Published online May 6, 2023. doi: 10.12998/wjcc.v11.i13.3099
Peer-review started: January 27, 2023
First decision: March 10, 2023
Revised: March 20, 2023
Accepted: March 31, 2023
Article in press: March 31, 2023
Published online: May 6, 2023
Processing time: 87 Days and 17.2 Hours
Angiosarcoma is a rare malignant tumor. Owing to the lack of specific clinical manifestations of this disease, it is difficult to achieve early diagnosis and start early treatment.
A 78-year-old male patient was admitted to the hospital because of a bump on his head that did not heal for 4 mo. The patient was diagnosed with a refractory head wound. The patient underwent neoplasm resection and skin grafting surgery in the Plastic Surgery. The neoplasm was sent for pathological examination during the operation. The final pathological results were confirmed scalp angiosarcoma.
Our research suggests that pathological examination should be performed for refractory ulcers of the scalp, and physical factor therapy should be used with caution before the diagnosis is clear.
Core Tip: Angiosarcoma is a rare malignant tumor. Owing to the lack of specific clinical manifestations of this disease, it is difficult to achieve early diagnosis and start early treatment. Our research suggests that pathological examination should be performed for refractory ulcers of the scalp, and physical factor therapy should be used with caution before the diagnosis is clear.
- Citation: Yan ZH, li ZL, Chen XW, Lian YW, Liu LX, Duan HY. Misdiagnosis of scalp angiosarcoma: A case report. World J Clin Cases 2023; 11(13): 3099-3104
- URL: https://www.wjgnet.com/2307-8960/full/v11/i13/3099.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v11.i13.3099
Angiosarcoma is a rare malignant tumor that originates from the endothelial cells of blood vessels or lymphatic vessels and accounts for approximately 1% to 2% of soft tissue sarcomas, of which more than 50% occur in the head and neck, accounting for 0.1% of head and neck malignancies[1]. Because the incidence of scalp angiosarcoma is extremely low, it attracts little clinical attention. Owing to the lack of specific clinical manifestations of this disease, it is difficult to achieve early diagnosis and start early treatment. Some patients suffer from head trauma, and the wound is repeatedly ruptured and is difficult to heal. Angiosarcoma is difficult to diagnose at an early stage, and treatment of the condition is often delayed by mistakenly attributing it to trauma-related abrasions and abscesses. Imaging examinations such as computed tomography (CT) or magnetic resonance imaging have a certain value for understanding the location, extent of invasion and whether there is distant metastasis. Thus, timely local tissue biopsy is the main method of diagnosis. The diagnosis is finally confirmed by pathological examination. Recently, the department of rehabilitation of the first hospital of jilin university used physical methods to treat a patient with refractory scalp wounds. The treatment was ineffective. Finally, the pathological examination was used to diagnose scalp angiosarcoma. The report is as follows.
A 78-year-old male patient was admitted to the hospital because of a bump on his head that did not heal for 4 mo.
The patient accidentally bumped his head on a cabinet approximately 4 mo ago, which caused the skin of the top of the skull to rupture. After the injury, the patient was conscious, with headache, no nausea or vomiting, and no ulceration of the lips. There were no abnormal secretions in the nose, mouth and external auditory canal, no incontinence, and no convulsions. Motor movements were normal. The patient had been treated at a local hospital for head wounds, but the wounds did not heal. The patient was sent to our hospital for further diagnosis and treatment. The outpatient was admitted to the neurosurgery department of our hospital for head and neck refractory wounds, based on the symptoms, signs and examination (October 20, 2017).
There is no obvious history of past illness related to this disease.
There is no obvious personal or family history related to this disease.
On admission to the hospital, he was conscious; his vital signs were stable, and no enlarged lymph nodes were discovered in the neck or behind the ears. Both muscle strength and muscle tension of the extremities were normal, and voluntary activities were normal. The bilateral Babinski sign and neck stiffness were negative. The ulcerated wound was visible on the top of the skull; the wound was 3 cm × 4 cm, and some bloody scabs and granulation tissue could be observed on the top of the wound, with a small amount of secretions and no peculiar smell (Figure 1).
Routine blood test (October 20, 2017) results were as follows: White blood cell count, 7.30 × 109/L (reference value: 3.50-9.50 × 109/L); neutrophil percentage: 78% (reference value: 20%-75%). The patient was diagnosed with a refractory head wound.
Brain CT showed no obvious abnormalities in the skull and brain tissue.
After admission, the patient received routine disinfection treatment. After the wound was fully disinfected, it was covered with sterile gauze, which was fixed with a mesh cap, once every 2 d. After the wound had no secretions, surgical treatment was planned. After 14 d of treatment, the wound showed no signs of healing, with a small amount of secretions still remaining. The patient began feeling pain and was then transferred to the department of rehabilitation. Considering that the patient had a history of trauma and a high white blood cell count, semiconductor laser treatment, ultra violet treatment and ultrashort-wave treatment were administered once a day. After 14 d of treatment, the wound did not heal, and the pain was not relieved. The patient underwent neoplasm resection and skin grafting surgery in the plastic surgery department on November 16, 2017 (Figure 2). The neoplasm was sent for pathological examination during the operation (Figure 3). The rapid pathological results showed angiosarcoma.
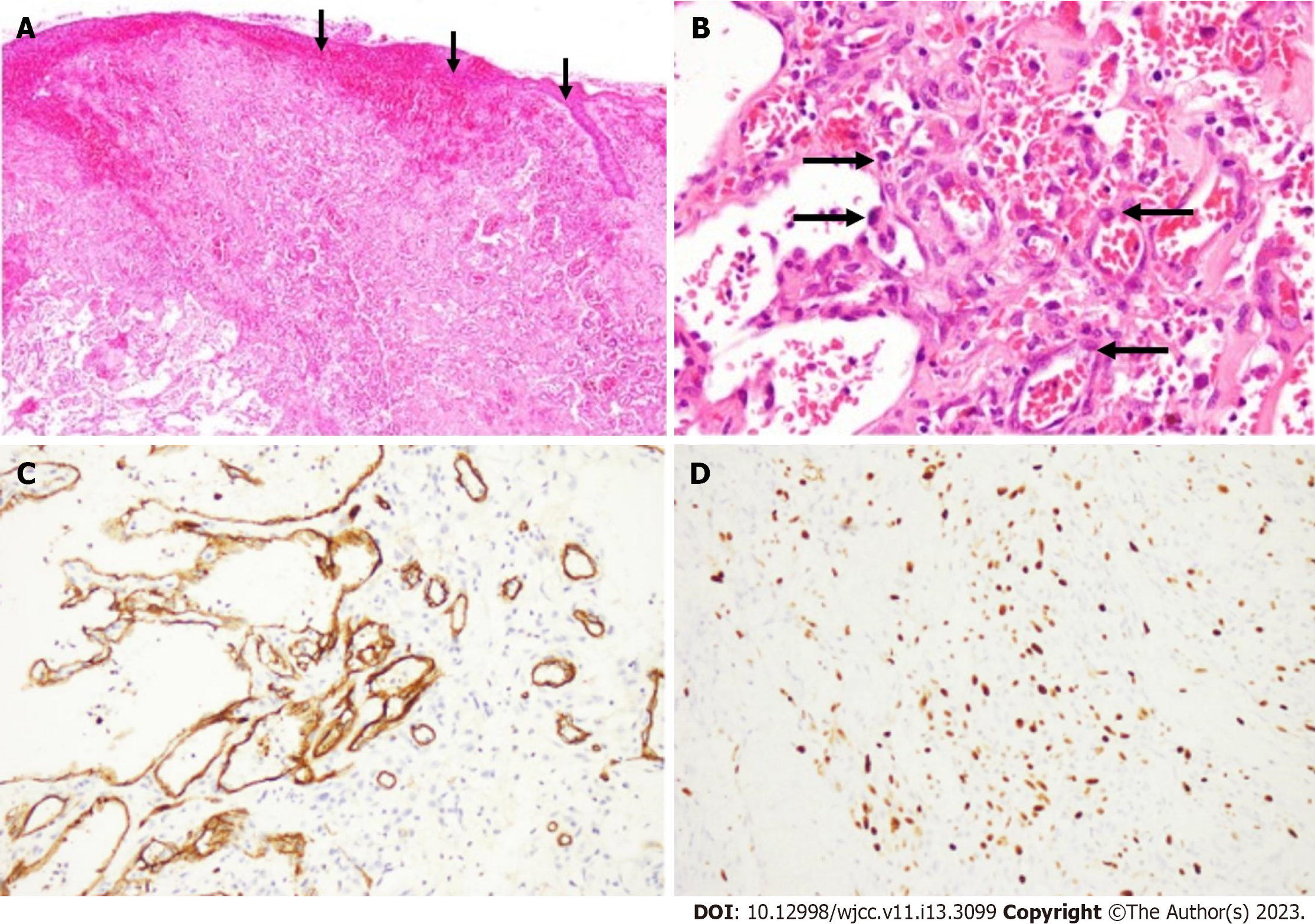
The final pathological results were reported on November 21, 2017 and confirmed scalp angiosarcoma (Figure 4).
No tumor was observed on the front, back, left, and right margins, but the tumor was close to the undercut margin. The patient was advised to undergo radiotherapy, but he discontinued the treatment and was discharged.
A follow-up was continued after the discharge. In March 2018, the wound on the top of the head ruptured again, and disinfection was conducted at home. In August 2018, the patient passed away, the cause of death is the recurrence of tumor.
Angiosarcoma, also known as malignant hemangioendothelioma, is a malignant tumor of blood vessels, originating from endothelial cells. Angiosarcoma can occur in various parts of the body[2,3], such as the head, neck, breasts, limbs and trunk, and most of the tumor is mainly located in the skin. Because of different clinical manifestations and biological behaviors of these malignant vascular proliferations, Enzinger and Weiss in 1983 divided these tumors into 4 groups according to their location: (1) Cutaneous angiosarcoma not related to lymphedema; (2) Angiosarcoma of the skin related to lymphedema, namely, lymphangiosarcoma; (3) Deep soft tissue angiosarcoma; and (4) Breast angiosarcoma. Angiosarcoma of the scalp is the most common form, which mainly affects the skin of the head[4]. This disease occurs more often in the elderly. The skin lesions are characterized by infiltration and expansion to the surrounding or subcutaneous tissues, which involve the scalp, before metastasis. Owing to these extensive infiltrations, the edges of the damage are often unclear. The disease progresses rapidly and can be spread to nearby lymph nodes or to the lungs, liver, bones, etc., through blood circulation. Owing to its highly aggressive and multifocal nature, the prognosis of angiosarcoma is poor, with a 5-year survival rate of less than 35%. Moreover, 75% of patients have local recurrence within 24 mo of local treatment[5].
There is currently no radical cure for angiosarcoma, and the prognosis is poor. The importance of early diagnosis and early treatment is emphasized. Scalp angiosarcoma is the first choice for extensive surgical resection. As far as possible, extensive surgical resection of skin lesions should be performed; otherwise, angiosarcoma is prone to recurrence. For those with multiple or extensive skin lesions, which are difficult to operate, radiotherapy can be used before or after surgery. For patients with distant metastases, chemotherapy-based treatment is the main option, but there is currently no standard chemotherapy regimen[6], and the remission period is short. Cyclophosphamide, epirubicin, vincristine and dacarbazine are often used clinically. Ye et al[7] believed that scalp angiosarcoma recurred and metastasized after surgery. After failure of a first-line chemotherapy, docetaxel, cisplatin, gemcitabine, and radiotherapy can be administered to patients to prolong their overall survival time. For patients with a poor physical status or an old age, monotherapy with taxanes is recommended[8]. For general refractory wounds, using appropriate physical methods can promote wound healing. The patient in this case was older, had high neutrophils in the blood routine at the first visit, exuded fluid on the scalp ulcer wound, had a risk of infection, and could not be treated directly by surgery. Therefore, local physical factor treatment was adopted to reduce the wound exudate and prevent wound infection, but the treatment effect was not ideal, and wound healing was not promoted. The pathological results allowed us to confirm the patient's diagnosis as scalp angiosarcoma. Physical factor therapy is ineffective for scalp angiosarcoma, and it should be noted that some physical factor therapy is contraindicated for the treatment of local tumors. In future clinical work, pathological examination should be performed for refractory ulcers in any part of the skin, and physical factors should be used with caution before the diagnosis is clear, because this may delay the correct treatment plan.
Our research suggests that pathological examination should be performed for refractory ulcers of the scalp, and physical factor therapy should be used with caution before the diagnosis is clear.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Alkhatib AJ, Jordan; Covantsev S, Russia; Guo HR, Taiwan S-Editor: Liu XF L-Editor: A P-Editor: Zhang XD
| 1. | Guadagnolo BA, Zagars GK, Araujo D, Ravi V, Shellenberger TD, Sturgis EM. Outcomes after definitive treatment for cutaneous angiosarcoma of the face and scalp. Head Neck. 2011;33:661-667. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 105] [Cited by in RCA: 128] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 2. | Qitao Huang, Haiming Wei, Lili Li. Angiosarcoma: A case report. Journal of Clinical Dermatology. 2015;44:810-811. |
| 3. | Hillenbrand T, Menge F, Hohenberger P, Kasper B. Primary and secondary angiosarcomas: a comparative single-center analysis. Clin Sarcoma Res. 2015;5:14. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 4. | Cuda J, Mirzamani N, Kantipudi R, Robbins J, Welsch MJ, Sundram UN. Diagnostic utility of Fli-1 and D2-40 in distinguishing atypical fibroxanthoma from angiosarcoma. Am J Dermatopathol. 2013;35:316-318. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 5. | Yu Liang, Jianzhong Cao, Hong Li. Rh-endostatin combined with radiotherapy in treatment of scalp angiosarcoma: Report of one case and review of literatur. Cancer Res. 2017;29:273-275. [DOI] [Full Text] |
| 6. | Fujisawa Y, Yoshino K, Kadono T, Miyagawa T, Nakamura Y, Fujimoto M. Chemoradiotherapy with taxane is superior to conventional surgery and radiotherapy in the management of cutaneous angiosarcoma: a multicentre, retrospective study. Br J Dermatol. 2014;171:1493-1500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 73] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 7. | Ye J, Li XF, Wang YD, Yuan Y. Long-term survival of a patient with scalp angiosarcoma and multiple metastases treated using combination therapy: A case report. Oncol Lett. 2015;9:1725-1728. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 8. | Karube R, Sasaki H, Shinozuka K, Fujisawa Y, Yanagawa T, Yamagata K, Onizawa K, Otsuka F, Bukawa H. Angiosarcoma of the scalp diagnosed by the presence of neck inflammation: a case report. Int J Oral Sci. 2012;4:166-169. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (1)] |