Published online Nov 6, 2022. doi: 10.12998/wjcc.v10.i31.11523
Peer-review started: May 26, 2022
First decision: June 27, 2022
Revised: June 29, 2022
Accepted: September 19, 2022
Article in press: September 19, 2022
Published online: November 6, 2022
Processing time: 154 Days and 4.5 Hours
It is very rare to suffer from colorectal adenocarcinoma and abdominal tuberculosis simultaneously. Even in a country such as China, where tuberculosis is still endemic, its diagnosis and treatment are challenging. This article describes in detail a case of rectal cancer complicated by abdominal tuberculosis and its pathological features.
We outline the case of a 71-year-old female who was admitted with intermittent blood in the stool over the past year. The patient was diagnosed with low rectal cancer and received neoadjuvant therapy. The patient then returned to the hospital for surgery, but diffusely distributed nodules were found during laparoscopic exploration. The diagnosis of rectal cancer with extensive metastasis was considered during the operation. There was no opportunity for radical surgery. Thus, nodules were taken for pathological examination, and the abdomen was closed. The histopathological diagnosis was tuberculous granuloma, and the patient was treated with standardized anti-tuberculosis drugs in a specialized hospital. Later, the patient again came to our hospital and underwent abdominoperineal resection. She was discharged 10 d after the operation in good clinical condition.
We aim to emphasize the importance of preoperative and postoperative pathological examination in diagnosis and treatment.
Core Tip: We report a relatively rare case of rectal adenocarcinoma combined with abdominal tuberculosis. The difficulty is that it is easily misdiagnosed as rectal cancer with extensive abdominal and pelvic metastasis, thus delaying treatment. Therefore, the pathological examination of abdominal and pelvic nodules during and after surgery is very important in diagnosis and treatment.
- Citation: Liu PG, Chen XF, Feng PF. Rectal cancer combined with abdominal tuberculosis: A case report. World J Clin Cases 2022; 10(31): 11523-11528
- URL: https://www.wjgnet.com/2307-8960/full/v10/i31/11523.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i31.11523
Tuberculosis is a chronic infectious disease that is caused by Mycobacterium tuberculosis invading the human body. According to the global tuberculosis report released by the World Health Organization in 2019, tuberculosis is an infectious disease with the highest mortality rate in the world, causing 1.5 million deaths in 2018. The incidence of tuberculosis in China ranks third in the world, and China is one of 22 countries with a high burden of tuberculosis[1,2]. Abdominal tuberculosis is a form of extrapulmonary tuberculosis, and it accounts for approximately 1%-5% of the total number of tuberculosis cases[3]. The clinical manifestations are mostly nonspecific symptoms[4]. The common diseased organs of abdominal tuberculosis are the colon, peritoneum and mesentery[5], and peritoneal biopsy is the gold standard for diagnosis. It is very rare to suffer from colorectal cancer and abdominal tuberculosis at the same time, and only 5 cases have been reported in the English literature published in the past 20 years[6-10]. We report a case of rectal adenocarcinoma combined with abdominal tuberculosis and emphasize the key role of the pathological examination of abdominal and pelvic nodules on intraoperative and postoperative diagnosis and treatment.
A 71-year-old female patient reported changes in stool characteristics with intermittent blood in the stool over the past year without obvious cause.
The patient was diagnosed with low rectal cancer and received neoadjuvant therapy in our hospital several months ago. The long-course chemoradiotherapy included a total radiotherapy dose of 50.4 Gray unit (Gy) and a daily dose of 1.8 Gy, combined with capecitabine [625-825 mg/(m2 · time), peros, twice/day, (day 1 - day 7) × 5 wk].
The patient had no underlying disease and no history of living in foci of infection or endemic areas.
She had no personal or family history of other disease.
The patient’s abdomen was soft without tenderness, rebound pain and abdominal mass. During the digital rectal examination, a 3 cm × 2 cm tumor was touched on the anterior wall of the rectum 4 cm from the anal margin. Her blood pressure was 113/54 mmHg and pulse rate was 94 bpm.
The tumor-related biological indicators carcinoembryonic antigen was 2.30 ng/mL and carbohydrate antigen (CA) 199 was 28.4 U/mL, which were within the normal range. The value of CA242 was 35.20 U/mL, which was slightly high.
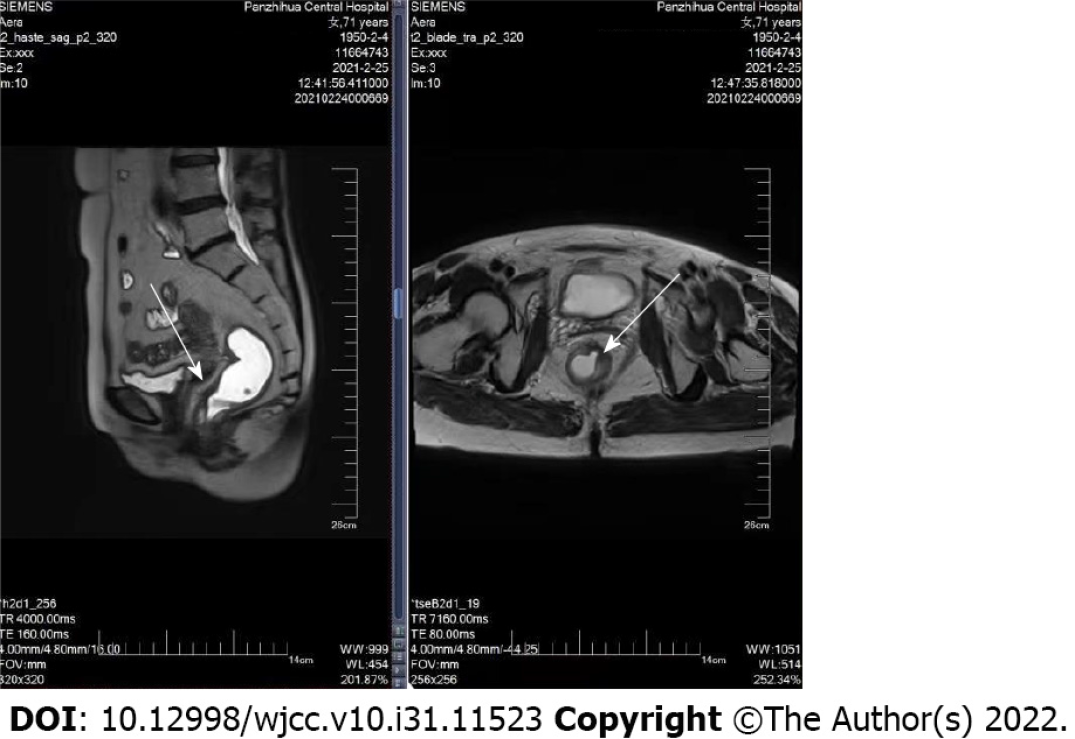
Magnetic resonance imaging (MRI) examination showed that the lesion was located below the peritoneal reentry, about 0.7 cm from the dentate line and about 3.3 cm from the anal margin (Figure 1). Chest computed tomography (CT) showed no obvious abnormalities.
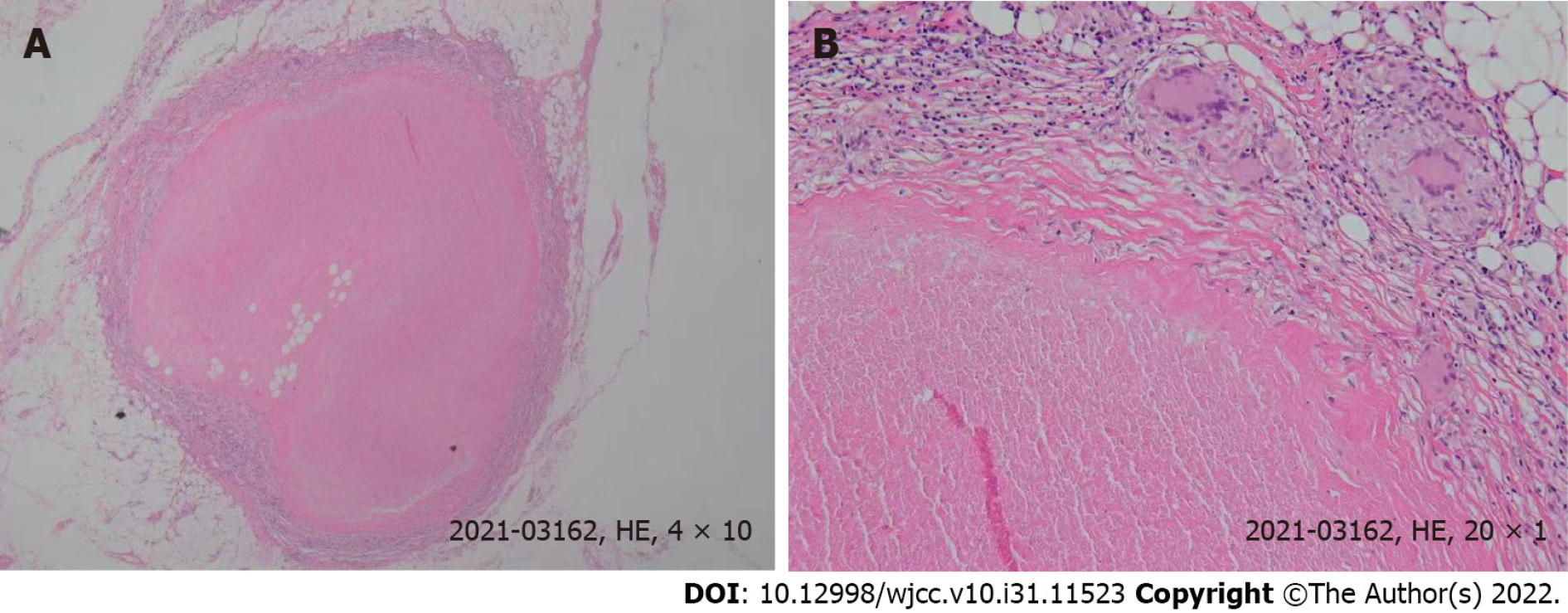
During the first operation, laparoscopic exploration revealed pelvic floor effusion, as well as diffuse gray-white nodules on the surface of the abdominal pelvic cavity, greater omentum, and the intestinal wall. The largest nodule was approximately 0.3 cm in diameter (Figure 2). Histopathological exa
The patient received standardized anti-tuberculosis treatment (isoniazid, rifampicin, ethambutol) for three months in a specialist hospital. She then returned to our hospital to undergo abdominoperineal resection.
During the operation, there was no obvious effusion and lymphadenectasis in the abdominal cavity. Postoperative pathology showed moderately differentiated rectal adenocarcinoma. A large number of peritoneal nodules were necrotic, and the surrounding tissues were granulomas. In addition, no cancer was found. After the operation, the patient was in stable condition and was discharged from the hospital ten days later. Her clinical condition has been good since then.
Tuberculosis is still a global health problem. It has caused high morbidity and mortality in developing countries and has shown an upwards trend each year in the western world[11]. The definition of abdominal tuberculosis refers to tuberculosis infection involving the abdomen, such as the peritoneum, mesentery, abdominal lymph nodes, gastrointestinal tract, liver and gallbladder and other substantial organs[12]. According to reports, the ileo-colic junction is the most common site of abdominal tuberculosis[13], and the peritoneum and abdominal lymph nodes are the most common sites of involvement in children[14]. Abdominal tuberculosis is a relatively rare type of tuberculosis. The clinical symptoms are nonspecific, ranging from acute symptoms, such as perforation and obstruction, to chronic symptoms, such as abdominal pain, bloating, fatigue, diarrhea, and weight loss[15]. The initial symptoms can be confusing, especially in the context of a history of cancer or elevated tumor indicators. If the patient is not treated in time, the delay in the diagnosis of abdominal tuberculosis is associated with high morbidity and mortality[16,17]. Currently, there is no reliable tool to diagnose abdominal tuberculosis. Chest X-ray is a routine and simple imaging test, but it has been reported that only 15%-56% of patients with abdominal tuberculosis have chest X-ray evidence of pulmonary tuberculosis[18]. In the era of laparoscopy, the diagnosis rate of histopathological examination by peritoneal biopsy is 85%-100%[19]. In addition, PCR detection of tissue is also an effective tool that has a high degree of specificity and sensitivity[20].
This is a relatively rare case. The patient was diagnosed with rectal adenocarcinoma on admission to our hospital. The ulcerative mass was 4 cm from the anal margin. MRI showed that the tumor stage was cT3-4NxM0. Neoadjuvant therapy was performed according to treatment guidelines. However, during the first laparoscopic exploration, a small amount of yellow effusion was found in the pelvic cavity, and grey-white nodules were diffusely distributed on the surface of the abdominal pelvic cavity, omentum, and intestinal wall. We hypothesized that the patient had rectal cancer with extensive abdominal and pelvic metastasis, and there was no chance of radical surgery. Therefore, the peritoneum, mesenteric and greater omentum nodules were removed and sent for paraffin pathology. As the patient's rectal disease was not obstructed, colostomy was not performed temporarily. Moreover, the patient had no chest CT abnormalities, so the possibility of tuberculosis was not considered.
However, it was surprising that histopathological examination revealed granulomatous tissue nodules, suggesting tuberculosis. At this time, further inspection was needed to clarify its nature to formulate the next treatment plan. If it was determined to be rectal cancer with abdominal tuberculosis, it should be reviewed after regular anti-tuberculosis treatment, and then rectal cancer surgery should be performed according to the situation. If rectal cancer surgery can be completed, the patient's prognosis will be greatly improved. If it is suggested that it is a metastatic nodule, chemotherapy is recommended, but the prognosis is very poor. Fragments of Mycobacterium tuberculosis were found by Tb-PCR. Therefore, the patient was clearly diagnosed with abdominal tuberculosis and rectal adenocarcinoma.
After three months of standardized anti-tuberculosis treatment in a specialist hospital, the patient was ready for surgery. As the patient was in the locally advanced stage of low rectal cancer, was older, had poor cardiac function, and had tuberculosis, sphincter-preserving surgery was not performed. Instead, a radical resection of the abdominal perineum combined with rectal cancer excision was performed. The patient recovered well after the operation.
Histopathological examination is still the gold standard for the diagnosis of abdominal tuberculosis[21], but there are certain difficulties in obtaining suitable tissue materials in clinical practice, which brings certain difficulties to our comprehensive diagnosis. Clinically, the understanding of abdominal tuberculosis should be strengthened, and the awareness and ability of differential diagnosis should be enhanced. The pathological examination of abdominal and pelvic nodules during and after the operation is very important in the diagnosis and treatment of the disease.
Pathological examination during and after surgery is very important in the diagnosis and treatment of complex diseases.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Elfeki H, Egypt; Poullis A, United Kingdom S-Editor: Wang DM L-Editor: Webster JR P-Editor: Wang DM
| 1. | Hernandez-Andrade E. Re: Childhood cognitive development after fetal growth restriction. E. Llurba, A. A. Baschat, O. M. Turan, J. Harding and L. M. McCowan. Ultrasound obstet gynecol 2013; 41: 383-389. Ultrasound Obstet Gynecol. 2013;41:364-365. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Floyd K, Glaziou P, Zumla A, Raviglione M. The global tuberculosis epidemic and progress in care, prevention, and research: an overview in year 3 of the End TB era. Lancet Respir Med. 2018;6:299-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 196] [Cited by in RCA: 270] [Article Influence: 38.6] [Reference Citation Analysis (0)] |
| 3. | Cho JK, Choi YM, Lee SS, Park HK, Cha RR, Kim WS, Kim JJ, Lee JM, Kim HJ, Ha CY, Kim TH, Jung WT, Lee OJ. Clinical features and outcomes of abdominal tuberculosis in southeastern Korea: 12 years of experience. BMC Infect Dis. 2018;18:699. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 37] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Lata Verma M, Tripathi V, Singh U, Agarwal P, Sachan R, Lata Sankwar P. Peritoneal tuberculosis with benign ovarian tumor. Indian J Tuberc. 2019;66:499-501. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Debi U, Ravisankar V, Prasad KK, Sinha SK, Sharma AK. Abdominal tuberculosis of the gastrointestinal tract: revisited. World J Gastroenterol. 2014;20:14831-14840. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 231] [Cited by in RCA: 217] [Article Influence: 19.7] [Reference Citation Analysis (4)] |
| 6. | Roh WS, Lee S, Park JH, Kang J. Abdominal Sarcoidosis Mimicking Peritoneal Carcinomatosis. Ann Coloproctol. 2018;34:101-105. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Buch K, Christiansen EG, Skau AM. [Simultaneous intestinal tuberculosis and adenocarcinoma]. Ugeskr Laeger. 2017;179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 8. | Choi YJ, Kim HG, Choi YA, Joo WC, Son DW, Kim CH, Shin YW, Kim YS. [A case of pseudomembranous colitis associated with rifampicin therapy in a patient with rectal cancer and gastrointestinal tuberculosis]. Korean J Gastroenterol. 2009;53:53-56. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Fahlbusch T, Künzli B, Schlottmann R, Tannapfel A, Uhl W, Braumann C. Tuberculosis Mimicking Disseminated Peritoneal Carcinomatosis of a Sigmoid Carcinoma. J Gastrointest Surg. 2019;23:877-878. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Demetriou GA, Nair MS, Navaratnam R. Concurrent caecal and transverse colonic tuberculosis masqueratingsynchironous colonic carcinima. BMJ Case Rep. 2013;bcr2013009379. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Pattanayak S, Behuria S. Is abdominal tuberculosis a surgical problem? Ann R Coll Surg Engl. 2015;97:414-419. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Rathi P, Gambhire P. Abdominal Tuberculosis. J Assoc Physicians India. 2016;64:38-47. [RCA] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 13. | Gill P, Coatsworth NR, Gundara JS, Hugh TJ, Samra JS. Tuberculosis: experience in a low endemic area Australian tertiary hospital. World J Surg. 2013;37:984-990. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Sartoris G, Seddon JA, Rabie H, Nel ED, Schaaf HS. Abdominal Tuberculosis in Children: Challenges, Uncertainty, and Confusion. J Pediatric Infect Dis Soc. 2020;9:218-227. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 17] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 15. | Chen CH, Yang CC, Yeh YH, Yang JC, Chou DA. Pancreatic tuberculosis with obstructive jaundice--a case report. Am J Gastroenterol. 1999;94:2534-2536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 41] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Yeh HF, Chiu TF, Chen JC, Ng CJ. Tuberculous peritonitis: analysis of 211 cases in Taiwan. Dig Liver Dis. 2012;44:111-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Chow KM, Chow VC, Szeto CC. Indication for peritoneal biopsy in tuberculous peritonitis. Am J Surg. 2003;185:567-573. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 83] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 18. | Hassan I, Brilakis ES, Thompson RL, Que FG. Surgical management of abdominal tuberculosis. J Gastrointest Surg. 2002;6:862-867. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 21] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 19. | Rath T, Atreya R, Geißdörfer W, Lang R, Nägel A, Neurath MF. A Severe Case of Tuberculosis Radiologically and Endoscopically Mimicking Colorectal Cancer with Peritoneal Carcinomatosis. Case Rep Gastrointest Med. 2017;2017:6206951. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Lazarus AA, Thilagar B. Abdominal tuberculosis. Dis Mon. 2007;53:32-38. [RCA] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 53] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 21. | Ahmad R, Changeez M, Khan JS, Qureshi U, Tariq M, Malik S, Ahmad SH, Shafique MS. Diagnostic Accuracy of Peritoneal Fluid GeneXpert in the Diagnosis of Intestinal Tuberculosis, Keeping Histopathology as the Gold Standard. Cureus. 2018;10:e3451. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |