Published online Dec 16, 2022. doi: 10.12998/wjcc.v10.i35.12812
Peer-review started: August 23, 2022
First decision: October 24, 2022
Revised: November 4, 2022
Accepted: November 28, 2022
Article in press: November 28, 2022
Published online: December 16, 2022
Processing time: 112 Days and 20.2 Hours
Minimally invasive adrenalectomy has become the main treatment modality for most adrenal lesions. Both laparoscopic transabdominal and retroperitoneoscopic approaches are safe and feasible options, each with respective advantages, including better surgical outcomes, fewer complications, and faster recovery over open adrenalectomy. While open surgery remains a valid modality in treatment of adrenocortical cancer in the presence of some findings such as invasion, robotic platforms, and minimally invasive surgery have gained popularity as technology continues to evolve. Organ preservation during adrenalectomy is feasible in some conditions to prevent adrenal insufficiency. Ablative technologies are increasingly utilized in benign and malignant tumors, including the adrenal gland, with various outcomes. A multidisciplinary team, an experienced surgeon, and a high-volume center are recommended for any surgical approaches and management of adrenal lesions. This review article evaluated recent findings and current evidence on minimally invasive adrenalectomy.
Core Tip: Minimally invasive adrenalectomy is the standard treatment for most adrenal lesions. Options to approach the adrenal gland include a transabdominal or retroperitoneoscopic route via laparoscopy or robotic platform. While each presents their own advantages, all are safe and produce excellent outcomes. Although open surgery for adrenocortical carcinoma remains suitable in some situations, partial adrenalectomy may be appropriate in certain cases to prevent adrenal insufficiency.
- Citation: Dogrul AB, Cennet O, Dincer AH. Minimally invasive techniques in benign and malignant adrenal tumors. World J Clin Cases 2022; 10(35): 12812-12821
- URL: https://www.wjgnet.com/2307-8960/full/v10/i35/12812.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i35.12812
Minimally invasive surgery has become the standard therapy for most adrenal neoplasms, widely accepted since the first laparoscopic adrenalectomy was reported by Wagner et al[1]. With its multilayered anatomy and localization, minimally invasive adrenalectomy offers several current surgical options. It can be performed through either a transabdominal or retroperitoneoscopic approach using laparoscopy or robot-assisted surgery. Each route and technique offers remarkable advantages and disadvantages (Table 1)[2].
| Therapeutic approach | Advantages | Disadvantages |
| Laparoscopic transabdominal approach | Familiarity for surgeons, larger working space, suitable for larger lesions | Repositioning for bilateral surgery, learning curve |
| Retroperitoneoscopic approach | Less pain and time, fewer adhesion-related problems | Inability to fully explore abdomen |
| Transabdominal robotic adrenalectomy | Improved vision, articulating instruments, and surgeon’s comfort | Cost, learning curve |
| Single-port adrenalectomy | Better cosmesis, less pain, faster recovery | Special instruments |
| Open adrenalectomy | Vascular/organ invasion, large malignant tumors | Postoperative pain, longer recovery, large wound with risk of infection |
| Ablative therapies | Better for poor surgical candidates | Hypertensive crisis, lack of evidence |
With the increasing use of diagnostic imaging modalities, adrenal masses are commonly encountered as so-called incidentalomas[3]. Its prevalence varies between 1% and 7% depending on the data source (autopsy vs radiology) and population (age, sex), being slightly more common in females[4-7]. While almost equal distribution of incidentalomas on the right and left sides has been reported, bilateral of nodules may present in up to 15% of cases[3,8].
In general, if the nodule is producing excess hormone (functional) or suspected of primary or secondary malignancy, surgery is indicated[9]. Almost all nodules - even malignant in some cases - can be treated with minimally invasive surgical techniques depending on the experience of the surgeon, facilities of the institution, and the patient’s and/or tumor’s characteristics. Adrenal-sparing surgery has gained popularity for preventing insufficiency in terms of long-term morbidity[10]. In rare situations, thermal ablation may give promising results[11].
This article reviews the findings and controversies of recent studies regarding the minimally invasive techniques for adrenal surgery.
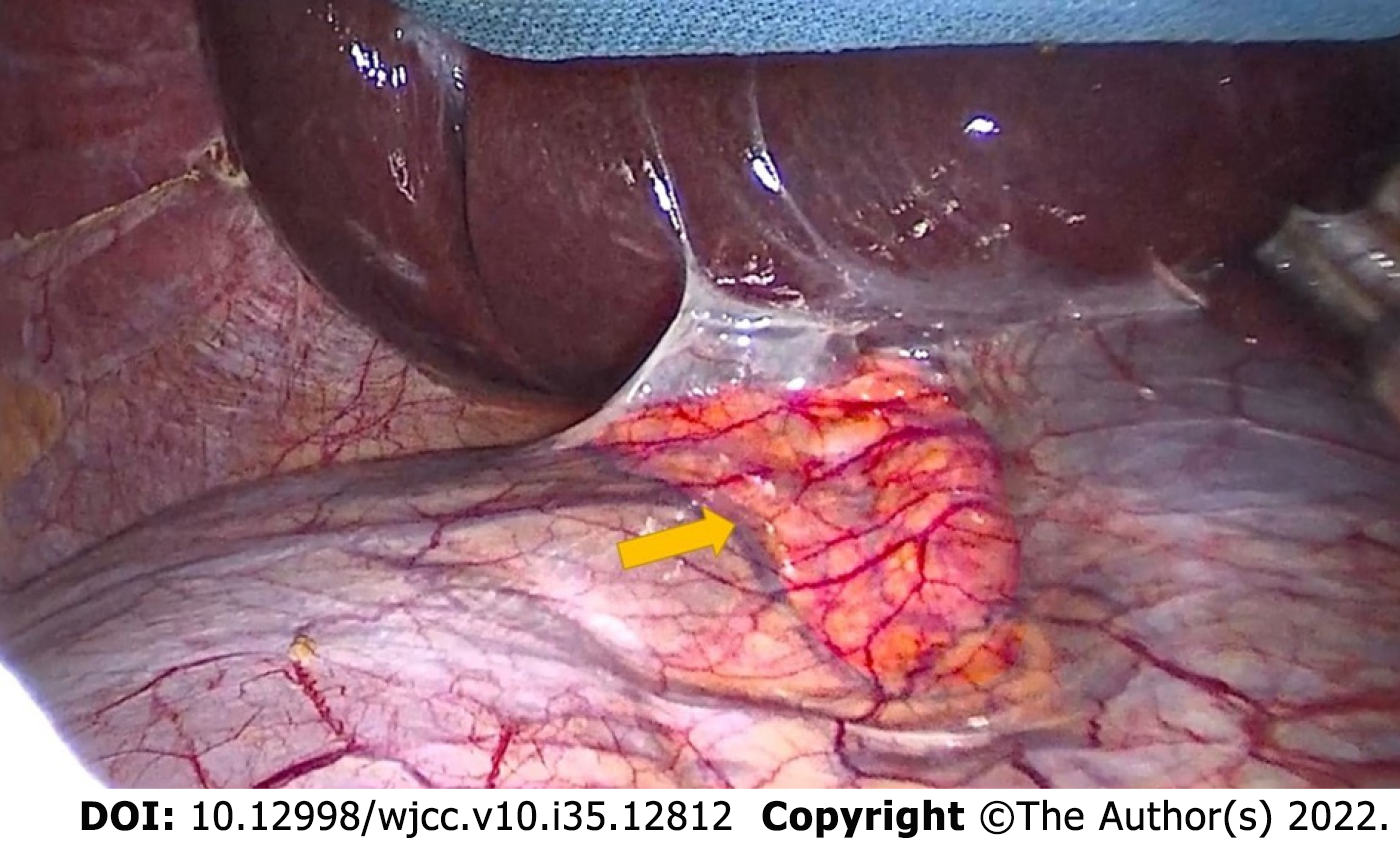
Since the first laparoscopic transabdominal adrenalectomy (LTA) was performed, multiple studies have been reported on experiences with and consequences of this technique[1,12-14]. As usage spread, LTA became the gold standard[15]. Many surgeons choose the transabdominal approach because it has a larger working space, and surgeons are familiar with the laparoscopic abdominal anatomy and landmarks (Figure 1)[16].
Laparoscopic transabdominal adrenalectomy can be performed in either the lateral decubitus or anterior position. The lateral position allows the gravity of organs for self-retraction, so it is widely used[2]. On the other hand, bilateral adrenalectomy requires repositioning the patient. As the right and left sides present distinct vascular anatomy, surgical techniques and complications differ respectively. Some studies have reported similar or higher complication rates on the left side due to the complexity of the anatomy[17,18]. However, a recent small-sized meta-analysis reported a higher risk of bleeding and conversion rate on the right side[19]. Port positions are similar for both left and right adrenalectomy. After access to the peritoneal cavity using either a Hassan or Veress needle technique nearly 2 cm inferior to the costal margin at the semicircular line, the other two working ports are placed substantially with the lateral one in the mid axillary line[20]. Generally, three trocars are used on the left side and an additional trocar is used for liver retraction on the right side.
The definitive indications or contraindications of LTA remain uncertain. Increasing experience and evolving technology have expanded the size criterion. Some authors reported giant adrenal masses (> 10 cm) resected laparoscopically, especially for rare, benign lesions such as myelolipoma[20-22]. Laparoscopic adrenalectomy is more advantageous via the transperitoneal route than the retroperitoneoscopic approach in terms of the larger operating field, but also requires advanced technical skills and expertise. Some parameters and scoring systems can predict the difficulty of laparoscopic adrenalectomy. For example, lesion size is related to longer operating times and higher conversion rates[23,24]. Most studies suggest that a suspicious or malignant adrenal mass smaller than 6 or 8 cm without invasion and suspected malignant lymph nodes can be managed microscopically without disturbing oncological safety. However, high-volume center is emphasized, and the surgeons’ experience is of paramount importance[25-27].
While obesity is considered a risk factor for complications in most surgeries, LTA is feasible for obese or morbidly obese patients[28]. This is because although obesity is associated with a longer operation time, it is not associated with morbidity or conversion in LTA[29,30]. Conversely, the retroperitoneal approach is adversely affected by obesity or periadrenal fat due to limited working space[31,32].
Concomitant surgery is sometimes needed. If the necessity of any other intraabdominal surgery arises, the transabdominal approach may be a viable option[33,34].
Minimally invasive adrenal surgery in children has been adopted in many centers[35,36]. The most common adrenal pathology is neuroblastomas in childhood. Due to the tendency of this tumor to adhere to vascular structures, a relatively small number of neuroblastomas patients are managed laparoscopically[37]. The transabdominal route is used most commonly in this subset of patients[38].
Posterior retroperitoneoscopic adrenalectomy (PRA) became widespread after it was first introduced to the surgical world[39]. This technique approaches the adrenal glands directly without entering the abdomen, and thus avoids dissection or mobilization of intraabdominal organs such as the liver and colon. It has distinctive features compared to the transperitoneal approach, including the prevention of complications that may occur during entry into the abdominal cavity (bowel injury, etc). Previous surgery-related adhesions are not problematic. In addition, both adrenal glands can be reached in the same position, as repositioning may prolong operation time. The patient is placed in a modified prone position for maximizing the distance between the costal margin and iliac crest. The first trocar is placed at the tip of the 12th rib. The other two trocars are inserted approximately 4 cm medial and lateral to the first middle trocar below the rib cage. Higher insufflation pressure (up to 25 mm Hg) is required to create working space when compared to the LTA approach. This pressure results in less blood loss, as it compresses small vessels. Nevertheless, rare but fatal air embolism complications associated with vena cava injury may be encountered during surgery[40]. Also, higher carbon dioxide insufflation causes some physiological changes such as acidosis and greater end-tidal values[41]. Accordingly, the anesth
Several studies compared the two approaches. Most have shown that PRA offers distinctive advantages over LTA, including less estimated blood loss, shorter time to oral food intake, less operative time, and a shorter hospital stay[42-44]. However, these lesser complications may be related to the smaller tumor size in the PRA group[44,45], and thus should be carefully evaluated in the light of additional data such as the experience of the surgeon and the center. Moreover, the learning curve is longer and another possible drawback of this approach[46]. Finally, capsular disruption, which is an important problem when operating for malignancy, may be higher in PRA[16]. Overall, both approaches are safe and have similar outcomes in experienced hands.
Robot-assisted surgery is currently used in all surgical disciplines, and considered the standard approach in some types of surgery. In adrenal surgery, robot-assisted adrenalectomies began to be reported in the early 2000s[47,48]. The general advantages of robotic systems include three-dimensional magnified image, stable and tremor-free image and intervention, articulated arms, and the comfort for the surgeon.
Although many studies have compared the robotic and laparoscopic approaches in adrenal surgery, none have demonstrated a clinically meaningful superiority of one over the other. One small-sized, randomized prospective trial that was previously published compared both methods, concluding that as the perioperative morbidity is higher in the robotic group, the laparoscopic approach is therefore superior to robot-assisted adrenalectomy[49]. However, increasing experience with robotic technology have improved perioperative outcomes. Recent studies and meta-analyses reveal that robotic adrenalectomy results in shorter hospital stays, less estimated blood loss, and similar postoperative complications compared to laparoscopic adrenalectomy[50-52]. Operative times differ between studies as the docking step may add extra operative time[53,54]. The robotic approach may offer an advantage for obese patients and larger and left-sided lesions[55-57]. A robotic platform may be advantageous when used in combination with indocyanine green in cases of partial adrenalectomy[58]. However, the studies are on a case-by-case basis, and there is no study comparing robotic and laparoscopic partial adrenalectomy.
Cost-effectiveness is an important drawback of robotic adrenalectomy, even in high-volume centers. The robotic approach doubles or triples the cost at $900 per case, although for subgroups where more benefits are expected for the robotic approach, such as larger and more difficult lesions, may reduce this cost[59,60]. In addition, a learning curve is needed in about 20 cases to achieve comparable results, even for the experienced laparoscopic surgeon[54]. Overall, robotic adrenalectomy is a safe and acceptable method compared to laparoscopic adrenalectomy in terms of postoperative outcomes.
Single-port (single incision, reduced port) surgery has been introduced in the last 20 years for numerous surgical types. In adrenal surgery, the first cases and series were published with different routes and instruments[61,62]. Single-port surgery aims to reduce incisions and pain and improve cosmetics. It is applicable via numerous instruments (articulating or straight) and port systems[63-65]. Even a handmade “glove port” can be used to reduce the cost[66,67].
Many studies have compared multiport and single-port adrenalectomy with different routes (retroperitoneal or transabdominal) on different platforms (robotic or laparoscopic). There are five meta-analyses for laparoscopic single port vs multiport adrenalectomy[68-72]. Laparoscopic single-port adrenalectomy is better in postoperative pain, hospitalization days, and recovery, but requires longer operative time. However, most of the included studies are retrospective, small-sized, and heterogeneous in terms of the route (transabdominal-retroperitoneal) and the devices[72]. Robotic single-incision adrenalectomy may overcome the disadvantages of laparoscopy through articulation of the instruments and surgeons’ comfort. Retrospective studies reveal robotic single-port adrenalectomy as a safe and potentially feasible alternative to the multiport approach, but cost-effectiveness and risk of incisional hernia remain a matter of debate[73-75].
The philosophy behind preserving endocrine organs comes from the prevention of lifelong hormone replacement therapy. For instance, thyroid lobectomy is an established option to avoid lifelong levothyroxine replacement therapy, which is related to lower quality of life[76]. Similarly, preserving healthy adrenal tissue especially for bilateral conditions may avoid steroid dependence. Partial adrenalectomy (sometimes called cortical sparing adrenalectomy) is more difficult and needs meticulous dissection. In technical aspects, it is crucial to understand the anatomy and landmarks of the nodule in preoperative imaging and vascular supply of remnant tissue. Recently, indocyanine green has been used intraoperatively to check the remnant gland’s vascularity[77]. During partial adrenalectomy, intraoperative bleeding and blood loss may be higher than in total adrenalectomy, as it is a highly vascular gland[78,79]. Even so, partial adrenalectomy is safe and offers similar or better postoperative surgical outcomes, including shorter hospital stay and operative time when compared to total adrenalectomy[80,81].
After partial adrenalectomy for hormonally active lesions, the requirement of hormone supplementation and recurrence also must be considered. Although studies are heterogeneous, most of the patients remain steroid-independent after partial adrenalectomy[82-85]. However, bilateral disease and resection may decrease this success. In most series, tumor recurrence due to hereditary conditions or multinodularity is low (< 10%) or acceptable when compared to total adrenalectomy[86,87].
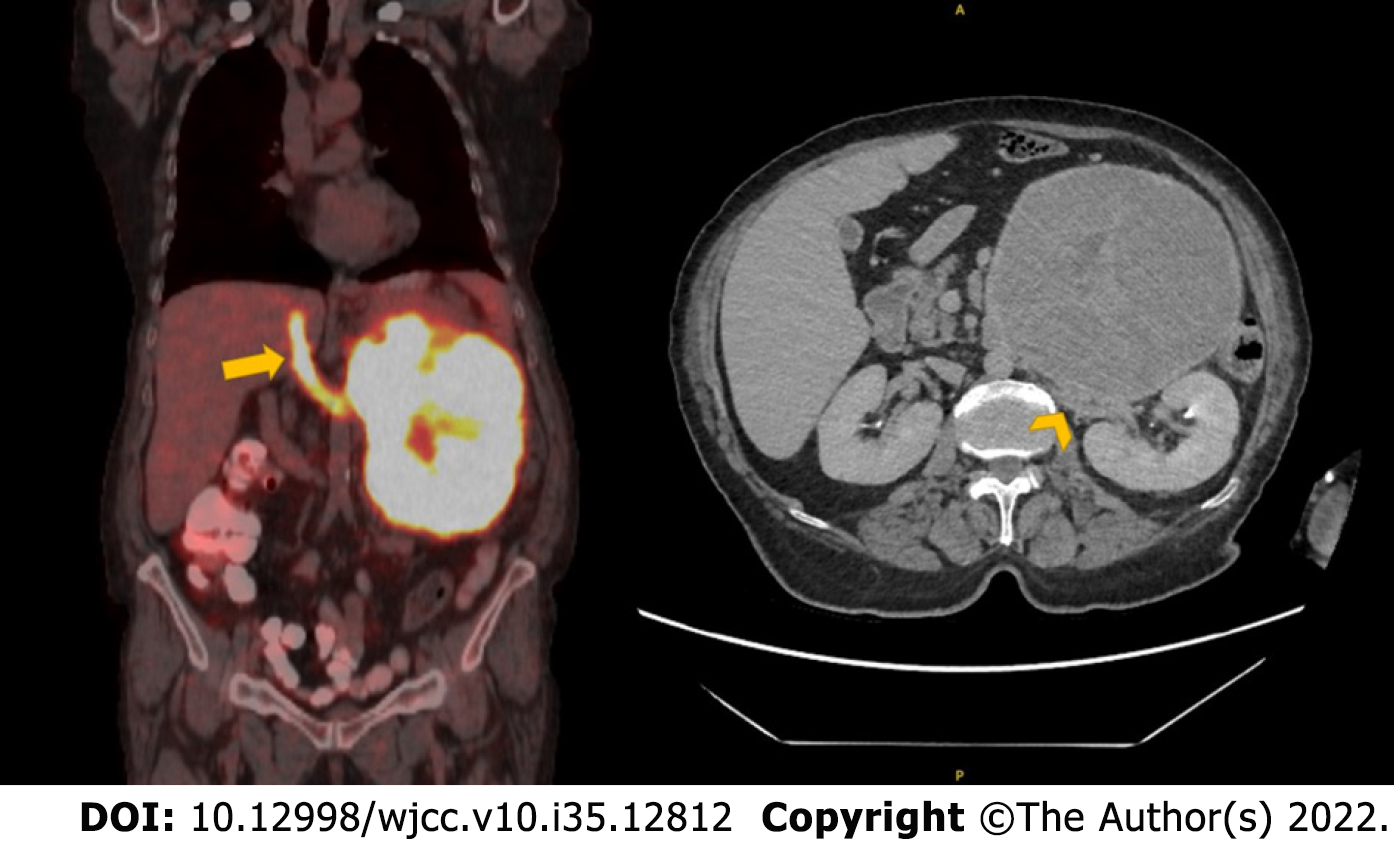
Although minimally invasive adrenalectomy is the first choice in many cases, open surgery plays an important role in malignant adrenal tumors such as adrenocortical carcinoma (ACC). General surgical principles for localized ACC are en bloc resection (including invaded structure or organ) together with locoregional (periadrenal, renal hilum) lymphadenectomy[88]. ACC may invade the kidney, liver, pancreas, or spleen, and tumor thrombus or vena cava extension may also occur, which are conditions that mandate open surgery (Figure 2)[89]. Preoperative evaluation and imaging for the presence of these findings are crucial. Intraoperative tumor rupture/spillage and violation of the capsule are associated with poorer survival[26].
No randomized studies have compared the two methods. A laparoscopic approach without evidence of invasion should be performed by only an experienced surgeon. The described oncological principles must be followed during laparoscopy. Most endocrine and endocrine surgery societies accept a cutoff of 6 cm for size criterion[25,88]. A retrospective study comparing open and laparoscopic adrenalectomy for < 10 cm ACC revealed similar oncological outcomes but a higher peritoneal recurrence in the laparoscopy group than in open adrenalectomy[90]. In choosing laparoscopy, the transabdominal approach is recommended, as there is more experience with this approach. In addition, this route is more suitable for intra-abdominal exploration in terms of metastasis, invasion, and carcinomatosis[25]. The role of the robotic approach for ACC remains unclear. A recently published article comparing robotic and laparoscopic adrenalectomy for malignancy found higher conversion rates tied to poorer survival in the laparoscopy group. However, this dataset lacks detail about the reason for conversion and data for the rupture of tumor capsule[91]. More comparative studies are needed for this situation.
For adrenal metastatic diseases, a minimally invasive approach may be preferred. There is no difference in local recurrence and margin status between the laparoscopic and open approaches. However, tumor size and radiological evaluation for the invasion are of paramount importance in this group[92].
Adrenal gland tumors are typically operated/resected using the techniques outlined above. Ablative technologies such as radiofrequency ablation, microwave ablation, cryoablation, and laser ablation are currently in use for many tumors, including liver, lung, bone, or kidney[93-95]. Its use in endocrine tumors such as benign or malignant thyroid tumors is increasingly discussed in the literature[96].
Supporting literature draws on small series or cases of adrenal tumors. For functional adenomas (aldosterone or cortisol producing, pheochromocytoma), short-term outcomes and biochemical cure rates are satisfactory[97,98]. Planned future studies may address questions on this issue[99]. Additi
Adrenal metastases are ablated more rarely than functional adenomas. Outcomes depend on the primary tumors’ characteristics and size. The effect on survival is unknown because of the heterogenity of primary malignancies[11]. Adrenocortical carcinoma can be managed with ablative options in addition to surgery for advanced cases[25,88]. In general, adrenal ablation may be an alternative for poor candidates for adrenalectomy[101,102].
Minimally invasive adrenalectomy is well established and effective for most adrenal lesions. It may be performed via transabdominal or retroperitoneal route using laparoscopy or a robotic platform. Each approach has its pros and cons. The most preferred method is laparoscopic transabdominal adrenalectomy, as it is familiar to most surgeons. The cost is the leading disadvantage of robotic surgery. Malignant adrenal tumors that are greater in size and invade adjacent structures warrant open surgery. Whichever approach is used, the contribution of an experienced endocrine surgeon is indisputable. Partial adrenalectomy may be a suitable option in some conditions such as hereditary or bilateral diseases. Ablative therapies are still in their infancy and further studies are needed.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: Turkish Society of Surgery; Turkish Society of Hepatopancreatobiliary Surgery.
Specialty type: Medicine, research and experimental
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): C, C, C
Grade D (Fair): D, D
Grade E (Poor): 0
P-Reviewer: Boopathy Vijayaraghavan KM, India; Chisthi MM, India; Fakhradiyev I, Kazakhstan; Giordano A, Italy; Navarrete Arellano M, Mexico S-Editor: Wang LL L-Editor: Filipodia P-Editor: Wang LL
| 1. | Gagner M, Lacroix A, Prinz RA, Bolté E, Albala D, Potvin C, Hamet P, Kuchel O, Quérin S, Pomp A. Early experience with laparoscopic approach for adrenalectomy. Surgery. 1993;114:1120-1124; discussion 1124. [PubMed] |
| 2. | Madani A, Lee JA. Surgical Approaches to the Adrenal Gland. Surg Clin North Am. 2019;99:773-791. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Sherlock M, Scarsbrook A, Abbas A, Fraser S, Limumpornpetch P, Dineen R, Stewart PM. Adrenal Incidentaloma. Endocr Rev. 2020;41:775-820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 139] [Cited by in RCA: 181] [Article Influence: 36.2] [Reference Citation Analysis (0)] |
| 4. | Song JH, Chaudhry FS, Mayo-Smith WW. The incidental adrenal mass on CT: prevalence of adrenal disease in 1,049 consecutive adrenal masses in patients with no known malignancy. AJR Am J Roentgenol. 2008;190:1163-1168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 370] [Cited by in RCA: 386] [Article Influence: 22.7] [Reference Citation Analysis (0)] |
| 5. | Davenport C, Liew A, Doherty B, Win HH, Misran H, Hanna S, Kealy D, Al-Nooh F, Agha A, Thompson CJ, Lee M, Smith D. The prevalence of adrenal incidentaloma in routine clinical practice. Endocrine. 2011;40:80-83. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 55] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 6. | Sington JD, Syn WK, Suvarna SK, Rassl DM, Jenkins RC, Weetman AP, Ross RJ. Lack of association between thyroid and adrenal nodules: a histological study. J Endocrinol Invest. 1999;22:262-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 7. | Alesina PF, Walz MK. Adrenal Tumors: Are Gender Aspects Relevant? Visc Med. 2020;36:15-19. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Terzolo M, Stigliano A, Chiodini I, Loli P, Furlani L, Arnaldi G, Reimondo G, Pia A, Toscano V, Zini M, Borretta G, Papini E, Garofalo P, Allolio B, Dupas B, Mantero F, Tabarin A; Italian Association of Clinical Endocrinologists. AME position statement on adrenal incidentaloma. Eur J Endocrinol. 2011;164:851-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 347] [Cited by in RCA: 327] [Article Influence: 23.4] [Reference Citation Analysis (0)] |
| 9. | Hadjikyriacou E, Egan R. Adrenal incidentalomas. Br J Surg. 2022;109:647-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Perysinakis I, Aggeli C, Kaltsas G, Zografos GN. Adrenal-sparing surgery: current concepts on a theme from the past. Hormones (Athens). 2020;19:317-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 11. | Donlon P, Dennedy MC. Thermal ablation in adrenal disorders: a discussion of the technology, the clinical evidence and the future. Curr Opin Endocrinol Diabetes Obes. 2021;28:291-302. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Higashihara E, Tanaka Y, Horie S, Aruga S, Nutahara K, Homma Y, Minowada S, Aso Y. [A case report of laparoscopic adrenalectomy]. Nihon Hinyokika Gakkai Zasshi. 1992;83:1130-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 44] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Suzuki K, Kageyama S, Ueda D, Ushiyama T, Kawabe K, Tajima A, Aso Y. Laparoscopic adrenalectomy: clinical experience with 12 cases. J Urol. 1993;150:1099-1102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 115] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 14. | Terachi T, Matsuda T, Terai A, Ogawa O, Kakehi Y, Kawakita M, Shichiri Y, Mikami O, Takeuchi H, Okada Y, Yoshida O. Transperitoneal laparoscopic adrenalectomy: experience in 100 patients. J Endourol. 1997;11:361-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 97] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Smith CD, Weber CJ, Amerson JR. Laparoscopic adrenalectomy: new gold standard. World J Surg. 1999;23:389-396. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 252] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 16. | Marrero AP, Kazaure HS, Thomas SM, Stang MT, Scheri RP. Patient selection and outcomes of laparoscopic transabdominal versus posterior retroperitoneal adrenalectomy among surgeons in the Collaborative Endocrine Surgery Quality Improvement Program (CESQIP). Surgery. 2020;167:250-256. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 17. | Chiang PH, Yu CJ, Lee WC, Wang HJ. Is right-sided laparoscopic adrenalectomy truly more challenging than left-sided? Urolog Sci. 2013;117. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 18. | Rieder JM, Nisbet AA, Wuerstle MC, Tran VQ, Kwon EO, Chien GW. Differences in left and right laparoscopic adrenalectomy. JSLS. 2010;14:369-373. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Wang Y, Yang Z, Chang X, Li J, Zhang Y, Teng Z, Han Z. Right laparoscopic adrenalectomy vs left laparoscopic adrenalectomy: a systematic review and meta-analysis. Wideochir Inne Tech Maloinwazyjne. 2022;17:9-19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 20. | Uberoi J, Munver R. Surgical management of metastases to the adrenal gland: open, laparoscopic, and ablative approaches. Curr Urol Rep. 2009;10:67-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 34] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 21. | Tinozzi FP, Morone G, Calì B, Rebba A, Osman N, Albertario S, Abbiati F, Ruggiero R. Laparoscopic adrenalectomy for a giant adrenal myelolipoma: A case report. Int J Surg Case Rep. 2022;90:106678. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 22. | Al Harthi B, Riaz MM, Al Khalaf AH, Al Zoum M, Al Shakweer W. Adrenal myelolipoma a rare benign tumour managed laparoscopically: Report of two cases. J Minim Access Surg. 2009;5:118-120. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 23. | Chaudhary R, Deshmukh A, Singh K, Biswas R. Is size really a contraindication for laparoscopic resection of giant adrenal myelolipomas? BMJ Case Rep. 2016;2016. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 24. | Alberici L, Paganini AM, Ricci C, Balla A, Ballarini Z, Ortenzi M, Casole G, Quaresima S, Di Dalmazi G, Ursi P, Alfano MS, Selva S, Casadei R, Ingaldi C, Lezoche G, Guerrieri M, Minni F, Tiberio GAM. Development and validation of a preoperative “difficulty score” for laparoscopic transabdominal adrenalectomy: a multicenter retrospective study. Surg Endosc. 2022;36:3549-3557. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 25. | Natkaniec M, Dworak J, Pędziwiatr M, Pisarska M, Major P, Dembiński M, Winiarski M, Budzyński A. Patients criteria determining difficulty of the laparoscopic lateral transperitoneal adrenalectomy. A retrospective cohort study. Int J Surg. 2017;43:33-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Gaujoux S, Mihai R; joint working group of ESES and ENSAT. European Society of Endocrine Surgeons (ESES) and European Network for the Study of Adrenal Tumours (ENSAT) recommendations for the surgical management of adrenocortical carcinoma. Br J Surg. 2017;104:358-376. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 133] [Article Influence: 16.6] [Reference Citation Analysis (0)] |
| 27. | Henry JF, Peix JL, Kraimps JL. Positional statement of the European Society of Endocrine Surgeons (ESES) on malignant adrenal tumors. Langenbecks Arch Surg. 2012;397:145-146. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 28. | Fassnacht M, Arlt W, Bancos I, Dralle H, Newell-Price J, Sahdev A, Tabarin A, Terzolo M, Tsagarakis S, Dekkers OM. Management of adrenal incidentalomas: European Society of Endocrinology Clinical Practice Guideline in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2016;175:G1-G34. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1045] [Cited by in RCA: 1016] [Article Influence: 112.9] [Reference Citation Analysis (0)] |
| 29. | Danwang C, Agbor VN, Bigna JJ. Obesity and postoperative outcomes of the patients with laparoscopic adrenalectomy: a systematic review and meta-analysis. BMC Surg. 2020;20:194. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 30. | Rodríguez-Hermosa JI, Planellas-Giné P, Cornejo L, Gironès J, Recasens M, Ortega FJ, Moreno-Navarrete JM, Latorre J, Fernandez-Real JM, Codina-Cazador A. Comparison of Outcomes between Obese and Nonobese Patients in Laparoscopic Adrenalectomy: A Cohort Study. Dig Surg. 2021;38:237-246. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 31. | Pędziwiatr M, Major P, Pisarska M, Natkaniec M, Godlewska M, Przęczek K, Dworak J, Dembiński M, Zub‐Pokrowiecka A, Budzyński A. Laparoscopic transperitoneal adrenalectomy in morbidly obese patients is not associated with worse short‐term outcomes. Int J Urol. 2017;24:59-63. [RCA] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 16] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 32. | Pearlstein SS, Kuo JH, Chabot JA, Lee JA. Periadrenal Volume is a Better Predictor of Prolonged Operative Time in Laparoscopic Retroperitoneal Adrenalectomy than BMI. World J Surg. 2020;44:578-584. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 33. | Zonča P, Bužga M, Ihnát P, Martínek L. Retroperitoneoscopic Adrenalectomy in Obese Patients: Is It Suitable? Obes Surg. 2015;25:1203-1208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 24] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 34. | Alqahtani A, Almayouf M, Billa S, Helmi H. Laparoscopic sleeve gastrectomy with adrenalectomy, feasibility, safety and outcome. J Surg Case Rep. 2022;2022:rjac130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 35. | Corallino D, Meoli F, Palmieri L, Puliani G, Isidori A, Paganini AM. One-stage laparoscopic bilateral adrenalectomy, cholecystectomy and choledochotomy by a transperitoneal anterior approach Case report of a combined management for a challenging condition. Ann Ital Chir. 2020;91:314-320. [PubMed] |
| 36. | Fascetti-Leon F, Scotton G, Pio L, Beltrà R, Caione P, Esposito C, Mattioli G, Saxena AK, Sarnacki S, Gamba P. Minimally invasive resection of adrenal masses in infants and children: results of a European multi-center survey. Surg Endosc. 2017;31:4505-4512. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 37. | St Peter SD, Valusek PA, Hill S, Wulkan ML, Shah SS, Martinez Ferro M, Bignon H, Laje P, Mattei PA, Graziano KD, Muensterer OJ, Pontarelli EM, Nguyen NX, Kane TD, Qureshi FG, Calkins CM, Leys CM, Baerg JE, Holcomb GW. Laparoscopic adrenalectomy in children: a multicenter experience. J Laparoendosc Adv Surg Tech A. 2011;21:647-649. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 38. | de Campos Vieira Abib S, Chui CH, Cox S, Abdelhafeez AH, Fernandez-Pineda I, Elgendy A, Karpelowsky J, Lobos P, Wijnen M, Fuchs J, Hayes A, Gerstle JT. International Society of Paediatric Surgical Oncology (IPSO) Surgical Practice Guidelines. Ecancermedicalscience. 2022;16:1356. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 39. | Yankovic F, Undre S, Mushtaq I. Surgical technique: Retroperitoneoscopic approach for adrenal masses in children. J Pediatr Urol. 2014;10:400.e1-400.e2. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Reference Citation Analysis (0)] |
| 40. | Walz MK, Peitgen K, Hoermann R, Giebler RM, Mann K, Eigler FW. Posterior retroperitoneoscopy as a new minimally invasive approach for adrenalectomy: results of 30 adrenalectomies in 27 patients. World J Surg. 1996;20:769-774. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 193] [Cited by in RCA: 172] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 41. | Alexeev M, Fedorov E, Kuleshov O, Rebrova D, Efremov S. Carbon dioxide embolism during posterior retroperitoneal adrenalectomy. Anaesth Rep. 2022;10:e12164. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 42. | Fraser S, Norlén O, Bender K, Davidson J, Bajenov S, Fahey D, Li S, Sidhu S, Sywak M. Randomized trial of low versus high carbon dioxide insufflation pressures in posterior retroperitoneoscopic adrenalectomy. Surgery. 2018;163:1128-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 43. | Barczyński M, Konturek A, Nowak W. Randomized clinical trial of posterior retroperitoneoscopic adrenalectomy versus lateral transperitoneal laparoscopic adrenalectomy with a 5-year follow-up. Ann Surg. 2014;260:740-7; discussion 747. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 86] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 44. | Alberici L, Ingaldi C, Ricci C, Selva S, Di Dalmazi G, Vicennati V, Pagotto U, Casadei R, Minni F. Minimally invasive adrenalectomy: a comprehensive systematic review and network meta-analysis of phase II/III randomized clinical controlled trials. Langenbecks Arch Surg. 2022;407:285-296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 45. | Gavriilidis P, Camenzuli C, Paspala A, Di Marco AN, Palazzo FF. Posterior Retroperitoneoscopic Versus Laparoscopic Transperitoneal Adrenalectomy: A Systematic Review by an Updated Meta-Analysis. World J Surg. 2021;45:168-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 46. | Arezzo A, Bullano A, Cochetti G, Cirocchi R, Randolph J, Mearini E, Evangelista A, Ciccone G, Bonjer HJ, Morino M. Transperitoneal vs retroperitoneal laparoscopic adrenalectomy for adrenal tumours in adults. Cochrane Database Syst Rev. 2018;12:CD011668. [RCA] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 47. | Vrielink OM, Engelsman AF, Hemmer PHJ, de Vries J, Vorselaars WMCM, Vriens MR, Karakatsanis A, Hellman P, Sywak MS, van Leeuwen BL, El Moumni M, Kruijff S. Multicentre study evaluating the surgical learning curve for posterior retroperitoneoscopic adrenalectomy. Br J Surg. 2018;105:544-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 48. | Desai MM, Gill IS, Kaouk JH, Matin SF, Sung GT, Bravo EL. Robotic-assisted laparoscopic adrenalectomy. Urology. 2002;60:1104-1107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 69] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 49. | Piazza L, Caragliano P, Scardilli M, Sgroi AV, Marino G, Giannone G. Laparoscopic robot-assisted right adrenalectomy and left ovariectomy (case reports). Chir Ital. 1999;51:465-466. [PubMed] |
| 50. | Morino M, Benincà G, Giraudo G, Del Genio GM, Rebecchi F, Garrone C. Robot-assisted vs laparoscopic adrenalectomy: a prospective randomized controlled trial. Surg Endosc. 2004;18:1742-1746. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 133] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 51. | Du L, Yang Z, Qi J, Wang Y. Robotic adrenalectomy versus laparoscopic adrenalectomy for pheochromocytoma: a systematic review and meta-analysis. Wideochir Inne Tech Maloinwazyjne. 2022;17:1-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 52. | Xia Z, Li J, Peng L, Yang X, Xu Y, Li X, Li Y, Zhang Z, Wu J. Comparison of Perioperative Outcomes of Robotic-Assisted vs Laparoscopic Adrenalectomy for Pheochromocytoma: A Meta-Analysis. Front Oncol. 2021;11:724287. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 53. | Ma W, Mao Y, Zhuo R, Dai J, Fang C, Wang C, Zhao J, He W, Zhu Y, Xu D, Sun F. Surgical outcomes of a randomized controlled trial compared robotic versus laparoscopic adrenalectomy for pheochromocytoma. Eur J Surg Oncol. 2020;46:1843-1847. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 54. | Economopoulos KP, Mylonas KS, Stamou AA, Theocharidis V, Sergentanis TN, Psaltopoulou T, Richards ML. Laparoscopic vs robotic adrenalectomy: A comprehensive meta-analysis. Int J Surg. 2017;38:95-104. [RCA] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 77] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 55. | Materazzi G, Rossi L. Robot-assisted adrenalectomy: state of the art. Updates Surg. 2021;73:1131-1146. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 56. | Gan L, Meng C, Li K, Lei Peng, Li J, Wu J, Li Y. Safety and effectiveness of minimally invasive adrenalectomy vs open adrenalectomy in patients with large adrenal tumors (≥ 5 cm): A meta-analysis and systematic review. Int J Surg. 2022;104:106779. [RCA] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 57. | Piccoli M, Pecchini F, Serra F, Nigro C, Colli G, Gozzo D, Zirilli L, Madeo B, Rochira V, Mullineris B. Robotic Versus Laparoscopic Adrenalectomy: Pluriannual Experience in a High-Volume Center Evaluating Indications and Results. J Laparoendosc Adv Surg Tech A. 2021;31:375-381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 58. | Shalaby H, Abdelgawad M, Omar Md M, Zora Md G, Alawwad S, Alameer E, Youssef M, Attia AS, Buell J, Grace L, Kandil E. Robotic and Laparoscopic Approaches for Adrenal Surgery in Obese Patients. Am Surg. 2021;87:588-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 59. | Manny TB, Pompeo AS, Hemal AK. Robotic partial adrenalectomy using indocyanine green dye with near-infrared imaging: the initial clinical experience. Urology. 2013;82:738-742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 64] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 60. | Aliyev S, Karabulut K, Agcaoglu O, Wolf K, Mitchell J, Siperstein A, Berber E. Robotic versus laparoscopic adrenalectomy for pheochromocytoma. Ann Surg Oncol. 2013;20:4190-4194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 73] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 61. | De Crea C, Arcuri G, Pennestrì F, Paolantonio C, Bellantone R, Raffaelli M. Robotic adrenalectomy: evaluation of cost-effectiveness. Gland Surg. 2020;9:831-839. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 62. | Hirano D, Minei S, Yamaguchi K, Yoshikawa T, Hachiya T, Yoshida T, Ishida H, Takimoto Y, Saitoh T, Kiyotaki S, Okada K. Retroperitoneoscopic adrenalectomy for adrenal tumors via a single large port. J Endourol. 2005;19:788-792. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 113] [Cited by in RCA: 103] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 63. | Castellucci SA, Curcillo PG, Ginsberg PC, Saba SC, Jaffe JS, Harmon JD. Single port access adrenalectomy. J Endourol. 2008;22:1573-1576. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 141] [Cited by in RCA: 130] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 64. | Goo TT, Agarwal A, Goel R, Tan CT, Lomanto D, Cheah WK. Single-port access adrenalectomy: our initial experience. J Laparoendosc Adv Surg Tech A. 2011;21:815-819. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 65. | Cindolo L, Gidaro S, Tamburro FR, Schips L. Laparo-endoscopic single-site left transperitoneal adrenalectomy. Eur Urol. 2010;57:911-914. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 66. | Sho S, Gott DC, Yeh MW, Livhits MJ. Right single-incision retroperitoneoscopic adrenalectomy using the mini gelpoint device. VideoEndocrinology. 2016;3. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 67. | Choi SH, Hwang HK, Kang CM, Lee WJ. Transumbilical single port laparoscopic adrenalectomy: a technical report on right and left adrenalectomy using the glove port. Yonsei Med J. 2012;53:442-445. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 22] [Cited by in RCA: 23] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 68. | Hayashi M, Asakuma M, Komeda K, Miyamoto Y, Hirokawa F, Tanigawa N. Effectiveness of a surgical glove port for single port surgery. World J Surg. 2010;34:2487-2489. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 54] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 69. | Wang L, Wu Z, Li M, Cai C, Liu B, Yang Q, Sun Y. Laparoendoscopic single-site adrenalectomy vs conventional laparoscopic surgery: a systematic review and meta-analysis of observational studies. J Endourol. 2013;27:743-750. [RCA] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 70. | Hu Q, Gou Y, Sun C, Xu K, Xia G, Ding Q. A systematic review and meta-analysis of current evidence comparing laparoendoscopic single-site adrenalectomy and conventional laparoscopic adrenalectomy. J Endourol. 2013;27:676-683. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 71. | Wu S, Lai H, Zhao J, Chen J, Mo X, Zuo H, Lin Y. Laparoendoscopic Single-site Adrenalectomy vs Conventional Laparoscopic Adrenalectomy: An Updated Meta Analysis. Urol J. 2016;13:2590-2598. |
| 72. | Wu JC, Wu PC, Kang YN, Tai TE. Laparoendoscopic single-site adrenalectomy vs multi-port laparoendoscopic adrenalectomy: A systemic review and meta-analysis. Ann Med Surg (Lond). 2021;66:102388. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 73. | Jia J, Yang Z, Teng Z, Han Z. Efficacy and safety of laparoendoscopic single-site adrenalectomy versus conventional laparoscopic adrenalectomy: an updated systematic review and meta-analysis. Wideochir Inne Tech Maloinwazyjne. 2022;17:20-34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 74. | Kim WW, Lee YM, Chung KW, Hong SJ, Sung TY. Safety and feasibility of reduced-port site surgery for robotic posterior retroperitoneal adrenalectomy. Surg Endosc. 2020;34:4291-4297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 75. | Lee IA, Kim JK, Kim K, Kang SW, Lee J, Jeong JJ, Nam KH, Chung WY. Robotic Adrenalectomy Using the da Vinci SP Robotic System: Technical Feasibility Comparison with Single-Port Access Using the da Vinci Multi-arm Robotic System. Ann Surg Oncol. 2022;29:3085-3092. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 76. | Morales-Conde S, Peeters A, Meyer YM, Antoniou SA, Del Agua IA, Arezzo A, Arolfo S, Yehuda AB, Boni L, Cassinotti E, Dapri G, Yang T, Fransen S, Forgione A, Hajibandeh S, Mazzola M, Migliore M, Mittermair C, Mittermair D, Morandeira-Rivas A, Moreno-Sanz C, Morlacchi A, Nizri E, Nuijts M, Raakow J, Sánchez-Margallo FM, Sánchez-Margallo JA, Szold A, Weiss H, Weiss M, Zorron R, Bouvy ND. European association for endoscopic surgery (EAES) consensus statement on single-incision endoscopic surgery. Surg Endosc. 2019;33:996-1019. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 48] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 77. | Nickel B, Tan T, Cvejic E, Baade P, McLeod DSA, Pandeya N, Youl P, McCaffery K, Jordan S. Health-Related Quality of Life After Diagnosis and Treatment of Differentiated Thyroid Cancer and Association With Type of Surgical Treatment. JAMA Otolaryngol Head Neck Surg. 2019;145:231-238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (0)] |
| 78. | Lerchenberger M, Gündogar U, Al Arabi N, Gallwas JKS, Stepp H, Hallfeldt KKJ, Ladurner R. Indocyanine green fluorescence imaging during partial adrenalectomy. Surg Endosc. 2020;34:2050-2055. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 79. | Fu B, Zhang X, Wang GX, Lang B, Ma X, Li HZ, Wang BJ, Shi TP, Ai X, Zhou HX, Zheng T. Long-term results of a prospective, randomized trial comparing retroperitoneoscopic partial vs total adrenalectomy for aldosterone producing adenoma. J Urol. 2011;185:1578-1582. [RCA] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 80. | Jeong YB, Shin YS, Kim HJ. Significance of Laparoscopic Partial Adrenalectomy in the Era of Organ Preservation. Urol Int. 2020;104:663-664. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 81. | Li KP, Duan X, Yang XS, Huang J, Wu T. Partial vs total adrenalectomy for the treatment of unilateral aldosterone-producing adenoma: a systematic review and meta-analysis. Updates Surg. 2021;73:2301-2313. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 82. | Flammia RS, Anceschi U, Tufano A, Bologna E, Proietti F, Bove AM, Misuraca L, Mastroianni R, Tirone G, Carrara A, Luciani L, Cai T, Leonardo C, Simone G. Minimally Invasive Partial vs Total Adrenalectomy for the Treatment of Unilateral Primary Aldosteronism: A Systematic Review and Meta-Analysis. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 83. | Kaye DR, Storey BB, Pacak K, Pinto PA, Linehan WM, Bratslavsky G. Partial adrenalectomy: underused first line therapy for small adrenal tumors. J Urol. 2010;184:18-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 74] [Cited by in RCA: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 84. | Gomella PT, Sanford TH, Pinto PA, Bratslavsky G, Metwalli AR, Linehan WM, Ball MW. Long-term Functional and Oncologic Outcomes of Partial Adrenalectomy for Pheochromocytoma. Urology. 2020;140:85-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 85. | Volkin D, Yerram N, Ahmed F, Lankford D, Baccala A, Gupta GN, Hoang A, Nix J, Metwalli AR, Lang DM, Bratslavsky G, Linehan WM, Pinto PA. Partial adrenalectomy minimizes the need for long-term hormone replacement in pediatric patients with pheochromocytoma and von Hippel-Lindau syndrome. J Pediatr Surg. 2012;47:2077-2082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 27] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 86. | Billmann F, Billeter A, Thomusch O, Keck T, El Shishtawi S, Langan EA, Strobel O, Müller-Stich BP. Minimally invasive partial versus total adrenalectomy for unilateral primary hyperaldosteronism-a retrospective, multicenter matched-pair analysis using the new international consensus on outcome measures. Surgery. 2021;169:1361-1370. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 87. | Alesina PF, Knyazeva P, Hinrichs J, Walz MK. Tailored Approach in Adrenal Surgery: Retroperitoneoscopic Partial Adrenalectomy. Front Endocrinol (Lausanne). 2022;13:855326. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 12] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 88. | Neumann HPH, Tsoy U, Bancos I, Amodru V, Walz MK, Tirosh A, Kaur RJ, McKenzie T, Qi X, Bandgar T, Petrov R, Yukina MY, Roslyakova A, van der Horst-Schrivers ANA, Berends AMA, Hoff AO, Castroneves LA, Ferrara AM, Rizzati S, Mian C, Dvorakova S, Hasse-Lazar K, Kvachenyuk A, Peczkowska M, Loli P, Erenler F, Krauss T, Almeida MQ, Liu L, Zhu F, Recasens M, Wohllk N, Corssmit EPM, Shafigullina Z, Calissendorff J, Grozinsky-Glasberg S, Kunavisarut T, Schalin-Jäntti C, Castinetti F, Vlcek P, Beltsevich D, Egorov VI, Schiavi F, Links TP, Lechan RM, Bausch B, Young WF Jr, Eng C; International Bilateral-Pheochromocytoma-Registry Group. Comparison of Pheochromocytoma-Specific Morbidity and Mortality Among Adults With Bilateral Pheochromocytomas Undergoing Total Adrenalectomy vs Cortical-Sparing Adrenalectomy. JAMA Netw Open. 2019;2:e198898. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 87] [Article Influence: 14.5] [Reference Citation Analysis (0)] |
| 89. | Fassnacht M, Dekkers OM, Else T, Baudin E, Berruti A, de Krijger R, Haak HR, Mihai R, Assie G, Terzolo M. European Society of Endocrinology Clinical Practice Guidelines on the management of adrenocortical carcinoma in adults, in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2018;179:G1-G46. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 425] [Cited by in RCA: 568] [Article Influence: 81.1] [Reference Citation Analysis (0)] |
| 90. | Ranvier GG, Inabnet WB 3rd. Surgical management of adrenocortical carcinoma. Endocrinol Metab Clin North Am. 2015;44:435-452. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 91. | Wu K, Liu Z, Liang J, Tang Y, Zou Z, Zhou C, Zhang F, Lu Y. Laparoscopic vs open adrenalectomy for localized (stage 1/2) adrenocortical carcinoma: Experience at a single, high-volumecenter. Surgery. 2018;164:1325-1329. [RCA] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 92. | Hue JJ, Ahorukomeye P, Bingmer K, Drapalik L, Ammori JB, Wilhelm SM, Rothermel LD, Towe CW. A comparison of robotic and laparoscopic minimally invasive adrenalectomy for adrenal malignancies. Surg Endosc. 2022;36:5374-5381. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 93. | Kiernan CM, Lee JE. Minimally Invasive Surgery for Primary and Metastatic Adrenal Malignancy. Surg Oncol Clin N Am. 2019;28:309-326. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 94. | Arrigoni F, Bianchi G, Formiconi F, Palumbo P, Zugaro L, Gravina GL, Barile A, Masciocchi C. CT-guided cryoablation for management of bone metastases: a single center experience and review of the literature. Radiol Med. 2022;127:199-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 95. | Hendriquez R, Keihanian T, Goyal J, Abraham RR, Mishra R, Girotra M. Radiofrequency ablation in the management of primary hepatic and biliary tumors. World J Gastrointest Oncol. 2022;14:203-215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 6] [Cited by in RCA: 6] [Article Influence: 2.0] [Reference Citation Analysis (2)] |
| 96. | Shah DR, Green S, Elliot A, McGahan JP, Khatri VP. Current oncologic applications of radiofrequency ablation therapies. World J Gastrointest Oncol. 2013;5:71-80. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 46] [Cited by in RCA: 65] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 97. | Orloff LA, Noel JE, Stack BC Jr, Russell MD, Angelos P, Baek JH, Brumund KT, Chiang FY, Cunnane MB, Davies L, Frasoldati A, Feng AY, Hegedüs L, Iwata AJ, Kandil E, Kuo J, Lombardi C, Lupo M, Maia AL, McIver B, Na DG, Novizio R, Papini E, Patel KN, Rangel L, Russell JO, Shin J, Shindo M, Shonka DC Jr, Karcioglu AS, Sinclair C, Singer M, Spiezia S, Steck JH, Steward D, Tae K, Tolley N, Valcavi R, Tufano RP, Tuttle RM, Volpi E, Wu CW, Abdelhamid Ahmed AH, Randolph GW. Radiofrequency ablation and related ultrasound-guided ablation technologies for treatment of benign and malignant thyroid disease: An international multidisciplinary consensus statement of the American Head and Neck Society Endocrine Surgery Section with the Asia Pacific Society of Thyroid Surgery, Associazione Medici Endocrinologi, British Association of Endocrine and Thyroid Surgeons, European Thyroid Association, Italian Society of Endocrine Surgery Units, Korean Society of Thyroid Radiology, Latin American Thyroid Society, and Thyroid Nodules Therapies Association. Head Neck. 2022;44:633-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 146] [Article Influence: 36.5] [Reference Citation Analysis (0)] |
| 98. | Liang KW, Jahangiri Y, Tsao TF, Tyan YS, Huang HH. Effectiveness of Thermal Ablation for Aldosterone-Producing Adrenal Adenoma: A Systematic Review and Meta-Analysis of Clinical and Biochemical Parameters. J Vasc Interv Radiol. 2019;30:1335-1342.e1. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 99. | Kako Y, Ueki R, Yamamoto S, Takaki H, Aoki Y, Yokoyama O, Yamakado K. Adrenal pheochromocytoma treated by combination of adrenal arterial embolization and radiofrequency ablation. Clin Case Rep. 2021;9:1261-1265. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 100. | Brown A. A prospective randomised trial comparing radiofrequency ablation with laparoscopic adrenalectomy as an alternative treatment for unilateral asymmetric primary aldosteronism (WAVE). ClinicalTrials.gov Identifier: NCT05405101 [cited 6 June 2022]. Available from: https://clinicaltrials.gov/ct2/show/study/NCT05405101. |
| 101. | Zheng L, Zhou F, Yu X, Liang P, Cheng Z, Han Z, Yu J, Liu F, Wang W. Hypertensive Crisis during Microwave Ablation of Adrenal Neoplasms: A Retrospective Analysis of Predictive Factors. J Vasc Interv Radiol. 2019;30:1343-1350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 102. | Park BK. Percutaneous Adrenal Radiofrequency Ablation: A Short Review for Endocrinologists. Endocrinol Metab (Seoul). 2020;35:750-755. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |