Published online May 16, 2023. doi: 10.12998/wjcc.v11.i14.3351
Peer-review started: February 23, 2023
First decision: March 28, 2023
Revised: April 2, 2023
Accepted: April 10, 2023
Article in press: April 10, 2023
Published online: May 16, 2023
Processing time: 82 Days and 2.3 Hours
Atlantoaxial rotatory subluxation (AARS) is an uncommon disease with a greater prevalence among children than adults, and it is mostly associated with trauma. Iatrogenic spinal injury accounts for a low percentage of injuries. However, in AARS, 20%-40% of cases are associated with surgery, and 48% are caused by infection. Here, we describe our experience with a case of iatrogenic AARS after general anesthesia.
A 12-year-old girl presented with right-sided torticollis and cervical motion limit. The patient had undergone thyroidectomy 2 mo ago. Computed tomography revealed AARS with bilateral locked facets. Following the failure of repeated external reduction under general anesthesia, the patient underwent an open surgical reduction. The patient gained atlantoaxial alignment without any complications. Follow-up radiographs showed a normal appearance without instability. The cervical spine of children is more predisposed to injury due to anatomical and biomechanical differences. AARS secondary to infection and surgery is known as Grisel’s syndrome, which involves non-traumatic AARS. Several cases of AARS after surgery and other procedures with no evidence of inflammation have been reported. Our experience shows that surgery requiring hyperextension of the neck after general anesthesia should also be included as a risk factor.
Surgeons and anesthesiologists should be careful not to excessively extend the neck during pediatric surgery. Moreover, clinicians caring for pediatric patients with recent head and neck procedures must be aware of common AARS presentations.
Core Tip: Atlantoaxial rotatory subluxation (AARS) is a rare condition with a higher prevalence in children, often associated with trauma or infection, and occasionally surgery. This case highlights iatrogenic AARS after general anesthesia and the importance of caution during surgery for AARS in pediatric patients.
- Citation: Hong WJ, Lee JK, Hong JH, Han MS, Lee SS. Iatrogenic atlantoaxial rotatory subluxation after thyroidectomy in a pediatric patient: A case report. World J Clin Cases 2023; 11(14): 3351-3355
- URL: https://www.wjgnet.com/2307-8960/full/v11/i14/3351.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i14.3351
Atlantoaxial rotatory subluxation (AARS) is an uncommon disease with a greater prevalence among children than adults, and it is mostly associated with trauma. Traumatic spinal injuries in children have been reported to be relatively rare, accounting for 1%-10% of all spinal injuries. The incidence of traumatic spinal injuries increases with age, with most injuries being associated with car accidents, followed by falls and sports. Other causes comprise only 3% of spinal injuries, including iatrogenic causes[1,2]. Therefore, iatrogenic spinal injury accounts for only a low percentage of injuries. However, in AARS, 20%-40% of cases are associated with surgery, and 48% are caused by infection (Grisel’s syndrome)[3,4]. As mentioned above, AARS has a high prevalence in the pediatric population. The cervical spine is the most vulnerable and commonly injured part of the pediatric spine. Moreover, pediatric spine kinematics is significantly different from that of adults. The facet joints are more horizontally oriented and provide less resistance to rocking and translation between the vertebrae, and the uncinate processes are not developed. Therefore, cervical dislocation after a surgical procedure in pediatric patients is a complication that may occur more often than expected. Nevertheless, only few cases of cervical dislocation due to the surgical position of the patient have been reported. Here, we describe our experience with a case of AARS after thyroid surgery.
The patient complained of right-sided torticollis and cervical motion limit.
A 12-year-old female patient visited our department with right torticollis and cervical motion limit 2 mo ago.
The patient underwent thyroidectomy 2 mo ago. The symptoms appeared after thyroidectomy.
There was no significant past or family history.
There was no motor weakness or sensory change.
There were no significant laboratory findings.
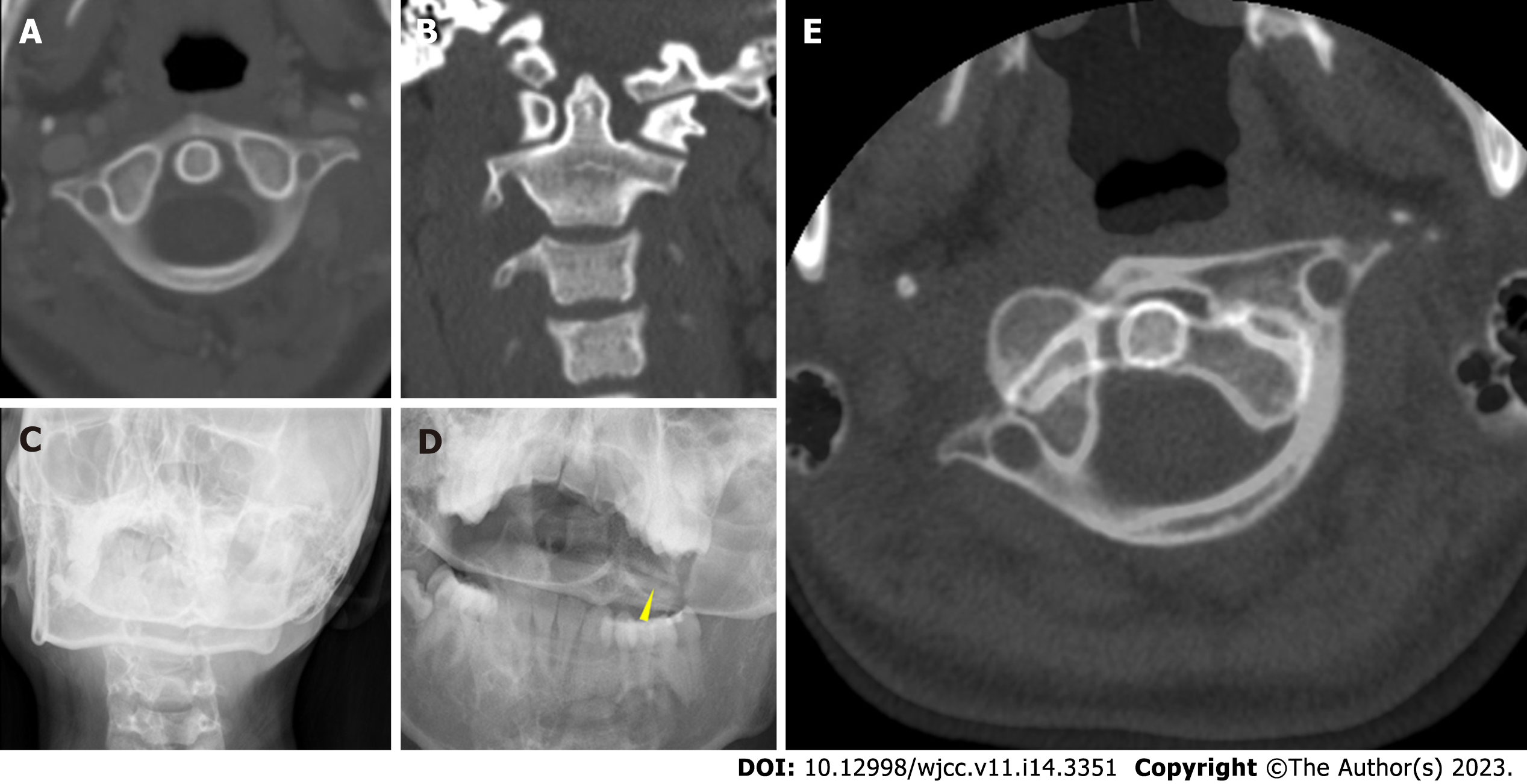
Plain radiographs demonstrated torticollis and the “cock robin” position of the head (Figure 1A and B). Cervical computed tomography (CT) revealed AARS with bilateral locked facets (Figure 1C and D). Neck CT before thyroidectomy showed the normal alignment of the atlantoaxial joint.
The patient was diagnosed with iatrogenic AARS with bilateral locked facets based on imaging and clinical findings.
Halter neck traction with 5 pound weight was applied with sedatives and analgesia. Follow-up CT was performed after a week of continuous halter traction; however, AARS remained. Following the failure of repeated external reduction under general anesthesia, we decided on an open surgical reduction. First, through a posterior cervical midline approach, we exposed the C1 and C2 Lamina. Manual reduction was performed by wiring C1, which failed. As there was no other alternative, we sacrificed the C2 root, and the facet subluxation was reduced by manual traction. After confirming the reduction, iliac bone graft and interspinous wiring were performed. The patient gained atlantoaxial alignment without any complications.
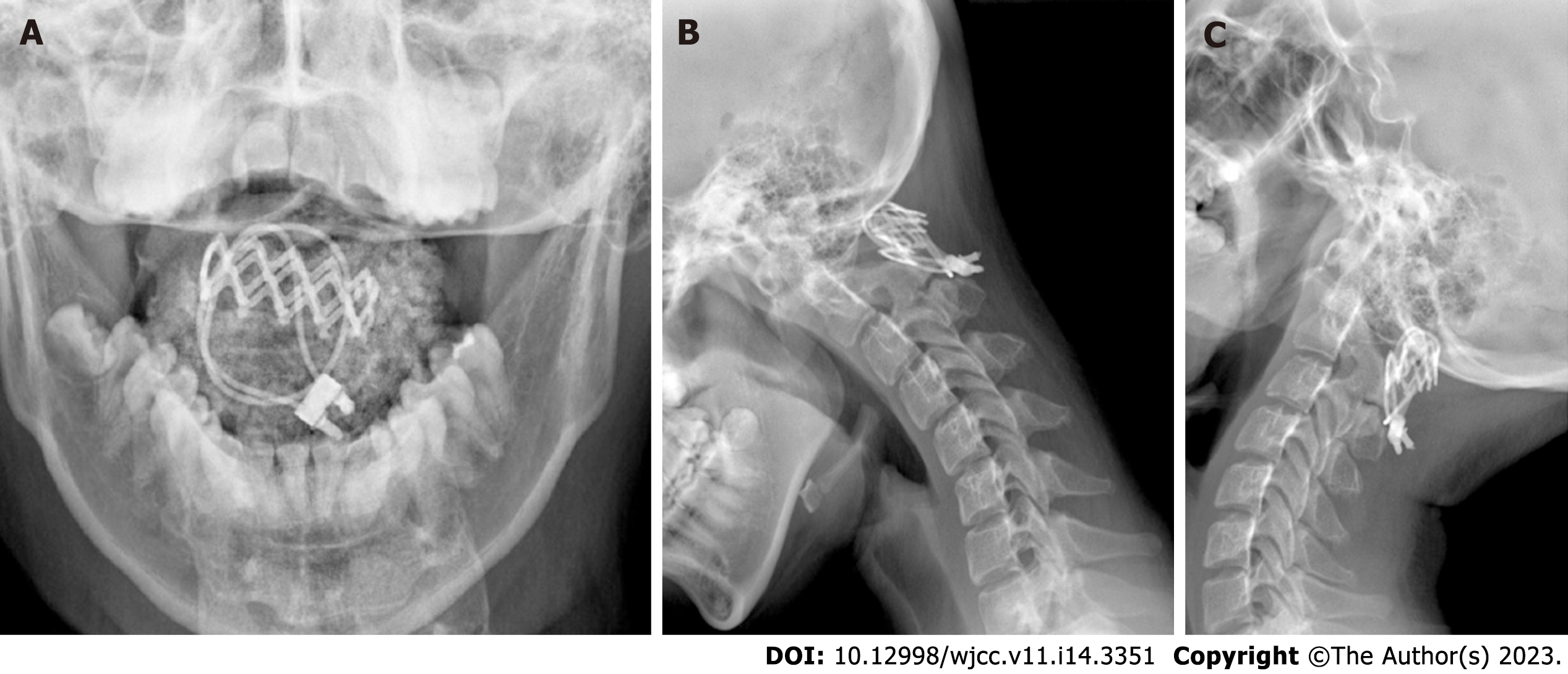
After surgery, the patient's torticollis was corrected, and she was discharged without any complications. One-year follow-up dynamic radiographs showed a normal appearance without instability (Figure 2). The patient remained asymptomatic without recurrence until 8 years after surgery.
Pediatric AARS can be divided into three main categories depending on their cause: Traumatic, congenital, and inflammatory. Traumatic and congenital causes are related to instability. The cervical spine of children is more predisposed to injury than that of adults due to anatomical and biomechanical differences. In children, the head mass is relatively high, and neck muscles are underdeveloped. The vertebral bodies are anterior wedge-shaped, the facets are angled horizontally, the uncinate process is absent, and the ligaments and joint capsules are highly elastic. Various congenital abnormalities contribute to vertebral dysplasia, leading to instability of the cervical spine (e.g., Klippel-Feil syndrome, Chiari malformation, and Down syndrome). Due to this instability, the pediatric spine is relatively vulnerable to external forces and is easily damaged by minor trauma.
AARS secondary to infection is known as Grisel’s syndrome. It can be caused by infections, such as in otitis media, viral syndromes, or pharyngitis. Additionally, AARS after head and neck surgery has been occasionally reported in the literature. Symptoms associated with inflammatory reactions after surgery have been observed[3]. The specific mechanism of Grisel’s syndrome is unknown; however, the hematogenous spread of infection from the pharynx to the cervical spine with hyperemia and abnormal relaxation of the atlantoaxial ligaments is accepted as a reasonable explanation[5]. Therefore, AARS rarely appears immediately and is usually detected during postoperative recovery, and laboratory tests show increased inflammatory markers. The most common inflammatory markers measured in clinical practice are C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR). In our case, both CRP and ESR were in a normal range 2 wk after thyroidectomy. In addition, the patient had no specific neurological symptoms other than mild neck discomfort, which could be considered a postoperative change.
Several cases of AARS after surgery and other procedures, such as ventricular abdominal shunt surgery, otitis media surgery, and central venous catheter insertion, have been reported with no evidence of inflammation in pediatric patients[6-8]. The common features of these cases include a pediatric population and a head rotation procedure under general anesthesia. The use of muscle relaxants and general anesthesia loosens the neck muscles, which increases instability in the cervical joint. In addition, pediatric spine kinematics may contribute to the development of AARS. According to Kim et al[9], the risk factors for iatrogenic AARS could include pediatric surgery, oropharyngeal inflammation, general anesthesia, and extreme rotation of the head. Nevertheless, we believe that surgery requiring hyperextension of the neck after general anesthesia should also be included as a risk factor.
Early diagnosis is crucial for patients with cervical dislocation, including AARS. Late diagnosis may lead to late management, thereby resulting in invasive treatment. This case required surgical treatment with posterior C1–C2 fusion, resulting in extended hospital stay, additional expenses, and complications. We hope that our experience may help other clinicians prevent such rare and unfortunate incidents from occurring among pediatric patients.
Surgeons and anesthesiologists should be careful not to excessively extend the neck during surgery for pediatric patients and ensure that it is in the normal axis even after the operation is complete. Moreover, clinicians caring for pediatric patients with recent head and neck procedures must be aware of the common presentations of AARS.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mei XF, China; Nambi G, Saudi Arabia S-Editor: Ma YJ L-Editor: Wang TQ P-Editor: Zhang YL
| 1. | Bilston LE, Brown J. Pediatric spinal injury type and severity are age and mechanism dependent. Spine (Phila Pa 1976). 2007;32:2339-2347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 2. | Carreon LY, Glassman SD, Campbell MJ. Pediatric spine fractures: a review of 137 hospital admissions. J Spinal Disord Tech. 2004;17:477-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 120] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 3. | Karkos PD, Benton J, Leong SC, Mushi E, Sivaji N, Assimakopoulos DA. Grisel's syndrome in otolaryngology: a systematic review. Int J Pediatr Otorhinolaryngol. 2007;71:1823-1827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 67] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 4. | Pang D, Li V. Atlantoaxial rotatory fixation: part 3-a prospective study of the clinical manifestation, diagnosis, management, and outcome of children with alantoaxial rotatory fixation. Neurosurgery. 2005;57:954-72; discussion 954. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 81] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 5. | Richter GT, Bower CM. Cervical complications following routine tonsillectomy and adenoidectomy. Curr Opin Otolaryngol Head Neck Surg. 2006;14:375-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 26] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Brisson P, Patel H, Scorpio R, Feins N. Rotary atlanto-axial subluxation with torticollis following central-venous catheter insertion. Pediatr Surg Int. 2000;16:421-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 7. | Hashide S, Aihara Y, Nagahara A, Mitsuyama T, Okada Y. Atlantoaxial Rotatory Subluxation after Removal of a Ventriculoperitoneal Shunt in the Supine-Lateral Position. Pediatr Neurosurg. 2015;50:229-232. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Sakaida H, Akeda K, Sudo A, Takeuchi K. Atlantoaxial rotatory fixation as a rare complication from head positioning in otologic surgery: Report of two cases in young children. Patient Saf Surg. 2017;11:5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Kim B, Iwata K, Sugimoto K, Suzuki S, Ema Y, Tsunobuchi H, Nishiwaki K. Significance of prevention and early treatment of a postoperative twisted neck: atlantoaxial rotatory subluxation after head and neck surgery. J Anesth. 2010;24:598-602. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |