Published online Dec 16, 2022. doi: 10.12998/wjcc.v10.i35.13081
Peer-review started: September 24, 2022
First decision: October 24, 2022
Revised: October 26, 2022
Accepted: November 14, 2022
Article in press: November 14, 2022
Published online: December 16, 2022
Processing time: 80 Days and 17.9 Hours
Hammered silver appearance of the corneal endothelium is considered a characteristic change in iridocorneal-endothelial syndrome. Herein we report an interesting case of hammered silver appearance of the corneal endothelium in Fuchs uveitis syndrome (FUS).
A 49-year-old man with progressive vision loss in the right eye for one year was admitted to our hospital. The clinical manifestations of the patient’s right eye were mild conjunctival hyperemia, scattered stellate keratic precipitates on the corneal endothelium, normal depth anterior chamber, 2+ cellular reaction in the aqueous humor, diffuse iris depigmentation, absence of synechia, Koeppe nodules, opalescent lens, and vitreous opacity. FUS and a complicated cataract were diagnosed based on the typical clinical manifestations. The corneal endothelial changes were recorded in detail by slit-lamp examination, specular microscopy, and in vivo confocal microscopy before cataract extraction, revealing a hammered silver appearance of the corneal endothelium in the affected eye, a wide-band dark area, as well as irregular corneal endothelial protuberances and dark bodies of various sizes. Subsequently, the patient underwent phacoemulsification combined with intraocular lens implantation, and his postoperative visual acuity recovered to 1.0.
Hammered silver appearance of the corneal endothelium in FUS, which is considered a more serious manifestation of endothelial damage, is rare and may be caused by many irregular protrusions in the corneal endothelium.
Core Tip: A 49-year-old man was diagnosed with Fuchs uveitis syndrome (FUS) and a complicated cataract based on typical clinical manifestations. Slit-lamp examination, specular microscopy, in vivo confocal microscopy revealed a hammered silver appearance of the corneal endothelium in the affected eye, a wide-band dark area, as well as irregular corneal endothelial protuberances and dark bodies of various sizes. Subsequently, the patient underwent phacoemulsification combined with intraocular lens implantation. Hammered silver appearance of the corneal endothelium in FUS, which is considered a more serious manifestation of endothelial damage, is rare and may be caused by many irregular protrusions in the corneal endothelium.
- Citation: Cheng YY, Wang CY, Zheng YF, Ren MY. Hammered silver appearance of the corneal endothelium in Fuchs uveitis syndrome: A case report. World J Clin Cases 2022; 10(35): 13081-13087
- URL: https://www.wjgnet.com/2307-8960/full/v10/i35/13081.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i35.13081
Fuchs uveitis syndrome (FUS) also referred to as Fuchs heterochromic uveitis or Fuchs heterochromic iridocyclitis, was first described by Ernst Fuchs in 1906. It is non-granulomatous uveitis primarily affecting a single eye, characterized by low-grade activity, diffuse depigmentation, and diffuse or central distribution of stellate keratic precipitates (KPs) on the corneal endothelium. Patients typically present in their third or fourth decades, and both sexes are equally affected[1,2]. Complicated cataracts, vitreous opacity, and secondary glaucoma are common complications[1], with cataract treatment leading to a good prognosis[3-5].
Inflammation of the anterior segment is known to affect the corneal endothelium[6]. In vivo confocal microscopy (IVCM) has also been used to characterize KPs and to evaluate endothelial cell layer damage in FUS, revealing that FUS is characterized by dendriform KPs and is associated with decreased endothelial cell density and altered endothelial cell morphology[7]. However, the appearance changes of the corneal endothelium on slit lamp examination are rarely described. Herein, we report an interesting case of hammered silver appearance of the corneal endothelium in FUS.
A 49-year-old man with progressive vision loss in the right eye for one year was admitted to our hospital.
The patient had been diagnosed with uveitis of the right eye three years previously and was treated with hormone eye drops and nonsteroidal anti-inflammatory eye drops in several hospitals.
The patient had no systemic diseases.
There was no remarkable family history.
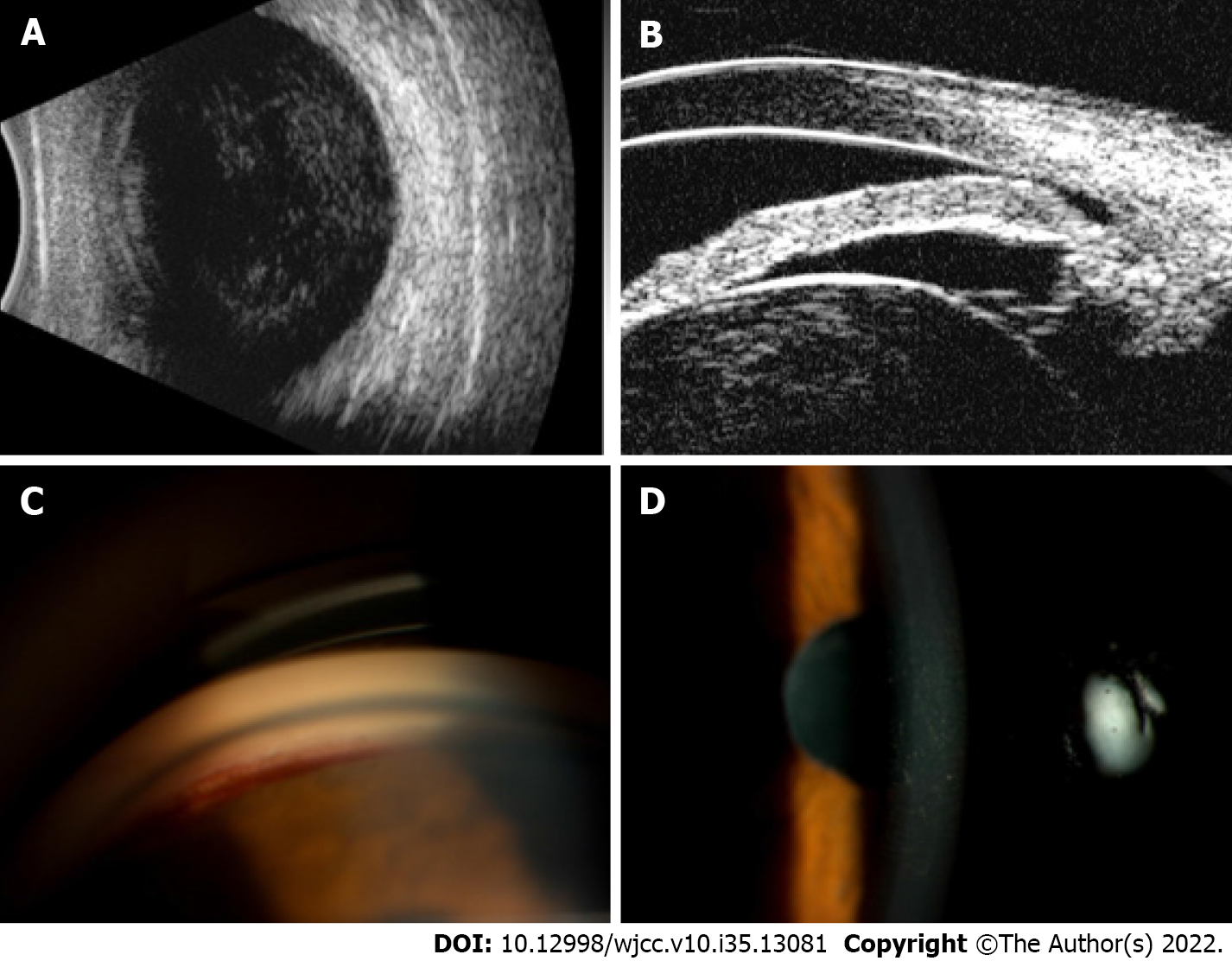
The visual acuity was counting fingers/40 cm in the right eye and 1.0 in the left eye. Intraocular pressure was 12 mmHg in the right eye and 14 mmHg in the left eye. The clinical manifestations of the patient’s right eye were mild conjunctival hyperemia, scattered stellate KPs on the corneal endothelium, normal depth anterior chamber, 2+ cellular reaction in the aqueous humor, diffuse iris depigmentation (Figure 1A), absence of synechia, Koeppe nodules (Figure 1B), opalescent lens, and vitreous opacity. No obvious abnormalities were observed in the anterior segment of the left eye (Figure 1C).
Laboratory tests were normal, including red and white blood cell counts, C-reactive protein, erythrocyte sedimentation rate, anti-streptolysin O titer, rheumatoid factor, and antinuclear antibody. Rubella immunoglobulin G (IgG) detected in the aqueous humor of the affected eye was 14.24 IU/mL, which was higher than the normal value.
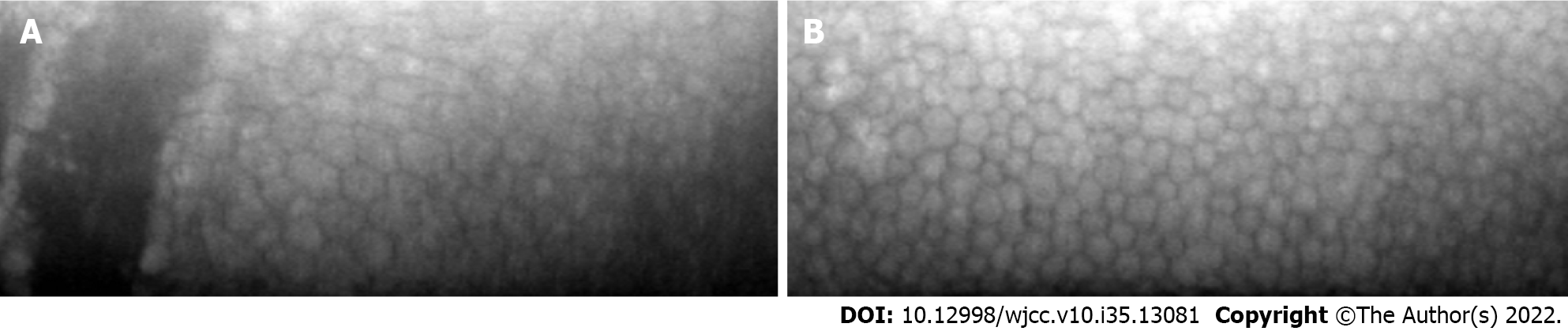
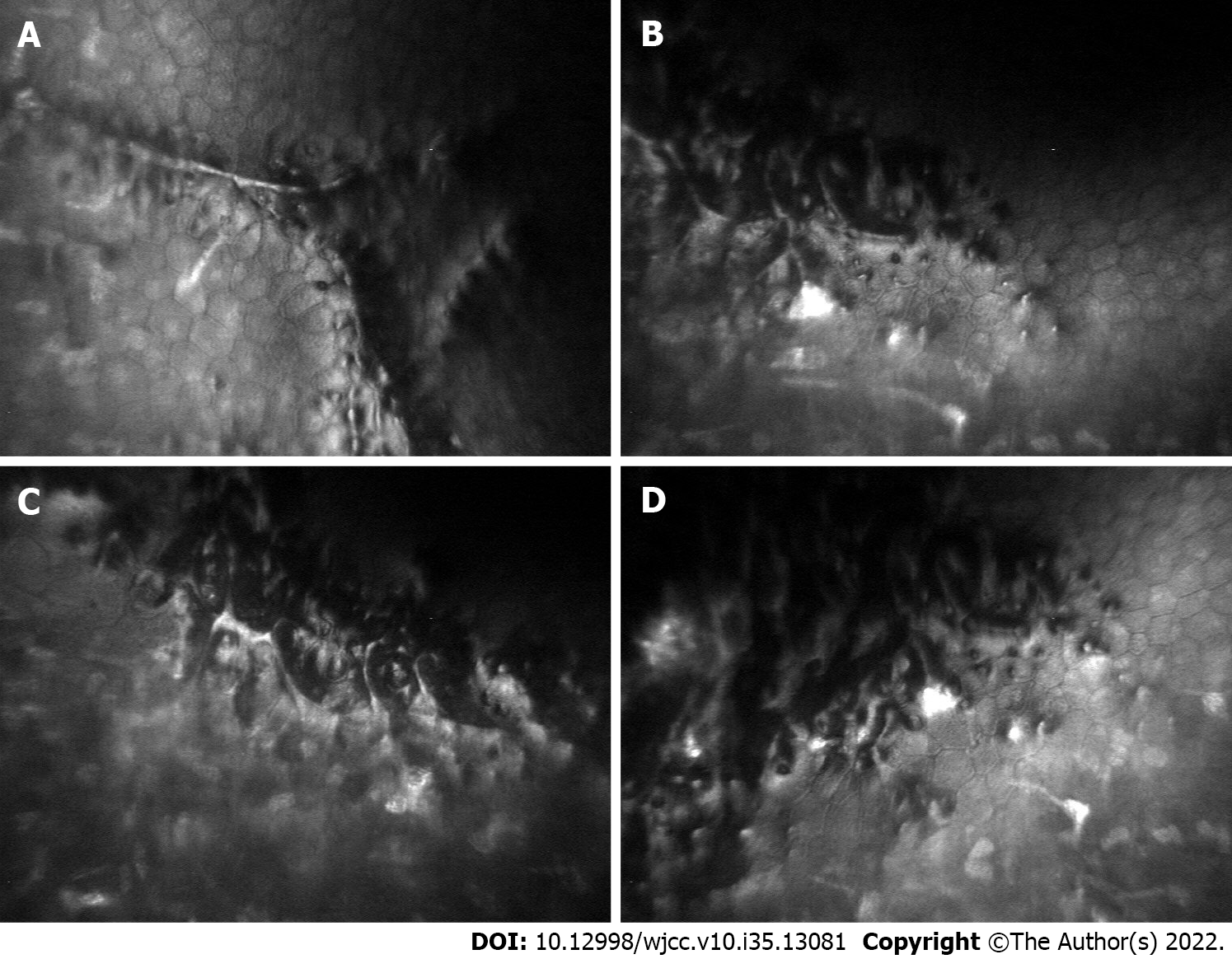
B-ultrasound revealed vitreous opacity in the affected right eye (Figure 2A). Ultrasound biomicroscopy showed a shallow anterior chamber, lens opacification, and expansion (Figure 2B). During gonioscopy, fresh bleeding was noted at the anterior chamber angle of the affected eye (Figure 2C). Slit-lamp examination revealed a hammered silver appearance of the central corneal endothelium in the affected eye (Figure 2D). Specular microscopy showed a wide-band dark area in the affected eye (Figure 3A), whereas the fellow eye showed a completely normal endothelial morphology (Figure 3B). The endothelial cell density of the affected eye was 2158 cells/mm2, and the coefficient of variation was 46%, whereas the endothelial cell density of the fellow eye was 2836 cells/mm2, and the coefficient of variation was 25%. IVCM revealed irregular corneal endothelial protuberances and dark bodies of various sizes in the affected eye (Figure 4). The corneal endothelial cells around the lesion were enlarged, and the corneal endothelium was evaluated before cataract extraction.
FUS and a complicated cataract were diagnosed based on the typical clinical manifestations.
During hospitalization, the anterior chamber quickly became shallow, with ultrasound biomicroscopy revealing opacity and expansion of the lens. Subsequently, phacoemulsification combined with intraocular lens implantation was performed in the right eye, and the postoperative visual acuity recovered to 1.0.
One year after cataract surgery, a telephone follow-up was conducted due to the pandemic of coronavirus disease 2019. The patient went to the ophthalmology department of a local hospital for further consultation. The visual acuity of his right eye was 0.8 and the intraocular pressure was normal.
The diagnosis of FUS is often based on clinical manifestations, and it is one of the frequently misdiagnosed forms of uveitis[8]. Yang et al[9] developed a novel set of revised diagnostic criteria for FUS with high sensitivity and specificity, confining the diagnosis to three essential criteria and five associated findings as support for the diagnosis, which are simpler and superior. In the present case, the clinical manifestations were in complete agreement with the diagnostic criteria for FUS.
Characteristic filiform hemorrhage and formation of hyphaema after anterior chamber paracentesis is a hallmark of FUS and is known as Amsler’s sign, which was first described by Amsler and Verrey[10] in 1946. Amsler’s sign can be spontaneous or associated with minor trauma, gonioscopy, applanation tonometry, pharmacological mydriasis, or cataract surgery[11]. The role of Amsler’s sign in diagnosing FUS is highly controversial, and paracentesis is unnecessary for patients with typical clinical manifestations[1]. Our patient showed Amsler’s sign during gonioscopy, which strongly supports the diagnosis of FUS, but no hemorrhage or other complications occurred during phacoemulsification.
The exact etiology of FUS remains unclear, but possible pathogenic mechanisms include sympathetic, immunological, hereditary, and infectious theories. Many of these theories have been largely disproven over the years, and rubella virus infection may be a possible etiological agent of FUS[12,13]. Metagenomic deep sequencing showed that persistent and active rubella virus infection is associated with FUS[14]. Treatment should be reserved for complications of FUS and not for inflammation associated with the disease[2]. In our case, the patient had not been vaccinated against rubella, and rubella IgG in the aqueous humor was increased, consistent with previous studies[15].
Alterations in corneal endothelial cells have been detected in patients with FUS, but there is no significant difference in endothelial cell density between the affected and healthy fellow eyes[16]. However, a decrease in endothelial cell density and percentage of endothelial hexagonal cells and an increase in polymegethism in FUS eyes compared to fellow eyes were detected in various studies[7,17]. Recent studies suggest that eyes with FUS have increased corneal densitometry values, especially in the posterior and midstromal layers of the cornea, which is considered to be due to impairment of endothelial cell function[18]. In our case, the endothelial cell density decreased, and the coefficient of variation increased compared with the contralateral eye.
In this case, we report a hammered silver appearance of the corneal endothelium in FUS. The hammered silver appearance of the corneal endothelium is common in iridocorneal-endothelial (ICE) syndrome and can also be seen with the corneal guttae present in primary endothelial dystrophy. Specular microscopy of ICE syndrome shows ICE cells with a typical dark-light reversal pattern[19], in this case, revealed a wide-band dark area of the affected eye, which does not support ICE diagnosis. Simultaneously, the contralateral eye of our patient was normal, ruling out the possibility of primary endothelial dystrophy. Recently, it has been reported that some patients with FUS have corneal guttae, but the authors did not describe whether they had a hammered silver appearance of the corneal endothelium[20]. At present, whether there are true corneal guttae in patients with FUS is controversial.
Labbé et al[16] observed hyperreflective deposits corresponding to KPs, smaller hyperreflective deposits, and hyporeflective small round defects in the affected eye of FUS using IVCM during a stable period. However, in our case, the inflammation had recently increased, the central corneal endothelium had a hammered silver appearance, and there were numerous irregular protrusions in the corneal endothelium, which may be the cause of the hammered silver appearance of the corneal endothelium, a more serious manifestation of the corneal endothelium damage. Potential damage to endothelial cells in patients with anterior uveitis includes direct contact with inflammatory cells or the role of proteins in the aqueous humor[6]. In this case, the corneal endothelial damage may be caused by active inflammation based on chronic inflammation.
This is a rare report of hammered silver appearance of corneal endothelium in FUS, possibly caused by many irregular protrusions in the corneal endothelium, which is considered a more serious manifestation of endothelial damage.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Vyshka G, Albania; Yang P, China S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
| 1. | Yang P, Fang W, Jin H, Li B, Chen X, Kijlstra A. Clinical features of Chinese patients with Fuchs' syndrome. Ophthalmology. 2006;113:473-480. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 57] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 2. | Rashid W, Lone I, Mir AM, Rashid A, Latif M. Fuchs Heterochromic Iridocylitis: Clinical Characteristics and Outcome of Cataract Extraction with Intra Ocular Lens Implantation in a Kashmiri Population- A Hospital Based Study. J Clin Diagn Res. 2016;10:NC13-NC16. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Nalçacıoğlu P, Çakar Özdal P, Şimşek M. Clinical Characteristics of Fuchs' Uveitis Syndrome. Turk J Ophthalmol. 2016;46:52-57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 4. | Mehta S, Linton MM, Kempen JH. Outcomes of cataract surgery in patients with uveitis: a systematic review and meta-analysis. Am J Ophthalmol. 2014;158:676-692.e7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 90] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 5. | Al-Mansour YS, Al-Rajhi AA, Al-Dhibi H, Abu El-Asrar AM. Clinical features and prognostic factors in Fuchs' uveitis. Int Ophthalmol. 2010;30:501-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 34] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Alfawaz AM, Holland GN, Yu F, Margolis MS, Giaconi JA, Aldave AJ. Corneal Endothelium in Patients with Anterior Uveitis. Ophthalmology. 2016;123:1637-1645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 68] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 7. | Mocan MC, Kadayifcilar S, Irkeç M. In vivo confocal microscopic evaluation of keratic precipitates and endothelial morphology in Fuchs' uveitis syndrome. Eye (Lond). 2012;26:119-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Sun Y, Ji Y. A literature review on Fuchs uveitis syndrome: An update. Surv Ophthalmol. 2020;65:133-143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 9. | Yang P, Zhang W, Chen Z, Zhang H, Su G, Cao Q, Zhu Y, Zhong Z, Zhou C, Wang Y, Kijlstra A. Development of revised diagnostic criteria for Fuchs' uveitis syndrome in a Chinese population. Br J Ophthalmol. 2021;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 10. | Amsler M, Verrey F. Fuchs heterochromia and vascular fragility. Ophthalmologica. 1946;111:177-181. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 33] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Srinivasan S, Lyall D, Kiire C. Amsler-Verrey sign during cataract surgery in Fuchs heterochromic uveitis. BMJ Case Rep. 2010;2010. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 12. | Suzuki J, Goto H, Komase K, Abo H, Fujii K, Otsuki N, Okamoto K. Rubella virus as a possible etiological agent of Fuchs heterochromic iridocyclitis. Graefes Arch Clin Exp Ophthalmol. 2010;248:1487-1491. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 49] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Ruokonen PC, Metzner S, Ucer A, Torun N, Hofmann J, Pleyer U. Intraocular antibody synthesis against rubella virus and other microorganisms in Fuchs' heterochromic cyclitis. Graefes Arch Clin Exp Ophthalmol. 2010;248:565-571. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 65] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 14. | Gonzales JA, Hinterwirth A, Shantha J, Wang K, Zhong L, Cummings SL, Qian Y, Wilson MR, Acharya NR, Doan T. Association of Ocular Inflammation and Rubella Virus Persistence. JAMA Ophthalmol. 2019;137:435-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 15. | Kang H, Bao H, Shi Y, Feng J, Yang W, He Y, Wang H, Hu X, Tao Y. Clinical Characteristics and Aqueous Humor Laboratory Analysis of Chinese Patients With Rubella Virus-Associated and Cytomegalovirus-Associated Fuchs Uveitis Syndrome. Front Med (Lausanne). 2020;7:610341. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Labbé A, Dupas B, Offret H, Baudouin C, Labetoulle M. Evaluation of keratic precipitates and corneal endothelium in Fuchs' heterochromic cyclitis by in vivo confocal microscopy. Br J Ophthalmol. 2009;93:673-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 29] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Szepessy Z, Tóth G, Barsi Á, Kránitz K, Nagy ZZ. Anterior Segment Characteristics of Fuchs Uveitis Syndrome. Ocul Immunol Inflamm. 2016;24:594-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Simsek M, Cakar Ozdal P, Cankurtaran M, Ozdemir HB, Elgin U. Analysis of Corneal Densitometry and Endothelial Cell Function in Fuchs Uveitis Syndrome. Eye Contact Lens. 2021;47:196-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 19. | Silva L, Najafi A, Suwan Y, Teekhasaenee C, Ritch R. The iridocorneal endothelial syndrome. Surv Ophthalmol. 2018;63:665-676. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 47] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 20. | Sravani NG, Mohamed A, Chaurasia S, Durgam SS, Murthy SI. Corneal endothelium in unilateral Fuchs heterochromic iridocyclitis. Indian J Ophthalmol. 2020;68:447-449. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |