Published online Feb 6, 2022. doi: 10.12998/wjcc.v10.i4.1410
Peer-review started: September 3, 2021
First decision: October 29, 2021
Revised: November 10, 2021
Accepted: December 25, 2021
Article in press: December 25, 2021
Published online: February 6, 2022
Processing time: 143 Days and 4.8 Hours
Hoffa fracture is rare, especially in adolescents, and has a high rate of complications such as avascular necrosis and osteoarthritis; moreover, there are no definitive guidelines for its treatment. This report could provide a new potential treatment for Hoffa fracture.
A 16-year-old girl presented to the orthopedic emergency department of No. 2 People’s Hospital of Yibin City with persistent pain following a right knee injury sustained during a sprint race. Her knee was swollen and tender, and the range of motion was restricted by the pain. X-ray and computed tomography revealed a Hoffa fracture in the right knee. After consultation, surgical treatment was performed, and the fracture was fixed with three 3.5-mm cannulated cancellous screws; osteochondral plugs that were harvested from the screw insertion site were re-implanted to cover the screw head. The patient’s fracture and osteo
Here, we describe an innovative surgical procedure for Hoffa fracture that could provide a new possibility for the treatment of similar fractures, and further improve their management.
Core Tip: A 16-year-old girl presented to our orthopedic emergency department with persistent pain following a right knee injury sustained during a sprint race. On examination, the right knee was swollen and tender with decreased range of motion. Laboratory examination revealed no obvious abnormality. She was treated by open reduction and internal fixation with osteochondral plug re-implantation, and had no postoperative complications. The fracture and osteochondral plug had completely healed, 6 mo postoperatively.
- Citation: Jiang ZX, Wang P, Ye SX, Xie XP, Wang CX, Wang Y. Hoffa’s fracture in an adolescent treated with an innovative surgical procedure: A case report. World J Clin Cases 2022; 10(4): 1410-1416
- URL: https://www.wjgnet.com/2307-8960/full/v10/i4/1410.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i4.1410
Hoffa fracture, a fracture of the femoral condyle in the coronal plane involving one or both of the condyles, was first described in 1904 by Hoffa[1]. The conventional classification system includes the three subtypes proposed by Letenneur et al[2]. The diagnosis of these fractures is challenging, since they are easily misdiagnosed and missed in anteroposterior X-rays, because the unfractured condylar part of the femur can obscure the fractured condyle[3]. Therefore, when Hoffa's fracture is suspected, further computed tomography (CT) is necessary. This is an uncommon injury in adults, which is even rarer in adolescents. It accounts for 8.7% to 13% of distal femoral fractures[4]. There are no data on the potential injury mechanism. Although in children and individuals with osteoporosis, low-energy trauma can produce the lesion, the main cause of a Hoffa fracture is a high-energy injury (e.g., a traffic collisions or a fall)[5,6]. Surgical treatment, anatomical reduction, and stable fixation are recommended to reduce the rate of complications, such as arthritis, nonunion, and osteonecrosis[7]. However, as far as the literature reports, there is no optimal surgical approach and fixation method[3]. Hence, we present the case of an adolescent girl with a medial condyle fracture (type III) of the distal femur, which was successfully managed with an innovative surgical procedure. We hope to provide a new possibility for the treatment of similar fractures, and further improve their management.
A 16-year-old girl presented to our orthopedic emergency department with sustained pain following a right knee injury in a sprint race.
She felt persistent pain in her right knee and was unable to walk normally. She had no other symptoms, including dizziness, headache, chest tightness, and abdominal pain.
She had no other history of past illnesses.
She had no genetic or familial disease history.
On examination, the patient's vital signs were stable. Right knee was swollen and tender with bone crepitation and decreased range of motion. There were no open wounds or distal neurovascular deficits.
Laboratory examination revealed no obvious abnormality.
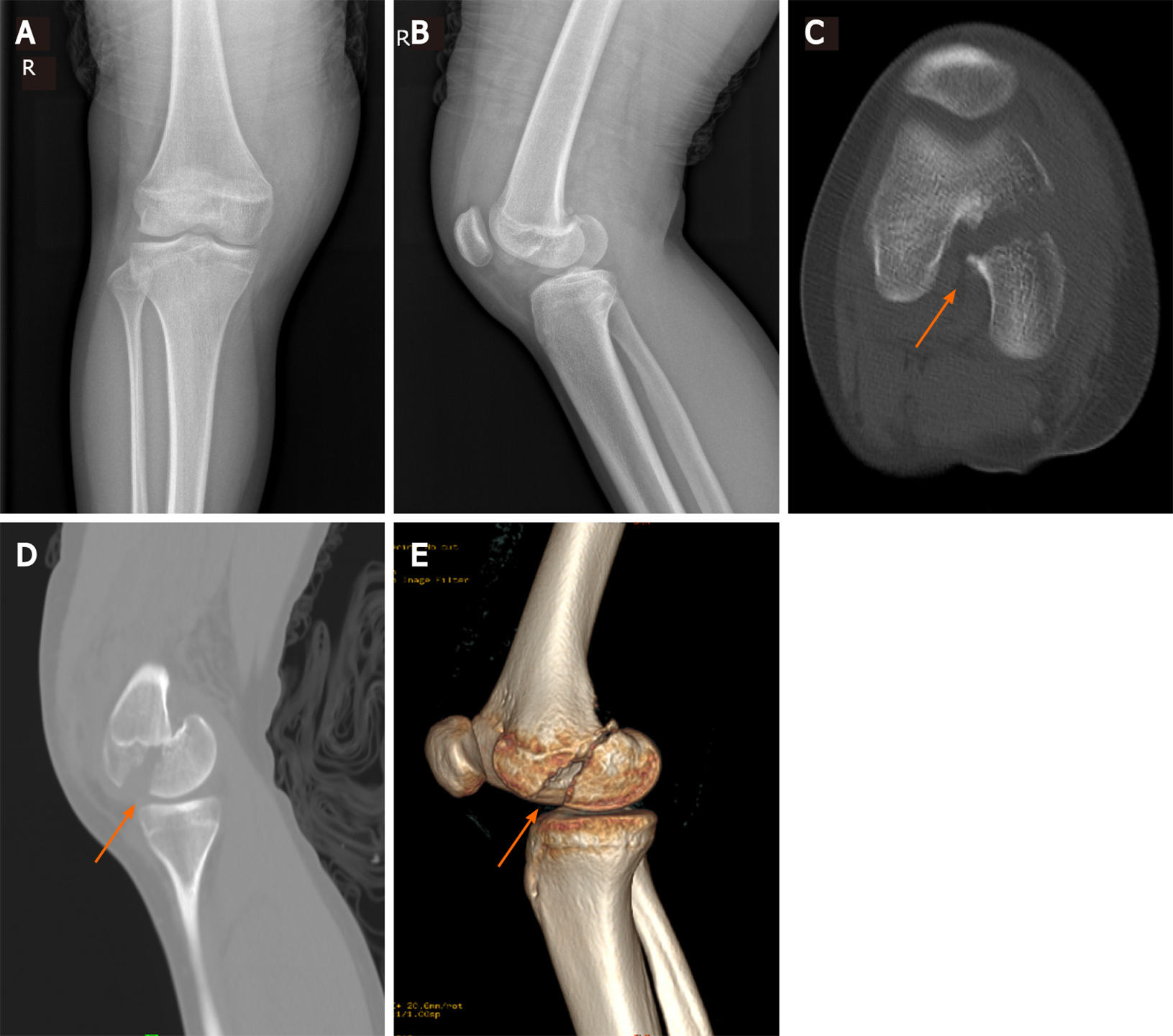
Knee radiographs and CT images confirmed a coronal plane fracture of the posterior part of the medial femoral condyle with epiphyseal injury (Figure 1).
Hoffa fracture.
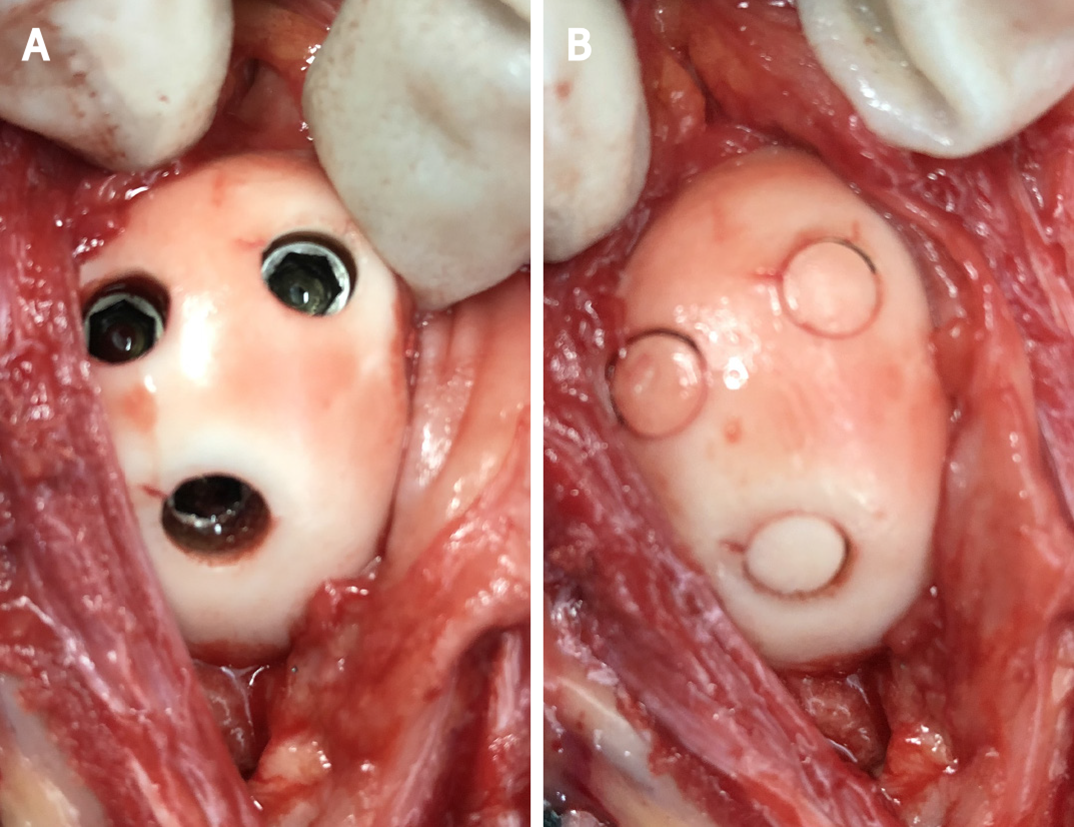
Following examination and under anesthesia, the patient was placed in the prone position, with the knee stabilized and locked in a flexed 30° position. The fracture was accessed through a posteromedial incision to the knee. Under X-ray guidance, the medial femoral condyle fragment was reduced and temporarily fixed with Kirschner wires. A 5.0 mm annular drill (Wellbone, Suzhou, China) was used to remove the 5.0 mm × 5.0 mm cylindrical articular cartilage and subchondral bone. After fixing the fragment with three 3.5 mm partially threaded cancellous screws (inserted in a posterior-to-anterior direction), the articular cartilage and subchondral bone were re-implanted in situ and the screw heads were covered (Figure 2) to ensure stability and ease upon pressure. Postoperatively, the limb was maintained on a long-leg back slab with the knee in a 30° flexion position for approximately 2 wk. Active isometric muscle contractions were permitted during this period. Subsequently, the slab was removed, and passive flexion and extension exercises were initiated.
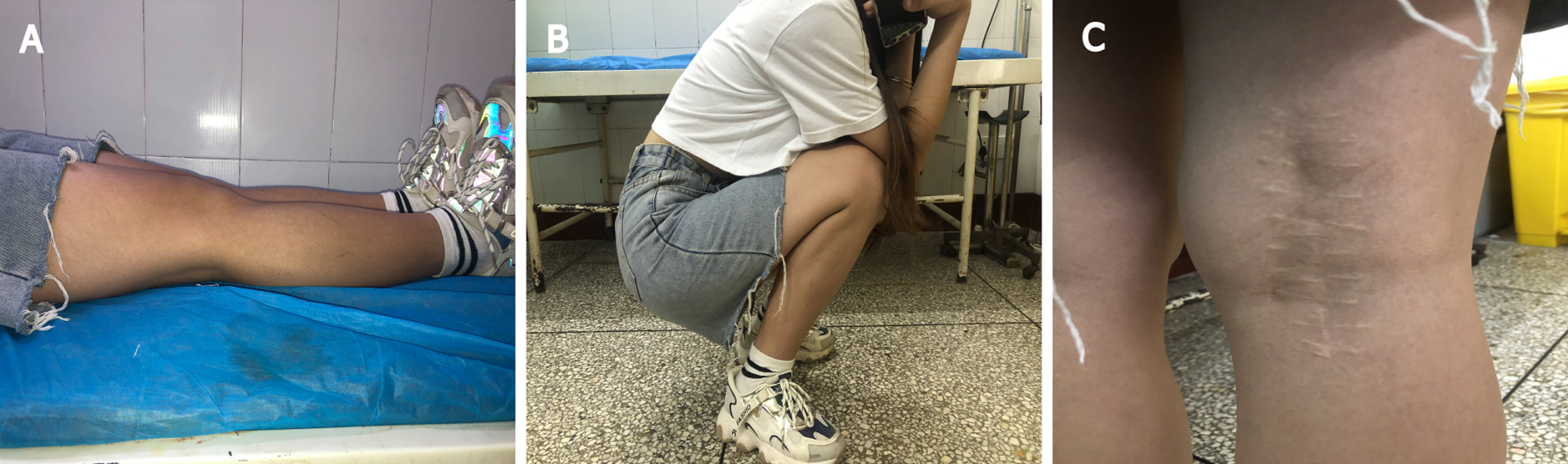
Upon radiographic monitoring, weight-bearing was gradually permitted at 2 mo. At the 6-mo follow-up, the patient presented a knee range of motion of 0°–135° without pain, and was walking without support with a normal gait (Figure 3). The fracture and osteochondral plug had completely healed. There were no signs of avascular necrosis of the femoral condyle or knee osteoarthritis (Figure 4). The patient and her parents provided consent for the publication of the images.
A coronal fracture of the distal femur is termed as Hoffa fracture; Letenneur et al[2] divided it into three types according to the relationship between the fracture line and the posterior cortex of the femoral shaft in 1978[2]. Type I is a fracture in the posterior cortical extension of the distal femur. Type II fracture is similar to type I fracture, but the fracture line is closer to the posterior condyle, and is further divided into A, B, and C subtypes based on the distance. Type III is a fracture oblique to the femur condyle, and can be divided into the medial, lateral, or conjoint bicondylar fracture according to the fracture site[1,8,9]. A summary of the main surgical approaches and fixation methods for different Hoffa fracture types is provided in Table 1[10-16]. There is no optimal surgical approach and fixation method for Hoffa fractures as described in Table 1. Direct lateral/medial and posterolateral approaches can expose small Hoffa fragments and employ the more biologically advantageous posterior-anterior direction screws, as well as a plate if necessary, but with a risk of neurovascular injury; lateral/medial parapatellar approaches are suitable for large Hoffa fragments and can expose both the femoral condyles, but small Hoffa fragments are difficult to expose and reduce, and posterior-anterior direction screws are not feasible[17]. Other studies[18-21] reported the treatment of the nonunion of Hoffa fracture, suggesting bone grafting following debridement and fixation with screws and bone plates, and finally achieved satisfactory results. Currently, there is no optimal surgical approach and fixation method[3]; hence, the treatment of the different types of Hoffa fractures are mainly determined by the experience and skill of the surgeon. Studies have demonstrated that the biomechanics of the screws in the posterior-anterior direction are superior to the screws in the anterior-posterior direction[22,23].Furthermore, if the fracture is small, such as a type II fracture, posterior-anterior direction screws are strongly recommended except for the type II C fracture[11]. Therefore, the posterior- anterior direction screws should be preferred for Hoffa fractures. However, this will inevitably damage the articular cartilage when holes are punched in the articular surface. Even though Borse et al[14] attempted to avoid damage to the articular cartilage by using headless screws, the cartilage was still damaged to a certain extent. However, the method we provide solves this problem well. Our paper reports a rare case; although open isolated Hoffa fractures of the medial femoral condyle have been reported in children[24], no study has reported a similar case treated by open reduction and internal fixation with osteochondral plug re-implantation.
| Condyle | Approach | Fixation technique | Letenneur classifification | Ref. |
| Lateral | LPPA | A-P screw | Ⅰ, Ⅲ | Singh et al[10] |
| Posterolateral | Suture | ⅡC | Tan et al[11] | |
| Direct lateral | P-A screw | ⅡB | Egol et al[12] | |
| Medial | MPPA | A-P screw | Ⅲ | Dhillon et al[13] |
| Direct medial | P-A screw | Ⅲ | Borse et al[14] | |
| Bicondylar | Lateral incision | Screw plus plate | Not mentioned | Agarwal et al[15] |
| Swashbuckler approach | A-P screw | Not mentioned | Ul Haq et al[16] |
This type of fracture has a high rate of complications, such as avascular necrosis and osteoarthritis, owing to the subsequent reduction of blood supply to the area and the absence of soft tissue attachment. Surgical stabilization is the preferred treatment for Hoffa’s fractures to achieve satisfactory long-term functional results[25]. In our case, we chose the posteromedial approach to access the knee and used the screws to fix the fragment. The articular cartilage and subchondral bone at the location of the screw were removed in advance, and the head of the screw lowered following its fixation; the articular cartilage and subchondral bone were re-implanted and used to cover the screw heads. Similar to osteochondral autograft implantation, osteochondral plug re-implantation in situ can reduce the extent of cartilage damage. Osteochondral autograft implantation is commonly used in articular cartilage defects, and excellent results have been achieved[26]. This report offers similar methods. The osteochondral plug healed successfully, because fragmentation of healthy cartilage is meant to activate the mitogenic activity of chondrocytes, which proliferate and secrete extracellular matrix to repair damaged cartilage tissue in vivo[27]. We obtained sufficient stability between the fragments, and minimized the damage to the articular cartilage attributed to the surgical procedure. The fracture and osteochondral plug healed, and joint function improved 6 mo postoperatively.
The potential risks, the non-healing and failure of the osteochondral plugs, and minor difficulties in removing the internal fixation when necessary are the potential problems that need to be resolved.
To date, a similar surgical treatment has not been reported in the literature. We believe that this innovative surgical procedure could provide a new possibility for the treatment of Hoffa fracture, and further improve the treatment system in patients with similar conditions; however, more cases are warranted to confirm our claims.
We would like to thank the nursing team of the Department of Orthopedics, No. 2 People’s Hospital of Yibin City, for the support, and our patient for participating in this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: cascella M, Shekouhi R S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Hoffa A. Lehrbuch der Frakturen und Luxationen. Stuttgart: Verlag von Ferdinand Enke; 1904: 451. |
| 2. | Letenneur J, Labour PE, Rogez JM, Lignon J, Bainvel JV. [Hoffa's fractures. Report of 20 cases (author's transl)]. Ann Chir. 1978;32:213-219. [PubMed] |
| 3. | Mierzwa AT, Toy KA, Tranovich MM, Ebraheim NA. Surgical Approaches, Postoperative Care, and Outcomes Associated with Intra-Articular Hoffa Fractures: A Comprehensive Review. JBJS Rev. 2019;7:e8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (1)] |
| 4. | Gavaskar AS, Tummala NC, Krishnamurthy M. Operative management of Hoffa fractures--a prospective review of 18 patients. Injury. 2011;42:1495-1498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 5. | Trikha V, Das S, Gaba S, Agrawal P. Analysis of functional outcome of Hoffa fractures: A retrospective review of 32 patients. J Orthop Surg (Hong Kong). 2017;25:2309499017718928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 6. | Hill BW, Cannada LK. Hoffa Fragments in the Geriatric Distal Femur Fracture: Myth or Reality? Geriatr Orthop Surg Rehabil. 2017;8:252-255. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Somford MP, van Ooij B, Schafroth MU, Kloen P. Hoffa nonunion, two cases treated with headless compression screws. J Knee Surg. 2013;26 Suppl 1:S89-S93. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 8. | Lal H, Bansal P, Khare R, Mittal D. Conjoint bicondylar Hoffa fracture in a child: a rare variant treated by minimally invasive approach. J Orthop Traumatol. 2011;12:111-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 35] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 9. | Julfiqar, Huda N, Pant A. Paediatric conjoint bicondylar Hoffa fracture with patellar tendon injury: An unusual pattern of injury. Chin J Traumatol. 2019;22:246-248. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Singh R, Singh RB, Mahendra M. Functional Outcome of Isolated Hoffa Fractures Treated with Cannulated Cancellous Screw. Malays Orthop J. 2017;11:20-24. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Tan Y, Li H, Zheng Q, Li J, Feng G, Pan Z. A modified posterolateral approach for Hoffa fracture. Eur J Orthop Surg Traumatol. 2014;24:1321-1323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Egol KA, Broder K, Fisher N, Konda SR. Repair of Displaced Partial Articular Fracture of the Distal Femur: The Hoffa Fracture. J Orthop Trauma. 2017;31 Suppl 3:S10-S11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Dhillon MS, Mootha AK, Bali K, Prabhakar S, Dhatt SS, Kumar V. Coronal fractures of the medial femoral condyle: a series of 6 cases and review of literature. Musculoskelet Surg. 2012;96:49-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 14. | Borse V, Hahnel J, Cohen A. Hoffa fracture: fixation using headless compression screws. Eur J Trauma Emerg Surg. 2010;36:477-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 29] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 15. | Agarwal S, Giannoudis PV, Smith RM. Cruciate fracture of the distal femur: the double Hoffa fracture. Injury. 2004;35:828-830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Ul Haq R, Modi P, Dhammi I, Jain AK, Mishra P. Conjoint bicondylar Hoffa fracture in an adult. Indian J Orthop. 2013;47:302-306. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 19] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 17. | Orapiriyakul W, Apivatthakakul T, Buranaphatthana T. How to determine the surgical approach in Hoffa fractures? Injury. 2018;49:2302-2311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 24] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 18. | Soni A, Kansay R, Gupta S, Malhotra A. In Situ Fixation of Symptomatic Fibrous Non-union Hoffa Fracture: A Case Report. Malays Orthop J. 2019;13:57-59. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 19. | Nandy K, Raman R, Vijay RK, Maini L. Non-union coronal fracture femoral condyle, sandwich technique : A case report. J Clin Orthop Trauma. 2015;6:46-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 20. | Jiang YR, Wang ZY, Zhang DB, Gu GS. Twenty-seven-year nonunion of a Hoffa fracture in a 46-year-old patient. Chin J Traumatol. 2015;18:54-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 2.1] [Reference Citation Analysis (1)] |
| 21. | Zhang P, Zhang XZ, Tao FL, Li QH, Zhou DS, Liu FX. Surgical Treatment and Rehabilitation for Hoffa Fracture Nonunion: Two Case Reports and a Literature Review. Orthop Surg. 2020;12:1327-1331. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 22. | Jarit GJ, Kummer FJ, Gibber MJ, Egol KA. A mechanical evaluation of two fixation methods using cancellous screws for coronal fractures of the lateral condyle of the distal femur (OTA type 33B). J Orthop Trauma. 2006;20:273-276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 61] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 23. | Arastu MH, Kokke MC, Duffy PJ, Korley RE, Buckley RE. Coronal plane partial articular fractures of the distal femoral condyle: current concepts in management. Bone Joint J. 2013;95-B:1165-1171. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 24. | Bali K, Mootha AK, Prabhakar S, Dhillon MS. Isolated Hoffa fracture of the medial femoral condyle in a skeletally immature patient. Bull NYU Hosp Jt Dis. 2011;69:335-338. [PubMed] |
| 25. | Flanagin BA, Cruz AI, Medvecky MJ. Hoffa fracture in a 14-year-old. Orthopedics. 2011;34:138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | de l'Escalopier N, Barbier O, Mainard D, Mayer J, Ollat D, Versier G. Outcomes of talar dome osteochondral defect repair using osteocartilaginous autografts: 37 cases of Mosaicplasty®. Orthop Traumatol Surg Res. 2015;101:97-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 24] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 27. | Salzmann GM, Ossendorff R, Gilat R, Cole BJ. Autologous Minced Cartilage Implantation for Treatment of Chondral and Osteochondral Lesions in the Knee Joint: An Overview. Cartilage. 2020;1947603520942952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 55] [Article Influence: 13.8] [Reference Citation Analysis (0)] |