Published online Nov 16, 2022. doi: 10.12998/wjcc.v10.i32.11967
Peer-review started: August 2, 2022
First decision: September 5, 2022
Revised: September 15, 2022
Accepted: October 18, 2022
Article in press: October 18, 2022
Published online: November 16, 2022
Processing time: 97 Days and 8.3 Hours
The trigeminocardiac reflex (TCR) is usually caused by an increased parasympathetic tone when pressure or traction is applied to the surrounding tissue of the trigeminal nerve. However, the inexperienced anesthesiologists may have challenges on the management of TCR patients.
This is the case of an 18-year-old woman diagnosed with hemangioma of the upper lip. During the operation, about 1 h after surgery started, a constant 1:1 premature ventricular complex was detected, and blood pressure was decreased when approaching the deeper part with more strong traction for exposure of the part. Although the management of arrhythmias, such as lidocaine and atropine, was injected, arrhythmia induced by surgical stimulation could not be eliminated completely. As the traction repeated, bradycardia was also repeated, despite injecting additional atropine. Therefore, the anesthesiologist and the surgeon decided to perform the operation only to the extent that the vascular tissue was selectively removed only at the site without the reflex.
With TCR, anesthesiologists should perform appropriate monitoring. In addition to proper drug administration, surgeons should be consulted to cope with stopping the surgery and setting the scope of the surgery even if the site is superficial.
Core Tip: The trigeminocardiac reflex (TCR) occurs when stimulation occurs adjacent to the trigeminal nerve. TCR usually results from stimulation of the central region of the trigeminal nerve and can result in lowered blood pressure and heart rate. Mild symptoms can be overcome with anticholinergic drugs such as atropine. But in this case, it is challenging to expect due to peripheral stimulation. And the bradycardia repeatedly occurred after the drug action time passed. In the end, it is crucial to quickly prevent complications by the reflex with proper monitoring and management.
- Citation: Cho SY, Jang BH, Jeon HJ, Kim DJ. Repeated ventricular bigeminy by trigeminocardiac reflex despite atropine administration during superficial upper lip surgery: A case report. World J Clin Cases 2022; 10(32): 11967-11973
- URL: https://www.wjgnet.com/2307-8960/full/v10/i32/11967.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i32.11967
The trigeminocardiac reflex (TCR) is regarded as a brainstem reflex, resulting in a series of hemodynamic nonuniformities as a decrease in heart rate (HR) and blood pressure during surgical stimulation of any point or branches of the trigeminal nerve[1]. TCRs are classified into subtypes of centrality, peripheral type, and gasserian ganglion type according to the location of the stimulation point[2].
Generally, TCR incurred during surgery has been reported mainly due to sudden bradyarrhythmia and hypotension in the central part of the trigeminal nerve. Moreover, TCR also occurs in the peripheral part of the trigeminal nerve; the skin or the nasopharynx may bring TCR by diving reflex. It differs from central TCR in that it can show bradyarrhythmia, hypertension, or normal blood pressure[3].
We experienced TCR-induced bradyarrhythmia during surgical removal of tissue in patients diagnosed with congenital hemangioma to the upper lip. A few case reports have demonstrated that repeated TCR was generated during the surgical treatment of peripheral tissues such as the lips, but only TCR due to direct nerve periphery and bone tissue manipulation has been reported in previous cases.
This is the case of a 18-year-old woman who visited the surgery due to discomfort caused by hypertrophy of the upper lip.
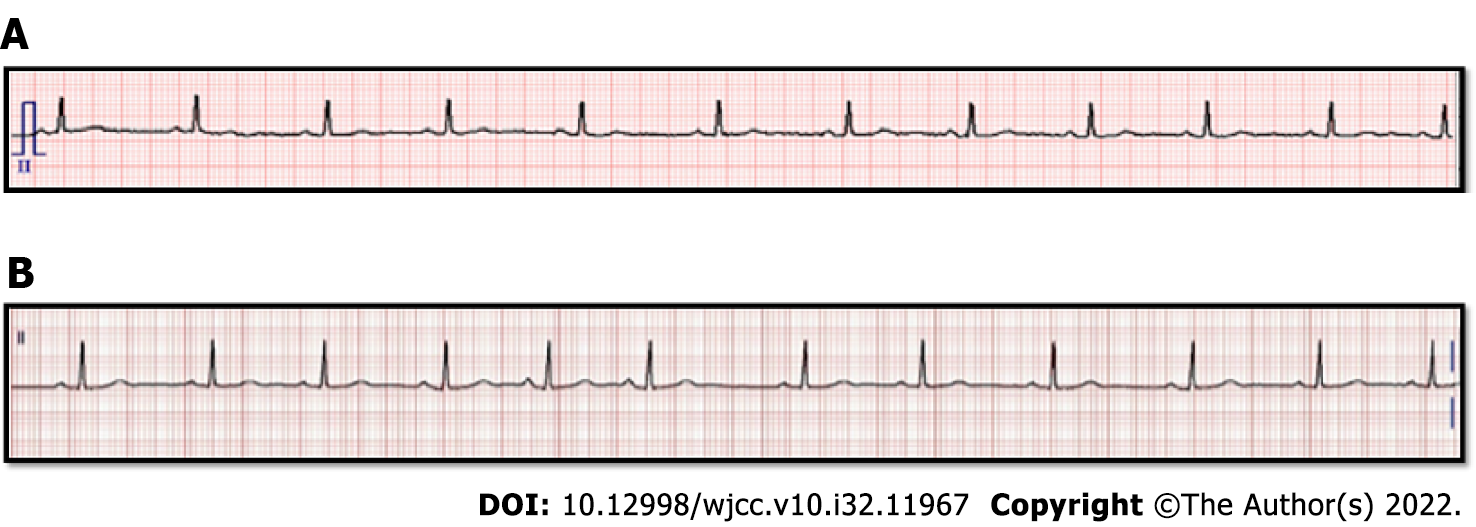
No findings were found on preoperative examination and electrocardiogram (ECG) (Figure 1A).
No specific findings were found on the patient's history.
The patient had no family or genetic disease history.
Vital signs were assessed before anesthesia induction: Blood pressure, 111/79 mmHg; HR, 94 beats/min; and SpO2, 99%.
On perioperative laboratory examinations and the C-reactive protein (CRP) level were within normal range.
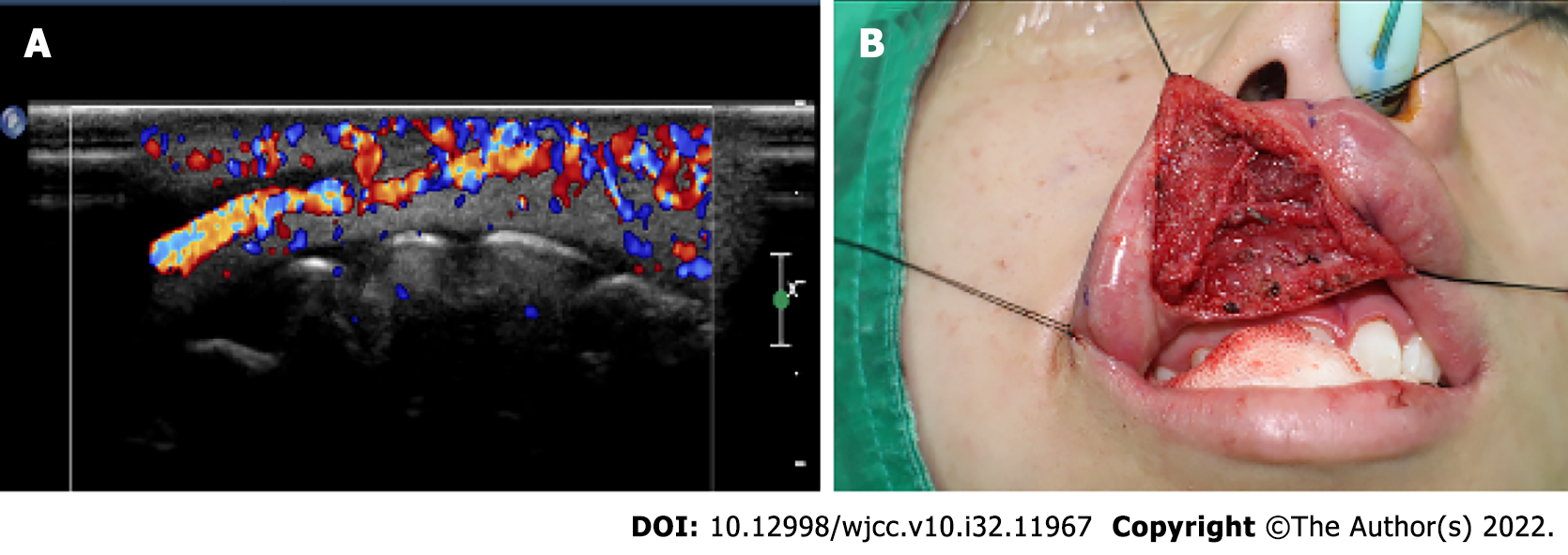
She was diagnosed with hemangioma by ultrasound (Figure 2A). Intraoperative picture, tracing with black silk to expose the surgical site during the approach to the surgical site (Figure 2B).
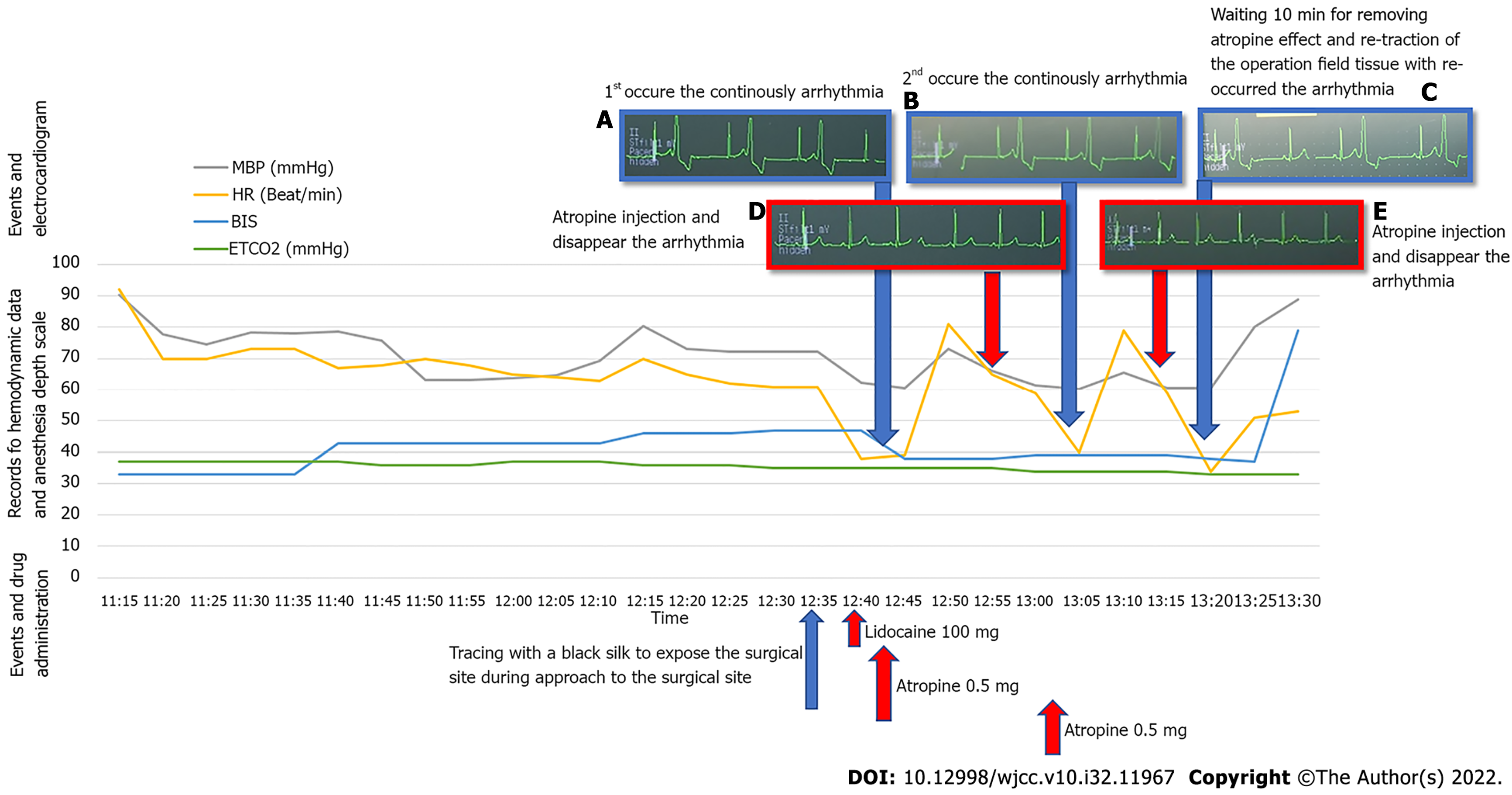
Anesthesia was induced by injecting 2 mg/kg of IV propofol, ventilating with 5%–6 vol % of desflurane using a mask, and simultaneously administering remifentanil at the target site with a concentration of 2.0 ng/mL for balanced anesthesia using a target- controlled infusion pump (Orchestra®, Fresenius Vial, France). After the loss of consciousness was confirmed by a bispectral index (BIS) of less than 40, rocuronium 0.6 mg/kg IV was administered. After confirming that the muscle had appropriately relaxed, endotracheal intubation was performed. The blood pressure measured after intubation was 110/62 mmHg, and the heart rate was 59 beats/min. During the operation, the respiratory rate was controlled to maintain the end-tidal CO2 partial pressure of 32–38 mmHg, and mechanical ventilation was performed with oxygen 1 L/min and air 2 L/min. Desflurane was controlled to maintain BIS from 40 to 60. The operation proceeded normally for about 1 hour, but a constant 1:1 premature ventricular complex (PVC) was detected in the course of approaching the more profound part with more strong traction for exposure of the part (Figure 2B), and blood pressure was decreased from 97/60 mmHg to 88/47 mmHg, respectively. The procedure was stopped after vital signs and ECG had changed. Arrhythmia disappeared shortly after traction was released, and vital signs were stabilized within a few seconds. When traction stimulation started for surgery again, bradycardia recurred with 35 PVCs.
It was diagnosed ventricular bigeminy due to TCR.
To manage arrhythmia with surgical stimulation, lidocaine 2 mg/kg IV was injected to alleviate the patient's condition, but the arrhythmia induced by surgical stimulation could not be eliminated. After re-experiencing one arrhythmia with bradycardia, atropine 0.5 mg was intravenously injected. After atropine injection, wait 10 min for atropine to take effect, and arrhythmia reoccurs with retraction of the surgical field tissue. When arrhythmia has been stabilized within a few seconds after stopping the traction and the repeated occurrence of bradycardia when the surgical stimulus is given, we hypothesized that the excision hemangioma surrounding the trigeminal nerve and passing through the upper lip, by the trigeminal nerve, is stimulated and then TCR occurred (Figure 3). Therefore, the surgeon decided to perform the operation only to the extent that the vascular tissue was selectively removed only at the site where the bradycardia did not occur upon surgical stimulation, and the operation was terminated safely.
In the postanesthesia care unit, the patient's vital signs were all within normal range. A 12-lead ECG was performed to exclude cardiovascular causes of bradyarrhythmia and sinus rhythm with a HR of 71 beats/min with premature atrial complex and without any symptoms (Figure 1B). The patient did not show signs of postoperative bradycardia in the ward or abnormal changes in the trigeminal nerve and was discharged 6 d postoperatively.
TCR was reported to be caused by intracranial maxillofacial surgery, cranial base surgery, and cerebrovascular surgery. According to the type of brain surgery, TCR incidence was experienced from 11% to 18% of cases[4]. The trigeminal nerve is responsible for the sensory supply to the scalp, face, nose, and mouth mucosa. Stimulation of the trigeminal receptors that innervate the nasal passage area is thought to produce a crucial stimulus for initiating the trigeminal-respiratory reflex, and arrhythmias could happen with it. This reflex may be fatal but may occur when the surgical site is a peripheral region such as the lips. It may occur in a simple incision and upon suturing in close proximity to the trigeminal nerve branch or during device insertion for surgery.
In this operation, TCR reaction occurred after traction (plausibility), and when traction was stopped, TCR was also stopped, and bigeminy was reduced (reversibility). Additionally, the above phenomenon was repeatedly generated by traction (reversibility) and has shown a temporary bigeminy loss when traction or atropine was applied with weak traction. This case seems to be consistent with the definition of TCR presented by Meuwly et al[5].
The risk factors known to increase TCR incidence include hypercapnia, hypoxemia, the lighter depth of anesthesia, an individual's high resting vagal tone like younger age group, opioids, preoperative use of beta-blockers calcium channel blockers, acidosis, and the strength and length of the irritant stimulus. Opioids may increase vagal tone through their inhibitory action on the sympathetic nervous system. Beta-blockers reduce the sympathetic response of the heart and, by so doing, increase the vagal response resulting in bradyarrhythmia. Calcium channel blockers result in peripheral arterial smooth muscle relaxation and vasodilatation, causing a reduction in blood pressure[6].
This patient had relative risk factors, which include lighter anesthesia, younger age, and use of narcotics such as remifentanil. Importantly, a stronger link between a lighter depth of anesthesia and more episodes of asystole has been observed than that of a stronger depth of anesthesia. Another report has shown that TCR episodes were aborted by boluses of propofol by increasing the anesthesia depth and additional medication such as neostigmine to prevent bradycardia following propofol injection[7]. Adjusting the narcotics or anesthesia depth during surgery may be necessary. If bradycardia was maintained, a question about whether remifentanil could be stopped and atropine could be used to proceed with the operation was raised.
One of the most important factors for TCR development is the nature of surgical stimulation. Blanc[8] reported that sudden and persistent stimulation during craniofacial surgery produces TCR better than soft stimulation. Arnold et al[9] also reported that when operating gently, TCR did not occur. It is thought that the traction to the surgical tie for exposing the surgical site is a factor that increases the possibility of TCR occurrence.
Unlike, in this case, TCR may occur without pre-onset hemodynamic changes. The changes help to identify possible danger signals[10]. TCR studies have shown that CRP, noradrenaline, and specific markers of ischemic biomarkers called tissue necrosis factor - a change when TCR occurs. This suggests that it is helpful as an alternative marker that can prevent TCR development in later studies[11]. In this case, the CRP level was within normal range perioperatively.
Most of the surgeries for which TCR has been reported were eye surgery and manipulation of trigeminal nerve branches, dental surgery, and cranial surgery[12]. Reports have shown that it has also occurred in simple procedures such as skin suturing[13]. However, it was not predicted that this operation would occur in the lip of the peripheral branch. Peripheral stimulation of the nasopharynx, like rhinoplasty, may also trigger TCR[14]. Even in the peripheral area, caution is required in operation surrounding the trigeminal nerve branches. This case has shown that mixed stimulations through the skin or the mucosa and the maxilla-mandibular branch from peripheral types of TCR may cause bradycardia and hypotension[15]. Sudden bradycardia and hypotension can occur during adjacent area manipulation, and anticholinergic pretreatment like atropine and appropriate monitoring during operation is recommended to prevent cardiac reflex[16]. Moreover, more detailed events in the ECG, like the transient asystole, may occur by TCR[17]. And for the management of results, the administration of drugs such as lidocaine and atropine was not helpful in maintaining normal HR due to their vagolytic effect in a specific situation. The only and next step to maintain the normal rhythm is to stop surgical stimulation. However, the operation cannot be stopped due to the opened surgical site, and the surgical site must be exposed by fixing any device or surgical tie for proper surgical procedures. Like in this case, and if the nerves were in the vicinity from the operation site, a nerve monitoring device needs to be used, and then surgery should be performed through appropriate traction. So, appropriate monitoring equipment should be provided, and the situation should be managed appropriately if the surgical site is close to the trigeminal nerve branches. In the case of sensory nerve monitoring, the effects of inhalation anesthetics and muscle relaxants are greatly affected. In the case of monitoring and surgery, 0.5 to 0.7 minimum alveolar concentration inhalation anesthetic and train-of-four should be maintained at least 2 to ensure proper monitoring[18].
Stimulating the adjacent area of the trigeminal nerve during maxillofacial surgery is inevitable, and understanding the mechanism of TCR is necessary to avoid the technique of generating such reflexes. Intraoperative neurophysiological monitoring is recommended for high-risk surgery for the occurrence of TCR. Moreover, the surgical staff should obtain perioperative informed consent from the patients for safe surgery. During anesthesia monitoring, adequate background knowledge of the situations and risks that TCR can occur is necessary to minimize the use of drugs that can stimulate TCR occurrence, avoid hypercapnia and hypoxemia, and maintain proper anesthesia depth. In the event of TCR, the surgeon should be immediately aware of countermeasures, including stopping surgical manipulation and administering anticholinergic drugs. However, anticholinergics limit one's ability to control the reflex, and the most important thing is to stop surgical stimulation for safety if the vital signs threaten the patient's condition.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mhamunkar PA, India; Zhang YN, China S-Editor: Liu XF L-Editor: A P-Editor: Liu XF
| 1. | Arasho B, Sandu N, Spiriev T, Prabhakar H, Schaller B. Management of the trigeminocardiac reflex: Facts and own experience. Neurol India. 2009;57:375-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 66] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Chowdhury T, Mendelowith D, Golanov E, Spiriev T, Arasho B, Sandu N, Sadr-Eshkevari P, Meuwly C, Schaller B; Trigemino-Cardiac Reflex Examination Group. Trigeminocardiac reflex: The current clinical and physiological knowledge. J Neurosurg Anesthesiol. 2015;27:136-147. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 91] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 3. | Schaller BJ, Filis A, Buchfelder M. Trigemino-cardiac reflex in humans initiated by peripheral stimulation during neurosurgical skull-base operations. Its first description. Acta Neurochir (Wien). 2008;150:715-7; discussion 717. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 40] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 4. | Schaller B, Sandu N, Filis A, Ottaviani G, Rasper J, Nöethen C, Buchfelder M; Trigemino-Cardiac-Reflex-Examination-Group (T. C.R.E.G.). Trigemino-cardiac reflex: The trigeminal depressor responses during skull base surgery. Clin Neurol Neurosurg. 2009;111:220. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Meuwly C, Chowdhury T, Sandu N, Golanov E, Erne P, Rosemann T, Schaller B. Definition and Diagnosis of the Trigeminocardiac Reflex: A grounded theory approach for an update. Front Neurol. 2017;8:533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 23] [Cited by in RCA: 42] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 6. | Schmeling WT, Kampine JP, Warltier DC. Negative chronotropic actions of sufentanil and vecuronium in chronically instrumented dogs pretreated with propranolol and/or diltiazem. Anesth Analg. 1989;69:4-14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Chowdhury T, Ahuja N, Schaller B. Severe bradycardia during neurosurgical procedure: Depth of anesthesia matters and leads to a new surrogate model of the trigeminocardiac reflex: A case report. Medicine (Baltimore). 2015;94:e2118. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 8. | Blanc VF. Trigeminocardiac reflexes. Can J Anaesth. 1991;38:696-699. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 47] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 9. | Arnold RW, Jensen PA, Kovtoun TA, Maurer SA, Schultz JA. The profound augmentation of the oculocardiac reflex by fast acting opioids. Binocul Vis Strabismus Q. 2004;19:215-222. [PubMed] |
| 10. | Prabhakar H, Anand N, Chouhan RS, Bithal PK. Sudden asystole during surgery in the cerebellopontine angle. Acta Neurochir (Wien). 2006;148:699-700; discussion 700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 37] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 11. | Schaller BJ, Weigel D, Filis A, Buchfelder M. Trigemino-cardiac reflex during transsphenoidal surgery for pituitary adenomas: Methodological description of a prospective skull base study protocol. Brain Res. 2007;1149:69-75. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 12. | Chowdhury T, Rizk AA, Azazi EA, Venkatraghavan L, Shankar JS, Schaller B. Brain and heart crosstalk during neurointerventional procedures: The role of the trigeminocardiac reflex: An updated systematic review. J Neurosurg Anesthesiol. 2022;34:282-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 9] [Reference Citation Analysis (0)] |
| 13. | Chowdhury T, Cappellani RB, West M. Recurrent bradycardia and asystole in a patient undergoing supratentorial tumor resection: Different types of trigeminal cardiac reflex in same patients. Saudi J Anaesth. 2013;7:216-218. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Özçelik D, Toplu G, Türkseven A, Sezen G, Ankarali H. The Importance of the Trigeminal Cardiac Reflex in Rhinoplasty Surgery. Ann Plast Surg. 2015;75:213-218. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Champion A, Masi J. Profound trigeminocardiac reflex from lingual nerve stimulation: A case report. J Dent Anesth Pain Med. 2022;22:61-65. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Lee DI, Won SG, Kim DW, Kim DO, Choi YK, Shin KI. Bezold-Jarish Reflex during Shoulder Arthroscopy (in the Sitting Position) under Interscalene Block. Korean J Pain. 1997;10:166-169. |
| 17. | Yamada S, Yano Y, Fujita T, Taneda M. Efficacy of transcutaneous cardiac pacing for transient asystole caused by trigeminocardiac reflex: Illustrative case. J Neurosurg Case Lessons. 2021;2:CASE21198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 18. | Chong CT, Manninen P, Sivanaser V, Subramanyam R, Lu N, Venkatraghavan L. Direct comparison of the effect of desflurane and sevoflurane on intraoperative motor-evoked potentials monitoring. J Neurosurg Anesthesiol. 2014;26:306-312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 45] [Article Influence: 4.1] [Reference Citation Analysis (0)] |