Published online Nov 26, 2022. doi: 10.12998/wjcc.v10.i33.12328
Peer-review started: July 10, 2022
First decision: September 5, 2022
Revised: September 16, 2022
Accepted: October 26, 2022
Article in press: October 26, 2022
Published online: November 26, 2022
Processing time: 136 Days and 4.2 Hours
Periprosthetic supracondylar femoral fractures (PSFs) present a challenge in terms of optimizing fixation in patients with poor bone quality. Surgical treatment and peri-operative management of PSFs in the elderly remain a burden for orthopedic surgeons. Among different treatment options, locking plate (LP) and retrograde intramedullary nail (RIMN) have shown favorable results. However, reduced mobility and protected weight-bearing are often present in the postoperative older population. With a purpose of allowing for early weight-bearing, a modified nail plate combination (NPC) was redesigned for PSF management.
In our cases, two elderly osteoporotic female underwent total knee arthroplasty (TKA), and then suffered from low energy trauma onto their knees after falling to the floor. Plain radiographs or computed tomography scans demonstrated oblique or transverse PSFs, both of which occurred at the distal femur above TKA. The modified NPC technique was performed for treatment of PSFs. The patient was made foot flat weight bearing in 1 wk. At 6-mo follow-up, the union was ultimately achieved using modified NPC with satisfactory implant outcomes.
Neither LP nor RIMN alone may provide adequate support to allow for union in circumstances where the patient has severely osteopenic bone. Therefore, developing a modified implant offer an alternative choice for treating PSFs. These two cases revealed that this technique is a viable option for the geriatric osteoporotic PSFs, offering safe, early weight bearing and favorable clinical outcomes.
Core Tip: In this article, we reported two cases of elderly osteoporotic patients with periprosthetic supracondylar femoral fractures (PSFs) in the setting of total knee arthroplasty (TKA) after treated with modified nail plate combination (NPC), which was granted by the Trademark Office of China National Intellectual Property Administration. Unlike inserting retrograde intramedullary nail (RIMN) for holding the reduction after the initial reduction of fragments in previous NPC cases, it is the modified locking plate (LP) that performs the initial reduction and fixation of the distal femoral fragments in our cases. Initial reduction and fixation with LP and then insertion of RIMN can avoid an extension deformity in nailing of PSFs due to the femoral component of the TKA occluding the optimal start point. In patients with osteoporosis, modified NPC is beneficial and effective, attributed to early weight bearing and favorable clinical outcomes.
- Citation: Li QW, Wu B, Chen B. Modified fixation for periprosthetic supracondylar femur fractures: Two case reports and review of the literature. World J Clin Cases 2022; 10(33): 12328-12336
- URL: https://www.wjgnet.com/2307-8960/full/v10/i33/12328.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i33.12328
The rate of periprosthetic supracondylar femoral fractures (PSFs) above total knee arthroplasty (TKA) ranges between 0.3% and 2.5% in the literature, and higher after revision TKA[1]. The imminent raise of PSFs is associated with the increased life expectancy of the population as well as the steadily increased number of TKAs in the future[2]. The majority of these PSFs can be attributed to low-energy trauma including ground-level falls, and other common risk factors, including the aging, the female and other pathological conditions, such as osteoporosis, rheumatoid arthritis, chronic use of steroids, neurologic disorders along with revision TKA, making patients predisposed to periprosthetic fractures[3,4]. PSFs pose a management challenge by the prosthesis’s stability and type, the available bone’s quality and quantity for fracture fixation in the distal femoral metaphyseal region, the displacement’s fracture pattern and degree as well as the surgeons’ clinical experience[5]. Achieving stable fixation to allow early mobility is the goal of their treatment. Among different treatment options, the exclusive application of a laterally locking plate (LP)/an retrograde intramedullary nail (RIMN) usually warrants a 4-6 wk period of protected weight-bearing rather than early weight bearing as tolerated, especially in those with osteoporosis[6]. Combining the 2 implants could make the construct well balanced and adequate fixated, allowing for early weight bearing after surgery. Herein, we reported two cases of elderly osteoporotic patients with PSFs in the setting of TKA which went on to union after treated with modified nail plate combination (NPC) technique.
Case 1: A 71-year-old Chinese female was presented to our institution, complaining of the pain, swelling, and limitation of motion in right knee because of falling to the floor.
Case 2: Another 73-year-old Chinese female was presented to our institution with pain, swelling, and limitation of motion in the left knee because of slipping and falling from standing position.
Case 1: The patient suffered from pain, swelling, and limited movements of her right knee due to an accidental fall. She was taken to our institution quickly for radiograph examination.
Case 2: The patient went through an accidental fall to the left knee. She came to our institution for better treatment and nursing and given radiograph and computed tomography (CT) scan.
Case 1: The patient’s pertinent surgical history of a right TKA 1 mo earlier was pivotal for her PSF.
Case 2: Her left TKA was applied 2 years before presentation.
Case 1: The patient denied any traumatic history associated with PSFs in his family.
Case 2: Her family also had no significant trauma history of PSFs.
Case 1: Physical examination on admission revealed slight swelling of the right thigh and knee, local tenderness and percussion pain, and limited movement of the right knee.
Case 2: On admission, the results of the physical examination were consistent with Case 1.
Case 1: After admission, the bone mineral density (BMD) examination showed that her BMD values were 71% and 68% of the young adult mean (YAM) at the lumbar spine and femoral neck, respectively. Other routine examination indexes were basically normal.
Case 2: Her BMD values were 62% and 65% of the YAM at the lumbar spine and femoral neck, respectively. Other laboratory examinations before surgery were also basically normal.
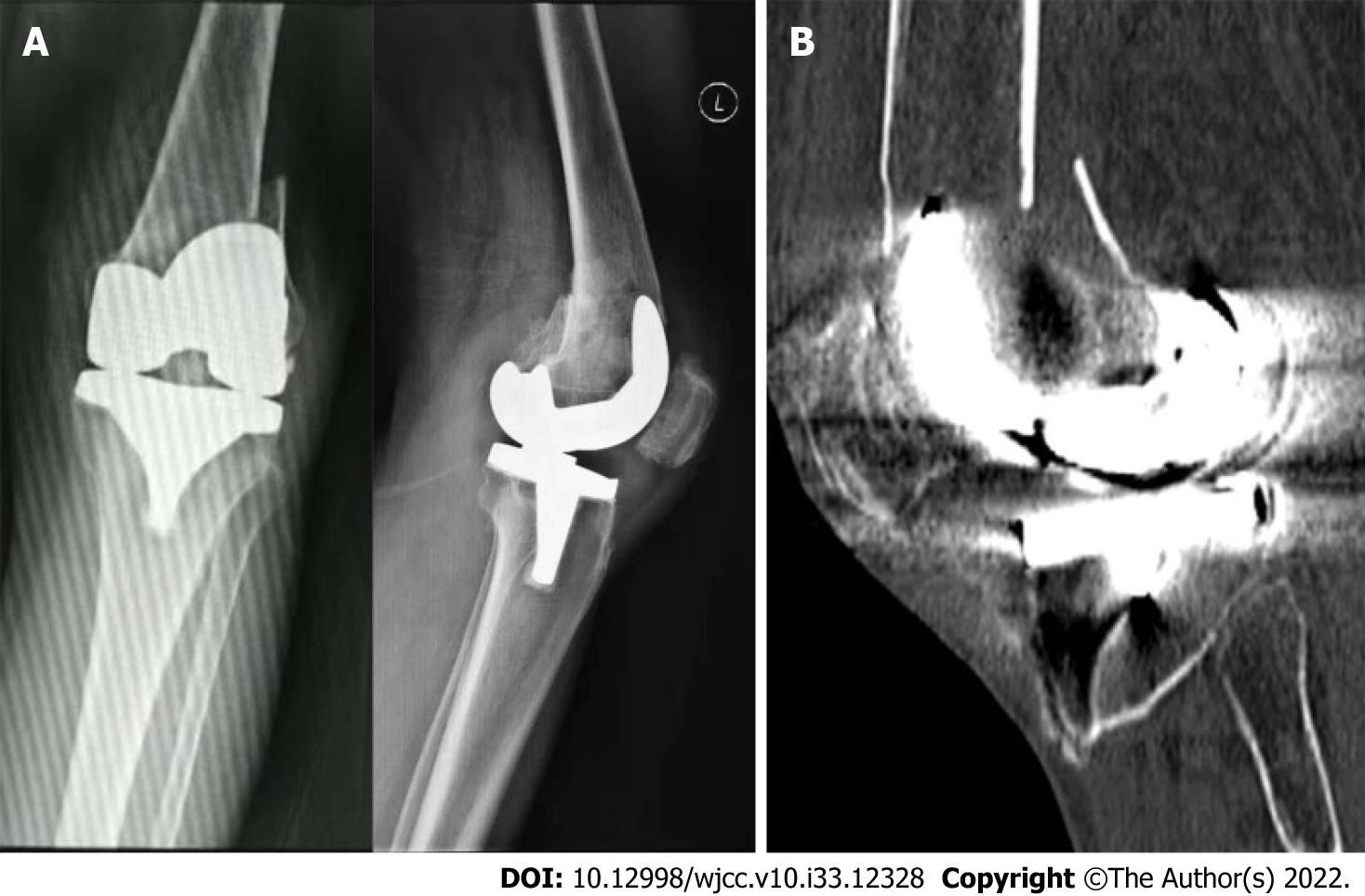
Case 1: Plain radiographs revealed a right PSF above the TKA femoral component, which was non-comminuted and oblique (Figure 1).
Case 2: Based on the results of radiographs and CT scans, a left PSF just above the anterior flange of femoral prosthesis was found, which was non-comminuted and transverse (Figure 2).
Cases 1 and 2: The patients were diagnosed as periprosthetic supracondylar femoral fractures and osteopetrosis.
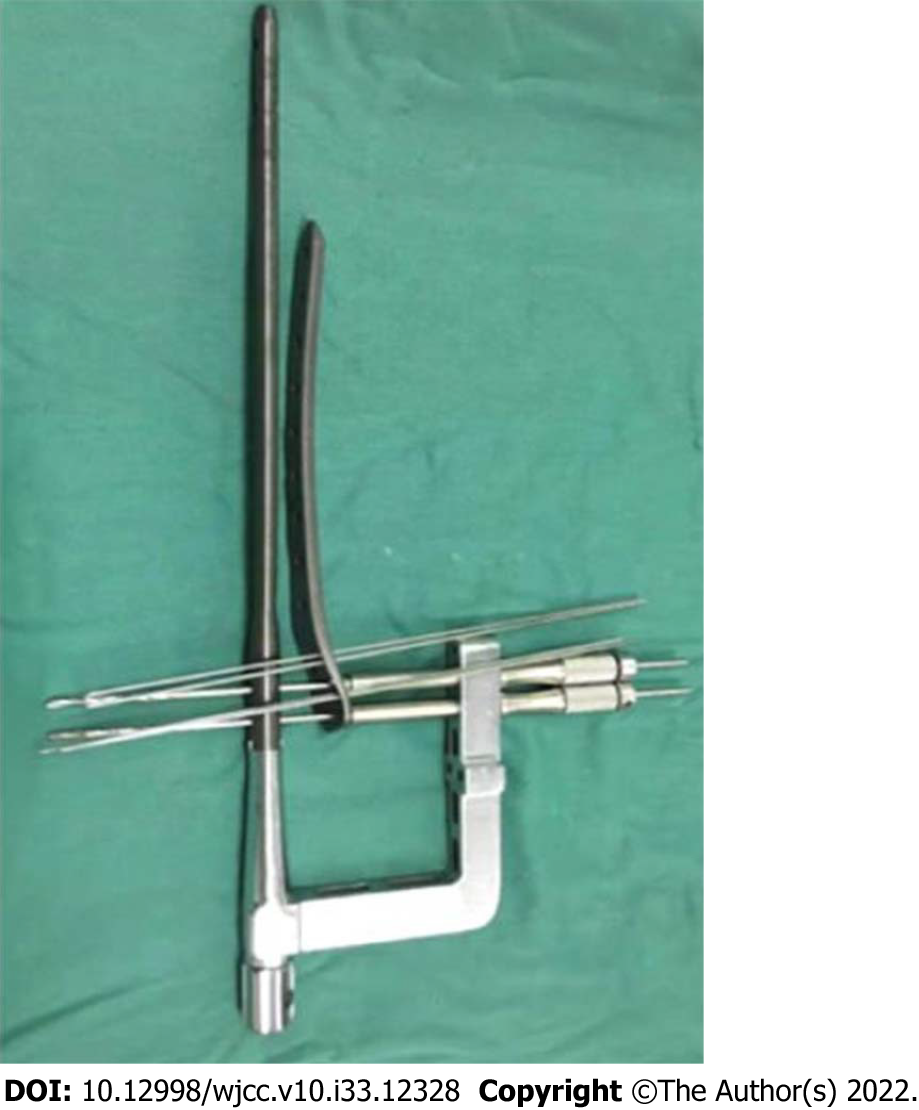
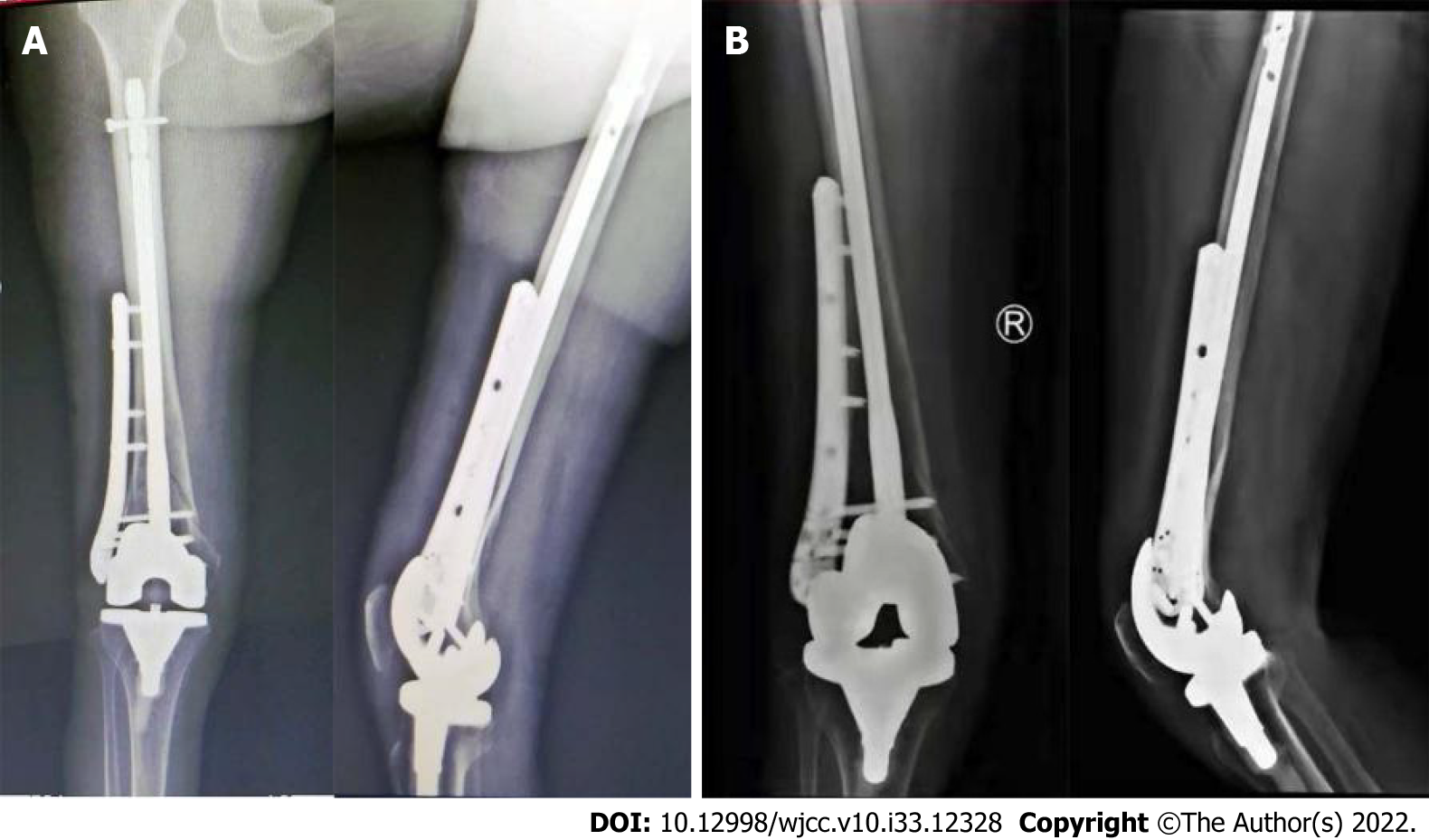
Cases 1: For surgery, modified NPC technique was applied in PSF situation, consisted by a specially designed periprosthetic LP, a RIMN and an intramedullary targeting arm, granted by the Trademark Office of China National Intellectual Property Administration (Patent for the invention No. ZL 2017 2 1268551.1 from September 29, 2017). As shown in Figure 3, the 2 distal locking holes of the specially designed periprosthetic LP were perfectly matched with the 2 distal interlocking holes of the RIMN in terms of spacing and angle. More importantly, the modified LP had a staggered pattern for insertions of other locking screws and K wires to avoid the nail and distal TKA implant. In operation, a limited lateral parapatellar approach facilitated enough exposure for proper assessment and fixation. Provisional reduction of the femur was successfully performed using reduction clamps. A modified LP was placed. Next, K wires were inserted to the distal end of femur to pin the plate in the appropriate site, while unicortical or bicortical screws were inserted to fix the proximal femur. Subsequently, a RIMN was transtendinously inserted. Usually, the targeting arm could help to choose the correct 2 distal locking holes of modified LP. With the application of 2 distal locking screws for the plate, the linkage was further reinforced based on the locking mechanism with a fixed angle. Then, 2 or 3 extra locking screws were filled at the distal end of LP. Finally, the proximal interlocking screw was placed in the RIMN, fixing proximal side of the construct (Figure 4A). Data on operative variables were obtained from medical record. Surgical duration totaling 126 min was recorded, while a hospital stay of 12 d was also observed.
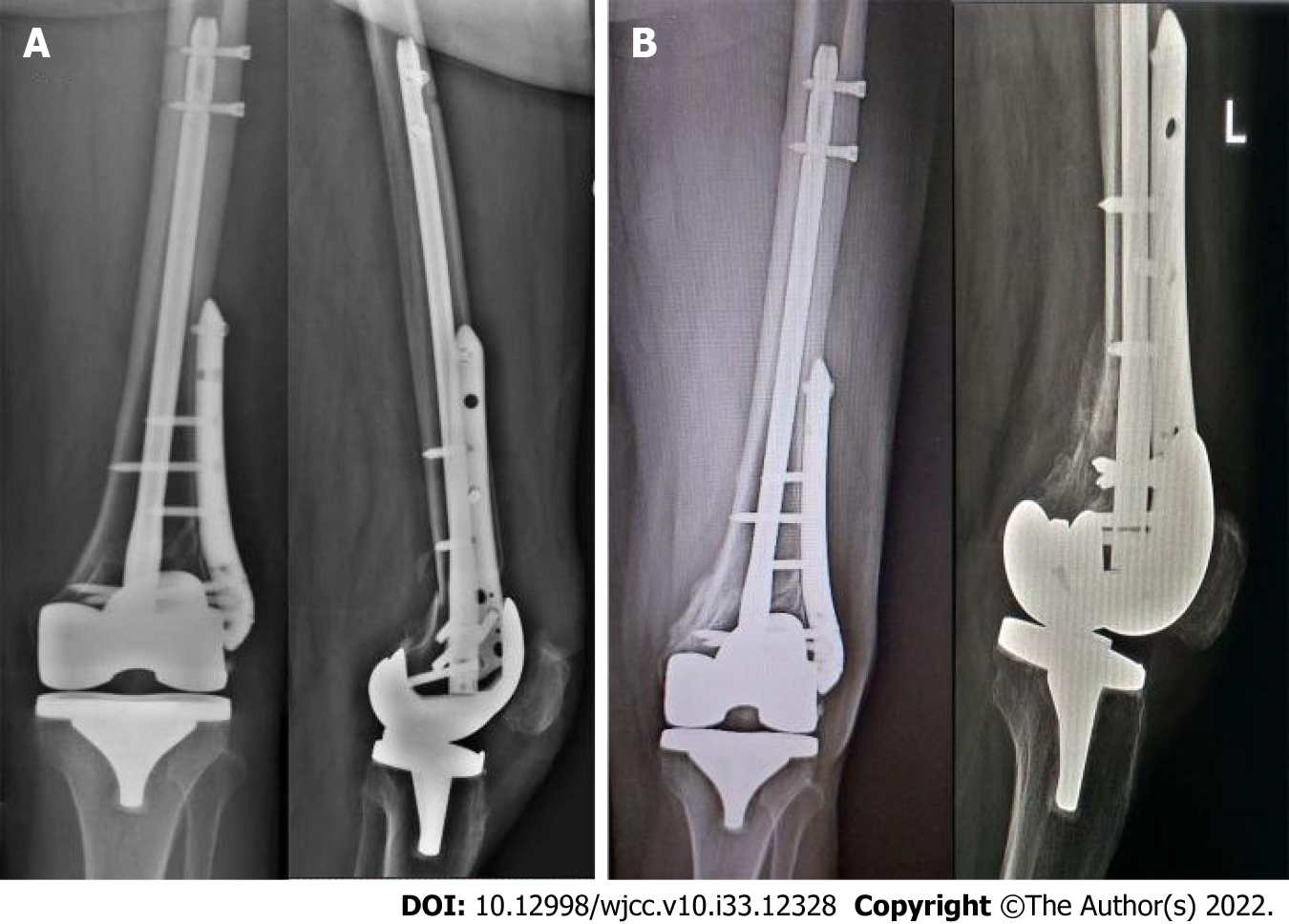
Case 2: Similar surgical procedures were carried out as described in case 1 (Figure 5A). Operative time was 135 min totally, and the hospital length of stay was 14 d.
Cases 1: The patient followed a protocol of active-assisted knee range of motion and quadriceps strengthening from day 1 and foot flat weight bearing in 1 wk. Finally, bone union in six months was observed in her follow-ups (Figure 4B).
Case 2: Similar post-operative rehabilitation protocols were carried out as described in case 1. Six months after the operation, the patient was able to walk unaided and without any pain. Her PSF was healed (Figure 5B).
PSFs are frequently observed in fragility fractures accompanied by osteoporotic bone quality, very demanding complications of TKA. In the metaphyseal region of the distal femur with an obvious long segment of thin cortex as well as a soft metaphysis, a simple twisting injury can cause a fracture propagating almost the entire distal third of the femur. Biomechanical studies have also revealed that the supracondylar bone proximal to a TKA implant was weaker due to stress shielding and osteolysis[7]. The occurrence of a TKA is linked with a bone loss of about 15% in the distal diaphyseal and metaphyseal region near the prosthesis[8].This bone loss in combination with the increased prevalence of osteopenia could obviously upregulate the risk for periprosthetic fractures. The great mass happened in female and the injury caused by “slip fall” is the most common[9].Reduced mobility along with general osteoporosis attributed to age or sex can be found in the elderly. In our cases, both of 2 osteoporotic patients were female and elderly that suffering from PSFs due to low energy trauma.
The management of PSFs remains challenging. A number of complications, such as the delayed union, nonunion, stiffness and infection have been ever observed during PSF treatments. Recently, a systematic analysis reported a non-union rate of PSFs to be 10%-15%, irrespectively of the treatment method[10]. Therefore, to decrease complication and reoperation rates, there have been various treatments for PSFs performed, including newer fixatives to maintain fracture reduction and additional strategies reported for unreconstructable fractures. Besides, it is well recognized that in most of the cases, operative intervention is in urgent need for these complex fractures, however, a gold standard for surgical fixation remains unclear. According to the literature, compared to extensive approaches and rigid anatomic fixation methods, the treatment of PSFs after TKA is evolving toward minimally invasive percutaneous plate osteosynthesis and RIMN[11]. The modern LP and RIMN technology have been demonstrated to be superior in biomechanical and clinical outcomes in contrast with conventional non-locked plating[12]. Due to the similarity in application period and fracture healing biomechanism between LP and RIMN, numerous comparative studies have been carried out[13]. Despite of their specific merits as well as the different indications attributing from their unique fixation mechanism, recent systematic reviews and meta-analysis consistently demonstrated no statistically significant differences in clinical results, time to fracture union, complication rate, or the range of postoperative motion between the two treatment options (Table 1)[14,15]. LP can be applied in most PSF types and prosthesis designs and allows for of direct reduction except for medial femoral cortical defects[10,16].Moreover, a polyaxial LP allows a reduction of distal small fragments in direction to the plate, accompanied by sufficient relative stability for fracture healing[17]. However, for elderly osteoporotic populations, surgeons are cautious about early weight bearing with a LP fixation. LP can also be inserted submuscularly through a minimally invasive approach with minimum disruption of the fracture healing microenvironments. However, it also inevitably dissect a certain amount of soft tissue with the potential of periosteal stripping. Comparatively, RIMN was also identified as a minimally invasive and soft-tissue-friendly internal fixation method as reported in orthopaedic literature for treating PSFs[18]. The fact that RIMN is coaxially implanted along the anatomical axis of the femur endowing this implant the stiffest construct under axial loading due to an short moment arm from the axis of applied load to the neutral axis of the nail[19]. Notably, the exclusive application of RIMN relies on fracture pattern as well as intercondylar box design of femoral components. The distal fixation is possibly not adequate for very low supracondylar fractures[20]. Malunion of typically extension deformities has been frequently reported in the setting of RIMN since the entry point of the RIMN is set based on the femoral component box, which forces the fracture into hyperextension, and make the reliance on indirect reduction with RIMN techniques[21]. The inevitably mismatched diameter of the nail with metaphyseal flare may make the nail toggled in the metaphysis, posing a risk to the fixating stability in osteoporotic patients[22]. Restricting postoperative mobilization can be a problem in the elderly osteoporotic patients based on the fact that early weight bearing and returning to baseline activity are able to directly reduce the morbidity and mortality of patients. Therefore, NPC is developed as a novel method for fracture fixation which has been applied in several years, with the aim of providing stable fracture fixation and allowing for early postoperative weight bearing[23].
| LP | RIMN | P value | |
| Six month union rate | 87.5% | 83.5% | 0.68 |
| Union time | 4.0 ± 0.27 mo | 3.7 ± 0.30 mo | 0.95 |
| Operation time | 87.4 ± 6.4 min | 91.6 ± 6.8 min | 0.46 |
| Complication rate | 20.6% | 16.7% | 0.73 |
| Postoperative knee functional score | 76.5 ± 14.5 | 80.6 ± 10.9 | 0.31 |
As previously reported, augmented fixation with NPC has been conducted in patients who failed from the fixation of single plate or nail and required surgeries for nonunion and revision, or when a proximal hip replacement stem needed to be bridged[24,25]. Currently, it has been increasingly applied in PSFs primary fixation. Over the past several years, there were relatively few cases using NPC for the treatment of PSFs after TKA, however, the union rate was approximately 100% at their follow-ups[23,26-28]. There have also been few comparative studies between NPC and traditional fixations performed previously. Compared to LP alone, fixation with NPC significantly improve fracture union rates in elderly patients[29,30]. Biomechanically, compared to LP or RIMN, NPC was more resistant to the failure in axial and torsional load tests as well as the load to failure tests[31,32]. According to their biomechanical experiments, higher mechanical strength of the combined construct and the possibility of earlier mobilization make it an advantageous option in patients with osteoporosis. An advantage of the NPC over dual plating is that there is less disturbance of the fracture milieu[29]. Furthermore, linking the LP and RIMN distally potentially achieve more evenly distribution of forces contributing to the stability and early weight bearing[27].In our cases, we presented a modified NPC technique, which involves a specially designed periprosthetic LP for adequate fixation of the fracture. Unlike inserting RIMN for holding the reduction following the initial reduction of fragments in previous NPC cases, the modified LP that performs the initial reduction and fixation of the distal femoral fragments in our cases. Insertion of RIMN then allows for further stable fixation of the distal construct and increasing torsional stiffness, further avoiding the extension deformity in nailing of PSFs due to the femoral component of the TKA occluding the optimal start point. Regarding of distal fixation, 2 bicortical interlocking screws were placed to link the plate and the nail. Based on available literature on distal screws, 2 distal interlocking screws in the nail are recommended in the setting of severely osteoporosis or those in need of the increased resistance to torque[28]. Furthermore, PSF patients should also bear the increased cost of supplemental implants for the potential early weight-bearing.
We reported two cases of periprosthetic supracondylar knee fractures treated with modified NPC technique in elderly osteoporotic patients. Since exclusive LP or RIMN is in need of protected weight bearing, NPC is much more preferable for elderly osteoporotic populations allowing for postoperative earlier mobilization and shared load bearing across the fracture site. In the two cases, the distal femoral fixation was achieved through the modified NPC technique with the reduction using a specially designed periprosthetic LP, which can avoid the extension deformity in the later healing period owing to more posterior starting point of RIMN. Future studies need to be directed toward larger populations of patients along with cost analysis for the increased costs for the implants.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Barik S, India; Ullah K, Pakistan S-Editor: Liu GL L-Editor: A P-Editor: Liu GL
| 1. | Su ET, DeWal H, Di Cesare PE. Periprosthetic femoral fractures above total knee replacements. J Am Acad Orthop Surg. 2004;12:12-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 180] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 2. | Della Rocca GJ. Periprosthetic fractures about the knee - an overview. J Knee Surg. 2013;26:3-7. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Hou Z, Bowen TR, Irgit K, Strohecker K, Matzko ME, Widmaier J, Smith WR. Locked plating of periprosthetic femur fractures above total knee arthroplasty. J Orthop Trauma. 2012;26:427-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 64] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 4. | Nauth A, Ristevski B, Bégué T, Schemitsch EH. Periprosthetic distal femur fractures: current concepts. J Orthop Trauma. 2011;25 Suppl 2:S82-S85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 40] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 5. | Horneff JG 3rd, Scolaro JA, Jafari SM, Mirza A, Parvizi J, Mehta S. Intramedullary nailing vs locked plate for treating supracondylar periprosthetic femur fractures. Orthopedics. 2013;36:e561-e566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 45] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 6. | Liporace FA, Aneja A, Carroll EA, Yoon RS. Maintaining the Neutral Axis in the Treatment of Distal Femur Fractures Via Dual Plate or Nail Plate Combination Technique: When and How? J Orthop Trauma. 2021;35:S38-S40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 7. | Sun ZH, Liu YJ, Li H. Femoral stress and strain changes post-hip, -knee and -ipsilateral hip/knee arthroplasties: a finite element analysis. Orthop Surg. 2014;6:137-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 8. | Soininvaara TA, Miettinen HJ, Jurvelin JS, Suomalainen OT, Alhava EM, Kröger HP. Periprosthetic femoral bone loss after total knee arthroplasty: 1-year follow-up study of 69 patients. Knee. 2004;11:297-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 50] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 9. | Gondalia V, Choi DH, Lee SC, Nam CH, Hwang BH, Ahn HS, Ong AC, Park HY, Jung KA. Periprosthetic supracondylar femoral fractures following total knee arthroplasty: clinical comparison and related complications of the femur plate system and retrograde-inserted supracondylar nail. J Orthop Traumatol. 2014;15:201-207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 27] [Cited by in RCA: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 10. | Shin YS, Kim HJ, Lee DH. Similar outcomes of locking compression plating and retrograde intramedullary nailing for periprosthetic supracondylar femoral fractures following total knee arthroplasty: a meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2017;25:2921-2928. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 36] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Herrera DA, Kregor PJ, Cole PA, Levy BA, Jönsson A, Zlowodzki M. Treatment of acute distal femur fractures above a total knee arthroplasty: systematic review of 415 cases (1981-2006). Acta Orthop. 2008;79:22-27. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 171] [Cited by in RCA: 160] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 12. | Ristevski B, Nauth A, Williams DS, Hall JA, Whelan DB, Bhandari M, Schemitsch EH. Systematic review of the treatment of periprosthetic distal femur fractures. J Orthop Trauma. 2014;28:307-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 82] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 13. | Rhee SJ, Cho JY, Choi YY, Sawaguchi T, Suh JT. Femoral Periprosthetic Fractures after Total Knee Arthroplasty: New Surgically Oriented Classification with a Review of Current Treatments. Knee Surg Relat Res. 2018;30:284-292. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 14. | Ebraheim NA, Kelley LH, Liu X, Thomas IS, Steiner RB, Liu J. Periprosthetic Distal Femur Fracture after Total Knee Arthroplasty: A Systematic Review. Orthop Surg. 2015;7:297-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 87] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 15. | Li B, Gao P, Qiu G, Li T. Locked plate vs retrograde intramedullary nail for periprosthetic femur fractures above total knee arthroplasty: a meta-analysis. Int Orthop. 2016;40:1689-1695. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 16. | Thukral R, Marya S, Singh C. Management of distal femoral periprosthetic fractures by distal femoral locking plate: A retrospective study. Indian J Orthop. 2015;49:199-207. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 17] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 17. | Ruchholtz S, Tomás J, Gebhard F, Larsen MS. Periprosthetic fractures around the knee-the best way of treatment. Eur Orthop Traumatol. 2013;4:93-102. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 49] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 18. | Shah JK, Szukics P, Gianakos AL, Liporace FA, Yoon RS. Equivalent union rates between intramedullary nail and locked plate fixation for distal femur periprosthetic fractures - a systematic review. Injury. 2020;51:1062-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 30] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 19. | Mäkinen TJ, Dhotar HS, Fichman SG, Gunton MJ, Woodside M, Safir O, Backstein D, Willett TL, Kuzyk PR. Periprosthetic supracondylar femoral fractures following knee arthroplasty: a biomechanical comparison of four methods of fixation. Int Orthop. 2015;39:1737-1742. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 31] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 20. | Matlovich NF, Lanting BA, Vasarhelyi EM, Naudie DD, McCalden RW, Howard JL. Outcomes of Surgical Management of Supracondylar Periprosthetic Femur Fractures. J Arthroplasty. 2017;32:189-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 21. | Quinzi DA, Ramirez G, Kaplan NB, Myers TG, Thirukumaran CP, Ricciardi BF. Early complications and reoperation rates are similar amongst open reduction internal fixation, intramedullary nail, and distal femoral replacement for periprosthetic distal femur fractures: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2021;141:997-1006. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 29] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 22. | Kyriakidis T, Kenanidis E, Akula MR, Zorman D, Tsiridis E. Locking plates vs retrograde intramedullary nails in the treatment of periprosthetic supracondylar knee fractures. A retrospective multicenter comparative study. Injury. 2019;50:1745-1749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 17] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 23. | Kanabur P, Sandilands SM, Whitmer KK, Owen TM, Coniglione FM, Shuler TE. Nail and Locking Plate for Periprosthetic Fractures. J Orthop Trauma. 2017;31:e425-e431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 24. | Hussain MS, Dailey SK, Avilucea FR. Stable Fixation and Immediate Weight-Bearing After Combined Retrograde Intramedullary Nailing and Open Reduction Internal Fixation of Noncomminuted Distal Interprosthetic Femur Fractures. J Orthop Trauma. 2018;32:e237-e240. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 46] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 25. | Attum B, Douleh D, Whiting PS, White-Dzuro GA, Dodd AC, Shen MS, Mir HR, Obremskey WT, Sethi MK. Outcomes of Distal Femur Nonunions Treated With a Combined Nail/Plate Construct and Autogenous Bone Grafting. J Orthop Trauma. 2017;31:e301-e304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 26. | Yoon RS, Patel JN, Liporace FA. Nail and Plate Combination Fixation for Periprosthetic and Interprosthetic Fractures. J Orthop Trauma. 2019;33 Suppl 6:S18-S20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 27. | Mirick Mueller GE. Nail-Plate Constructs for Periprosthetic Distal Femur Fractures. J Knee Surg. 2019;32:403-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 28. | Liporace FA, Yoon RS. Nail Plate Combination Technique for Native and Periprosthetic Distal Femur Fractures. J Orthop Trauma. 2019;33:e64-e68. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 95] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 29. | Garala K, Ramoutar D, Li J, Syed F, Arastu M, Ward J, Patil S. Distal femoral fractures: A comparison between single lateral plate fixation and a combined femoral nail and plate fixation. Injury. 2022;53:634-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 27] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 30. | Stoffel K, Sommer C, Lee M, Zhu TY, Schwieger K, Finkemeier C. Double fixation for complex distal femoral fractures. EFORT Open Rev. 2022;7:274-286. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 25] [Reference Citation Analysis (0)] |
| 31. | Chen SH, Tai CL, Yu TC, Wang CW, Lin CW, Chen CY, Liu KC. Modified fixations for distal femur fractures following total knee arthroplasty: a biomechanical and clinical relevance study. Knee Surg Sports Traumatol Arthrosc. 2016;24:3262-3271. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 32. | Başcı O, Karakaşlı A, Kumtepe E, Güran O, Havıtçıoğlu H. Combination of anatomical locking plate and retrograde intramedullary nail in distal femoral fractures: comparison of mechanical stability. Eklem Hastalik Cerrahisi. 2015;26:21-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |