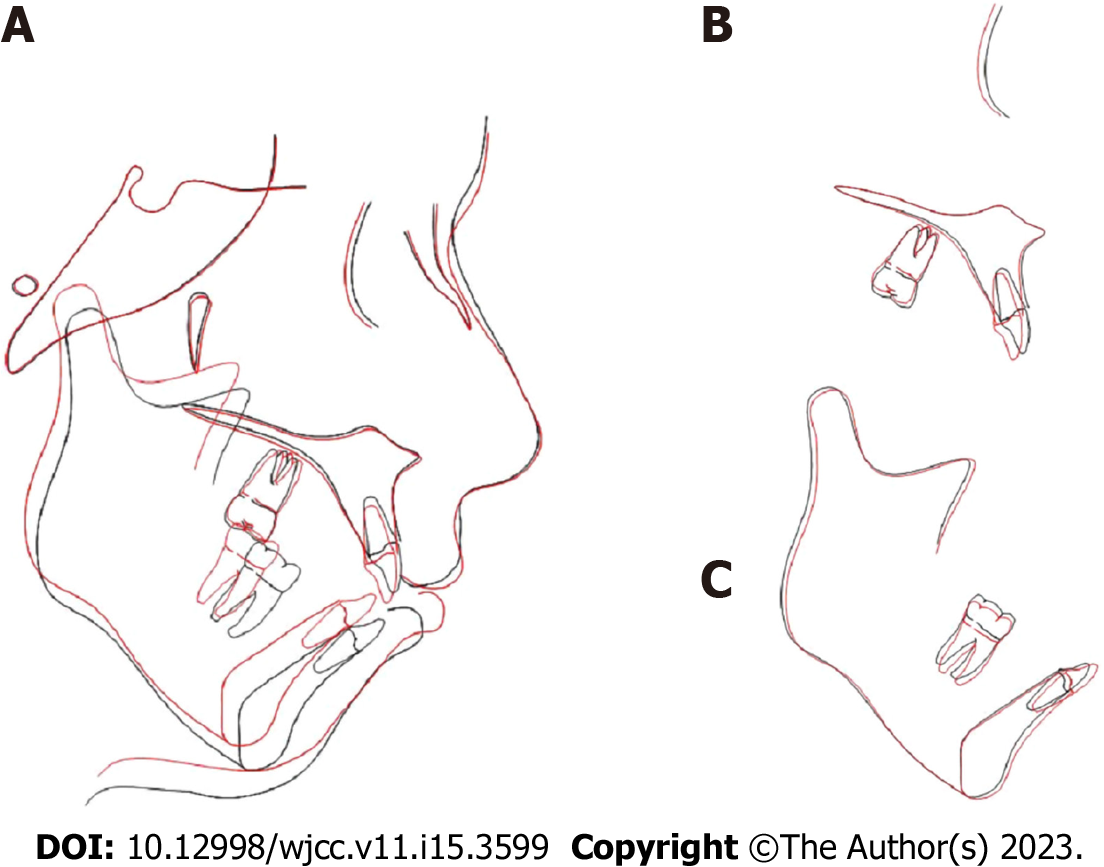
The root paralleling was good, and four third molars had erupted compared to the former panoramic radiograph (Figure 7). The ANB increased from 6.4° to 8° (Table 1). However, the facial aesthetics still improved, especially the frontal and smile aesthetics, because the significantly reduced ANS-Me (72.9 mm to 67.4 mm) and S-Go (89.7 mm to 85.7 mm) contributed to the reduction in facial muscular tension and created a harmonious and natural facial appearance. FMA was maintained after orthodontic treatment (FMA, 33.5° to 33.2°). The maxillary incisors were upright, and the mandibular incisors were slightly proclined (U1-SN, 106.9° to 101.8°; L1-MP, 102.6° to 103.7°; U1-L1, 111° to 114.8°). The superimpositions showed that the amount of molar intrusion was small (U6 – PP, 24.4 mm to 23.8 mm; L6 – MP, 39.8 mm to 38.3 mm), and there was a significant posterior and superior shift of the mandible, which was also confirmed by CBCT (Figures 8-10). CBCT showed a significant decrease in the posterior and superior joint space, and the bilateral condyles moved back to the articular fossa. The continuity of the condylar cortical bone and the morphology of the anterior surface of the left condyle also appeared to be improved after orthodontic treatment (Figure 4). The patient experienced no TMJ pain during the orthodontic treatment.
After 2 years, we called the patient to remind him of a return visit. However, he refused the return visit as he moved to another city. He was satisfied with the treatment results and reported no recurrence of open bite and TMJ pain.
Here, we presented a severe open bite case with apparent superior and posterior condylar position changes before and after treatment. This result suggested that in addition to the morphology of condyles, we need to consider the position of condyles and changes in joint spaces, which can be related to open bite malocclusion.
The etiology of the patient’s open bite caught our interest. We speculated that unstable condylar anterior displacement and the subsequent tooth extrusion contributed to the patient’s open bite, and the reasons are described as follows. The patient was an adult and had obvious abrasion on the anterior teeth, meaning that he had anterior occlusal contact in the past. With no change in the jaw position, it was difficult for the patient to have such a severe open bite, as only the second molars had occlusal contact after just one year. The characteristics of his malocclusion also gave us some clues. In contrast to most skeletal Class II open bite cases, he had a Class III molar relationship and posterior crossbite. It seemed as though the teeth had not adapted to the anterior repositioning of the jaw in the short term. Considering that he was a TMD patient with a long history of joint clicking, the lax capsule and weak ligaments may have also caused instability of the condylar position. By extracting 4 second molars and intruding the posterior teeth, we eliminated occlusal interference which may create an easily adapted environment for the TMJ to recover. Therefore, the bilateral condyles moved back to the articular fossa with improved morphological changes and bone remodeling accompanied by an increased ANB (ANB, 6.4° to 8°).
Many open bite studies have focused on how effective mini-screws are in intruding posterior teeth and inducing mandibular counterclockwise rotation, but few studies have discussed the accompanying changes in the condylar position. One study showed that the centre of mandibular autorotation was located 7.4 mm behind and 16.9 mm below the condylion after molar intrusion[15]. This demonstrates that using mini-screws to intrude posterior teeth can place the condyle in a more superior and posterior position. As our patient’s condyles were seated in an inferior and anterior position, we used mini-screws to intrude his bimaxillary posterior teeth, helping the condyles move back to the fossa.
The adaptive capacity of the TMJ condyle is truly a gift to orthodontists, regardless if we intentionally change the condylar position or not[16-21] However, we need to be cautious, as some patients fail to adapt to the new condylar position, and dual bite, muscular disorders or TMJ pain can be created. Usually, if possible, the patient’s original jaw position should be maintained or at least not fully changed, especially for adults without TMJ symptoms, because the relationship between the occlusal and TMJ results from a lifetime of homeostatic adaptations of muscle, occlusion and TMJ[22,23].
We treated a severe anterior open bite case that occurred in one year with TMJ condylar displacement. After treatment, we achieved ideal anterior overbite, and the occlusion was stable and functional. By extracting 4 second molars and intruding posterior teeth, we eliminated occlusal interference and the TMJ condyle moved back to an appropriate position, which provided an environment suitable for TMJ recovery. Therefore, we suggest that identifying the cause of open bite is essential, and the TMJ factors for hyperdivergent skeletal Class II cases should be particularly examined. The success of the homeostatic adaptation of muscle, occlusion and TMJ is vital for the stability of orthodontic treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bernardi S, Italy; Nagamine T, Japan S-Editor: Liu JH L-Editor: A P-Editor: Zhang XD
| 1. | Al-Moraissi EA, Wolford LM. Does Temporomandibular Joint Pathology With or Without Surgical Management Affect the Stability of Counterclockwise Rotation of the Maxillomandibular Complex in Orthognathic Surgery? J Oral Maxillofac Surg. 2017;75:805-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Chamberland S. Progressive idiopathic condylar resorption: Three case reports. Am J Orthod Dentofacial Orthop. 2019;156:531-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 3. | Elfeky HY, Fayed MS, Alhammadi MS, Soliman SAZ, El Boghdadi DM. Three-dimensional skeletal, dentoalveolar and temporomandibular joint changes produced by Twin Block functional appliance. J Orofac Orthop. 2018;79:245-258. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 4. | Gonçalves JR, Cassano DS, Wolford LM, Santos-Pinto A, Márquez IM. Postsurgical stability of counterclockwise maxillomandibular advancement surgery: affect of articular disc repositioning. J Oral Maxillofac Surg. 2008;66:724-738. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 78] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Greene CS, Obrez A. Treating temporomandibular disorders with permanent mandibular repositioning: is it medically necessary? Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;119:489-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 35] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 6. | Greenlee GM, Huang GJ, Chen SS, Chen J, Koepsell T, Hujoel P. Stability of treatment for anterior open-bite malocclusion: a meta-analysis. Am J Orthod Dentofacial Orthop. 2011;139:154-169. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 142] [Article Influence: 10.1] [Reference Citation Analysis (0)] |
| 7. | Jiang YY, Sun L, Wang H, Zhao CY, Zhang WB. Three-dimensional cone beam computed tomography analysis of temporomandibular joint response to the Twin-block functional appliance. Korean J Orthod. 2020;50:86-97. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 19] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 8. | Kandasamy S, Greene CS, Obrez A. An evidence-based evaluation of the concept of centric relation in the 21st century. Quintessence Int. 2018;49:755-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Kim JY, Jue SS, Bang HJ, Christine H, Moon JI, Nakatsuka M, Kumabe S, Owtad P, Park JH, Shin JW. Histological Alterations from Condyle Repositioning with Functional Appliances in Rats. J Clin Pediatr Dent. 2018;42:391-397. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 10. | Kim K, Choy K, Park YC, Han SY, Jung H, Choi YJ. Prediction of mandibular movement and its center of rotation for nonsurgical correction of anterior open bite via maxillary molar intrusion. Angle Orthod. 2018;88:538-544. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 29] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 11. | Koide D, Yamada K, Yamaguchi A, Kageyama T, Taguchi A. Morphological changes in the temporomandibular joint after orthodontic treatment for Angle Class II malocclusion. Cranio. 2018;36:35-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Kyburz KS, Eliades T, Papageorgiou SN. What effect does functional appliance treatment have on the temporomandibular joint? Prog Orthod. 2019;20:32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Lee KY, Park JH, Tai K, Chae JM. Treatment with Twin-block appliance followed by fixed appliance therapy in a growing Class II patient. Am J Orthod Dentofacial Orthop. 2016;150:847-863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Manfredini D, Segù M, Arveda N, Lombardo L, Siciliani G, Alessandro Rossi, Guarda-Nardini L. Temporomandibular Joint Disorders in Patients With Different Facial Morphology. A Systematic Review of the Literature. J Oral Maxillofac Surg. 2016;74:29-46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 93] [Cited by in RCA: 75] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 15. | Ngan P, Fields HW. Open bite: a review of etiology and management. Pediatr Dent. 1997;19:91-98. [PubMed] |
| 16. | Ooi K, Inoue N, Matsushita K, Yamaguchi H, Mikoya T, Minowa K, Kawashiri S, Nishikata S, Tei K. Incidence of anterior disc displacement without reduction of the temporomandibular joint in patients with dentofacial deformity. Int J Oral Maxillofac Surg. 2018;47:505-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Ooi K, Yura S, Inoue N, Totsuka Y. Factors related to the incidence of anterior disc displacement without reduction and bony changes of the temporomandibular joint in patients with anterior open bite. Oral Maxillofac Surg. 2014;18:397-401. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 18. | Park JH, Park JJ, Papademetriou M, Suri S. Anterior open bite due to idiopathic condylar resorption during orthodontic retention of a Class II Division 1 malocclusion. Am J Orthod Dentofacial Orthop. 2019;156:555-565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 19. | Reichert I, Figel P, Winchester L. Orthodontic treatment of anterior open bite: a review article--is surgery always necessary? Oral Maxillofac Surg. 2014;18:271-277. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 42] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 20. | Rijpstra C, Lisson JA. Etiology of anterior open bite: a review. J Orofac Orthop. 2016;77:281-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 21. | Schmid KM, Kugler R, Nalabothu P, Bosch C, Verna C. The effect of pacifier sucking on orofacial structures: a systematic literature review. Prog Orthod. 2018;19:8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 22. | Varvara G, Feragalli B, Turkyilmaz I, D'Alonzo A, Rinaldi F, Bianchi S, Piattelli M, Macchiarelli G, Bernardi S. Prevalence and Characteristics of Accessory Mandibular Canals: A Cone-Beam Computed Tomography Study in a European Adult Population. Diagnostics (Basel). 2022;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 23. | Wanjau J, Sethusa MP. Etiology and pathogenesis of anterior open bite: a review. East Afr Med J. 2010;87:452-455. [PubMed] |