Published online Feb 6, 2022. doi: 10.12998/wjcc.v10.i4.1320
Peer-review started: August 4, 2021
First decision: November 6, 2021
Revised: November 7, 2021
Accepted: December 23, 2021
Article in press: December 23, 2021
Published online: February 6, 2022
Processing time: 172 Days and 17.9 Hours
The radial nerve (RN) splits into two main branches at the elbow: The superficial branch of RN (SBRN) and the deep branch of RN. The SBRN can be easily damaged in acute trauma due to its superficial feature.
A 55-year-old male patient injured his right wrist 10 mo ago. Debridement, suturing and bandaging were performed in the emergency room. Six months after the scar had healed, he felt numbness and tingling in the dorsal surface of the thumb of the right hand. So the surgery of resection and SBRN anastomosis were performed. The pathological findings showed it as traumatic neuroma. Four months after surgery, the patient felt numbness and tingling in the right dorsal surface of the thumb again. The tenderness was marked in the operated area. Ultrasound indicated that the SBRN was adhered to the surrounding tissue. The patient refused further surgical treatment and underwent ultrasound-guided needle release plus corticosteroid injection of the SBRN. Four weeks later, the tenderness in the surgical area was reduced by 70%, the numbness in the dorsal surface of the thumb of the right hand was reduced by 40% and the nerve swelling evaluated by ultrasound was reduced. Four months passed, he did not feel any numbness or tingling sensation of his right wrist. This is the first report of ultrasound-guided needle release plus corticosteroid injection of the SBRN.
Ultrasound can evaluate the condition of the RN, and the relationship with surrounding tissues. Ultrasound-guided needle release plus corticosteroid injection is an effective and safe treatment for SBRN adhesion.
Core Tip: A patient felt numbness and tingling in the right dorsal surface of the thumb four months after traumatic neuroma resection and the superficial branch anastomosis. Ultrasound revealed that the superficial branch was adhered to the surrounding tissue. Four weeks after ultrasound-guided needle release plus corticosteroid injection of the superficial branch, the tenderness and numbness both reduced thus indicating ultrasound-guided needle release plus corticosteroid injection is an effective and safe treatment for superficial branch adhesion.
- Citation: Zeng Z, Chen CX. Ultrasound-guided needle release plus corticosteroid injection of superficial radial nerve: A case report. World J Clin Cases 2022; 10(4): 1320-1325
- URL: https://www.wjgnet.com/2307-8960/full/v10/i4/1320.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i4.1320
The radial nerve (RN) is the largest branch of the brachial plexus posterior cord. It splits into two main branches at the elbow: The superficial branch of RN (SBRN) and the deep branch of RN[1,2]. The RN supplies the skin of the dorsal forearm, the dorsal-radial region of the hand and the muscle of the extensor compartment[1,2].
Ultrasound (US) is currently used as an imaging modality to observe nerves, especially superficial nerves[3]. The RN has a twisted course in the upper limb and is superficial enough to be accurately found using an ultrasonic high frequency probe[1,2]. Herein, we report a patient who had numbness and tingling in the dorsal surface of the thumb after traumatic neuroma resection plus SBRN anastomosis. Treatment consisted of US-guided needle release plus corticosteroid injection of the SBRN. Tenderness and numbness were reduced 4 wk after treatment.
A 55-year-old male patient presented to the department of ultrasound with numbness and tingling in the dorsal surface of the right thumb.
The patient injured his right wrist 10 mo previously. Debridement, suturing and bandaging were performed in the emergency room. Six months after the scar had healed, he felt numbness and tingling in the dorsal surface of the right thumb and was diagnosed with traumatic neuroma. Traumatic neuroma resection and SBRN anastomosis were performed. Four months after this treatment, he felt numbness and tingling in the right dorsal surface of the thumb, with obvious tenderness in the operated area.
No data were available.
No data were available.
Tinel’s sign was found to be positive on percussion of the right wrist.
No data were available.
US revealed that the SBRN was adhered to the surrounding tissue.
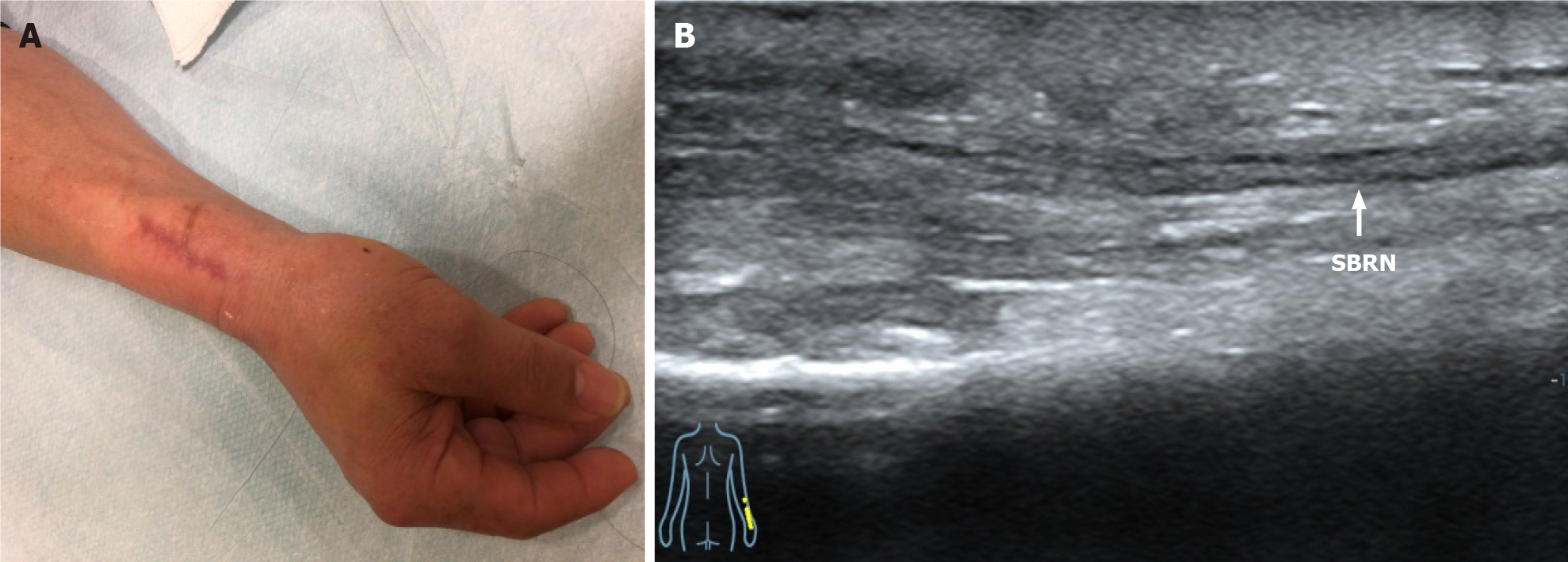
US indicated that the SBRN had adhered to the surrounding tissue after traumatic neuroma resection and SBRN anastomosis (Figure 1).
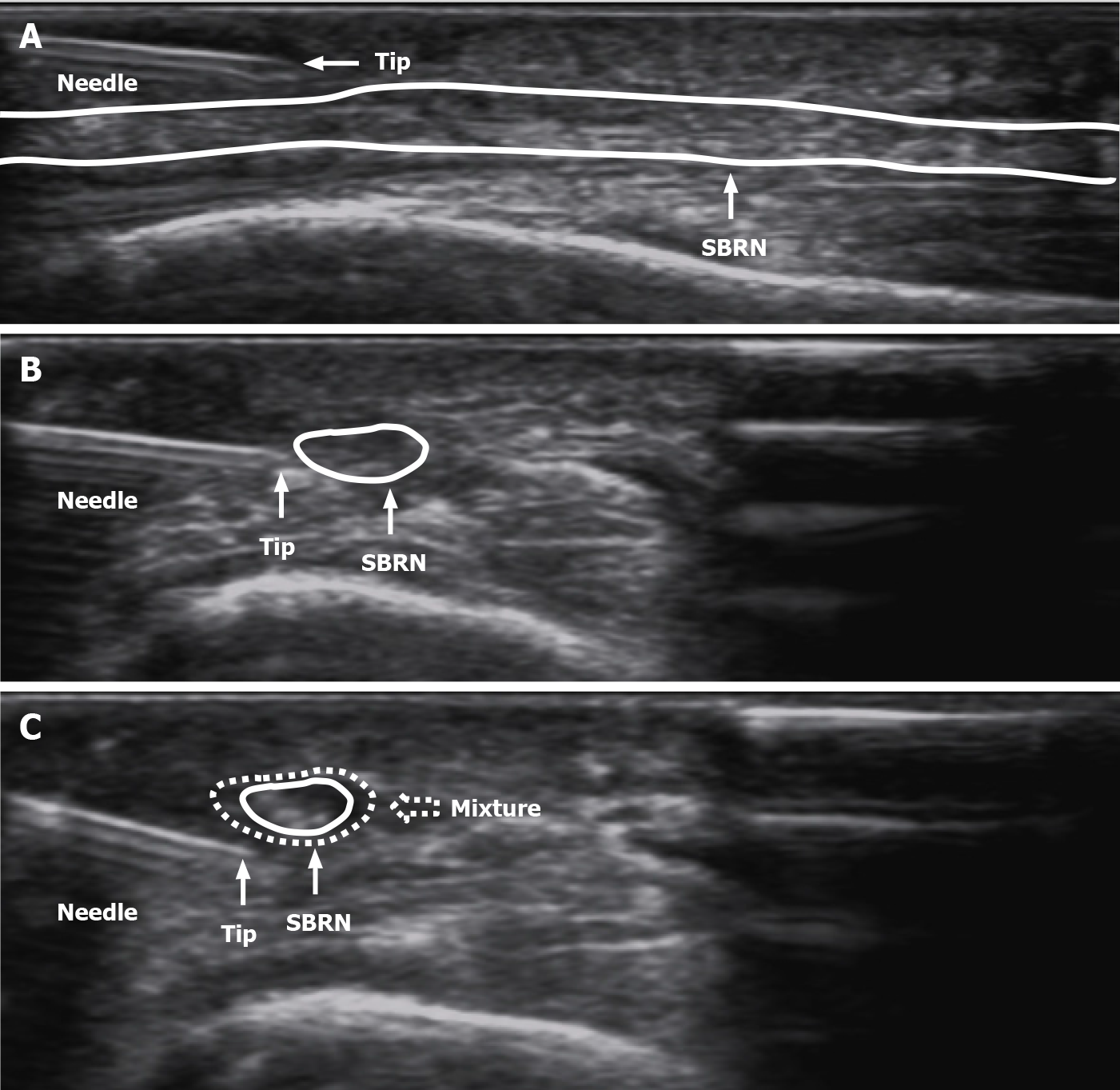
All treatment procedures were performed with the probe covered with surgical gloves. We used an acoustic coupling agent on the probe inside the surgical gloves (Figure 2). The patient’s skin was disinfected 3 times with complex iodine. A sterile surgical towel was then placed. A 4 mL aliquot of a mixed solution which contained 2 mL 0.9% sodium chloride and 2 mL 2% lidocaine (in a ratio of 1:1) was injected. Then local anesthesia layer by layer was performed via the SBRN surface.
The adhesion between the SBRN and the subcutaneous soft tissue was separated under US guidance. Due to the needle angle, we performed needle release to the middle incision (transverse incision level) as it was difficult to go further. Needle release was then performed from the incision distal area to the proximal area, above the level of the transverse incision. Separation of posterior and bilateral adhesions of the SBRN was carried out on both the short and long axis (transverse incision level). During needle release, the process was considered satisfactory when there was no resistance between the syringe and the tissues around the RN. Finally, a mixture of 1 mL corticosteroid (betamethasone) and 2 mL 2% lidocaine was injected into the area of severe adhesion on the short axis (Figure 3).
Four weeks later after ultrasound-guided needle release plus corticosteroid injection of superficial radial nerve, the tenderness in the surgical area was reduced by 70%, the numbness in the dorsal surface of the right thumb was reduced by 40% and the nerve swelling evaluated by US was reduced. Four months passed, he did not feel any numbness or tingling sensation of his right wrist.
Because of cost-effectiveness and non-invasive characteristics, US has gained popularity in diagnosing peripheral nerve diseases[4]. US can not only detect the nerve but can also reveal the location and the relationship to other structures[5]. In most studies, nerves in US images are always described as hypoechoic fascicles with surrounding hyperechoic tissue, appearing as a typical honeycomb structure[6]. The nerve is usually observed on US axial view from the proximal to distal area and is tracked along an extended length. Color Doppler is used to observe vessels which can serve as anatomical landmarks near the nerve. In US images, a muscle innervated by a nerve which is smaller and hyperechoic compared to the contralateral side indicates atrophy and thus may indicate an abnormal nerve.
The RNs are normal when they had a stippled honeycomb appearance with hypoechoic areas corresponding to the nerve fascicles and surrounding hyperechoic rims corresponding to endoneurium, perineurium, and epineurium on the short axis of US images[7]. The RN can be damaged during acute trauma by direct laceration or contusion, by traction in high-impact trauma with bone separation or by osseous fragments[2]. Humeral shaft fractures are the most common injuries to the RN[8,9]. The RN can also be compressed or stretched in patients who have undergone surgery. The SBRN can easily be affected by penetrating trauma especially the point which pierces the fascia due to its superficial characteristics. The symptoms include pain, dysesthesia and drop wrist. Conservative treatments include rest, nonsteroidal anti-inflammatory drugs (NSAIDs) and physical therapy. If symptoms persist 12 wk after conservative treatment, then surgery is strongly recommended[10].
In this case, we found that after traumatic neuroma resection and nerve anas
There are several lessons to be learned from this study. First, due to skin scar formation and subcutaneous soft tissue adhesion, local infiltration anesthesia is difficult to inject subcutaneously; therefore, preoperative local infiltration anesthesia combined with skin surface anesthesia can be used, thus making the patient feel less pain and more comfortable. Secondly, the puncture was carried out in the plane so that the needle tip could be observed during the whole process in order to avoid injury to the nerve. Thirdly, the SBRN is very superficial, thus probe compression can lead to deformation making it difficult to identify the nerve. Therefore, at puncture initiation, it should be noted that the insertion site should be superficial and should not allow pressure from the probe. Last, ultrasound-guided needle release has significant effect in many kinds of neural adhesion. We also tried other adhesive treatments for nerves, such as ultrasound-guided needle release of sciatic nerves and deep branches of the sciatic nerve. They all worked well.
Ultrasound is an effective method for evaluating the condition of the RN, as it can assess the RN and main terminal branches, observe any abnormalities and the relationship with surrounding tissues. Ultrasound-guided needle release plus corticosteroid injection is an effective and safe treatment for SBRN adhesion.
Provenance and peer review: Unsolicited manuscript; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Watanabe A S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Agarwal A, Chandra A, Jaipal U, Saini N. A panorama of radial nerve pathologies- an imaging diagnosis: a step ahead. Insights Imaging. 2018;9:1021-1034. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Bodner G, Buchberger W, Schocke M, Bale R, Huber B, Harpf C, Gassner E, Jaschke W. Radial nerve palsy associated with humeral shaft fracture: evaluation with US--initial experience. Radiology. 2001;219:811-816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 95] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 3. | Bianchi S. Ultrasound of the peripheral nerves. Joint Bone Spine. 2008;75:643-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 71] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 4. | Lawande AD, Warrier SS, Joshi MS. Role of ultrasound in evaluation of peripheral nerves. Indian J Radiol Imaging. 2014;24:254-258. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 58] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Foxall GL, Skinner D, Hardman JG, Bedforth NM. Ultrasound anatomy of the radial nerve in the distal upper arm. Reg Anesth Pain Med. 2007;32:217-220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Jacobson JA, Wilson TJ, Yang LJ. Sonography of Common Peripheral Nerve Disorders With Clinical Correlation. J Ultrasound Med. 2016;35:683-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 39] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 7. | Esparza M, Wild JR, Minnock C, Mohty KM, Truchan LM, Taljanovic MS. Ultrasound Evaluation of Radial Nerve Palsy Associated with Humeral Shaft Fractures to Guide Operative Versus Non-Operative Treatment. Acta Med Acad. 2019;48:183-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 8. | Pollock FH, Drake D, Bovill EG, Day L, Trafton PG. Treatment of radial neuropathy associated with fractures of the humerus. J Bone Joint Surg Am. 1981;63:239-243. [PubMed] |
| 9. | Bumbasirević M, Lesić A, Bumbasirević V, Cobeljić G, Milosević I, Atkinson HD. The management of humeral shaft fractures with associated radial nerve palsy: a review of 117 cases. Arch Orthop Trauma Surg. 2010;130:519-522. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 51] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 10. | Knutsen EJ, Calfee RP. Uncommon upper extremity compression neuropathies. Hand Clin. 2013;29:443-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |