Published online Nov 26, 2022. doi: 10.12998/wjcc.v10.i33.12221
Peer-review started: July 17, 2022
First decision: September 9, 2022
Revised: September 21, 2022
Accepted: October 31, 2022
Article in press: October 31, 2022
Published online: November 26, 2022
Processing time: 129 Days and 2.4 Hours
Increasing reports have demonstrated that recombinant human brain natriuretic peptide (rhBNP) can improve acute myocardial infarction (AMI) and heart failure. However, whether it can improve renal function and decrease the risk of contrast-induced nephropathy (CIN) in elderly AMI patients is still unclear.
To explore the effect of rhBNP on CIN in elderly AMI patients after percutaneous coronary intervention (PCI).
One hundred and thirty-one elderly AMI patients underwent PCI from January 2017 to July 2021. Patients were either given 1 mL of 0.9% normal saline/(kg/h) for 72 h after PCI (control group, n = 66) and or intravenous rhBNP [1.5 mg/kg followed by 0.0075 mg/(kg/min)] for 72 h (rhBNP treatment group, n = 65). Serum creatinine and cystatin C levels, creatinine clearance rate, and eGFR were measured at 24 h, 48 h, and 72 h after PCI. Research nurses collected data on hand
The creatinine clearance rate and eGFR were increased, while the creatinine and cystatin C levels were decreased significantly in the rhBNP treatment group compared to the control group at 48 h and 72 h. The incidence of CIN (P = 0.028) and acute heart failure (P = 0.017) also significantly decreased in the rhBNP group. No significant difference was noted between the two groups in cardiac death and recurrent AMI.
Early application of rhBNP could protect renal function and decrease the incidence of CIN after primary PCI and acute heart failure.
Core Tip: Increasing evidence indicates that emergency percutaneous coronary intervention (PCI) is the most effective method for the treatment of acute myocardial infarction (AMI). However, with the increase of emergency PCI, contrast-induced nephropathy (CIN) is becoming more and more common, which also leads to the increase of the proportion of patients with renal dysfunction, aggravating the cost of hospitalization and prolonging the length of hospital stay. CIN cannot be managed or prevented with current medications. Recombinant human B-type natriuretic peptide (rhBNP) is the natriuretic peptide receptor A, and increasing reports have demonstrated that rhBNP can improve AMI and heart failure. However, whe
- Citation: Zhang YJ, Yin L, Li J. Protective effect of recombinant human brain natriuretic peptide against contrast-induced nephropathy in elderly acute myocardial infarction patients: A randomized controlled trial. World J Clin Cases 2022; 10(33): 12221-12229
- URL: https://www.wjgnet.com/2307-8960/full/v10/i33/12221.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i33.12221
There are more than a billion people worldwide who die from cardiovascular diseases every year, and most of these cases are attributable to ischemic heart diseases[1]. Increasing evidence indicates that percutaneous coronary intervention (PCI) and coronary artery bypass grafting has replaced drug therapies and become the most important and effective treatment for acute myocardial infarction (AMI)[2,3]. Now, increasing studies have reported that PCI has become the best and preferred treatment option for AMI, saving many lives. With the popularization of PCI technology and more patients undergoing PCI operation, there has been an increase in the cases of contrast-induced nephropathy (CIN), which is one of the major reasons for iatrogenic renal failure, increasing the risk of death during hospitalization, hospitalization expenses, and hospital stays[4-6]. Since there are many side effects of drug therapy in elderly patients with cardiovascular diseases in China, PCI is more often used, thus leading to a higher incidence CIN. Sun et al[7] found that the overall incidence of CIN was 8.38% after PCI. Moreover, CIN increases hospitalization expenses and hospital stays and is an important predictor of unfavorable early and long-term outcomes[8-10]. Hydration therapy effectively prevents CIN, but its efficacy is inadequate and can aggravate strain on the heart[11]. CIN cannot be managed or prevented by current medications.
Recombinant human B-type natriuretic peptide (rhBNP) is the natriuretic peptide receptor A, which can decrease the preload, afterload, and pulmonary capillary wedge pressure. It also can increase cardiac output, urinary output, and glomerular filtration rate, restrain the renin-angiotensin-aldosterone system, and improve diastolic function[12,13]. Multiple reports have demonstrated that rhBNP can improve AMI and heart failure[14-16]. However, whether it can improve renal function and decrease the risk of CIN in elderly AMI patients is still unclear. Therefore, we explored the effectiveness of rhBNP treatment for postoperative CIN in elderly AMI patients.
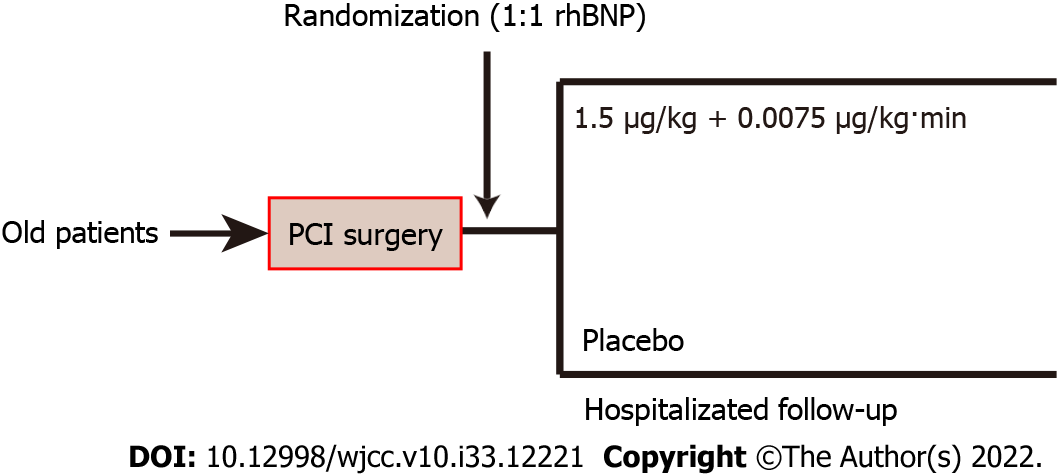
From January 2017 to July 2021, a prospective randomized controlled clinical trial was conducted with 131 elderly patients. This study evaluated the value of rhBNP intervention in postoperative CIN in elderly AMI patients. The study protocol was approved by the Wuxi Taihu Hospital Clinical Research Ethics Committees (2016-YXLL-051). Patients were randomly assigned (1:1) to receive either intravenous rhBNP (1.5 mg/kg, followed by 0.0075 mg/(kg/min)) for 72 h or 1 mL of 0.9% normal saline/(kg/h) for 72 h after PCI (Figure 1)[12,13]. Written informed consent was obtained from the patients or family members. Three days after PCI, the final follow-up was performed.
Eligible patients were diagnosed with acute ST-segment elevation AMI and received PCI. The inclusion criteria were: (1) Age > 60 years; (2) patients who can be randomized and received either rhBNP or placebo within 72 h after PCI; (3) the electrocardiogram was consistent with the characteristics of AMI; and (4) from the onset of chest pain to less than 12 h after operation, the serum creatine kinase isoenzyme was more than two times the normal value or troponin I was significantly increased. The exclusion criteria were: (1) Patients who were critically ill or close to death on admission; (2) patients with cardiomyopathies, pericarditis, primary pulmonary hypertension, and severe valvular heart disease; (3) patients diagnosed with connective tissue disease or autoimmune tissue disease; (4) AMI with other complications; and (5) allergy to contrast agent and/or rhBNP.
Permuted-block randomization was performed using SPSS (version 19.0, SPSS Institute) with an allocation list generated with random numbers (in a 1:1 ratio). An independent statistician conducted this analysis to ensure blinding and study integrity. To keep track of the results of randomization, sequentially numbered envelopes were sealed at the investigation site and stored until the study was finished. The research drugs were administered by a research nurse in accordance with the sequence of randomization. All patients and study members were blinded to the study medication allocation. It is possible to request the unmasking of the treatment allocation in emergency situations, such as a severe hepatic failure, and, if necessary to adjust or stop the study drug in case of an emergency. A thorough documentation of all events took place, including the demographics of the patients, their medical history, and any relevant investigation results.
In the pilot preliminary experiment study and previous clinical data, 72 h creatinine clearance rate in the placebo and rhBNP treatment groups were 1.12 ± 0.31 and 1.20 ± 0.38, respectively. The sample size was calculated to be 126 patients (63 in each category) according to the alpha of 0.05 and the statistical power of 80%. We decided to enroll 130 patients (65 in each category). The study database included all baselines and outcome data was entered by a study nurse.
As soon as the patients were admitted to the cardiology intensive care unit (CICU), they were assessed by two CICU physicians, and all clinical data were recorded. Routine admission examinations included electrocardiograms, chest radiographs, blood chemistry, arterial blood gas, serum electrolyte levels, and clotting function. All patients received similar treatment after a definitive diagnosis was achieved, including 0.3 g aspirin, 180 mg ticagrelor, 40 mg atorvastatin, and 20 mg rabeprazole sodium enteric-coated tablets. Patients were transferred to the interventional operating room, and the Judkins method was used to perform coronary angiography by puncturing radial or femoral arteries. Intraoperatively, the isotonic contrast agent iodixanol was used, and PCI was performed according to the characteristics of the lesions (balloon dilation or stent implantation). Coronary angiography was performed after PCI to check if TIMI grade 3 blood flow was restored and the patient’s chest pain was significantly relieved. After PCI, all patients received dual antiplatelet therapy, lipid regulation, ACEI/ARB, β-receptor blockers, and anticoagulators. Additionally, the rhBNP group received intravenous rhBNP [1.5 mg/kg, followed by 0.0075 mg/(kg/min)] for 72 h, whereas the control group received 1 mL of 0.9% normal saline/ (kg/h) for 72 h after PCI. All patients’ blood pressure was maintained at 120-140 mmHg during the study period, and urapidil was injected if necessary. At the same time, a balance of liquid was maintained in elderly AMI patients with an intravenous infusion of frontal fluid of approximately 1000 mL and an appropriate increase in oral rehydration solution after PCI.
All patients’ clinical and imaging data were collected and evaluated by an independent, masked diagnostic and assessment two-person committee. The two-person committee was comprised of researchers who had been trained before the study and were not associated with the patients’ management. The primary outcome was renal function at 72 h, and the secondary outcomes were the incidence of CIN, acute heart failure, and complications. All patients’ serum samples were collected before the operation and at 24 h, 48 h, and 72 h after PCI. The Cockcroft-Gault formula (Creatinine clearance rate = ([140-Age (years)] × Weight (kg))/(7.2 × SCr (mg/dL)) × 0.85 (if female)) was used to calculate the creatinine clearance rate, and the MDRD formula (Estimated glomerular filtration rate (eGFR) = 186 × (SCr)-1.154 × Age-0.203 × 0.742 (if female)) was used to calculate the eGFR. Creatinine clearance rate and eGFR made the diagnosis more accurate as some impaired renal function patients can have normal creatinine clearance. Left ventricular ejection fraction (LVEF) was detected by cardiac color ultrasound. Major adverse cardiovascular events and CIN were monitored.
All continuous variables are presented as the mean ± SD. SPSS 19.0 statistical software was used for the statistical analyses. Measurement data with a non-normal distribution are represented as the median (Q1, Q3). Independent-samples t-tests were used to assess for quantitative data. Qualitative data were compared by the chi square test or Fisher’s exact t-test. P < 0.05 was considered statistically significant.
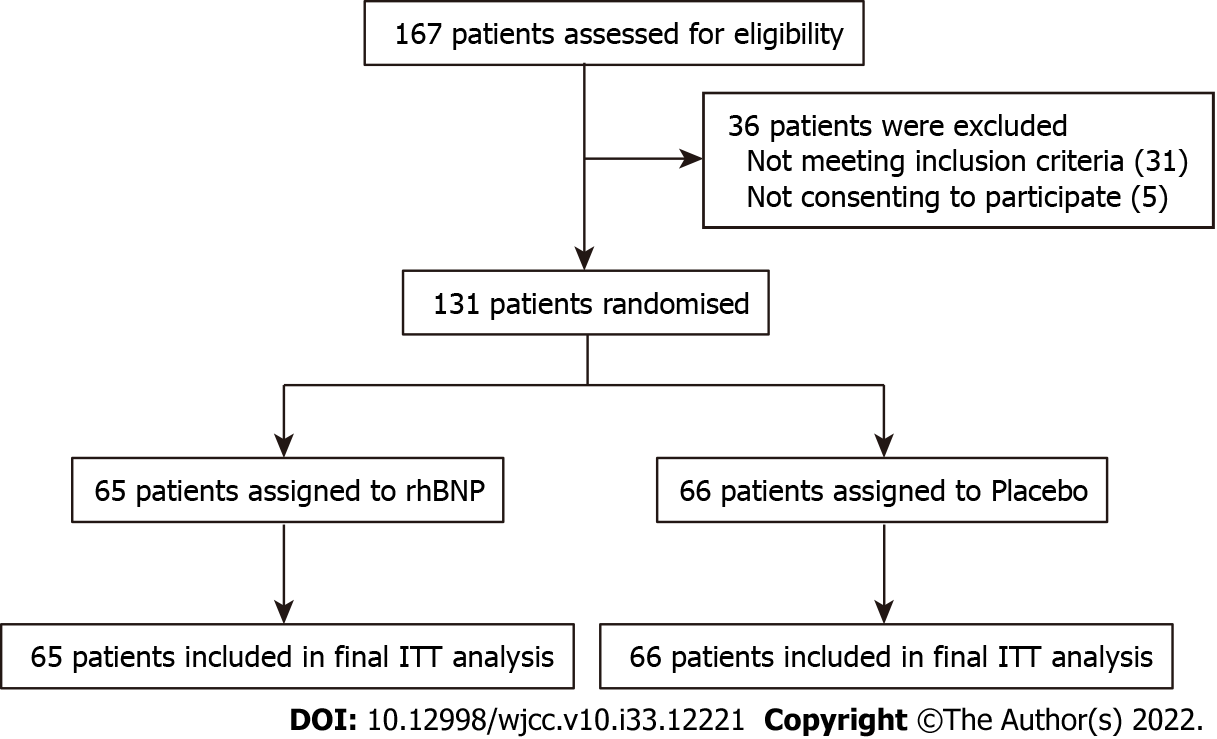
A total of 167 elderly patients were assessed from January 2017 to July 2021, and 36 were excluded according to the exclusion criteria. One hundred and thirty-one patients were randomly assigned to receive either rhBNP (n = 65) treatment or placebo (n = 66) treatment. The baseline data of the two groups were compared, and no significant difference was found (Table 1). No patients were lost to follow-up at the end, the final visit of the last randomized patient occurred on December 15, 2021, and 131 patients were included in the final analyses (Figure 2).
| Placebo group | rhBNP group | P value | |
| Age (mean ± SD) | 75.42 ± 12.88 | 75.58 ± 12.69 | 0.943 |
| Male | 49 (74.2) | 43 (66.2) | 0.311 |
| Hypertension | 36 (54.5) | 32 (49.2) | 0.543 |
| Diabetes | 7 (10.6) | 8 (12.3) | 0.760 |
| Hyperlipemia | 46 (69.7) | 43 (66.2) | 0.664 |
| Smoking | 18 (27.3) | 15 (23.1) | 0.580 |
| Killip score (mean ± SD) | 2.15 ± 0.52 | 2.09 ± 0.49 | 0.498 |
| B natriuretic peptide [median (Q1, Q3)] | 69 (18384) | 78 (35621) | 0.752 |
| Troponin I (ng/L, mean ± SD) | 55.18 ± 10.22 | 53.29 ± 11.08 | 0.312 |
| Treatment | 0.635 | ||
| Coronary arteriography | 9 (13.6) | 11 (16.9) | 0.759 |
| PCI | 57 (86.4) | 54 (83.1) | 0.787 |
| Lesion location | |||
| Left main | 7 (10.6) | 5 (7.7) | 0.563 |
| Left anterior descending branch | 30 (45.5) | 34 (52.3) | 0.433 |
| Left circumflex branch | 12 (18.2) | 9 (13.8) | 0.499 |
| Right coronary artery | 17 (25.7) | 17 (26.2) | 0.959 |
| LVEF (%, mean ± SD) | 59.47 ± 3.29 | 60.16 ± 3.15 | 0.223 |
| Contrast agent dosage [mL, median (Q1, Q3)] | 135 (60175) | 130 (70160) | 0.912 |
| Intro-operative IABP | 7 (10.6) | 8 (12.3) | 0.760 |
| Hospitalized | |||
| ACEI/ARB | 35 (53.0) | 32 (48.5) | 0.664 |
| Receptor antagonist | 52 (78.8) | 56 (86.2) | 0.268 |
| Calcium channel blocker | 29 (43.9) | 27 (41.5) | 0.781 |
| Natriuretic agent | 22 (33.3) | 25 (38.5) | 0.541 |
After primary PCI, the serum creatinine and cystatin C levels were elevated significantly (P < 0.05). Compared to the preoperative levels, the postoperative creatinine clearance rate and eGFR were reduced significantly (P < 0.05). Moreover, compared to the placebo group at 48 h and 72 h after primary PCI, the serum creatinine and cystatin C levels were reduced significantly (P < 0.05) in the rhBNP treatment group, and the creatinine clearance rate and eGFR levels were elevated significantly in the rhBNP group (P < 0.01, Table 2).
| Placebo | rhBNP | P value | |
| Serum creatinine (mol/L) | |||
| Preoperative | 72.35 ± 15.38 | 74.13 ± 16.28 | 0.521 |
| 24 h | 85.74 ± 19.21 | 83.26 ± 18.12 | 0.449 |
| 48 h | 101.55 ± 21.22 | 80.59 ± 19.46 | 0.001 |
| 72 h | 88.15 ± 18.72 | 76.29 ± 16.55 | 0.007 |
| Cystatin C (mg/L) | |||
| Preoperative | 0.91 ± 0.22 | 0.93 ± 0.21 | 0.596 |
| 24 h | 0.95 ± 0.25 | 0.96 ± 0.31 | 0.839 |
| 48 h | 1.07 ± 0.37 | 0.93 ± 0.32 | 0.020 |
| 72 h | 1.02 ± 0.30 | 0.88 ± 0.25 | 0.004 |
| Creatinine clearance rate (mL/min) | |||
| Preoperative | 1.12 ± 0.31 | 1.15 ± 0.38 | 0.621 |
| 24 h | 0.95 ± 0.32 | 1.03 ± 0.34 | 0.168 |
| 48 h | 0.82 ± 0.29 | 0.95 ± 0.28 | 0.010 |
| 72 h | 0.86 ± 0.25 | 1.05 ± 0.37 | 0.001 |
| eGFR [mL/(min/1.73 m2)] | |||
| Preoperative | 85.76 ± 22.46 | 86.35 ± 21.27 | 0.877 |
| 24 h | 78.43 ± 9.12 | 82.11 ± 10.23 | 0.030 |
| 48 h | 76.82 ± 8.55 | 83.27 ± 10.13 | 0.001 |
| 72 h | 77.432 ± 5.120 | 85.38 ± 7.22 | 0.001 |
We found that the incidence of CIN (P = 0.017) and acute heart failure (P = 0.028) in the rhBNP group was significantly lower than that of the placebo group after primary PCI (Table 3). We also evaluated the complications after PCI and did not find any significant difference in cardiogenic death and recurrent myocardial infarction during hospitalization (P > 0.05, Table 3).
| Placebo | rhBNP | P value | |
| Cardiogenic death | 6 (9.1) | 5 (7.7) | 0.773 |
| Recurrent myocardial infarction | 3 (4.5) | 3 (1.5) | 1.000 |
| Acute heart failure | 15 (22.7) | 5 (7.7) | 0.017 |
| CIN | 14 (21.2) | 5 (9.2) | 0.028 |
The condition of AMI is critical in most patients and requires coronary angiography and opening of the diseased vessels as soon as possible. Hence, almost all patients fail to undergo preoperative hydration therapy, leading to the utilization of more contrast agents during PCI, especially in complex lesions. This results in a high incidence of postoperative contrast agent nephropathy, which severely affects the prognosis of the patients[17]. A recent study reported that CIN was the third most common reason for hospital-acquired renal failure, and 49% of CIN cases occurred after cardiac catheterization and coronary angioplasty[18]. Although renal replacement therapy is rarely required for CIN patients, it increased the incidence of acute heart failure and stent thrombosis in the short-term and long-term follow-up compared to patients without CIN. Therefore, they risk lengthy hospital stays, hospitalization costs, and other hazards[19].
The exact reason for CIN is unclear and might be related to hemodynamic changes, renal vasoconstriction resulting in medullary hypoxemia, direct toxicity of renal tubular epithelial cells, and oxygen-free radical injury[20]. However, common renal ischemia induced by decreased renal blood flow and increased direct tubular toxicity mediated by oxygen free radicals and large amounts of iodine contrast agents is considered a significant reason for CIN. The potential mechanisms of pathological changes include contrast agent-induced sodium and diuretic drainage, and activation of tubule-glomerular feedback, resulting in glomerular afferent arteriole vasoconstriction and thereby reducing glomerular filtration rate[21]. Recent studies have demonstrated that N-acetylcysteine, hemofiltration, hemodialysis, and the hypotonic or isotonic contrast agent can reduce the incidence of CIN[22-24]. Continuous hydration treatment is still considered the clinically effective method against CIN. However, the effect of other methods or drugs in patients with AMI, mostly combined with heart failure, resulting in complex hydration measures, is unclear. Hence, new drugs are required to improve CIN after PCI in older patients.
rhBNP is the natriuretic peptide receptor A, and recent studies have found that rhBNP can prevent CIN[12,25]. Meng et al[26] reported that rhBNP could improve the clinical prognosis of patients with right ventricular dysfunction caused by acute pulmonary embolism who underwent catheter-directed therapy. A recent meta-analysis also indicated that rhBNP could markedly improve the clinical outcome of AMI and decrease their length of stay without elevating the rate of adverse reactions[27]. In anterior myocardial infarction complicated by cardiogenic shock, low-dose rhBNP can improve pulmonary capillary wedge pressure but does not increase drug-related severe adverse events[28]. Liu et al[29] reported that pre-treatment with rhBNP before coronary angiography or PCI could improve renal function and decrease CIN incidence. Due to their unique situation, more elderly AMI patients cannot receive hydration therapy, and the effectiveness of rhBNP in these patients after PCI was unclear. Here, for the first time, we established that rhBNP administration could protect renal function and decrease the risk of CIN and acute heart failure in elderly AMI patients, not increasing the adverse drug effects.
In this study, we found that early application of rhBNP after primary PCI could protect renal function, reduce serum creatinine and cystatin C levels, improve creatinine clearance rate, and decrease the risk of CIN and acute heart failure in elderly AMI patients. Together, our study demonstrated rhBNP as an effective drug to prevent CIN in the elderly after PCI.
Further clinical studies are needed to address several limitations of the present study. A number of additional clinical factors, including all-cause mortality rate, activities, and daily life, should be examined. A long-term follow-up study is required to further clarify the clinical efficacy of rhBNP after primary PCI. Furthermore, the small sample size was from a single center. To determine whether or not this treatment is effective, a multicenter, randomized, controlled trial is required.
Our study suggests that early rhBNP treatment might help to protect renal function and decrease the risk of CIN in elderly AMI patients after primary PCI, decreasing the incidence of acute heart failure. There was no corroborating evidence to support the claim that low-dose rhBNP enhanced the risk of post-surgical complications. However, long-term outcome and adverse effect are still uncertain after rhBNP treatment. More research is required with patients who receive varied dosages and longer-term follow-up to understand the prospective application of rhBNP in postoperative elderly patients.
The overall incidence of contrast-induced nephropathy (CIN) is high after percutaneous coronary intervention (PCI), which leads to unfavorable early and long-term outcomes.
How to decrease the risk of CIN after PCI and explore clinical drugs to improve the outcome of elderly acute myocardial infarction (AMI) patients deserves further study.
To explore the clinical effectiveness of recombinant human brain natriuretic peptide (rhBNP) for CIN in elderly AMI patients after PCI.
One hundred and thirty-one elderly AMI patients underwent PCI: The control group (n = 66) was given 1 mL of 0.9% normal saline/(kg/h) for 72 h after PCI and the rhBNP group (n = 65) received intravenous rhBNP [1.5 mg/kg followed by 0.0075 mg/(kg/min)] for 72 h. Serum creatinine and cystatin C levels, creatinine clearance rate, and eGFR were measured at 24 h, 48 h, and 72 h after PCI.
The creatinine clearance rate and eGFR were increased, while the creatinine and cystatin C levels were decreased significantly in the rhBNP group compared to the control group at 48 h and 72 h. The risk of CIN and acute heart failure also significantly decreased in the rhBNP group. We found no statistic difference between the two groups in cardiac death and recurrent AMI.
Early application of rhBNP can protect the renal function and decrease the incidence of CIN in elderly AMI patients after primary PCI, reducing the incidence of acute heart failure.
Our study suggests that early rhBNP treatment might help to protect renal function and decrease the incidence of CIN in elderly AMI patients after primary PCI, reducing the incidence of acute heart failure. Based on these results, rhBNP treatment can be widely promoted. Also, more research is required with patients who receive varied dosages to understand the prospective application of rhBNP in postoperative elderly patients.
We thank Jiangsu Brilliant Biological Technology Co., Ltd. for providing technical and linguistic help. We thank Bullet Edits Limited for the linguistic editing and proofreading of the manuscript.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Arunachalam J, India; Karim HMR, India S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Chen YL
| 1. | Eindhoven DC, Wu HW, Kremer SWF, van Erkelens JA, Cannegieter SC, Schalij MJ, Borleffs CJW. Mortality differences in acute myocardial infarction patients in the Netherlands: The weekend-effect. Am Heart J. 2018;205:70-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 2. | D'Errigo P, Seccareccia F, Barone AP, Fusco D, Rosato S, Maraschini A, Colais P, Casali G. Effectiveness of invasive reperfusion therapy and standard medical treatment in AMI. Acta Cardiol. 2010;65:645-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 3. | Thiele H, Akin I, Sandri M, Fuernau G, de Waha S, Meyer-Saraei R, Nordbeck P, Geisler T, Landmesser U, Skurk C, Fach A, Lapp H, Piek JJ, Noc M, Goslar T, Felix SB, Maier LS, Stepinska J, Oldroyd K, Serpytis P, Montalescot G, Barthelemy O, Huber K, Windecker S, Savonitto S, Torremante P, Vrints C, Schneider S, Desch S, Zeymer U; CULPRIT-SHOCK Investigators. PCI Strategies in Patients with Acute Myocardial Infarction and Cardiogenic Shock. N Engl J Med. 2017;377:2419-2432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 576] [Cited by in RCA: 819] [Article Influence: 102.4] [Reference Citation Analysis (0)] |
| 4. | Galal H, Shehta M, Attia S, Bastawy I. Comparing Trimetazidine with Allopurinol in Prevention of Contrast Induced Nephropathy After Coronary Angiography. J Saudi Heart Assoc. 2020;32:451-455. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 5. | Lian X, He W, Zhan H, Chen J, Tan N, He P, Liu Y. The effect of trimetazidine on preventing contrast-induced nephropathy after cardiac catheterization. Int Urol Nephrol. 2019;51:2267-2272. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Ghelich Khan Z, Talasaz AH, Pourhosseini H, Hosseini K, Alemzadeh Ansari MJ, Jalali A. Potential Role of Allopurinol in Preventing Contrast-Induced Nephropathy in Patients Undergoing Percutaneous Coronary Intervention: A Randomized Placebo-Controlled Trial. Clin Drug Investig. 2017;37:853-860. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Sun X, Zhang R, Fan Z, Liu Z, Hua Q. Predictive value of hemoglobin-to-red blood cell distribution width ratio for contrast-induced nephropathy after emergency percutaneous coronary intervention. Perfusion. 2022;2676591221119422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 8. | Azzalini L, Candilio L, McCullough PA, Colombo A. Current Risk of Contrast-Induced Acute Kidney Injury After Coronary Angiography and Intervention: A Reappraisal of the Literature. Can J Cardiol. 2017;33:1225-1228. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 68] [Article Influence: 8.5] [Reference Citation Analysis (0)] |
| 9. | Ma G, Li M, Teng W, He Z, Zhai X, Xia Z. Febuxostat combined with hydration for the prevention of contrast-induced nephropathy in hyperuricemia patients undergoing percutaneous coronary intervention: A CONSORT-compliant randomized controlled trial. Medicine (Baltimore). 2022;101:e28683. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Pistolesi V, Regolisti G, Morabito S, Gandolfini I, Corrado S, Piotti G, Fiaccadori E. Contrast medium induced acute kidney injury: a narrative review. J Nephrol. 2018;31:797-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 70] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 11. | Wang L, Xu E, Ren S, Gu X, Zheng J, Yang J. Reduced glutathione does not further reduce contrast-induced nephropathy in elderly patients with diabetes receiving percutaneous coronary intervention. J Int Med Res. 2020;48:300060520964017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 12. | Xing K, Fu X, Wang Y, Li W, Gu X, Hao G, Miao Q, Li S, Jiang Y, Fan W, Geng W. Effect of rhBNP on renal function in STEMI-HF patients with mild renal insufficiency undergoing primary PCI. Heart Vessels. 2016;31:490-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Seeliger E, Lenhard DC, Persson PB. Contrast media viscosity versus osmolality in kidney injury: lessons from animal studies. Biomed Res Int. 2014;2014:358136. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 14. | Fang J, Zeng W. A meta-analysis of the clinical efficacy of rhBNP in treating patients with acute myocardial infarction and heart failure. Am J Transl Res. 2021;13:2410-2421. [PubMed] |
| 15. | Li N, Gao X, Wang W, Wang P, Zhu B. Protective effects of recombinant human brain natriuretic peptide on the myocardial injury induced by acute carbon monoxide poisoning. Cardiovasc Diagn Ther. 2020;10:1785-1794. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Liang L, Tang R, Xie Q, Han J, Li W. The clinical effect of recombinant human brain natriuretic peptide on asymptomatic peri-procedural myocardial injury after percutaneous transluminal coronary angioplasty. Sci Rep. 2020;10:15902. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 17. | Zuo P, Li Y, Zuo Z, Wang X, Ma G. Glycemic variability as predictor of contrast-induced nephropathy in diabetic patients with acute myocardial infarction undergoing percutaneous coronary intervention. Ann Transl Med. 2020;8:1505. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 18. | Wong PC, Li Z, Guo J, Zhang A. Pathophysiology of contrast-induced nephropathy. Int J Cardiol. 2012;158:186-192. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 133] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 19. | Zhang MM, Lv QZ, Li XY. Drug Effects and Clinical Investigations for Contrast-Induced Nephropathy After Coronary Angiography or Percutaneous Coronary Intervention in Patients With Diabetes. Am J Ther. 2017;24:e423-e430. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Rundback JH, Nahl D, Yoo V. Contrast-induced nephropathy. J Vasc Surg. 2011;54:575-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 60] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 21. | Morcos R, Kucharik M, Bansal P, Al Taii H, Manam R, Casale J, Khalili H, Maini B. Contrast-Induced Acute Kidney Injury: Review and Practical Update. Clin Med Insights Cardiol. 2019;13:1179546819878680. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 54] [Article Influence: 9.0] [Reference Citation Analysis (0)] |
| 22. | Liu LY, Liu Y, Wu MY, Sun YY, Ma FZ. Efficacy of atorvastatin on the prevention of contrast-induced acute kidney injury: a meta-analysis. Drug Des Devel Ther. 2018;12:437-444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 19] [Cited by in RCA: 28] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 23. | Yayla Ç, Yayla KG, Ünal S, Açar B, Akboğa MK, Demirtaş K. N-Acetylcysteine and Contrast-Induced Nephropathy. Angiology. 2018;69:85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 24. | Ellis JH, Cohan RH. Prevention of contrast-induced nephropathy: an overview. Radiol Clin North Am. 2009;47:801-811, v. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 44] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 25. | Zhang J, Fu X, Jia X, Fan X, Gu X, Li S, Wu W, Fan W, Su J, Hao G, Jiang Y, Xue L. B-type natriuretic peptide for prevention of contrast-induced nephropathy in patients with heart failure undergoing primary percutaneous coronary intervention. Acta Radiol. 2010;51:641-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 19] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 26. | Meng X, Fu M, Wang J, Xu H. Effects of Recombinant Human Brain Natriuretic Peptide in Patients with Acute Pulmonary Embolism Complicated with Right Ventricular Dysfunction Who Underwent Catheter-Directed Therapy. Int Heart J. 2022;63:8-14. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 27. | Fang J, Zeng W. A meta-analysis of the clinical efficacy of rhBNP in treating patients with acute myocardial infarction and heart failure. Am J Transl Res. 2021;13:2410-2421. [PubMed] |
| 28. | Pan Y, Lu Z, Hang J, Ma S, Ma J, Wei M. Effects of Low-Dose Recombinant Human Brain Natriuretic Peptide on Anterior Myocardial Infarction Complicated by Cardiogenic Shock. Braz J Cardiovasc Surg. 2017;32:96-103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 29. | Liu JM, Xie YN, Gao ZH, Zu XG, Li YJ, Hao YM, Chang L. Brain natriuretic peptide for prevention of contrast-induced nephropathy after percutaneous coronary intervention or coronary angiography. Can J Cardiol. 2014;30:1607-1612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |