Published online Mar 16, 2022. doi: 10.12998/wjcc.v10.i8.2484
Peer-review started: September 25, 2021
First decision: October 18, 2021
Revised: November 17, 2021
Accepted: January 27, 2022
Article in press: January 27, 2022
Published online: March 16, 2022
Processing time: 166 Days and 15.5 Hours
Aorto-esophageal injury is a rare but life-threatening complication of esophageal foreign bodies, which typically requires open surgery. The best way to treat patients with this condition remains unclear. To date, few reports have described an aortic wall directly penetrated by a sharp foreign body. Here, we present a rare case of a fishbone completely embedded in the esophageal muscularis propria and directly piercing the aorta, which was successfully treated by endoscopy and thoracic endovascular aortic repair (TEVAR).
We report the case of a 71-year-old man with a 1-d history of retrosternal pain after eating fish. No abnormal findings were observed by the emergency esophagoscopy. Computed tomography showed a fishbone that had completely pierced through the esophageal mucosa and into the aorta. The patient refused to undergo surgery for personal reasons and was discharged. Five days after the onset of illness, he was readmitted to our hospital. Endoscopy examination showed a nodule with a smooth surface in the middle of the esophagus. Endoscopic ultrasonography confirmed a fishbone under the nodule. After performing TEVAR, we incised the esophageal mucosa under an endoscope and successfully removed the fishbone. The patient has remained in good condition for 1 year.
Incising the esophageal wall under endoscope and extracting a foreign body after TEVAR may be a feasible option for cases such as ours.
Core Tip: Aorto-esophageal injury is a rare but life-threatening complication of esophageal foreign bodies, which typically requires open surgery. The best way to treat patients with this condition remains unclear. To date, few reports have described an aortic wall directly penetrated by a sharp foreign body. Here, we present a rare case of a fishbone completely embedded in the esophageal muscularis propria and directly piercing the aorta, which was successfully treated by endoscopy and thoracic endovascular aortic repair.
- Citation: Chen ZC, Chen GQ, Chen XC, Zheng CY, Cao WD, Deng GH. Endoscopic extraction of a submucosal esophageal foreign body piercing into the thoracic aorta: A case report. World J Clin Cases 2022; 10(8): 2484-2490
- URL: https://www.wjgnet.com/2307-8960/full/v10/i8/2484.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i8.2484
Esophageal foreign body (EFB) is a common clinical emergency. In the United States, more than 100000 cases of esophageal foreign bodies occur each year[1]. Because of diet habits, animal bones (such as fish bones, poultry bones, etc.) are among the most commonly encountered foreign bodies in China, and most occur in people over 50 years of age[2]. Aorto-esophageal injury is a rare but life-threatening complication of EFB, which typically requires open surgery[3-6]. The best way to treat patients with this condition remains unclear. To date, there have been few reports of a sharp foreign body in the esophagus penetrating the thoracic aorta[7-16], possibly because this type of injury is extremely rare, and most patients do not receive timely treatment.
Here, we present a case of patient in who a fishbone had completely pierced through the esophageal mucosa and into the aorta; the EFB was successfully extracted by means of endoscopy combined with thoracic endovascular aorta repair (TEVAR).
A 71-year-old man presented to our hospital on October 12, 2020, with a 1-d history of retrosternal pain after eating fish.
The patient did not have fever, dysphagia, hematemesis, hematochezia, melena, or other symptoms.
The patient had no previous medical history.
The patient had a free personal and family history.
On physical examination, there were no abnormal findings.
Blood tests showed no obvious abnormalities.
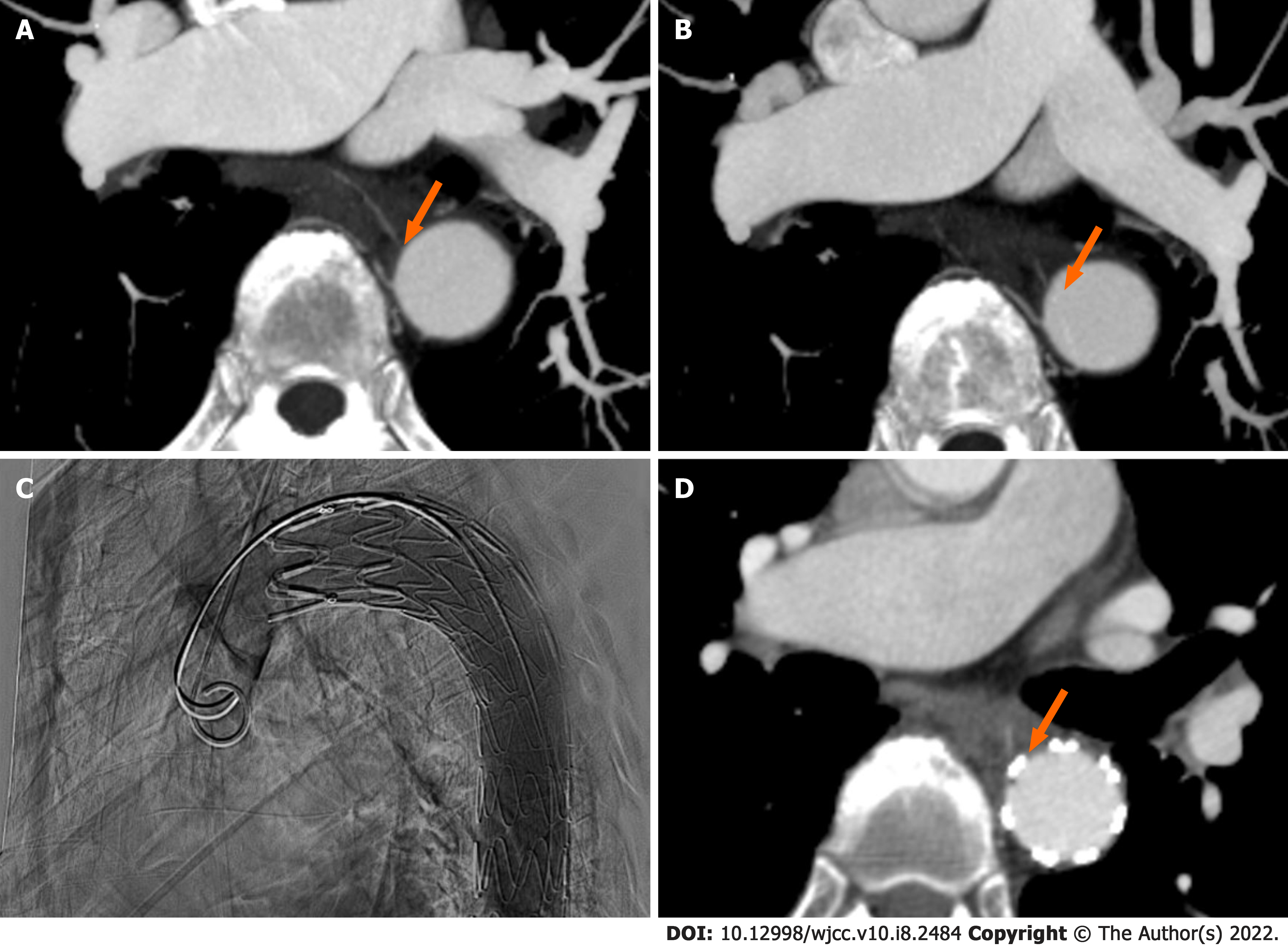
Emergency thoracic computed tomography (CT) (Figure 1A) revealed a high-density shadow of an EFB (highly suspected to be a fishbone) in the middle thoracic section of the esophagus (eighth thoracic vertebra) involving the wall of the thoracic aorta. The patient was admitted to the department of Ear, Nose, and Throat, and no abnormalities were observed in the esophagus after a careful esophagoscopy examination.
On October 13, 2020, enhanced CT angiography (Figure 1B) revealed that an EFB had directly penetrated the thoracic aorta.
Based on previous reports and our experience, our initial plan was to perform TEVAR and then consult with a multidisciplinary team for the next steps. Prior to any treatment, we fully informed the patient of the risk of surgery. It is common for patients and their families to feel hesitant and inquire about alternative treatment options, including by consult with other hospitals. Our patient wished to do such, and was discharged in accordance on October 13, 2020. The other hospital he attended provided an open surgery plan, which the patient chose not to accept. Ultimately, the patient chose to be re-admitted to our hospital, which occurred on October 17, 2020. At that time, we carried out the multidisciplinary team discussion, which led to the choice of a minimally invasive protocol to remove the foreign body using an endoscope after the placement of a thoracic aortic stent.
EFB penetrating the thoracic aorta.
On October 18, 2020, we successfully performed TEVAR (Figure 1C) with placement of an aortic stent (XJZDZ30200; Ankura, Lifetech Scientific Corporation, Shenzhen, China). CT angiography (Figure 1D) after the TEVAR showed that the EFB (suspected fishbone) was pressed against the edge of the blood vessel.
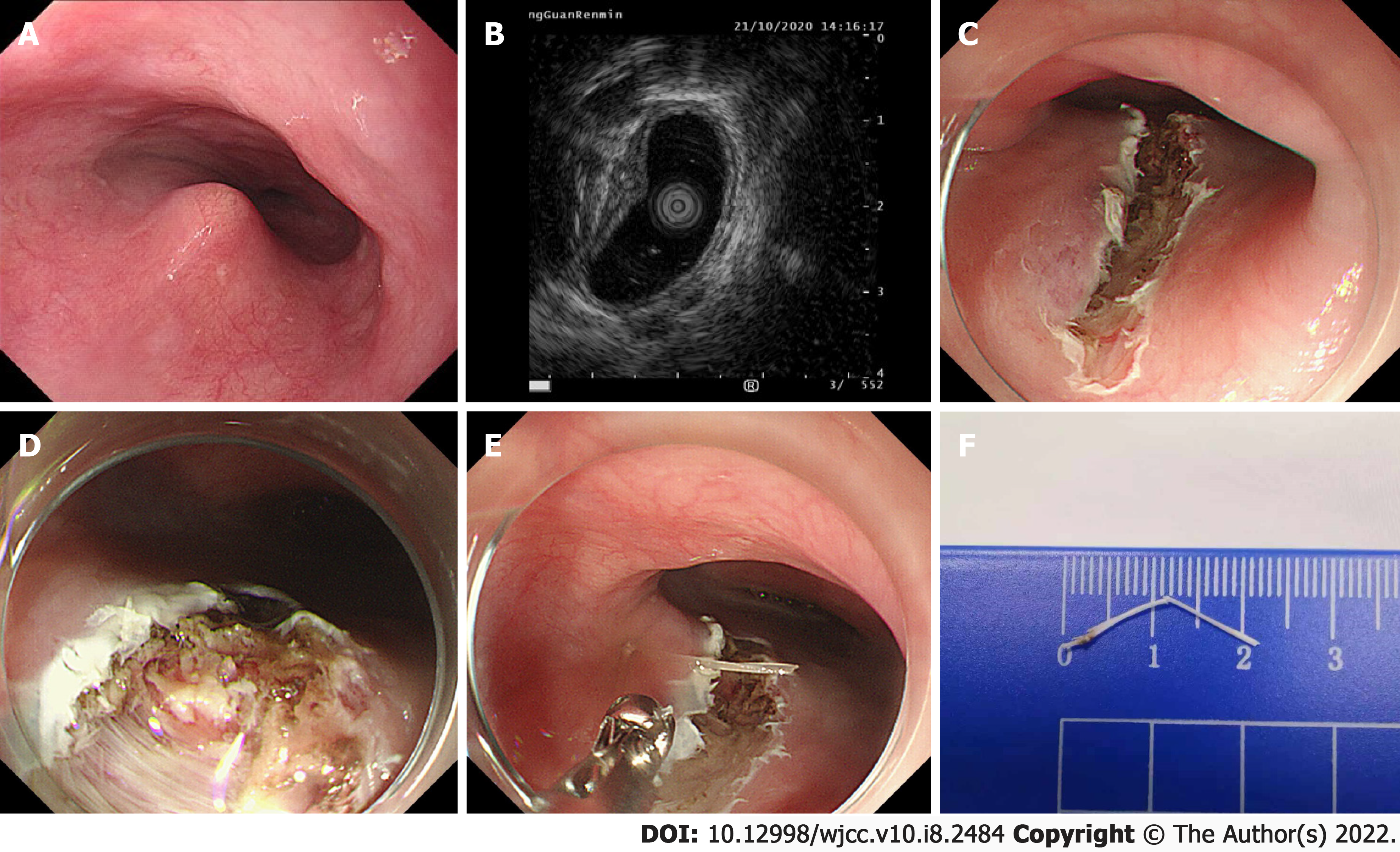
On October 21, 2020, an endoscopic examination (Figure 2A) was performed and a nodule was identified that was about 31 cm away from the incisors, 1.0 cm × 0.8 cm in size and hard, with a fixed position and smooth surface. Endoscopic ultrasonography (Figure 2B) was immediately performed with a 12-MHz probe, revealing a “bone-like image” protruding beyond the muscularis propria under the nodule. Subsequently, endoscopic foreign body removal was performed (Figure 2C–2E) with CO2 gas. First, the nodule was punctured with an injection needle; a small amount of yellow and white pus could be seen. After injection of sodium hyaluronate diluent into the mucous membrane of the superior side, a dual knife and IT knife were used to incise the nodule along the center and the inferior side to the deep part of the esophageal muscularis. The head end of the fishbone (approximately 1.5 mm in length) was found on the distal side of the nodule, and it was pulled out smoothly by use of biopsy forceps.
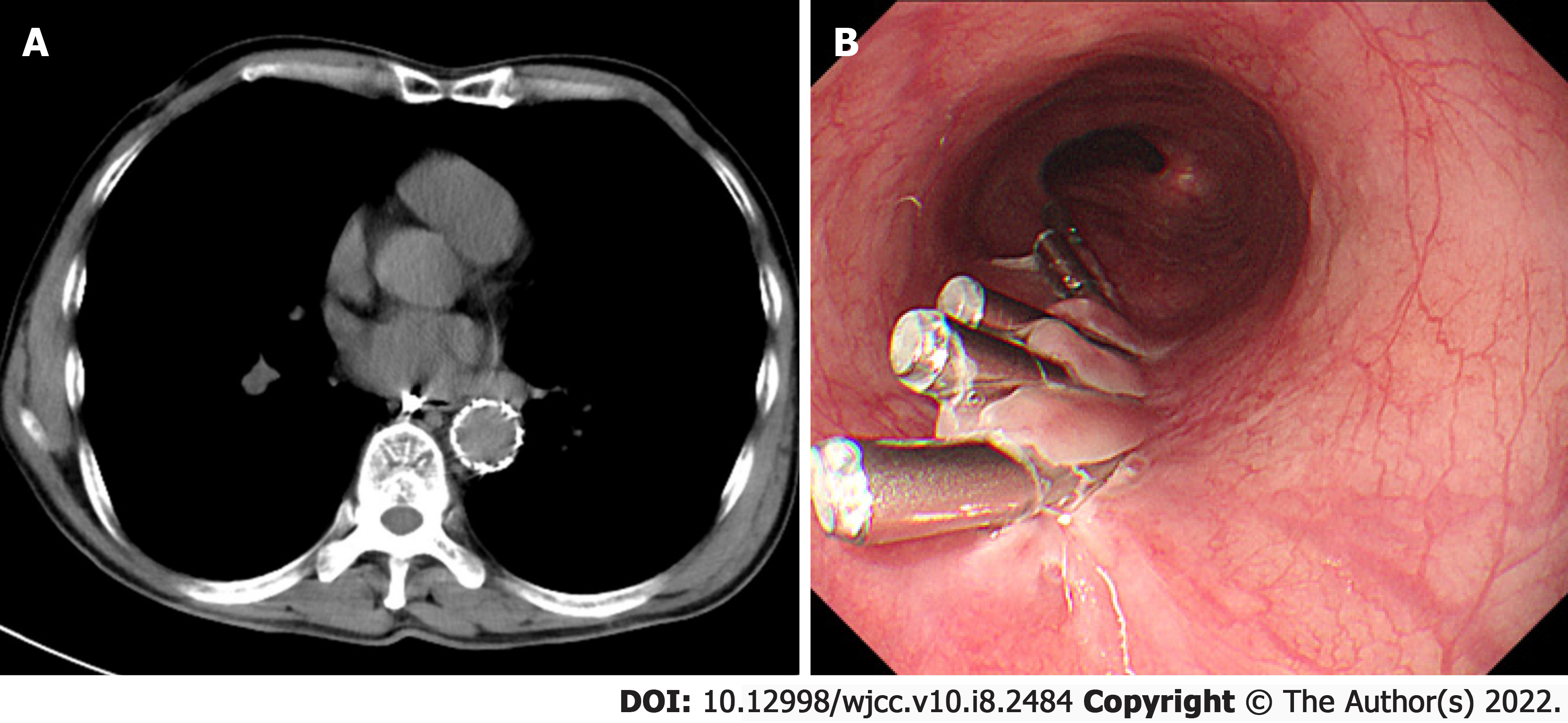
The length of the fishbone was approximately 22 mm (Figure 2F), and there was no breakage. There was also no obvious pus or bleeding at the excision location. As such, the wound was carefully and thoroughly irrigated and then loosely sealed with hemostatic clips. A gastric tube was placed for postoperative drainage, and the patient was continued on antibiotics for the postoperative recovery period. Immediate-postoperative CT scan showed no sign of EFB in the esophagus and mediastinum or aorta, serving as confirmation of successful removal of the fishbone (Figure 3A).
On November 2, 2020, the patient was re-examined with a gastroscope, which showed that the wounds had healed well (Figure 3B), and the gastric tube was removed.
Currently, it has been 1 year since the procedure, and the patient remains in good condition.
Aorto-esophageal injury is a rare but life-threatening complication of EFB, which typically requires open surgery. The invasiveness and high cost of that treatment, however, are remarkable determinants. At the same time, the complication rate of EFB removal and secondary outcome/injury increases with the increase of retention time[17,18]. Indeed, the mortality rate can reach 40%–60% if aorto-esophageal fistula arises[19] and such cases need to be treated as soon as possible. With the development of technology, there have been reports of successful minimally invasive treatment of similar patients in recent years. Hanif et al[13] reported a case of a 63-year-old man with a 2.7 cm-long chicken bone penetrating the esophageal wall and transversing into the aorta; treatment via an endoscopic approach with simultaneous endovascular stent-graft repair of the aorta was successful. Choi et al[10] reported a case of a 31-year-old man with a fishbone-induced aortic rupture that was successfully treated with an endovascular stent-graft, with the patient remaining in good condition at the 7-mo follow-up. Xi et al[15] reported a case of a sharp foreign object-induced aortic rupture with mediastinitis and pseudoaneurysm, which was successfully treated by exploratory thoracotomy after endovascular stent-graft repair. Zeng et al[8] reported a case similar to ours, in which a foreign body had lodged in the esophagus and caused a consequent aortic rupture; that case was successfully treated by endovascular stent-graft repair and endoscopic procedure. Ruan et al[20] summarized their experience of 12 patients with EFB combined with aortic injury, 11 of which were successfully removed after TEVAR. These reports highlight that when EFB combined with aortic injury has occurred, it has been safe to remove the EFB after TEVAR.
It is also rare that an EFB is embedded in the wall of the esophagus. Wang et al[21] had reported such a case and they extracted the fishbone using the endoscopic submucosal dissection method; however, the fishbone had not injured the aorta, as in our case.
Our case was unique, with the combination of an EFB embedded in the esophageal wall and causing aortic injury, which increased the difficulty and risk of extraction by standard means of an endoscope. We speculate that the reason why we did not see the fishbone during our initial esophagoscopy is that most fishbones puncturing the esophagus do not transverse it or subsequently puncture other organs, and the foreign body itself was relatively small. The nodules observed by the gastroscope may have resulted from the fishbone being ejected from a blood vessel after the indwelling aortic stent was placed, ultimately bouncing back to the esophageal wall. Consequent local inflammation would have resulted in tissue edema and formed a nodule after 5 d. In multidisciplinary discussions, we established the following four goals: prevention of hemorrhaging, removal of the EFB (suspected fishbone), repair of wounds, and control of infection. The safety of removing the EFB (fishbone) by endoscope increased after successfully repairing the thoracic aorta with a graft-stent. CT results showed that the fishbone had been pushing outside the lumen of the aorta, which increased our confidence in removing it without causing damage to the artery. To accurately locate the fishbone, we performed endoscopic ultrasonography after identifying a nodule in the cavity, which showed the stump of the fishbone located in the submucosa; however, extracting it was a practical challenge. Because we could not obtain direct visual access to the foreign object under the endoscope, incising the mucosa was necessary. The risk of incising the mucosa was that moving the foreign body may damage the stent membrane, which can lead to massive hemorrhaging. Thus, the incision process needs to be very carefully performed. We prepared a dilatation balloon for hemostasis. The vascular intervention department and cardiothoracic surgeon remained on standby for placement of another stent or open surgery. Considering the possibility of conversion to surgery, full informed consent was necessary and had been obtained.
After removal of the fishbone, preventing infection was the next challenge. To prevent further infection after the surgery, we administered imipenem (1 g intravenous drip twice a day for 10 d) for anti-infection treatment. The patient was discharged on November 2, 2020 and remains in good condition as of the writing of this case report (1 year after the procedure).
There are some limitations to our report that should be considered before applying this knowledge to other cases. In principle, EFBs should be treated urgently (recommended: ≤ 24 h), because the longer duration of presence, the higher the incidence of complications[17,18]. The fishbone in our patient had been retained for 5 d without manifestation of other serious complications, which may have been due to its very small size and the timely application of antibiotics. However, it is still unclear whether the location, shape and size of any foreign body will affect the success rate of TEVAR.
In conclusion, aortic injury caused by an EFB can be life-threatening. In rare conditions, the EFB will be embedded in the esophageal wall and pierce into the aorta. Our case suggested that incising the esophageal wall and extracting the foreign body after TEVAR may be a feasible option for this kind of EFB. But, the appropriate timing of the procedure and whether the size and location of foreign bodies in the esophagus affect successful treatment remain unclear.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Cabezuelo AS, Okasha HH S-Editor: Xing YX L-Editor: A P-Editor: Xing YX
| 1. | Longstreth GF, Longstreth KJ, Yao JF. Esophageal food impaction: epidemiology and therapy. A retrospective, observational study. Gastrointest Endosc. 2001;53:193-198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 161] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 2. | Zhong Q, Jiang R, Zheng X, Xu G, Fan X, Xu Y, Liu F, Peng C, Ren W, Wang L. Esophageal foreign body ingestion in adults on weekdays and holidays: A retrospective study of 1058 patients. Medicine (Baltimore). 2017;96:e8409. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Nandi P, Ong GB. Foreign body in the oesophagus: review of 2394 cases. Br J Surg. 1978;65:5-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 406] [Cited by in RCA: 365] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 4. | Ctercteko G, Mok CK. Aorta-esophageal fistula induced by a foreign body: the first recorded survival. J Thorac Cardiovasc Surg. 1980;80:233-235. [PubMed] |
| 5. | Hollander JE, Quick G. Aortoesophageal fistula: a comprehensive review of the literature. Am J Med. 1991;91:279-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 221] [Cited by in RCA: 234] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 6. | Zhang X, Liu J, Li J, Hu J, Yu F, Li S, Yang X. Diagnosis and treatment of 32 cases with aortoesophageal fistula due to esophageal foreign body. Laryngoscope. 2011;121:267-272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 7. | Jiang D, Lu Y, Zhang Y, Hu Z, Cheng H. Aortic penetration due to a fish bone: a case report. J Cardiothorac Surg. 2020;15:292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Zeng L, Shu W, Ma H, Hu J. Aortic injury caused by esophageal foreign body-case reports of 3 patients and literature review. Medicine (Baltimore). 2020;99:e20849. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 9. | Sica GS, Djapardy V, Westaby S, Maynard ND. Diagnosis and management of aortoesophageal fistula caused by a foreign body. Ann Thorac Surg. 2004;77:2217-2218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 38] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 10. | Choi J, Lee S, Moon J, Choi H. Fish bone induced aortic rupture treated with endovascular stent graft. Eur J Cardiothorac Surg. 2009;35:360. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Kelly SL, Peters P, Ogg MJ, Li A, Smithers BM. Successful management of an aortoesophageal fistula caused by a fish bone--case report and review of literature. J Cardiothorac Surg. 2009;4:21. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 34] [Cited by in RCA: 41] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 12. | Chen X, Li J, Chen J, Zhou Y, Zhang Y, Ding H, Huang S, Zhang Z. A combined minimally invasive approach for the treatment of aortoesophageal fistula caused by the ingestion of a chicken bone: case report and literature review. Clinics (Sao Paulo). 2012;67:195-197. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 19] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 13. | Hanif MZ, Li D, Jabeen S, Fan Q. Endovascular repair in penetrating aortoesophageal foreign body injury. Ann Thorac Surg. 2013;96:1457-1459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 14. | Ko SF, Lu HI, Ng SH, Kung CT. Fishbone penetration of the thoracic esophagus with prolonged asymptomatic impaction within the aorta. J Vasc Surg. 2013;57:518-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Xi EP, Zhu J, Zhu SB, Liu Y, Yin GL, Zhang Y, Zhang XM, Dong YQ. Surgical treatment of aortoesophageal fistula induced by a foreign body in the esophagus: 40 years of experience at a single hospital. Surg Endosc. 2013;27:3412-3416. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 16. | Ding X, Su Q, Zhong N, Jiang J. Endoscopic extraction of a fish bone with a Foley catheter after endovascular stent graft placement for penetrating aortoesophageal injury. Endoscopy. 2015;47 Suppl 1 UCTN:E406-E407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Loh KS, Tan LK, Smith JD, Yeoh KH, Dong F. Complications of foreign bodies in the esophagus. Otolaryngol Head Neck Surg. 2000;123:613-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 98] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 18. | Vidarsdottir H, Blondal S, Alfredsson H, Geirsson A, Gudbjartsson T. Oesophageal perforations in Iceland: a whole population study on incidence, aetiology and surgical outcome. Thorac Cardiovasc Surg. 2010;58:476-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 83] [Cited by in RCA: 101] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 19. | Takeno S, Ishii H, Nanashima A, Nakamura K. Aortoesophageal fistula: review of trends in the last decade. Surg Today 2019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 20. | Ruan WS, Lu YQ. The life-saving emergency thoracic endovascular aorta repair management on suspected aortoesophageal foreign body injury. World J Emerg Med. 2020;11:152-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Wang XM, Yu S, Chen X. Successful endoscopic extraction of a proximal esophageal foreign body following accurate localization using endoscopic ultrasound: A case report. World J Clin Cases. 2019;7:1230-1233. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |