Published online Nov 6, 2022. doi: 10.12998/wjcc.v10.i31.11419
Peer-review started: May 20, 2022
First decision: August 21, 2022
Revised: August 31, 2022
Accepted: September 29, 2022
Article in press: September 29, 2022
Published online: November 6, 2022
Processing time: 159 Days and 20.2 Hours
The proper cuff pressure of endotracheal tube (ET) plays an important role in sealing the airway and preventing airway complications during mechanical ventilation. The ET cuff shape affects the cuff pressure after positional change.
To investigate cuff pressure between tapered and cylindrical cuff after extension of head and neck during nasal endotracheal intubation.
In a randomized clinical trial, 52 patients were randomized to one of two groups: cylindrical cuff or Tapered cuff. Cuff pressure with 22 cmH2O was applied to patients in the neutral position. After extension of head and neck, the cuff pressure was evaluated again and readjusted to 22 cmH2O. In addition, the extent of cephalad migration of ET tip was assessed and postoperative airway complications such as sore throat, and hoarseness were measured.
The cuff pressure was higher in the tapered cuff (28.7 ± 1.0 cmH2O) than in the cylindrical cuff (25.5 ± 0.8 cmH2O) after head and neck extension (P < 0.001). The extent of cephalad migration of tube tip was greater in TaperGuard ET (18.4 ± 2.2 mm) than in conventional ET (15.1 ± 1.2 mm) (P < 0.001). The incidence of postoperative airway complications was comparable between two groups.
After head and neck extension, the cuff pressure and the extent of cephalad migration of ET was greater in tapered cuff than in cylindrical cuff during nasal intubation, respectively.
Core Tip: The proper cuff pressure of endotracheal tube is very important in a sealing airway and avoiding airway complication during mechanical ventilation. This was a clinical randomized clinical trial comparing cuff pressure between tapered and cylindrical cuff after head and neck extension during nasal endotracheal intubation. The cuff pressure and the extent of cephalad migration of tube tip was greater in TaperGuard endotracheal tube than in conventional endotracheal tube after head and neck extension, respectively.
- Citation: Seol G, Jin J, Oh J, Byun SH, Jeon Y. Pressure changes in tapered and cylindrical shaped cuff after extension of head and neck: A randomized controlled trial. World J Clin Cases 2022; 10(31): 11419-11426
- URL: https://www.wjgnet.com/2307-8960/full/v10/i31/11419.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i31.11419
The cuff of endotracheal tube (ET) plays an important role in providing a critical function of sealing the airway during mechanical ventilation. A cuff pressure of 20-30 cmH2O is clinically recommended for prevention of tracheal damage, leakage of gas and tracheal aspiration during mechanical ventilation[1,2]. It was found that the cuff pressure greater than 30 cmH2O decreases blood flow of tracheal mucosa, resulting in airway complications such as sore throat, hoarseness, and coughing[3-6].
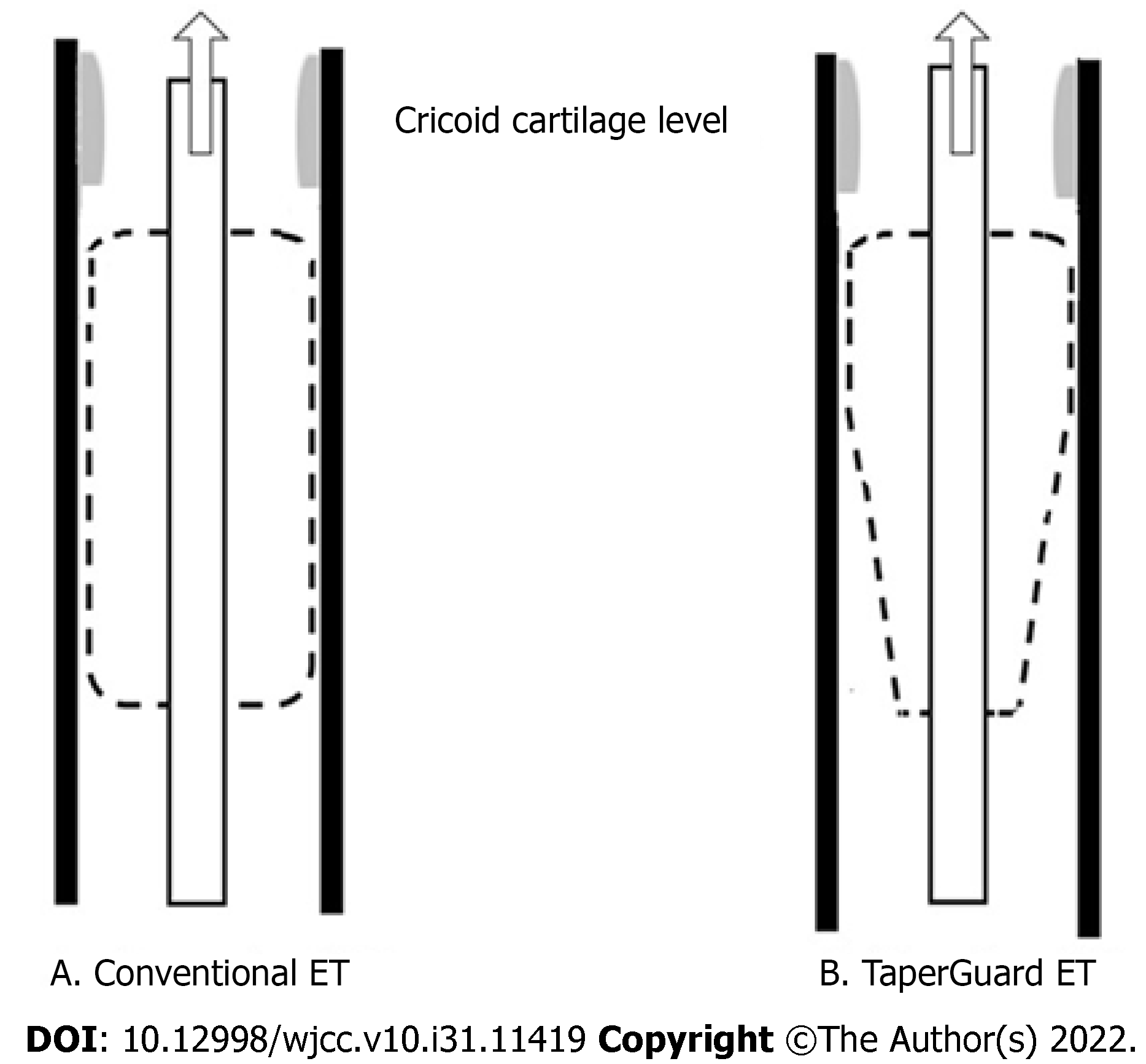
The newly developed TaperGuard ET has a taper shaped cuff, whereas the conventional ET has a cylindrical cuff (Figure 1). It is demonstrated that tapered cuff is effective to improve sealing performance and prevention of microaspiration, compared to a cylindrical cuff of conventional ET[7-9].
The cuff pressure of ET can be affected by positional change during surgery[10-12]. When the cephalad migration of ET occurs, the intracuff volume can be compressed at a narrower and less complaint airway space such as at level of cricoid cartilage, leading to increased cuff pressure[13,14]. The previous studies showed that the cuff pressure significantly increased in the TaperGuard ET than in the conventional ET after positional changes such as supine with lateral rotation of head and lateral frank position in orally intubated patients[13,14]. After rotation of head, the degree of cephalad migration of ET was significantly higher in the tapered cuff than in the cylindrical cuff during oral endotracheal intubation[14]. Oral surgery often requires nasal endotracheal intubation and supine position with head and neck extension to facilitate surgery, which can displace ET toward vocal cord[10]. However, there are only a few studies investigating the cuff pressure change and the degree of migration of ET following anterior-posterior movement during nasal endotracheal intubation. Therefore, this study was designed to compare the cuff pressure between nasal TaperGuard ET and nasal conventional ET after extension of head and neck during oral surgery. In addition, the distance from the carina to the ET tip after extension of head and neck was compared and postoperative airway complications such as sore throat, and hoarseness were assessed.
In this randomized clinical trial, 52 patients with American Society of Anesthesiologists physical status I (a normal healthy patient), II (a patient with mild systemic disease) III (a patient with severe systemic disease) who underwent nasal endotracheal intubation for oral surgery in the Kyungpook National Hospital were included. Patients with history of difficult intubation, and nasal trauma or surgery, limited head and neck movement, respiratory diseases and body mass index more than 35 kg/m2 were excluded. This study was approved by the Ethics Committee of Kyungpook National University Hospital (2019-11-043-001) and informed written consent was obtained from all patients. It was registered at the ClinicalTrials.GOV (NCT04503031).
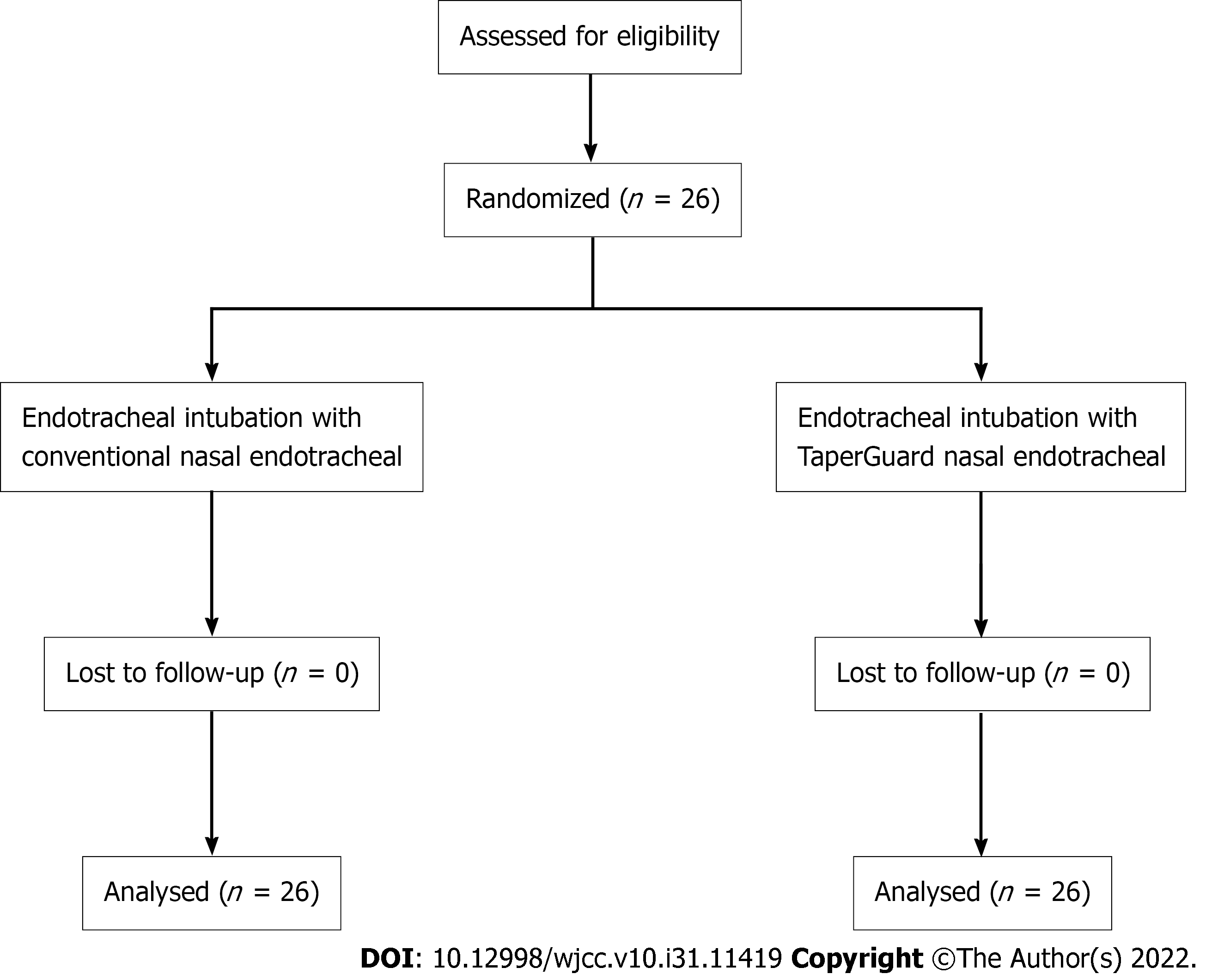
With computer-generated randomization method, patients were randomized into two groups by an anesthesiologist who was not involved in this trial: Group C (n = 26) were intubated with nasal conventional ET (Unomedical, Kedah, Malaysia) and Group T (n = 26) were intubated with nasal TaperGuard ET (Covidien, Athlone, Ireland). Nasal ET with a size of inner diameter 7.0 mm for male and 6.5 mm for female was used respectively.
No premedication was given. In the operating room, standard monitoring included noninvasive arterial blood pressure, pulse oximetry, electrocardiography and gas analyzer. Head ring (height: 2.5 cm) was placed under patient head. Propofol 2 mg/kg, and rocuronium 0.8 mg/kg were administered intravenously for induction of general anesthesia.
Nasal ET was softened in the warm sterile normal saline at 38°C 10 min before endotracheal intubation. The ET was lubricated with sterile, water-soluble jelly prior to intubation. Nasal endotracheal intubation was performed with a direct laryngoscope. The tip of ET was placed at 4 cm above carina using a fiberoptic bronchoscope (Olympus, Tokyo, Japan) in neutral position and ET was fixed with tape on the nares using tape. The tube cuff was inflated with air to attain a cuff pressure of 22 cmH2O using a manometer (Mallinckrodt Medical, Hennef, Germany). Pillow (height of 5 cm) was placed under shoulder to extend head and neck. The cuff pressure was evaluated again and readjusted to 22 cmH2O as necessary. In addition, the distance from the ET tip to the carina was assessed again using fiberoptic bronchoscope. The nasal endotracheal intubation was performed by the same anesthesiologist. The anesthesiologist measured cuff pressure and distance from the ET tip to carina. General anesthesia was provided with 2.0-2.5 sevoflurane with 50% oxygen in air and effect site concentration of remifentanil set at 1-3 ng/mL. Mechanical ventilation with a tidal volume of 8 mL/kg and respiratory rate of 10-12 cycle/min was set to maintain the end-tidal CO2 tension from 30 to 35 mmHg.
The incidence of airway complications such as hoarseness and sore throat was assessed during 24 h after surgery by a study blinded anesthesiologist. In this study the primary endpoint was the cuff pressure after head and neck extension. The secondary endpoint was the displacement of ET tip from carina after extension of head and neck and incidences of postoperative airway complications such as sore throat, and hoarseness.
A pilot study using 10 volunteers showed that cuff pressure of nasal TaperGuard ET was increased by 6.5 ± 1.9 (mean ± standard deviation) cmH2O after head extension from neutral position. In this study the differences in the mean cuff pressure between two groups was 50% considered as significant and it was calculated that 23 patients in each group were required with α = 0.05 and β = 0.2. Considering a 10 % drop out rate, 26 patients in each group were required.
Statistical analysis was performed using statistical software (SPSS, version 23.0 for Windows; SPSS, Chicago, IL). Student’s t test was used for analysis of continuous data such as cuff pressure and distance from the carina to tube tip. Fisher’s exact test or chi-squared test was used for analysis of categorial data sch as postoperative airway complications and the incidence of cuff pressure more than 30 cmH2O. A P-value less than 0.05 was considered to be statistically significant. Data were expressed as mean ± standard deviation or number (%).
Fifty-two patients were included in the present study (Figure 2). There were no differences between groups in terms of patient demographic data and intraoperative data (Table 1). The cuff pressure was significantly higher in the Tapered cuff than in the cylindrical cuff after extension of head and neck. (28.7 ± 1.0 cmH2O vs 25.5 ± 0.8 cmH2O) (P < 0.001). (Table 2). The incidence of cuff pressure more than 30 cmH2O was 11.5% in the TaperGuard group and 0% in the conventional group after head and neck extension. However, there was no statistical difference. After positional change, the degree of cephalad migration was greater in the TaperGuard group than in the conventional group (18.4 ± 2.2 mm vs 15.1 ± 1.1 mm, P < 0.001) (Table 2). The incidence of postoperative airway complications was comparable between two groups during 24 h after surgery (Table 3).
| Characteristics | Group C (n = 26) | Group T (n = 26) |
| Age, yr | 40.7 ± 14.5 | 38.1 ± 16.1 |
| Sex, M/F | 14/12 | 16/10 |
| Weight, kg | 59.8 ± 9.7 | 61.5 ± 8.1 |
| ASA (I/II/III) | 10/14/2 | 13/12/1 |
| Height, cm | 165.7 ± 8.6 | 167.2 ± 8.6 |
| Body mass index, kg/m2 | 21.6 ± 1.4 | 21.9 ± 1.2 |
| Duration of surgery, min | 154.5 ± 45.1 | 148. 4 ± 55.7 |
| Group C (n = 26) | Group T (n = 26) | P value | |
| Sore throat | 6 (23.1%) | 5 (19.2%) | 0.734 |
| Hoarseness | 3 (11.5%) | 5 (19.2%) | 0.442 |
In this study, the cuff pressure was significantly higher after extension of head and neck from neutral position in the TaperGuard ET than in the conventional ET during nasal endotracheal intubation. In addition, the ET tip was significantly displaced toward vocal cord in the TaperGuard ET, compared to the conventional ET.
The cuff diameter of cylindrical ET is equivalent to about 150% of the internal tracheal diameter. Therefore, upon inflation within the trachea, longitudinal folds or channels are made on the surface of cuff, leading to microaspiration and pneumonia[8,15]. The cuff of newly developed TaperGuard ET is distally tapered, which fits into tracheal diameter somewhere in the length when inflated in the trachea, leading to improving sealing effect[16,17].
The cuff pressure is affected by anesthetic gas such as nitrous oxide, which diffuses into the cuff, consequently resulting in an increase of cuff pressure[18,19]. Therefore, in the present study, general anesthesia was performed with remifentanil and sevoflurane.
The cephalad migration of ET occurs after extension of head and neck during oral or nasal endotracheal intubation[10]. In the present study, nasal ET migrated toward vocal cord after extension of head and neck, which is consistent with the previous study.
The trachea is not cylindrical and is surrounded by C shaped cartilage joined by a thin connective tissue. The tips of the C-shaped cartilages are closer to each other in the proximal region than in the distal region of the trachea and the tracheal compliance is higher in the proximal region than in the distal region[20,21]. In addition, the subglottic space at level of cricoid cartilage is the narrowest[22]. Boyle’s law is a gas law which states the pressure of a gas is inversely proportional to its volume at constant temperature within a closed system. When ET migrates toward vocal cord and the cuff is placed adjacent to narrower and less complaint upper airway structure such as cricoid cartilage, the cuff volume is compressed, leading to cuff pressure increment according to Boyles’ law[13,14] (Figure 3). In the recent study, the cuff pressure was significantly higher in the TaperGuard ET than in the conventional ET after changing from the supine to the lateral flank position, although the degree of cephalad migration of ET was comparable between two groups[13]. The TaperGuard ET with a tapered cuff has smaller cuff volume and narrower tracheal contact than conventional ET. Therefore, it was suggested that the geometric difference of ET cuff can account for the difference in the cuff pressure increment between two groups[13] (Figure 3). In the recent study, it was found that TaperGuard ET significantly moved toward vocal cord, compared to cylindrical cuff after head rotation during oral endotracheal intubation, which could be in part responsible for the difference of the cuff pressure between two groups[14]. In the present study, the increase of cuff pressure was significantly higher in the TaperGuard ET in the conventional ET after extension of head and neck during nasal endotracheal intubation. In addition, the degree of cephalad migration of ET was significantly greater in the TaperGuard group than in the conventional group.
In the present study, the frequency of postoperative airway complications including sore throat and hoarseness was comparable between groups. We readjusted cuff pressure to 22 cmH2O after head and neck extension, which may lead to no difference in the frequency of postoperative airway complications between two groups. However, it was difficult to clarify the relationship between the shape of ET cuff and airway complications due to small sample size. Therefore, further study is required to investigate the association between the shape of ET cuff and postoperative airway morbidity.
The present study has several limitations. First, this is a single blinded randomized study. The attending anesthesiologist is impossible to be blinded to the type of ET for nasal endotracheal intubation, which can be a source of bias. Second, anatomy of airway may differ between people. It was reported that intraluminal diameter of the subglottis and upper trachea of Indian population was less than that of western population[23]. This study was performed at single center including a relatively small size of only Asian population, which limited the ability to extrapolate the results beyond the selected population.
In conclusion, the cuff pressure significantly increased in the TaperGuard ET, compared to the conventional ET after head and neck extension during nasal intubation. In addition, the ET tip was significantly displaced toward vocal cord in the TaperGuard ET, compared to the conventional ET. Therefore, cuff pressure should be carefully monitored after positional change, particularly in when using TaperGuard ET during nasal endotracheal intubation.
The proper cuff pressure of endotracheal tube (ET) plays an important role in sealing the airway and preventing airway complications during mechanical ventilation. The cuff shape of ET affects the cuff pressure after positional change.
There are only a few studies investigating the cuff pressure change and the degree of migration of ET following anterior-posterior movement during nasal endotracheal intubation.
To compare cuff pressure between TaperGuard ET and conventional ET after extension of head and neck during nasal endotracheal intubation.
In this randomized clinical trial, patients were intubated with nasal conventional ET and nasal TaperGuard ET. After extension of head and neck, the cuff pressure and the degree of migration of tube was measured and postoperative airway complications were assessed.
The cuff pressure significantly increased in the TaperGuard ET, compared to the conventional ET. Additionally, the degree of cephalad migration of ET tip was greater in the TaperGuard ET. The incidence of postoperative airway complications was comparable between groups.
The increase of cuff pressure was higher in the TaperGuard ET than in the conventional ET after head and neck extension during nasal intubation. In addition, the cephalad migration of ET was greater in the TaperGuard ET than in the conventional ET.
The cuff pressure should be carefully monitored after positional change, particularly in when using TaperGuard ET during nasal endotracheal intubation. Further study is required to investigate the association between the shape of ET cuff and postoperative airway morbidity.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Anesthesiology
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Lin L, China; Singh A, India S-Editor: Chang KL L-Editor: A P-Editor: Chang KL
| 1. | Dullenkopf A, Schmitz A, Frei M, Gerber AC, Weiss M. Air leakage around endotracheal tube cuffs. Eur J Anaesthesiol. 2004;21:448-453. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Lorente L, Blot S, Rello J. Evidence on measures for the prevention of ventilator-associated pneumonia. Eur Respir J. 2007;30:1193-1207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 98] [Cited by in RCA: 95] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 3. | Seegobin RD, van Hasselt GL. Endotracheal cuff pressure and tracheal mucosal blood flow: endoscopic study of effects of four large volume cuffs. Br Med J (Clin Res Ed). 1984;288:965-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 365] [Cited by in RCA: 383] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 4. | Dobrin P, Canfield T. Cuffed endotracheal tubes: mucosal pressures and tracheal wall blood flow. Am J Surg. 1977;133:562-568. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 68] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Liu J, Zhang X, Gong W, Li S, Wang F, Fu S, Zhang M, Hang Y. Correlations between controlled endotracheal tube cuff pressure and postprocedural complications: a multicenter study. Anesth Analg. 2010;111:1133-1137. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 115] [Cited by in RCA: 136] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 6. | Geng G, Hu J, Huang S. The effect of endotracheal tube cuff pressure change during gynecological laparoscopic surgery on postoperative sore throat: a control study. J Clin Monit Comput. 2015;29:141-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 7. | Madjdpour C, Mauch J, Dave MH, Spielmann N, Weiss M. Comparison of air-sealing characteristics of tapered- vs. cylindrical-shaped high-volume, low-pressure tube cuffs. Acta Anaesthesiol Scand. 2012;56:230-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 31] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 8. | Dave MH, Frotzler A, Spielmann N, Madjdpour C, Weiss M. Effect of tracheal tube cuff shape on fluid leakage across the cuff: an in vitro study. Br J Anaesth. 2010;105:538-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 70] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Lucangelo U, Zin WA, Antonaglia V, Petrucci L, Viviani M, Buscema G, Borelli M, Berlot G. Effect of positive expiratory pressure and type of tracheal cuff on the incidence of aspiration in mechanically ventilated patients in an intensive care unit. Crit Care Med. 2008;36:409-413. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 72] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 10. | Hartrey R, Kestin IG. Movement of oral and nasal tracheal tubes as a result of changes in head and neck position. Anaesthesia. 1995;50:682-687. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 75] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 11. | Kim JT, Kim HJ, Ahn W, Kim HS, Bahk JH, Lee SC, Kim CS, Kim SD. Head rotation, flexion, and extension alter endotracheal tube position in adults and children. Can J Anaesth. 2009;56:751-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 79] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 12. | Rosero EB, Ozayar E, Eslava-Schmalbach J, Minhajuddin A, Joshi GP. Effects of Increasing Airway Pressures on the Pressure of the Endotracheal Tube Cuff During Pelvic Laparoscopic Surgery. Anesth Analg. 2018;127:120-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 13. | Kim HC, Lee YH, Kim E, Oh EA, Jeon YT, Park HP. Comparison of the endotracheal tube cuff pressure between a tapered- versus a cylindrical-shaped cuff after changing from the supine to the lateral flank position. Can J Anaesth. 2015;62:1063-1070. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 14. | Choi E, Park Y, Jeon Y. Comparison of the cuff pressure of a TaperGuard endotracheal tube and a cylindrical endotracheal tube after lateral rotation of head during middle ear surgery: A single-blind, randomized clinical consort study. Medicine (Baltimore). 2017;96:e6257. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Bernhard WN, Yost L, Joynes D, Cothalis S, Turndorf H. Intracuff pressures in endotracheal and tracheostomy tubes. Related cuff physical characteristics. Chest. 1985;87:720-725. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 65] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | D'Haese J, De Keukeleire T, Remory I, Van Rompaey K, Umbrain V, Poelaert J. Assessment of intraoperative microaspiration: does a modified cuff shape improve sealing? Acta Anaesthesiol Scand. 2013;57:873-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 27] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 17. | Zanella A, Scaravilli V, Isgrò S, Milan M, Cressoni M, Patroniti N, Fumagalli R, Pesenti A. Fluid leakage across tracheal tube cuff, effect of different cuff material, shape, and positive expiratory pressure: a bench-top study. Intensive Care Med. 2011;37:343-347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 89] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 18. | Tu H N, Saidi N, Leiutaud T, Bensai S, menival V, Duvaldestin P. Nitrous oxide increases endotracheal cuff pressure and the incidence of tracheal lesions in anesthetized patients. Anesth Analg 1999; 89: 187-190. [RCA] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 62] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 19. | Priebe HJ. N2O and endotracheal cuff pressure. Anesth Analg. 2000;90:230-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Vock P, Spiegel T, Fram EK, Effmann EL. CT assessment of the adult intrathoracic cross section of the trachea. J Comput Assist Tomogr. 1984;8:1076-1082. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 39] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 21. | Safshekan F, Tafazzoli-Shadpour M, Abdouss M, Behgam Shadmehr M, Ghorbani F. Investigation of the Mechanical Properties of the Human Tracheal Cartilage. Tanaffos. 2017;16:107-114. [PubMed] |
| 22. | Chan WH, Sung CW, Chang HC, Ko PC, Huang EP, Lien WC, Huang CH. Measurement of subglottic diameter and distance to pre-epiglottic space among Chinese adults. PLoS One. 2020;15:e0236364. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 23. | Prasanna Kumar S, Ravikumar A. Biometric study of the internal dimensions of subglottis and upper trachea in adult Indian population. Indian J Otolaryngol Head Neck Surg. 2014;66:261-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.0] [Reference Citation Analysis (0)] |