Published online Nov 26, 2022. doi: 10.12998/wjcc.v10.i33.12278
Peer-review started: June 15, 2022
First decision: June 27, 2022
Revised: July 23, 2022
Accepted: October 12, 2022
Article in press: October 12, 2022
Published online: November 26, 2022
Processing time: 161 Days and 0.4 Hours
Adult patients presenting with Angle Class II division 1 malocclusions that have a strong skeletal etiology can be challenging for clinicians, particularly if accompanied by retrognathia of the mandible and a dolichofacial growth pattern.
In this case report, we describe the successful orthodontic and surgical mana
The patient’s facial esthetics was significantly improved and a desirable occlusion was achieved after 16 mo treatment. Follow-up records after 2 years showed stable esthetics and function.
Core Tip: In this case report, we describe a combined surgical/orthodontic diagnosis and treatment of an Angle Class II division 1 malocclusion with a severely retruded mandible and a vertical growth pattern and discuss the pros and cons of this approach. The patient’s chief concerns were her retrognathic mandible, difficulty with lip closure, and two missing maxillary first molars. These problems were satisfactorily relieved through comprehensive orthodontic treatment by closing the spaces of missing maxillary first molars through forward movement of the maxillary second molars and retracting the proclined mandibular incisors, and orthognathic surgery for maxillary impaction, mandibular advancement, and genioplasty. After the combined treatment, her retrognathic mandible was more forward, and the patient could close her lips effortlessly. And the genioplasty assisted in achieving a harmonious profile.
- Citation: Li GF, Zhang CX, Wen J, Huang ZW, Li H. Orthodontic-surgical treatment of an Angle Class II malocclusion patient with mandibular hypoplasia and missing maxillary first molars: A case report. World J Clin Cases 2022; 10(33): 12278-12288
- URL: https://www.wjgnet.com/2307-8960/full/v10/i33/12278.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i33.12278
Adult patients presenting with Angle Class II division 1 malocclusions that have a strong skeletal etiology can be challenging for clinicians, particularly if accompanied by retrognathia of the mandible and a dolichofacial growth pattern. As one of the important manifestations of Class II malocclusion, mandibular hypoplasia can result from many congenital deformities and secondary reasons, including trauma, infection, or bad habits during early childhood. Besides, condylar growth restriction resulting from arthritis, idiopathic condylar resorption (ICR), or condylar injury may also lead to mandibular hypoplasia. ICR is a disease which occurs almost completely in young women, which results in mandibular deficiencies, causing a shorter mandibular ramus and body, and a vertical growth pattern[1]. Besides different degrees of facial deformity, mandibular deficiencies can also damnify breathing and occlusal function[2].
For correcting Class II malocclusions manifesting as mandibular hypoplasia, many things such as the skeletal components and the patient’s demands should be considered before undertaking any treatment protocol. Mandibular distraction osteogenesis (MDO) is becoming an attractive treatment choice for young patients[3]. The gradual lengthening of the mandibula and surrounding soft tissue of MDO makes the relapse decrease compared with traditional orthognathic procedures[4]. However, for adult patients, secondary orthognathic surgery is usually needed after MDO because of the decreasing capacity for self-adaptation of the occlusal relationship. Furthermore, the disturbance to life and work of the devices of MDO is also a challenge for adults. Many adults prefer traditional orthognathic surgery to achieve their treatment goals. What’s more, for patients with mandibular hypoplasia resulting from ICR, the treatment is advised to operate when ICR no longer is active, and doctors should pay close attention to the position of the condyle during and post the treatment.
This case report describes a combined surgical/orthodontic treatment of an Angle Class II division 1 malocclusion with a severely retruded mandible and a vertical growth pattern and discusses the pros and cons of this approach.
This patient was a 20-year-old woman with an Angle Class II malocclusion and a severe vertical growth pattern with lip protrusion. Her chief concerns were her retrognathic mandible, difficulty with lip closure, and two missing maxillary first molars.
The patient underwent extraction of two maxillary first molars because of deep cavities 1 year ago.
The patient denied any family history of present illness.
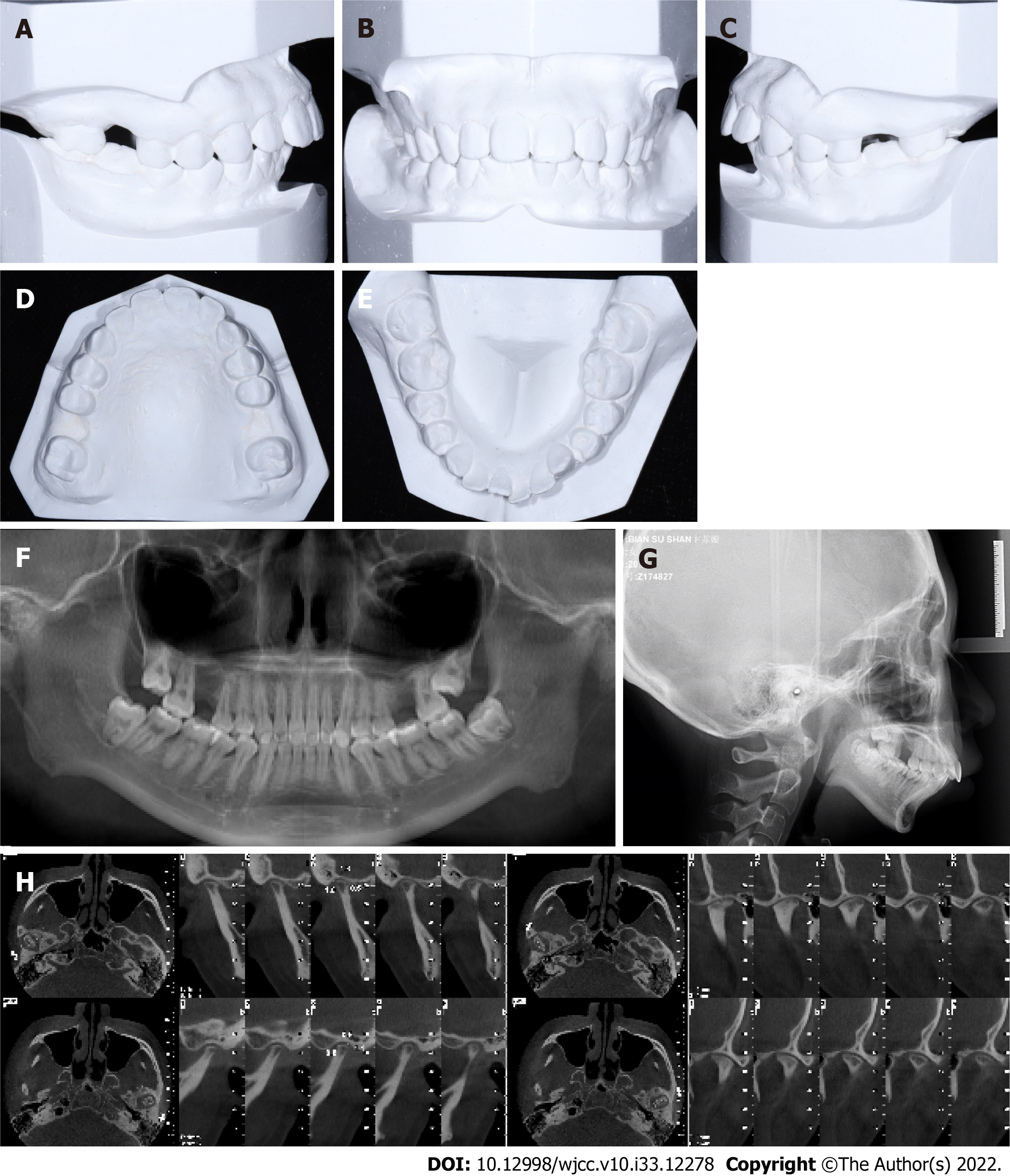
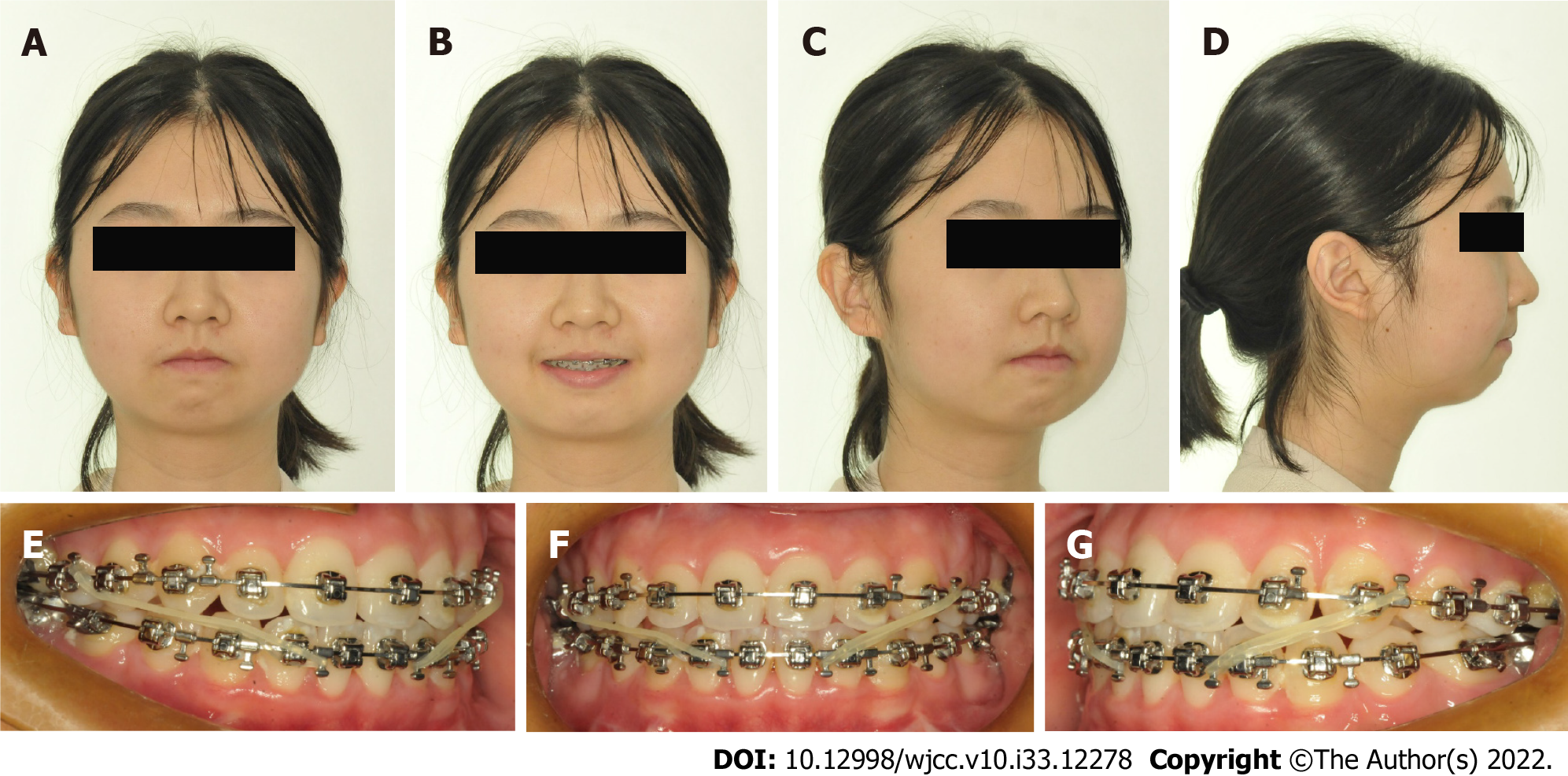
Pre-treatment facial photographs showed a symmetrical face, a severe convex profile, protrusion of upper and lower lips, and hyperactivity of the mentalis muscle. The oral examination showed an Angle Class II division 1 malocclusion with mandibular retrusion and two missing maxillary first molars (Figure 1). Model analysis showed 5 mm crowding in the lower arch, and a large overjet of 6 mm. No temporomandibular joint (TMJ) disorder symptoms or signs were observed in the clinical examination or the questionnaire survey. But there was TMJ click during her teenager.
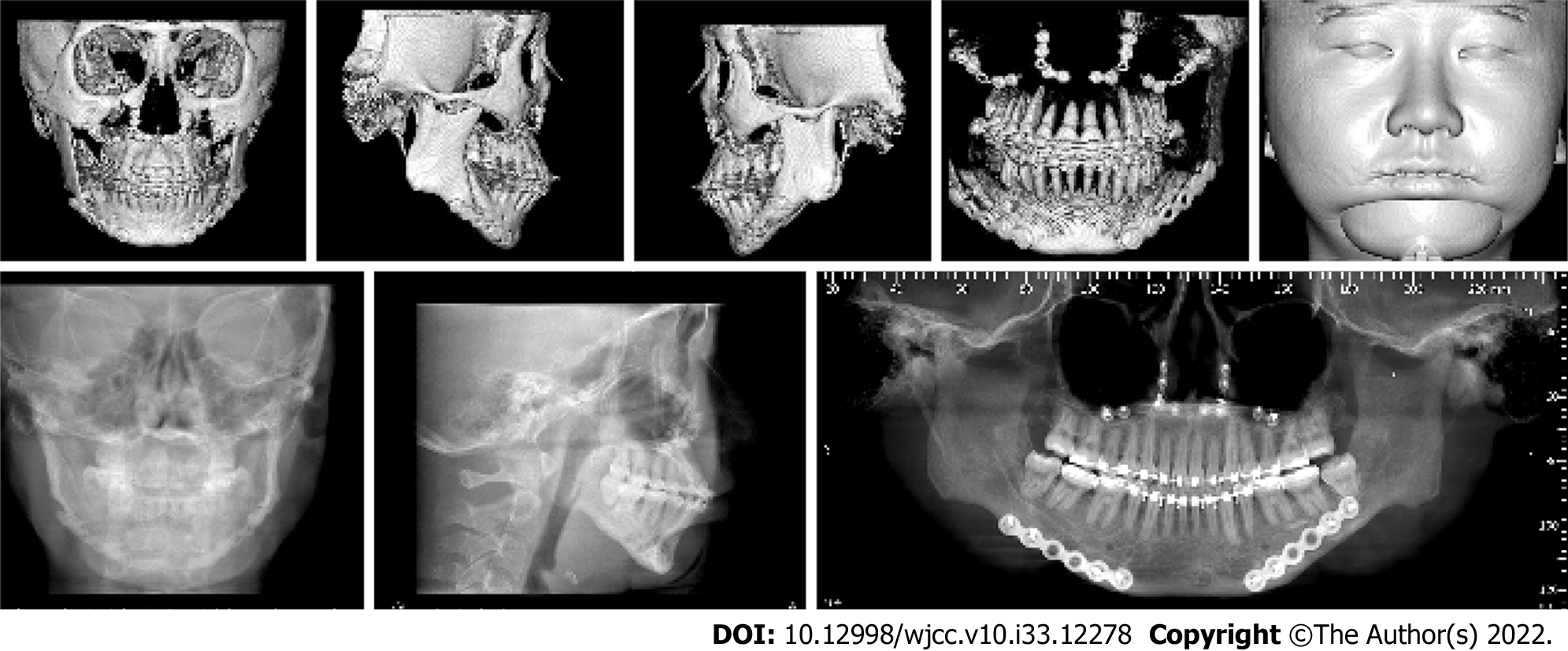
Cephalometric analysis presented a skeletal Class II malocclusion (SNA, 81.2; SNB, 70.2; ANB, 11), a high mandibular plane angle (MP-SN, 45), retroclined maxillary incisors (U1-SN, 97.2), and proclined mandibular incisors (L1-MP, 108.9) (Figure 2A-E; Table 1). Cone-beam computed tomography (CBCT) showed two missing maxillary first molars and four impacted third molars. There was erosion and flattening of the TMJ condyles bilaterally, and the joint spaces between the condyles and the glenoid fossae were small (Figure 2F-H).
| Group/measurement | Pre-treatment | Pre-surgery | Post-treatment | Norm | Std. Dev. |
| SNA (°) | 81.2 | 81.2 | 80.3 | 82 | 3.6 |
| SNB (°) | 71.2 | 70.5 | 76.9 | 80 | 3.2 |
| ANB (°) | 10.0 | 10.6 | 3.4 | 2 | 1.7 |
| MP-SN (°) | 46.2 | 49.3 | 40.4 | 33 | 4.2 |
| Interincisal angle (U1-L1) (°) | 107.7 | 114.4 | 131.0 | 131 | 8.5 |
| IMPA (L1-MP) (°) | 108.9 | 99.4 | 90.6 | 93 | 6.2 |
| U1-SN (°) | 97.2 | 96.9 | 98.0 | 101.4 | 6.0 |
| Occ plane to SN (°) | 30.0 | 29.1 | 22.4 | 14 | 3.9 |
| L1-NB (mm) | 11.0 | 9.2 | 6.1 | 4 | 2.0 |
| U1-NA (mm) | 3.0 | 2.2 | 3.8 | 4 | 2.3 |
| U1-NA (°) | 16.0 | 15.8 | 17.7 | 22 | 5.9 |
| L1-NB (°) | 46.3 | 39.2 | 27.9 | 25 | 5.6 |
| Pog-NB (mm) | -5.4 | -3.1 | 1.8 | -0.3 | 1.7 |
| Soft tissue convexity (°) | 118.7 | 119.7 | 132.9 | 143.3 | 4.0 |
| Lower lip to e-plane (mm) | 13.0 | 11.8 | -3.7 | -2 | 2.2 |
| Upper lip to e-plane (mm) | 8.7 | 8.3 | -4.0 | 3 | 1.9 |
Angle Class II division 1 malocclusion associated with mandibular hypoplasia and missing maxillary first molars.
The treatment goals included: (1) Obtaining a balanced facial profile; (2) obtaining aligned dental arches; (3) closing the spaces of both arches; (4) establishing ideal overjet and overbite; and (5) achieving a stable occlusion.
For this patient, a number of treatment alternatives were considered, including: (1) Camouflage orthodontic retraction of anterior teeth with temporary anchorage devices (TADs); (2) LeFort I osteotomy; (3) mandibular distraction osteogenesis (DO); (4) bilateral mandibular sagittal split osteotomy (BSSO); and (5) genioplasty.
The first alternative is a camouflage treatment. This choice could correct the occlusal relationship, but there would be little improvement of the retrognathic mandible. The patient and her family were keen to improve the profile, so this option was not considered.
Considering the extremely short mandible ramus and body, DO was recommended to the patient. This option was declined due to scar formation as well as its disturbance to life and work.
Overall, the suitable option for correcting the skeletal problem was traditional orthognathic surgery including a LeFort I osteotomy for maxillary impaction and rotation, a BSSO for mandibular advancement and rotation, and genioplasty for profile improvement. Considering the retroclinedmaxillary incisors, mesial second molars movement was suitable for closing the spaces of missing maxillary first molars, TADs or Class III elastics would be suitable for it. To retract the proclined mandibular incisors, extraction of the two mandibular first premolar teeth was indicated. After careful examination, 5 mm periodontal pocketing was detected around the two second premolar teeth, so the final decision was extracting the two mandibular second premolars. What’s more, we advised her to extract the impacted third molars, though there was no disturbance to orthodontic treatment. We informed the risk of orthognathic surgery to TMJs, and the patient gave informed consent.
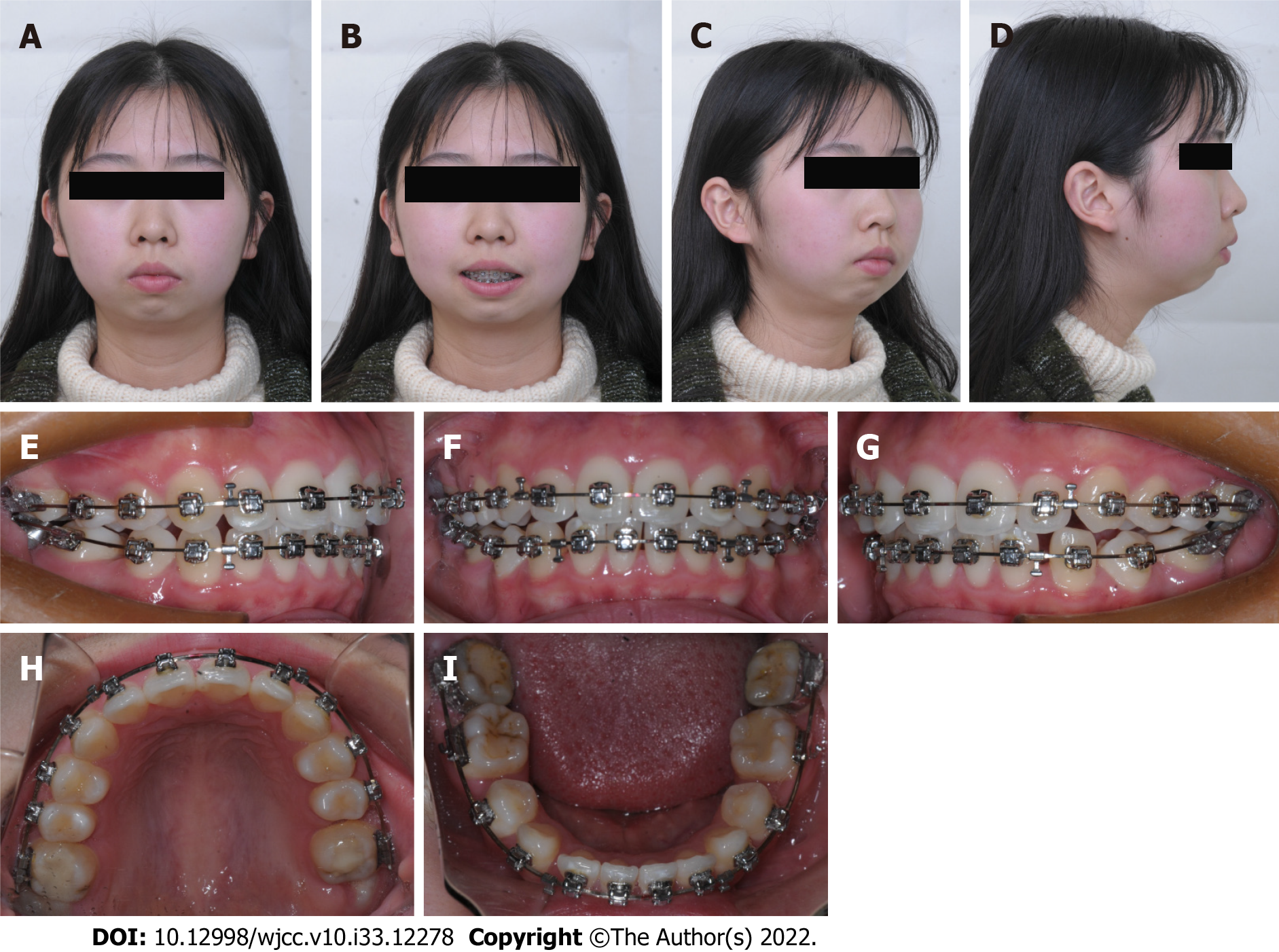
The total treatment included three stages. The initial one was pre-surgical orthodontic treatment over 8 mo. A self-ligating 0.022 × 0.028-inch slot appliance system (Damon Q, Ormco, Orange, California, United States) was used in both arches. Preoperative dental alignment and leveling were achieved with sequential nickel-titanium arch wires. Then Class III elastics (1/8 inch, 3.5 oz; Ormco) was used for maxillary second molars mesialization and mandibular incisors retraction with 0.018 × 0.025-inch stainless steel archwires in both arches. To control the anterior dental torque, a reverse curve of Spee in maxillary arch 0.018 × 0.025-inch stainless steel wire was used during the space-closing procedure. After the torque of the mandibular incisors returned to normal, power chain elastics was used to close the remaining space (Figures 3-5).
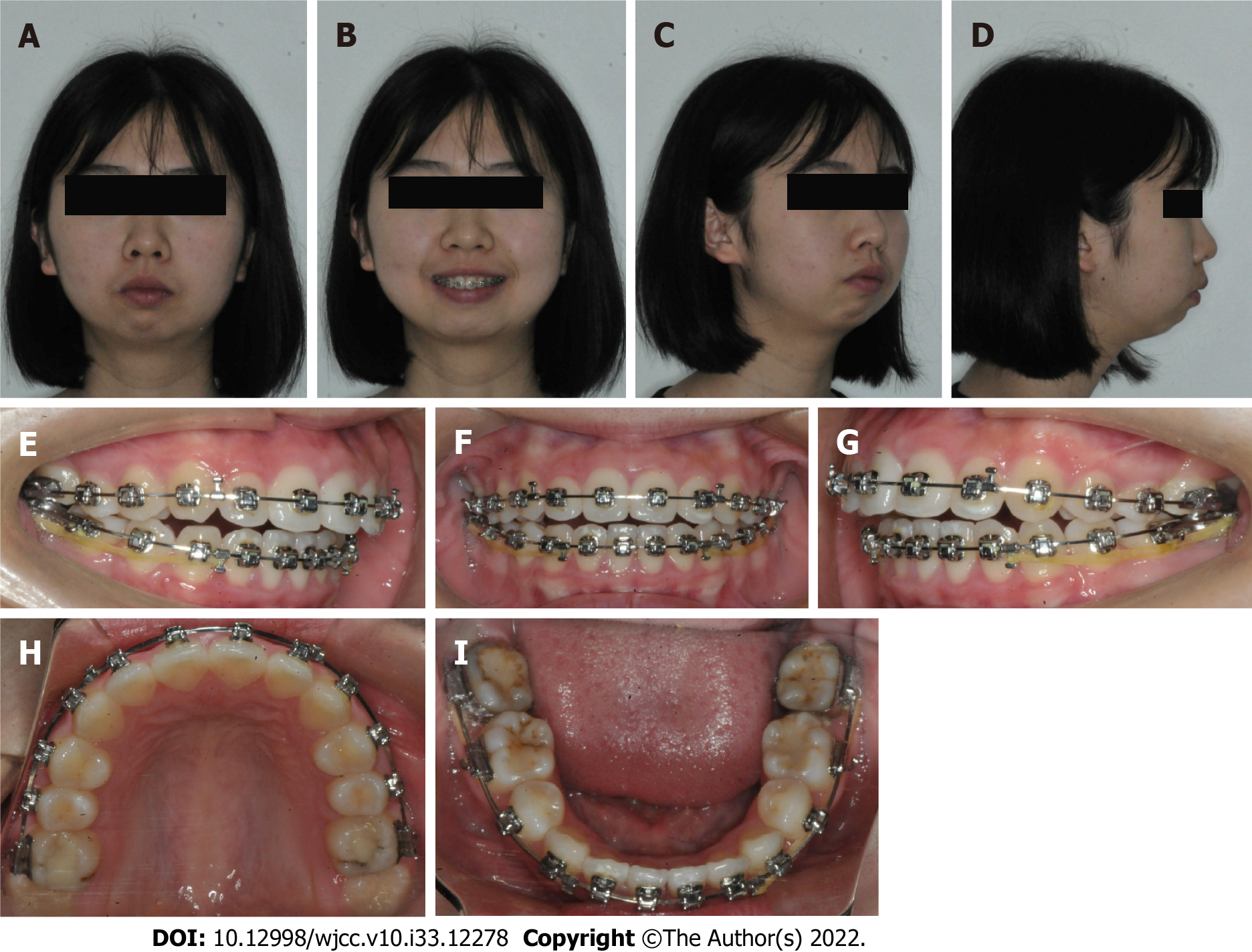
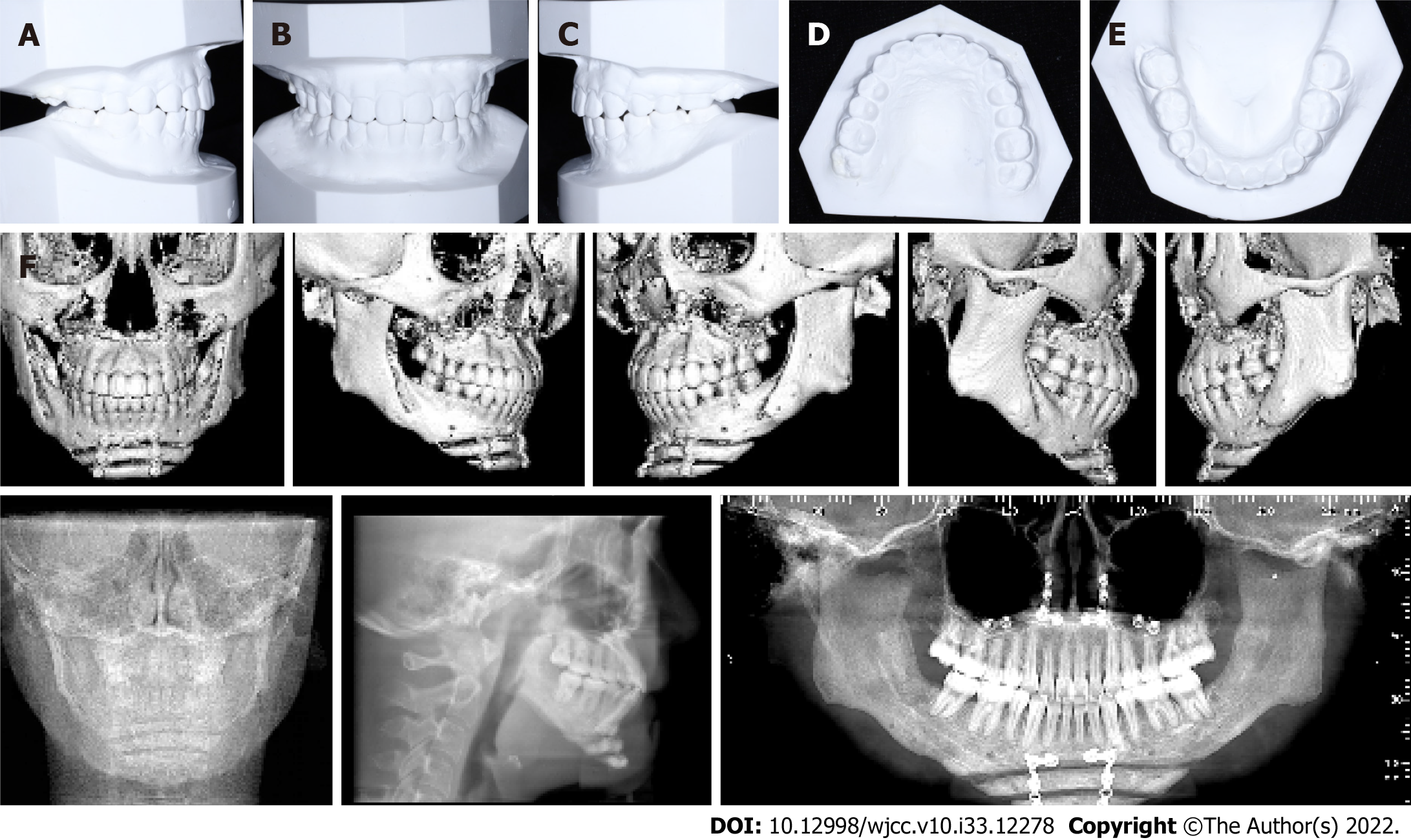
Following pre-surgical alignment, the second stage of orthognathic surgery was operated to resolve the skeletal deformity. The operation involved a LeFort I osteotomy for maxillary impaction (3 mm for the anterior sides) and retraction (3 mm), a BSSO for mandibular advancement (8 mm) and rotation, and a genioplasty (advancement of 12 mm) for chin reconstruction. However, after the LeFort I osteotomy and the BSSO, there was an acute massive hemorrhage when genioplasty was going to be performed. The surgeon decided to delay the genioplasty for her life safety. And an occlusal splint was used to fix the reestablished jaw relationship for 4 wk after surgery (Figures 6 and 7).
The post-surgery orthodontic therapy (the third treatment stage) lasted about 6 mo until an optimal occlusion was established. Asymmetric elastics (3/16 inch, 3.5 oz; Ormco) were immediately used after the orthgnathic surgery for a short period to coordinate the midline of upper jaw and lower jaw and prevent the skelatal relapse. During the postoperative orthodontic therapy, the genioplasty (advance
The total active treatment lasted about 16 mo. After debonding the fixed appliances, vacuum-formed retainers were used for retention. The patient was asked to wear them full time for 1 year and at night for the next 2 years. The patient was reviewed at 2 years into retention.
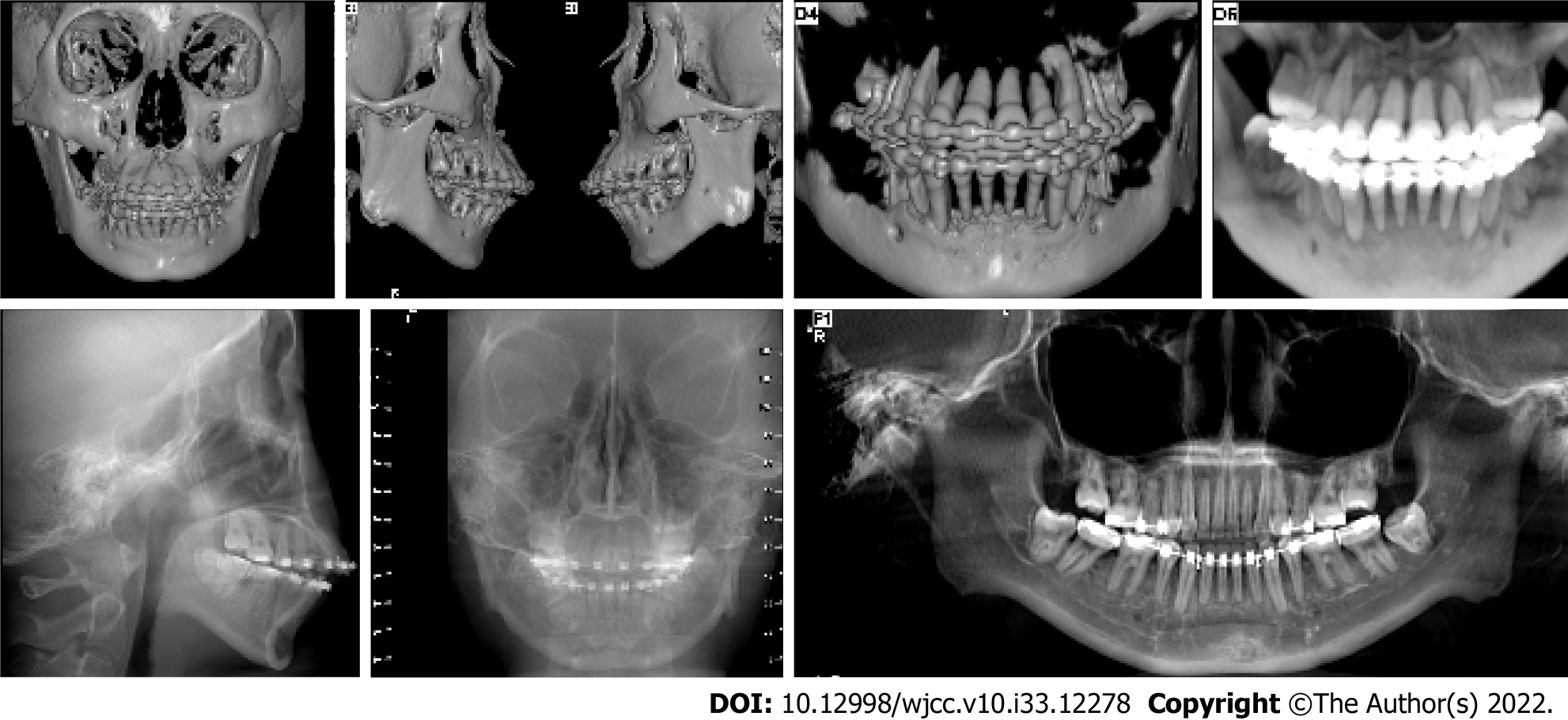
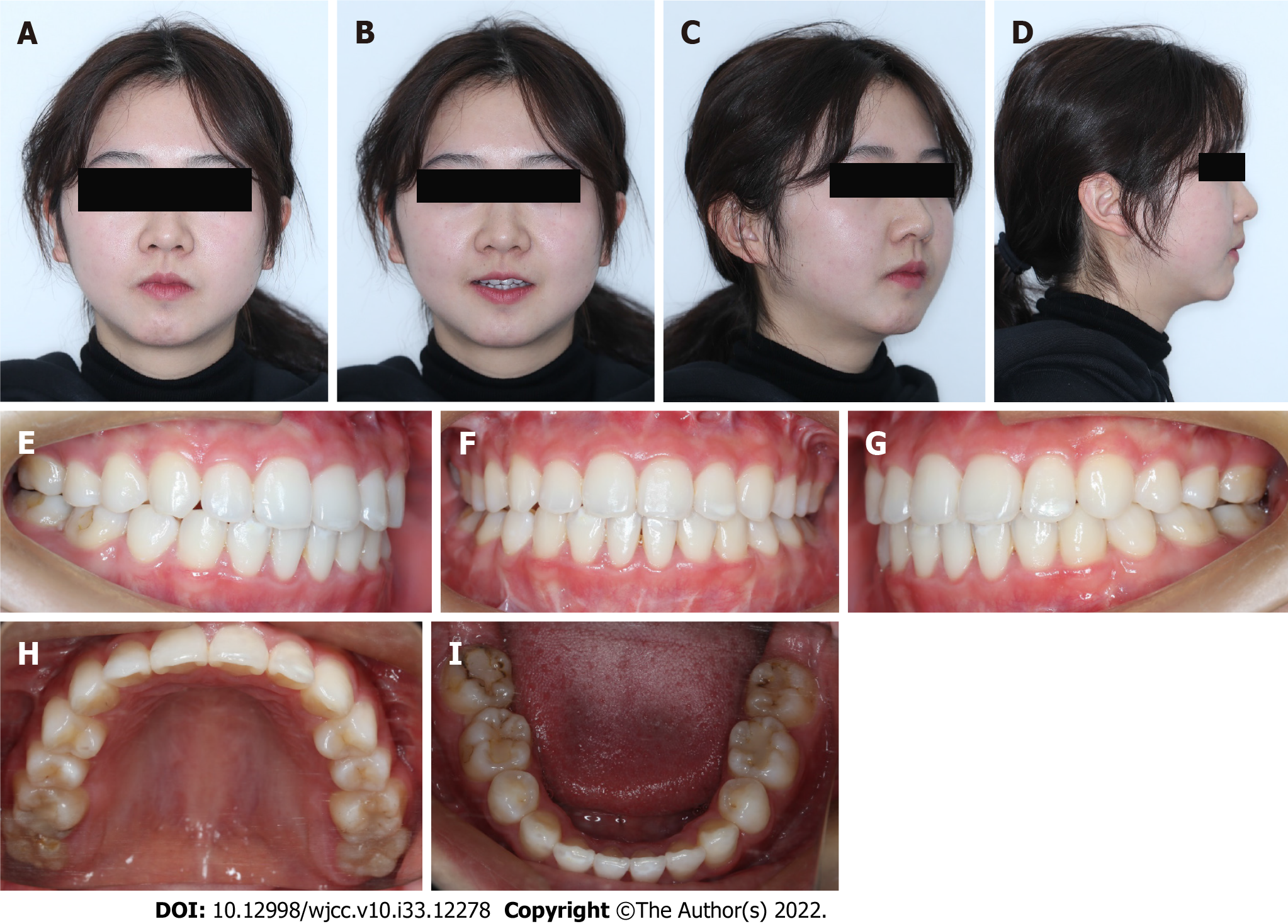
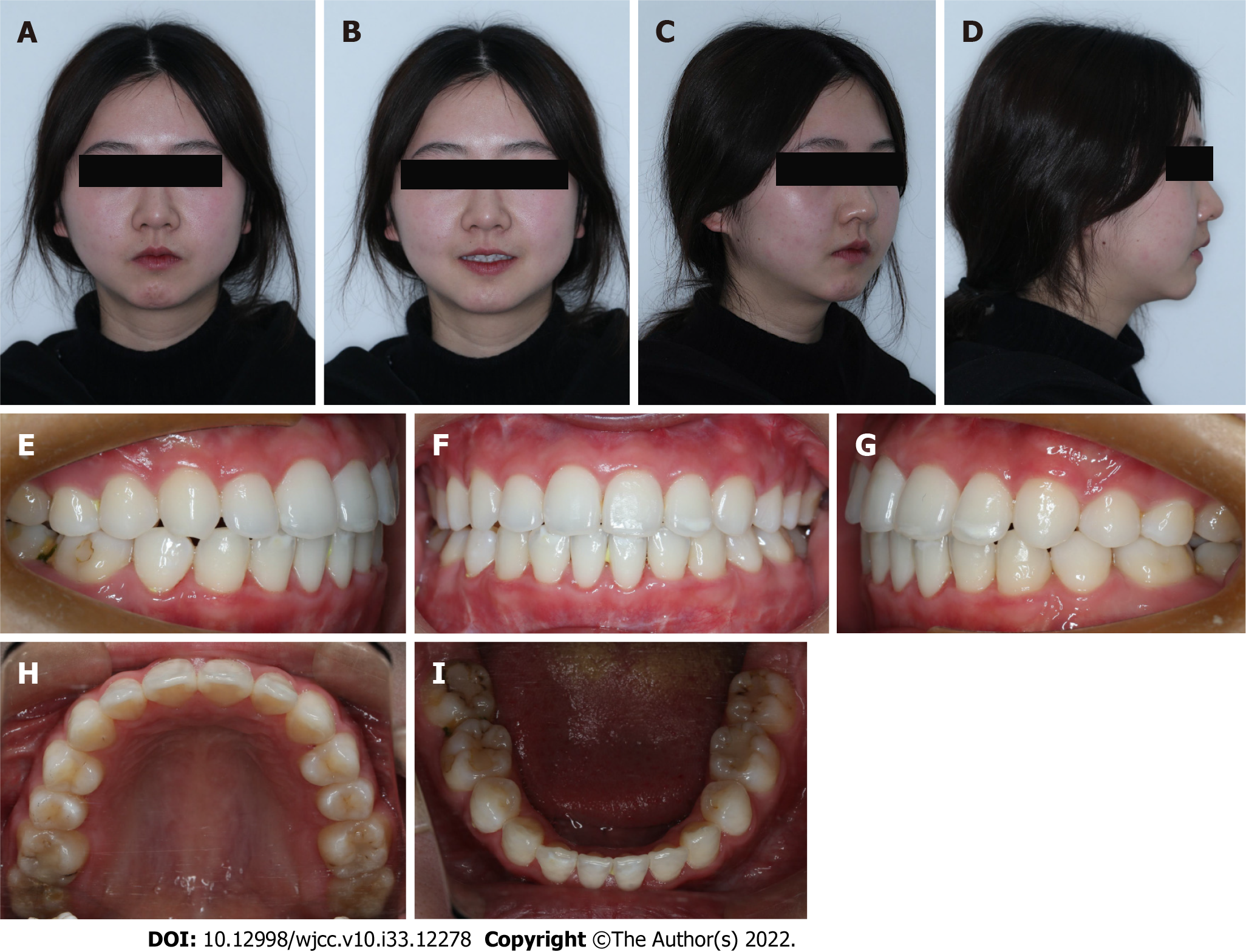
The patient’s orthodontic problems were remarkably improved. A pleasant and harmonious profile was established. Intraorally, both arches were well-coordinated and ovoid-shaped. An interdigitated occlusion with Class I canine and full class III molar relationships, and an optimal overbite and overjet was obtained (Figure 8).
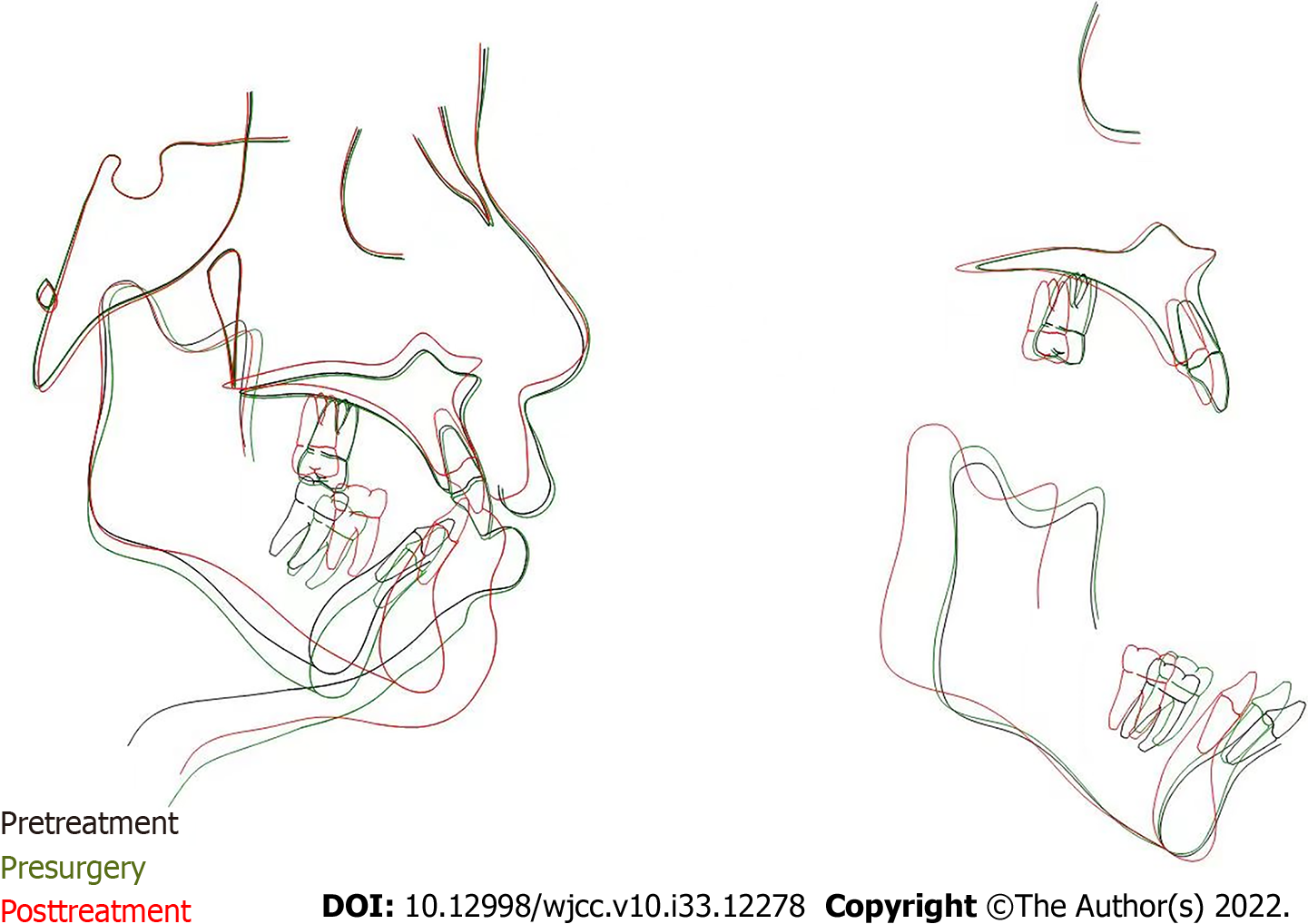
Post-treatment CBCT showed that all tooth roots were parallel to each other, and there was no significant root resorption or bone loss. The TMJs showed no morphologic change compared with the pre-treatment images. Cephalometric analysis presented a decrease of the ANB angle (11.0˚ to 1.9˚), a procline of maxillary incisors (U1-SN˚: 97.2˚ to 99.4˚), and a retrocline of the mandibular incisors (L1-NB˚: 45.3˚ to 30.6˚). An advancement of the mandible, a setback of the maxilla, and a counterclockwise mandibular rotation (SN-GoGn˚: 44.0˚ to 39.2˚) were shown on the superimposition of pre- and post-treatment lateral cephalograms (Figures 9 and 10).
After 2 years of retention, the post-treatment occlusion was stable. There was no skeletal or dental relapse, and both the patient and her families were satisfied with the results (Figure 11).
The patient’s chief concerns were her retrognathic mandible, difficulty with lip closure, and two maxillary missing molars. These problems were satisfactorily relieved through comprehensive orthodontic treatment by closing the spaces of missing upper first molars and retracting the proclined mandibular incisors, and orthognathic surgery for maxillary impaction, mandibular advancement, and genioplasty. After the combined treatment, her retrognathic mandible was more forward, and the patient could close her lips effortlessly. And the genioplasty assisted in achieving a harmonious profile.
Compared with traditional orthognathic surgery, DO has becoming an attractive alternative treatment for skeletal discrepancies in the craniofacial complex[5]. Doctors have used DO in both maxillary and mandibula in patients[5,6]. One advantage of DO is the relatively brief time in the operating room. However, the follow-up is extensive. Another interesting possible advantage is its minimum damage to the inferior alveolar nerve. It was reported that up to 10 mm of DO of the mandibula produced minimal effects on inferior alveolar nerve function compared with orthognathic surgery[7]. Furthermore, the stability of DO was much better in adult patients[8]. It has been reported that in patients with cleft lip and palate, the stability of DO was greater than LeFort I osteotomy for maxillary advancement[9,10]. And in the mandible, DO appears to be more stable than BSSO when movement greater than 7 mm is considered[11].
For this patient, she had an extremely short mandibular ramus and body with a decreased S-Go of 66 mm and decreased face height ratio of 60.1%. We recommended DO of the mandibular ramus and body as an alternative to improve her profile. Besides, she had an increased occlusal plane angle of 23°. Orthodontic treatment could be used to adjust the maxillary occlusal plane. And intrusion of upper incisors and extrusion of posterior teeth were common alternatives to flatten the steep occlusal plane. The amount of incisor intrusion varies between different researchers[12-15]. However, this patient did not show maxillary vertical excess or gummy smile, so excess incisor intrusion was not indicated. Molar extrusion was also contraindicated. The steep maxillary occlusal plane could not be adjusted by orthodontic treatment, and secondary orthognathic surgery after DO would be needed to adjust the occlusion. Considering the scar, protracted discomfort and disturbance to life and work, and secondary orthognathic surgery, she refused DO and chose the conventional, fast, and convenient orthognathic surgery-LeFort I osteotomy, BSSO, and genioplasty. And she and her families were satisfied with the results.
As a growth center, the mandibular condyle can affect the mandibular shape, size, and function and overall facial form secondarily. Conceptually, TMJ disabilities included undergrowth and overgrowth pattern. The undergrowth deformities such as ICR, juvenile idiopathic arthritis associated condylar growth restriction, traumatic condylar injury or posttraumatic TMJ hypomobility, and the resection of the condyle because of tumors in children may result in mandibular hypoplasia[16]. ICR is well-documented but poorly-understood, which predominantly affects young women, particularly during the pubertal growth spurt. It is characterized with a shorter mandibular condyloid process, ramus, and body, and an increase of facial vertical dimension resulting from bilateral and progressive volume loss of the TMJ condyles and mandibular rami. Although without standard guidelines for treatment of ICR by now, management of ICR should depend on the severity of condylar resorption and the activity of the disease. If ICR is inactive and there is a reliable centric relationship provided from enough condylar mass, routine orthognathic surgery can be operated; however, condylar/ramus reconstruction is required with active ICR[17].
For this patient, we have noticed the bone mass loss and the flattening of the condyle of TMJ from CBCT images, and the clinical characteristics meet the criteria for ICR. We have recommended her to take MRI images of the TMJ in other hospitals because the equipment was not available in ours. But she delayed it because she had no symptoms in the TMJ. There was a continuous white line of cortex on her two condyles of the TMJ, and we considered that the condylar resorption was at rest and ICR was inactive. It has been reported that conventional orthodontia and orthognathic surgery could be operated for the resultant deformity when the condylar resorption is quiescent[16]. We advised her to notice the symptoms of TMJ, and with any discomfort she should go and check.
The efficient and successful correction in this adult skeletal Angle Class II malocclusion patient with mandibular hypoplasia relied on a comprehensive diagnostic protocol and a rational treatment design. Moreover, the combination of bimaxillary orthognathic surgery and genioplasty facilitated the improvement of the facial esthetics. This case report highlights a multidisciplinary cooperation to correct a severe dentofacial deformity for a patient-centered outcome.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Dentistry, oral surgery and medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Lan TT, China; Suzuki EY, Thailand S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Zhao S
| 1. | Mercuri LG, Handelman CS. Idiopathic Condylar Resorption: What Should We Do? Oral Maxillofac Surg Clin North Am. 2020;32:105-116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Yin L, Tang X, Shi L, Yin H, Zhang Z. Mandibular distraction combined with orthognathic techniques for the correction of severe adult mandibular hypoplasia. J Craniofac Surg. 2014;25:1947-1952. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | McCarthy JG, Schreiber J, Karp N, Thorne CH, Grayson BH. Lengthening the human mandible by gradual distraction. Plast Reconstr Surg. 1992;89:1-8; discussion 9. [PubMed] |
| 4. | Vendittelli BL, Dec W, Warren SM, Garfinkle JS, Grayson BH, McCarthy JG. The importance of vector selection in preoperative planning of bilateral mandibular distraction. Plast Reconstr Surg. 2008;122:1144-1153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Molina F. Combined maxillary and mandibular distraction osteogenesis. Semin Orthod. 1999;5:41-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 6. | Figueroa AA, Polley JW. Management of severe cleft maxillary deficiency with distraction osteogenesis: procedure and results. Am J Orthod Dentofacial Orthop. 1999;115:1-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 145] [Cited by in RCA: 135] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 7. | Makarov MR, Harper RP, Cope JB, Samchukov ML. Evaluation of inferior alveolar nerve function during distraction osteogenesis in the dog. J Oral Maxillofac Surg. 1998;56:1417-23; discussion 1424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 49] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 8. | Batra P, Ryan FS, Witherow H, Calvert ML. Long term results of mandibular distraction. J Indian Soc Pedod Prev Dent. 2006;24:30-39. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Cheung LK, Chua HDP, Hägg MB. Cleft maxillary distraction vs orthognathic surgery: clinical morbidities and surgical relapse. Plast Reconstr Surg. 2006;118:996-1008. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 107] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 10. | Kloukos D, Fudalej P, Sequeira-Byron P, Katsaros C. Maxillary distraction osteogenesis vs orthognathic surgery for cleft lip and palate patients. Cochrane Database Syst Rev. 2016;9:CD010403. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 11. | Serafin B, Perciaccante VJ, Cunningham LL. Stability of orthognathic surgery and distraction osteogenesis: options and alternatives. Oral Maxillofac Surg Clin North Am. 2007;19:311-320, v. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | El Namrawy MM, Sharaby FE, Bushnak M. Intrusive Arch vs Miniscrew-Supported Intrusion for Deep Bite Correction. Open Access Maced J Med Sci. 2019;7:1841-1846. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Aras I, Tuncer AV. Comparison of anterior and posterior mini-implant-assisted maxillary incisor intrusion: Root resorption and treatment efficiency. Angle Orthod. 2016;86:746-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 14. | Deguchi T, Murakami T, Kuroda S, Yabuuchi T, Kamioka H, Takano-Yamamoto T. Comparison of the intrusion effects on the maxillary incisors between implant anchorage and J-hook headgear. Am J Orthod Dentofacial Orthop. 2008;133:654-660. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 15. | Jain RK, Kumar SP, Manjula WS. Comparison of intrusion effects on maxillary incisors among mini implant anchorage, j-hook headgear and utility arch. J Clin Diagn Res. 2014;8:ZC21-24. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 16. | Chouinard AF, Kaban LB, Peacock ZS. Acquired Abnormalities of the Temporomandibular Joint. Oral Maxillofac Surg Clin North Am. 2018;30:83-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 34] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 17. | Ji YD, Resnick CM, Peacock ZS. Idiopathic condylar resorption: A systematic review of etiology and management. Oral Surg Oral Med Oral Pathol Oral Radiol. 2020;130:632-639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 16] [Article Influence: 3.2] [Reference Citation Analysis (0)] |