Published online Dec 6, 2022. doi: 10.12998/wjcc.v10.i34.12678
Peer-review started: July 14, 2022
First decision: August 4, 2022
Revised: August 14, 2022
Accepted: November 2, 2022
Article in press: November 2, 2022
Published online: December 6, 2022
Processing time: 140 Days and 21.8 Hours
Multiple primary malignant neoplasms refer to multiple tumors with different origins. They may be synchronous or metachronous. The incidence is 0.73%– 11.7%. Synchronous cases of breast cancer with sarcoma are rare.
Here, we report a 78-year-old female patient admitted to hospital after accidental discovery of a left axillary mass. Preoperative examination revealed a breast mass. Pathology showed left breast cancer and left axillary sarcoma. The patient underwent surgery, endocrine therapy and radiotherapy. She has been followed up for 1 year, and no local recurrence or distant metastasis was observed.
Attention should be paid to multiple primary malignant neoplasms, not limited to the current diagnosis and analysis, avoiding missed diagnosis and misdiagnosis.
Core Tip: Multiple primary malignant neoplasms refer to multiple tumors with different origins. They may be synchronous or metachronous, with an incidence of 0.73%–11.7%. Synchronous cases of breast cancer with sarcoma are rare. In clinical practice, attention should be paid to multiple primary malignant neoplasms, not limited to the current diagnosis and analysis, avoiding missed diagnosis and misdiagnosis. For patients whose clinical symptoms cannot be explained by a single tumor, the possibility of multiple primary malignant neoplasms should be considered, and comprehensive examinations should be performed to achieve early diagnosis and treatment.
- Citation: Gao N, Yang AQ, Xu HR, Li L. Malignant fibrous histiocytoma of the axilla with breast cancer: A case report. World J Clin Cases 2022; 10(34): 12678-12683
- URL: https://www.wjgnet.com/2307-8960/full/v10/i34/12678.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i34.12678
Multiple primary malignant neoplasms (MPMNs) refer to the simultaneous or successive occurrence of ≥ 2 types of primary malignant tumors in a single organ or different organs of the same individual. With the improvement of diagnosis and treatment of malignant neoplasms, the survival of patients has been significantly prolonged. The number of patients with MPMNs is increasing gradually, affecting survival and quality of life[1]. MPMNs can be divided into synchronous and metachronous neoplasms according to the different chronological order of their occurrence. When the interval between two or more malignant neoplasms is ≤ 6 mo, they are synchronous neoplasms, and if the gap is > 6 mo, they are metachronous neoplasms.
A 78-year-old female patient was admitted to hospital after the accidental discovery of a left axillary mass for > 18 mo duration.
Eighteen months prior, the patient accidentally found a peanut-sized mass in her left axilla, accompanied by mild tenderness, without local skin redness, skin depression, nipple discharge or other abnormal manifestations. She had no fever, chills, chest tightness, dyspnea or other symptoms of general discomfort. She had been treated in a local hospital, but the treatment was unknown, and the tumor grew slowly. She came to the outpatient department of our hospital. Mammography showed that the high-density nodular shadow in the left breast was about 10 mm × 7 mm, BI-RADS 4B (a breast imaging reporting and data system). In the left axilla, there was a solid lymph node about 24 cm × 17 cm in size, with clear structure.
The patient had hypertension for > 20 years that was controlled by oral nifedipine. She had diabetes for > 20 years, and blood glucose was controlled by oral metformin.
The patient’s age of menarche was 14 years and menopause at 56 years. The patient married at 23 years and has two sons and a daughter. Her parents are deceased, and her father died of lung cancer. She had no family history of genetic disease.
Multiple enlarged lymph nodes were palpable in the left axilla and were fused. The largest one was about 4 cm × 2 cm and hard in texture with unclear boundaries. There was no palpable enlarged lymph node in the supraclavicular fossa of the affected side. There was no obvious abnormality in the contralateral mammary gland and axilla.
Laboratory examinations were normal.
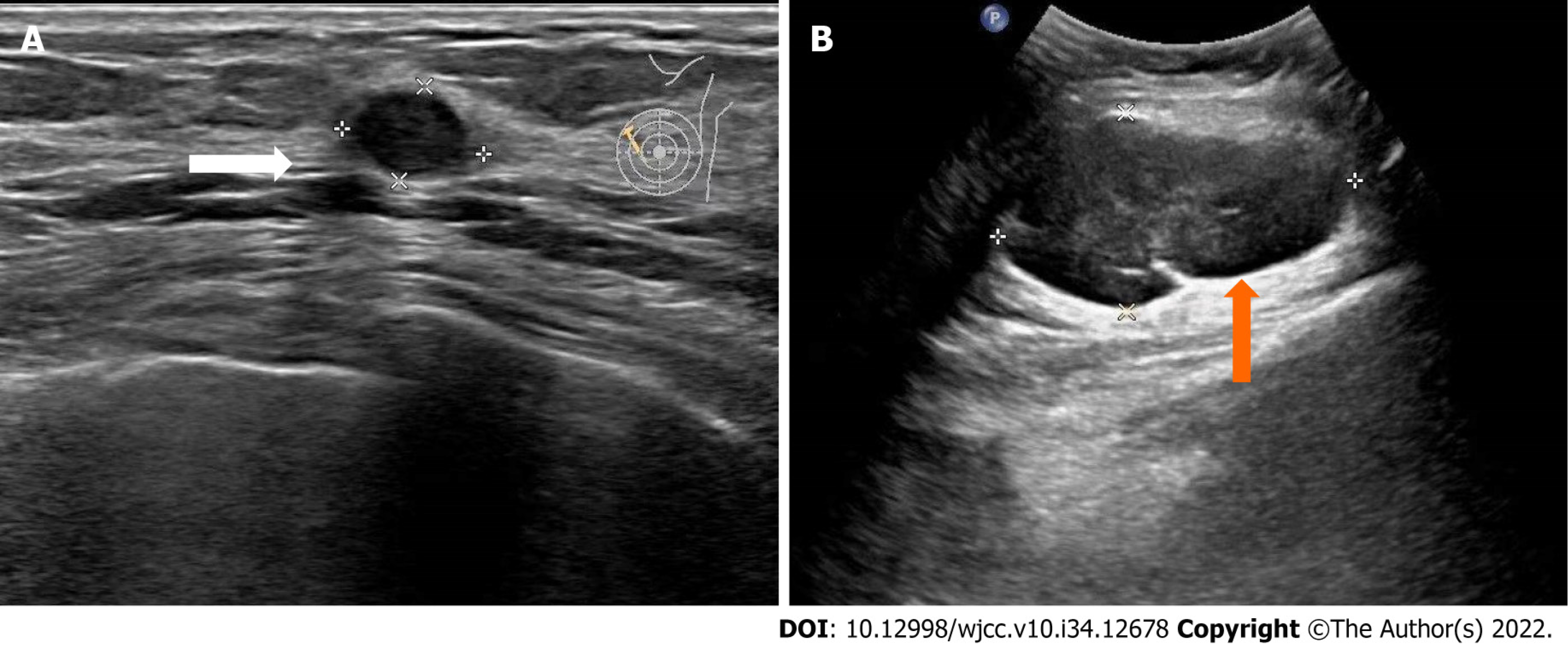
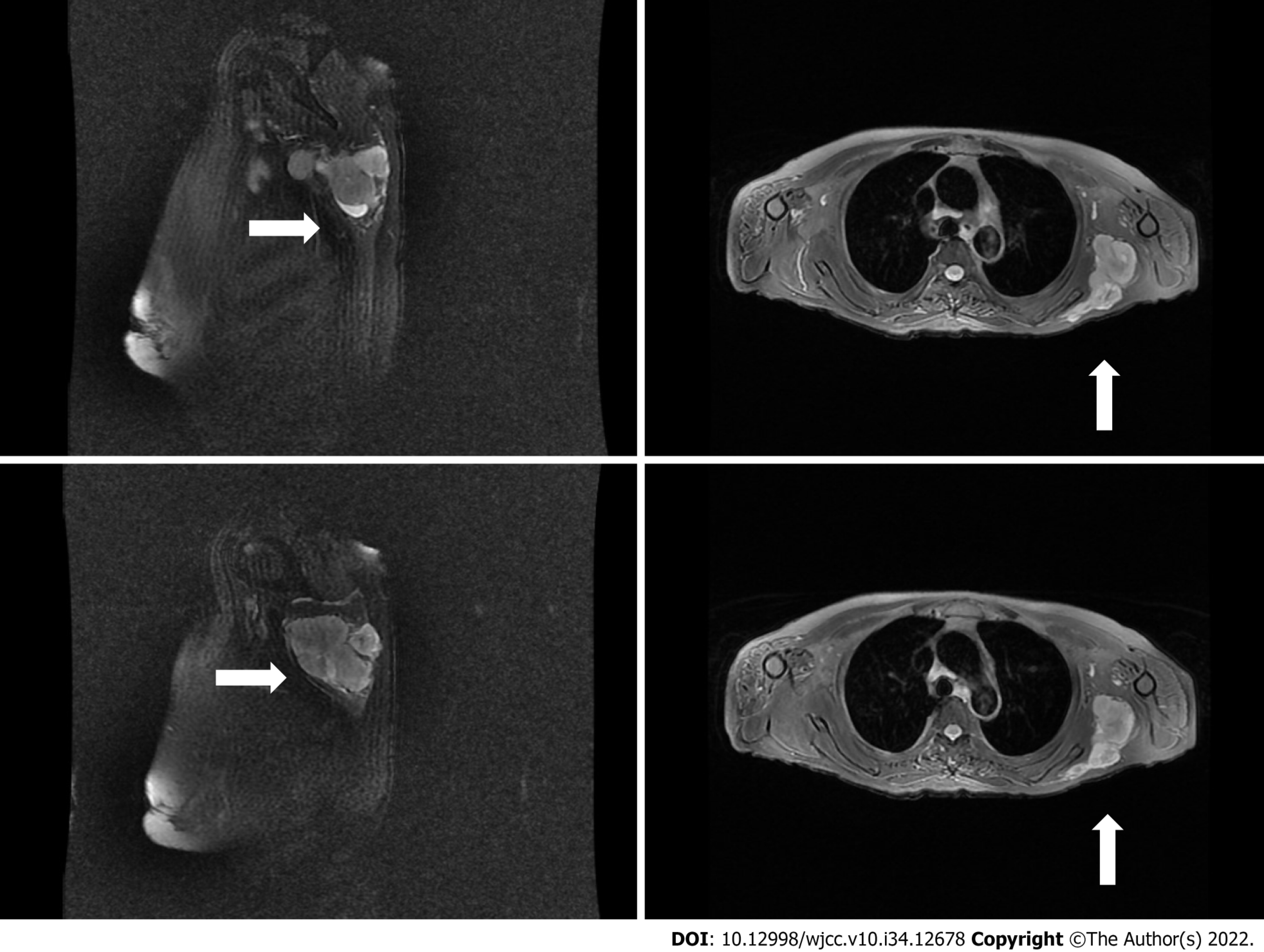
Color ultrasonography of the breast after admission showed multiple low-echo nodules in the left breast, the largest being about 9 mm × 6 mm, located at 10 o’clock in the left breast, 22 mm from the nipple, with irregular shape and BI-RADS 4A. Multiple lymph nodes in the left axilla were enlarged; the largest one was about 19 mm × 10 mm, with a clear boundary and irregular shape. The left axillary hypoechoic mass was about 73 mm × 40 mm, with a clear boundary and irregular shape (Figure 1). Magnetic resonance imaging of the shoulder joint showed abnormal mass signals in the left latissimus dorsi muscle, with irregular shape, lobulation and uneven internal signals; most of which showed iso-T1 and slightly longer T2 signal changes. The maximum axial cross-section was about 8.1 cm × 4.4 cm, and no obvious abnormal signal changes in the left scapula were observed (Figure 2).
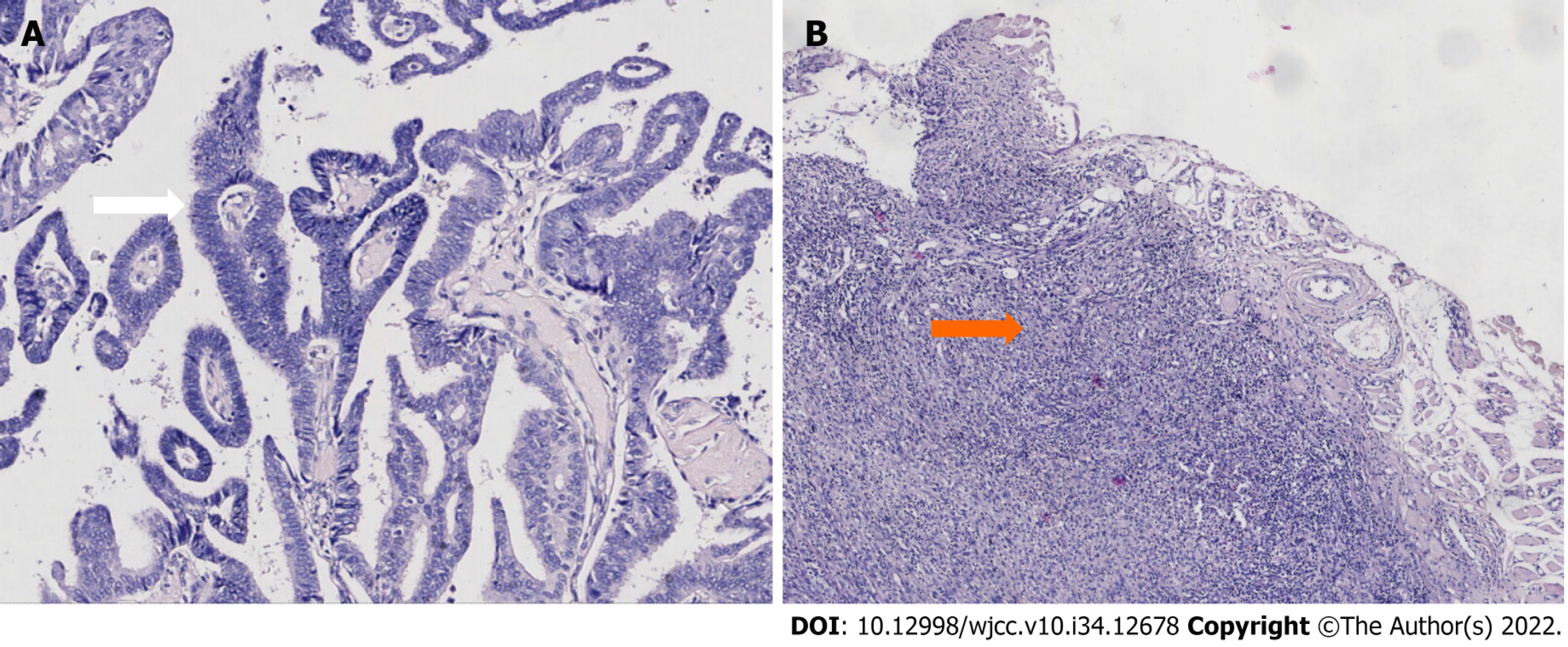
Core needle biopsy of the breast and axillary mass was performed, and histopathological examination (Figure 3) showed encapsulated papillary carcinoma of the left breast with micropapillary carcinoma and sarcoma of the left axilla.
Left mastectomy, sentinel lymph node biopsy of the left axilla and resection of the latissimus dorsi sarcoma were performed. She was treated with letrozole for breast cancer endocrine therapy after surgery. Radiotherapy (50 Gy in 25 fractions) was performed on the left latissimus dorsi muscle remnant 14 d after surgery.
She has received regular clinical follow-up for 1 year after diagnosis, and there was no local recurrence or distant metastasis.
Advances in diagnostic technology and development of comprehensive treatment have prolonged the survival time of patients with malignant tumors, and the incidence of MPMNs has been increasing gradually[2]. MPMNs vary according to pathogenic factors, geographic region, race, sex, age and other factors, and the most common sites affected also differ. The main mechanisms of MPMNs include genetic factors, environmental factors (smoking, alcoholism, obesity, etc) and iatrogenic factors (radiotherapy, chemotherapy, etc). It has been found that there is no difference in prognosis between patients with MPMNs and those with only one type of cancer[3,4]. The reasons may be related to the gradual increase of complete resection rate, standardized postoperative management and prolonged survival of patients. However, the prognosis of breast MPMNs was worse than that of breast non-MPMNs, and the prognosis of synchronous MPMNs was worse than that of metachronous MPMNs[5,6]. Many factors, such as age, degree of differentiation, disease stage, distribution of the second primary cancer, time between two cancers and tumor treatment, are related to the prognosis of MPMNs[5,7].
The first case of MPMNs including breast cancer and sarcoma was reported by Warren in 1936[8]. In MPMNs of breast and sarcoma, radiotherapy is considered to be a major causative factor[4,9]. The definition of radio-induced sarcoma proposed by Cahan and Woodard[10] and modified by Arlen et al[11] is characterized by the following: (1) Radiotherapy at least 3 years before the onset of the sarcoma; (2) The disease occurred in previously irradiated tissue; and (3) Different histology compared to a previously irradiated primary tumor. Radiation-induced sarcoma is a rare soft tissue sarcoma occurring in the postoperative radiation area, with an incidence of 0.03%–8.00%[12].
The most common histological type is angiosarcoma. Yap et al[13] reported that angiosarcoma accounted for 56.8% of the sarcomas occurring in the radiotherapy area, followed by malignant fibrous histiocytoma (MFH) (15.9%), fibrosarcoma and chondrosarcoma (6.8%) and leiomyosarcoma (4.5%). Most of the radiation-induced sarcoma reported in the literature has a poor prognosis and high recurrence rate. The mean recurrence time was 12.8 ± 10.6 mo (median 7.5 mo)[14], the 5-year survival rate was 27%–48%, the 5-year disease-free survival rate was 35%, and the mean survival time was 23 mo[15]. In most cases, leiomyosarcoma differs from other breast or chest wall sarcomas in that it is less aggressive and has a better prognosis. It is a slow-growing tumor[13]. Factors associated with poor prognosis include age, positive surgical margins, large highly differentiated tumors and distant metastasis. Therefore, early detection and diagnosis are important to improve the prognosis of radiation-induced sarcoma.
Our patient had synchronous breast cancer and MFH. She had no family history of cancer, poor living habits and no history of radiotherapy. The occurrence of MPMNs might be related to defective gene repair[16], but it has not been confirmed by genetic testing. For patients with MPMNs, whether or not to undergo radical surgery is the key to long-term survival. The treatment principle of MPMNs should be the same as that for single cancers. Radical surgery should be actively performed once diagnosed, as long as there is no contraindication to surgery. Considering the different degrees of malignancy of MPMNs, treatment of potentially life-threatening neoplasms should be given priority. Combined treatments such as radiotherapy and chemotherapy should be adopted to improve prognosis.
In our case, total mastectomy and radical resection of MFH were performed simultaneously. The patient received combined therapy of endocrine and local radiotherapy after surgery, and the therapeutic effect was good. At present, cases of synchronous MPMNs are rare in clinical practice. Since the axilla is the most common site of breast cancer metastasis, MFH of the axilla and synchronous breast cancer are easily misdiagnosed as breast cancer combined with axillary lymph node metastasis. Our patient was diagnosed with breast cancer and axillary soft tissue tumor by preoperative imaging and was pathologically confirmed as breast ductal carcinoma in situ and axillary MFH. Therefore, the possibility of MPMNs should be considered in patients with breast and axillary space-occupying lesions.
In clinical work, attention should be paid to MPMNs, not limited to the current diagnosis and analysis, resulting in missed diagnosis and misdiagnosis. For patients whose clinical symptoms cannot be explained by a single tumor, we should consider the possibility of MPMNs and conduct a comprehensive examination to achieve early detection, diagnosis and treatment.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Fang S; Sehrawat A, India; Serban D, Romania S-Editor: Xing YX L-Editor: Filipodia P-Editor: Xing YX
| 1. | Moertel CG, Dockerty MB, Baggenstoss AH. Multiple primary malignant neoplasms. II. Tumors of different tissues or organs. Cancer. 1961;14:231-237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 2. | Morton LM, Onel K, Curtis RE, Hungate EA, Armstrong GT. The rising incidence of second cancers: patterns of occurrence and identification of risk factors for children and adults. Am Soc Clin Oncol Educ Book. 2014;e57-e67. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 91] [Cited by in RCA: 132] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 3. | Izmajłowicz B, Kornafel J, Błaszczyk J. Multiple neoplasms among cervical cancer patients in the material of the lower Silesian cancer registry. Adv Clin Exp Med. 2014;23:433-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Shinjo K, Asai T, Saito S, Tuboi S, Tamura J. [Multiple primary malignant tumors of rhabdomyosarcoma in an upper arm and breast cancer]. Gan No Rinsho. 1988;34:123-129. [PubMed] |
| 5. | Kim BK, Oh SJ, Song JY, Lee HB, Park MH, Jung Y, Park WC, Lee J, Sun WY; Korean Breast Cancer Society. Clinical Characteristics and Prognosis Associated with Multiple Primary Cancers in Breast Cancer Patients. J Breast Cancer. 2018;21:62-69. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Motuzyuk I, Sydorchuk O, Kovtun N, Palian Z, Kostiuchenko Y. Analysis of Trends and Factors in Breast Multiple Primary Malignant Neoplasms. Breast Cancer (Auckl). 2018;12:1178223418759959. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 7. | Kim SW, Kong KA, Kim DY, Ryu YJ, Lee JH, Chang JH. Multiple primary cancers involving lung cancer at a single tertiary hospital: Clinical features and prognosis. Thorac Cancer. 2015;6:159-165. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Warren S, Sommer GN. Fibrosarcoma of the soft parts: with special reference to recurrence and metastasis. Archives of Surgery. 1936;33:425-450. |
| 9. | Huang YJ, Huang TW, Lin FH, Chung CH, Tsao CH, Chien WC. Radiation Therapy for Invasive Breast Cancer Increases the Risk of Second Primary Lung Cancer: A Nationwide Population-Based Cohort Analysis. J Thorac Oncol. 2017;12:782-790. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 46] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 10. | Cahan WG, Woodard HQ. Sarcoma arising in irradiated bone; report of 11 cases. Cancer. 1948;1:3-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 11. | Arlen M, Higinbotham NL, Huvos AG, Marcove RC, Miller T, Shah IC. Radiation-induced sarcoma of bone. Cancer. 1971;28:1087-1099. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 12. | Virtanen A, Pukkala E, Auvinen A. Incidence of bone and soft tissue sarcoma after radiotherapy: a cohort study of 295,712 Finnish cancer patients. Int J Cancer. 2006;118:1017-1021. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 60] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 13. | Yap J, Chuba PJ, Thomas R, Aref A, Lucas D, Severson RK, Hamre M. Sarcoma as a second malignancy after treatment for breast cancer. Int J Radiat Oncol Biol Phys. 2002;52:1231-1237. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 171] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 14. | Ulrich AE, Frossard E. On the history of a reoccurring concept: phosphorus scarcity. Sci Total Environ. 2014;490:694-707. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 39] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 15. | Erel E, Vlachou E, Athanasiadou M, Hassan S, Chandrasekar CR, Peart F. Management of radiation-induced sarcomas in a tertiary referral centre: a review of 25 cases. Breast. 2010;19:424-427. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 16. | Ahmed H, Salama A, Salem SE, Bahnassy AA. A case of synchronous double primary breast carcinoma and osteosarcoma: Mismatch repair genes mutations as a possible cause for multiple early onset malignant tumors. Am J Case Rep. 2012;13:218-223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |