Published online Oct 26, 2022. doi: 10.12998/wjcc.v10.i30.11004
Peer-review started: May 8, 2022
First decision: July 12, 2022
Revised: July 31, 2022
Accepted: September 16, 2022
Article in press: September 16, 2022
Published online: October 26, 2022
Processing time: 165 Days and 14.5 Hours
Cutaneous squamous cell carcinoma (cSCC) is a common malignant hyperplasia of the skin epithelium. However, cSCC progressing to giant squamous cell carcinoma of the popliteal fossa skin has not been reported. We used full-thickness skin graft from the lower left quadrant of the abdomen to reconstruct the popliteal fossa skin defect in our patient.
A 64-year-old woman presented with a 3-year history of a progressively enlarged integumentary tumor located on her left popliteal fossa, which was surgically treated. The resultant defect (15 cm × 25 cm) was repaired using full-thickness skin graft from the lower left quadrant of the abdomen.
Full-thickness skin graft is a good choice to repair popliteal fossa defect.
Core Tip: We report an exceedingly rare case of giant cutaneous squamous cell carcinoma (maximum diameter > 5 cm), which presented as skin invasion of the popliteal fossa that was excised with optimal clinical result.
- Citation: Wang K, Li Z, Chao SW, Wu XW. Giant cutaneous squamous cell carcinoma of the popliteal fossa skin: A case report. World J Clin Cases 2022; 10(30): 11004-11009
- URL: https://www.wjgnet.com/2307-8960/full/v10/i30/11004.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i30.11004
Cutaneous squamous cell carcinoma (cSCC) is a non-melanoma skin and keratinocyte cancer, accounting for 20% of all skin cancers, and it is the second most common cancer worldwide[1]. Unfortunately, cSCC is not included in the national cancer registry in the United States, which makes it difficult for us to know the exact morbidity and mortality in China. European data show that the age-standardized incidence of cSCC is 9 to 96 cases per 100000 male residents and 5 to 68 cases per 100000 female residents (2002-2007 estimate)[2-4].
Although cSCC is mostly a benign tumor, it can locally infiltrate and metastasize. The 10-year survival rate of patients with cSCC is over 90%, but when metastasis occurs, the survival rate drops sharply[5]. The frequency of lymph node metastasis is about 4%, and the mortality is close to 2%. Because of the high incidence of cSCC, it has a significant impact on the overall mortality[6]. Furthermore, most cSCCs can be completely removed by surgery. cSCC of the popliteal fossa skin, which is a very rare site, is closely related to the knee joint and important neurovascular system, posing a surgical challenge for reconstruction. Herein, we report an exceedingly rare case of giant cSCC (maximum diameter > 5 cm), which presented as skin invasion of the popliteal fossa that was excised with optimal clinical result.
Three-year history of pain and mobility problems due to a progressively enlarged integumentary tumor located on the left popliteal fossa.
In June 2020, a 64-year-old woman presented with a 3-year history of pain and mobility problems due to a progressively enlarged integumentary tumor located on her left popliteal fossa.
This patient had no history of chronic diseases, such as hypertension, hyperuricemia, hyperlipidemia, and coronary heart disease.
The patient was a non-smoker and had no family history of cSCC.
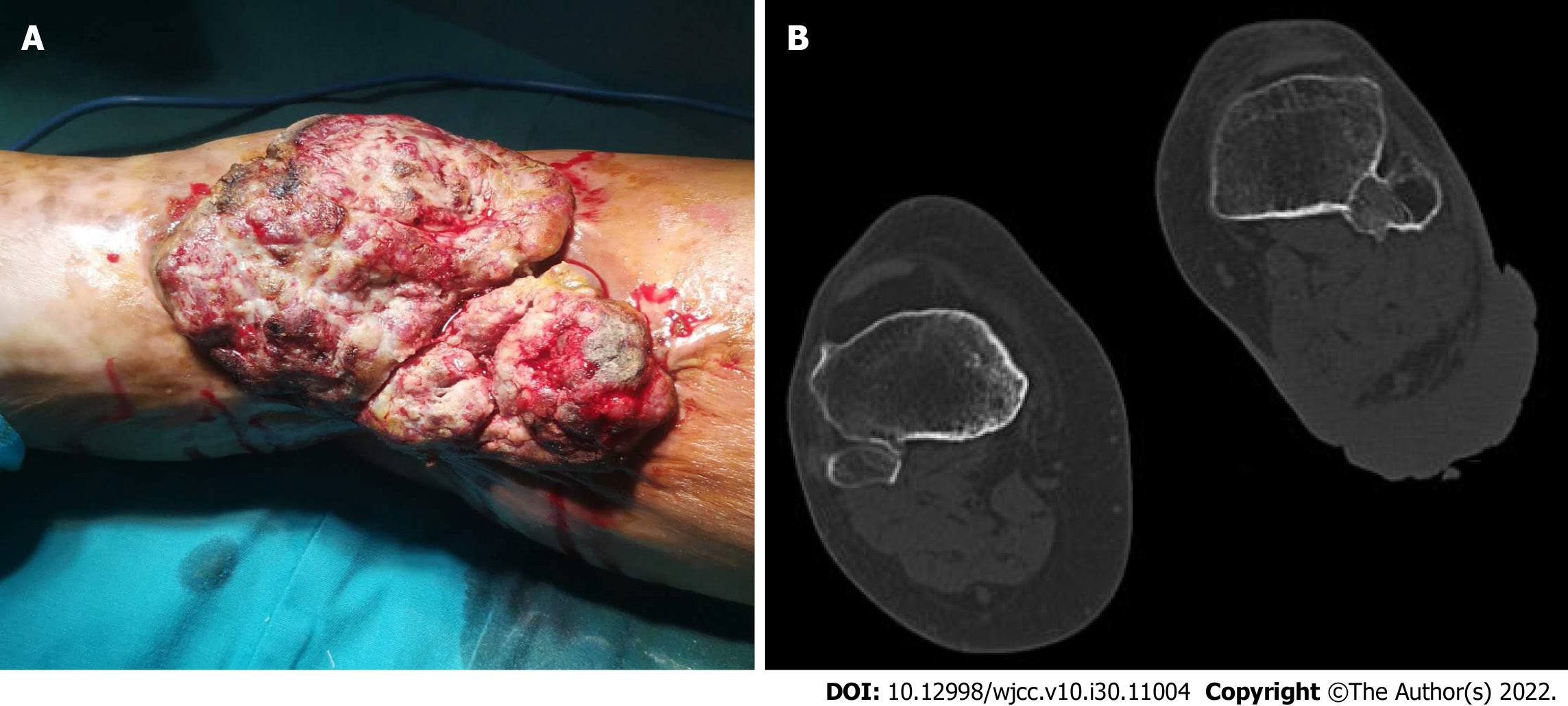
Physical examination showed an erythematous, nodular, protruding, ulcerative, mainly necrotic, foul smelling, cauliflower-like, firm skin tumor measuring 15 cm × 20 cm on the left popliteal fossa (Figure 1A). However, no significant lymph node or distant metastases were identified.
The laboratory results revealed that the level of squamous cell carcinoma antigen was 20 ng/mL, the C-reactive protein level was 15.5 mg/L, and the erythrocyte sedimentation rate was 42 mm/h. Other laboratory results were within the normal range.
Computed tomography showed that the tumor had infiltrated deep into the muscular layer of the left popliteal fossa, but not the skeletal layer (Figure 1B).
Giant cSCC of the popliteal fossa skin.
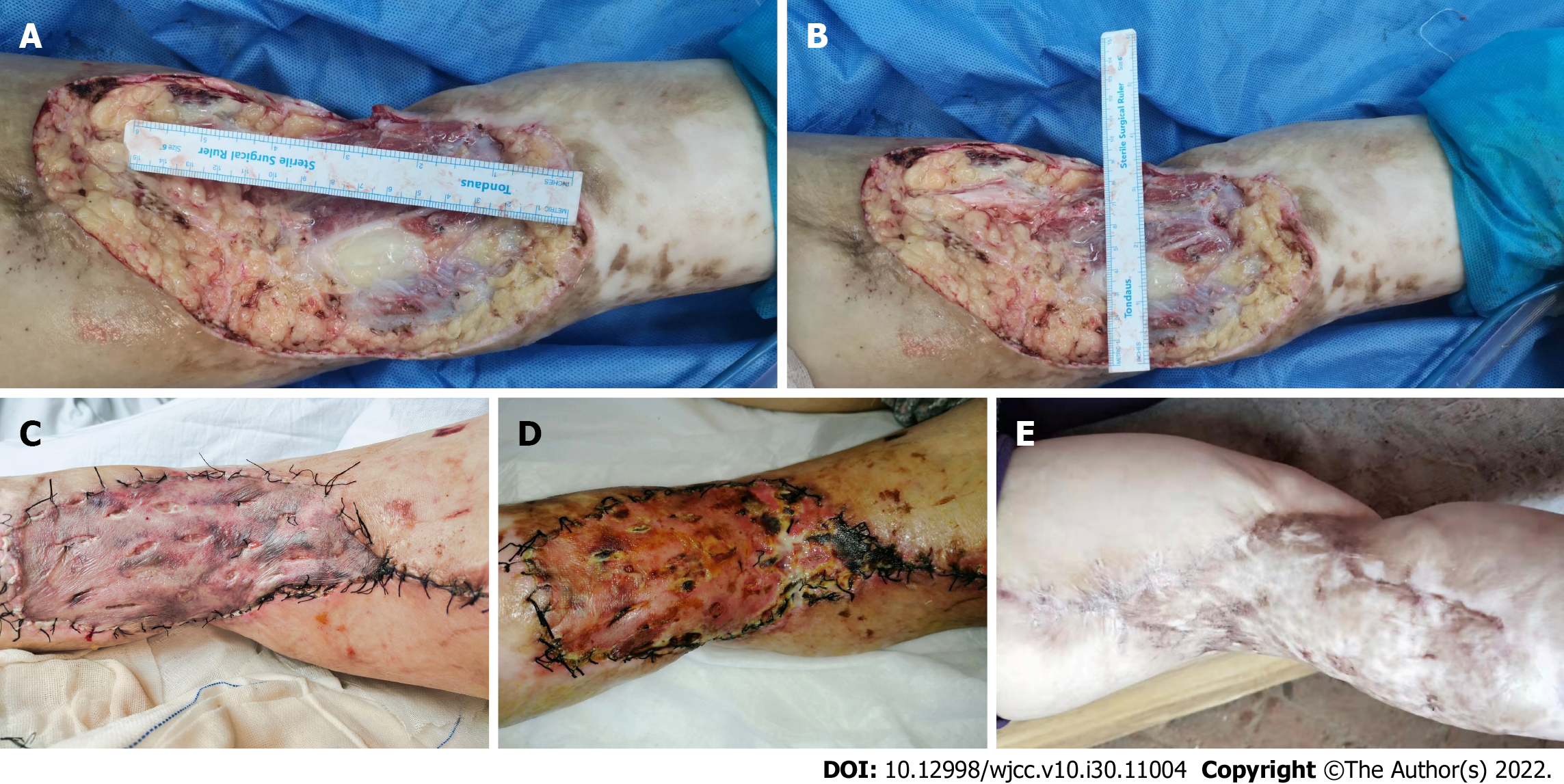
After popliteal fossa tumor excision and skin grafting, the tumor was totally excised. The tumor infiltrated the muscular layer and a 4 cm margin of muscular tissue was excised with the tumor. The final surgical defect measured 15 cm × 25 cm (Figure 2A and B). The surgical defect was repaired with a full-thickness skin graft from the lower left quadrant of the abdomen.
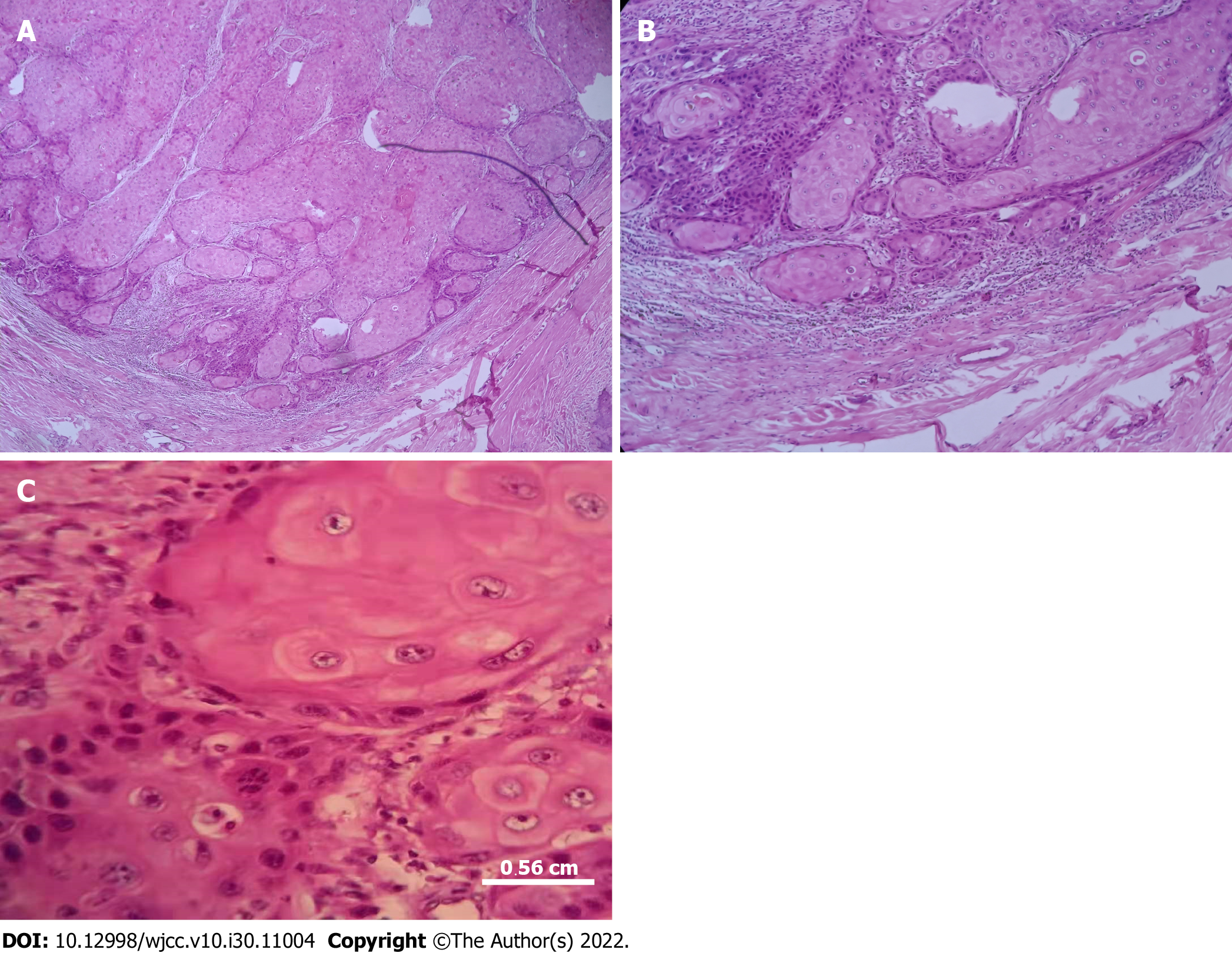
After surgery, the patient’s condition significantly improved (Figure 2C and D). Hematoxylin and eosin-stained section of the surgical specimen revealed an invasive, infiltrative well-differentiated cSCC (Figure 3). The patient was discharged 1 mo after operation, and had no recurrence and good wound healing after surgery. The patient was followed for one year after surgery (Figure 2E), without recurrent symptoms.
Although most cSCC cases have a good prognosis after surgical resection[7], 3.7%-5.2% of patients have lymph node metastasis, and 1.5%-2.1% of patients die of cSCC[8]. Although these incidences are relatively low compared with those of many other malignant tumors, the absolute number of cSCC patients with lymph node metastasis is estimated to be 5604 to 12572 in the United States alone[9]. In addition, the estimated number of cSCC-related deaths per year is between 3932 and 8791, and its upper limit is close to the number of melanoma-related deaths per year. Thus, it is important to identify such aggressive cSCC cases in time, which can guide additional testing and treatment to improve the prognosis[7].
Old age, fair skin, long-term sun exposure, long-term immunosuppression, and previous skin cancer diagnosis are all important risk factors for cSCC[10]. In addition, long-term skin inflammation seems to contribute to the development of cSCC, such as chronic wound, ulcer, sinus tract, burn, or scar[11]. This patient developed cSCC mainly due to repeated skin ulceration, leading to local chronic inflammation and popliteal squamous cell carcinoma, which not only affects the functional recovery of knee joint but also increases the probability of malignant degeneration and the difficulty of popliteal defect reconstruction.
Besides Bowen disease, keratoacanthoma (KA), and invariant cSCC classic variant described above, the pathological tissues of cSCC also have several types, such as fibroproliferative, spindle cell, keratolytic, pseudovascular, verrucous, wedge-shaped epithelioma, adenosquamous cell and neurotrophic cSCC[12]. Disordered maturation of atypical keratinocytes, single cell keratinization, nuclear pleomorphism, atypical mitosis, and multi-nucleated tumor cells appear in all epidermal layers, but the basal layer remains unchangedI[13]. KA is a symmetrical keratinocyte hyperplasia with limited proliferation, and its central horn plug and epidermis extend to the tumor. Histologically, invasive cSCC is characterized by atypical and abnormal keratinocytes, hyperchromic and pleomorphic nuclei, and atypical mitotic cells. Well-differentiated cSCC usually has horny pearls and single cell keratinization, while poorly differentiated cSCC usually lacks keratinization, and has many atypical mitoses and mixed inflammatory infiltration.
Pathological examination showed numerous squamous cells with keratosis and mitotic infiltration[13]. Considering that it was invasive cSCC with keratosis and no lymph node metastasis was found in our case, we performed surgery for complete tumor resection and skin grafting, and advised the patient to undergo regular postoperative reexamination.
The resection of cSCC at the popliteal fossa involves joint movement and numerous blood vessels and nerves. Therefore, it is critical to protect the important neurovascular system and prevent secondary scar contraction based on extensive activities of the popliteal fossa, which may be manifested as external aesthetic distortion and popliteal fossa retraction, thus seriously damaging the shape and function[14]. We chose a full- thickness skin graft from the lower left quadrant of the abdomen to repair the popliteal fossa defect. Full-thickness skin graft can survive on fresh sterile wounds or infected granulation wounds due to its characteristics of thin skin and strong vitality[15]. Additionally, the donor area is scar-free and cannot be easily infected[16]. In the present case, the patient could perform normal daily activities, without severe postoperative pain or any complications. Therefore, full-thickness skin repair is suitable for patients with popliteal cSCC who need extensive tumor resection, with fewer complications and faster postoperative recovery.
Full-thickness skin graft is a good alternative for the repair of popliteal fossa defects.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Oncology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): A
Grade B (Very good): 0
Grade C (Good): C, C, C, C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Aldiansyah D, Indonesia; Eccher A, Italy; Mijwil MM, Iraq; Ozden F, Turkey S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Chen YL
| 1. | Means AD, Leader NF, Siegel JA, Arron ST, Walker JL, Pomerantz H, Beatson M, Weinstock MA. Rate and Proportion of Malignant Skin Biopsies for Basal Cell and Squamous Cell Carcinoma on the Face and Ears After a Single Course of Topical 5-Fluorouracil: The Veterans Affairs Keratinocyte Carcinoma Chemoprevention Trial. Dermatol Surg. 2021;47:541-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 2. | Brewster DH, Bhatti LA, Inglis JH, Nairn ER, Doherty VR. Recent trends in incidence of nonmelanoma skin cancers in the East of Scotland, 1992-2003. Br J Dermatol. 2007;156:1295-1300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 92] [Cited by in RCA: 84] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Andersson EM, Paoli J, Wastensson G. Incidence of cutaneous squamous cell carcinoma in coastal and inland areas of Western Sweden. Cancer Epidemiol. 2011;35:e69-e74. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 4. | Katalinic A, Kunze U, Schäfer T. Epidemiology of cutaneous melanoma and non-melanoma skin cancer in Schleswig-Holstein, Germany: incidence, clinical subtypes, tumour stages and localization (epidemiology of skin cancer). Br J Dermatol. 2003;149:1200-1206. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 192] [Cited by in RCA: 200] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 5. | Varra V, Woody NM, Reddy C, Joshi NP, Geiger J, Adelstein DJ, Burkey BB, Scharpf J, Prendes B, Lamarre ED, Lorenz R, Gastman B, Manyam BV, Koyfman SA. Suboptimal Outcomes in Cutaneous Squamous Cell Cancer of the Head and Neck with Nodal Metastases. Anticancer Res. 2018;38:5825-5830. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 32] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 6. | Schmults CD, Karia PS, Carter JB, Han J, Qureshi AA. Factors predictive of recurrence and death from cutaneous squamous cell carcinoma: a 10-year, single-institution cohort study. JAMA Dermatol. 2013;149:541-547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 329] [Cited by in RCA: 411] [Article Influence: 34.3] [Reference Citation Analysis (0)] |
| 7. | Ferrarotto R, Amit M, Nagarajan P, Rubin ML, Yuan Y, Bell D, El-Naggar AK, Johnson JM, Morrison WH, Rosenthal DI, Glisson BS, Johnson FM, Lu C, Mott FE, Esmaeli B, Diaz EM Jr, Gidley PW, Goepfert RP, Lewis CM, Weber RS, Wargo JA, Basu S, Duan F, Yadav SS, Sharma P, Allison JP, Myers JN, Gross ND. Pilot Phase II Trial of Neoadjuvant Immunotherapy in Locoregionally Advanced, Resectable Cutaneous Squamous Cell Carcinoma of the Head and Neck. Clin Cancer Res. 2021;27:4557-4565. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 88] [Article Influence: 22.0] [Reference Citation Analysis (0)] |
| 8. | Kus KJB, Ruiz ES. Non-Surgical Treatments for Keratinocyte Carcinomas. Adv Ther. 2021;38:5635-5648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 9. | Rogers HW, Weinstock MA, Feldman SR, Coldiron BM. Incidence Estimate of Nonmelanoma Skin Cancer (Keratinocyte Carcinomas) in the U.S. Population, 2012. JAMA Dermatol. 2015;151:1081-1086. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 938] [Cited by in RCA: 1129] [Article Influence: 125.4] [Reference Citation Analysis (0)] |
| 10. | Knuutila JS, Riihilä P, Karlsson A, Tukiainen M, Talve L, Nissinen L, Kähäri VM. Identification of metastatic primary cutaneous squamous cell carcinoma utilizing artificial intelligence analysis of whole slide images. Sci Rep. 2022;12:9876. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 13] [Reference Citation Analysis (0)] |
| 11. | Zhang D, Yang Y, Liu J, Zhu T, Huang H, Zhou C. Severe inflammation in new-borns induces long-term cognitive impairment by activation of IL-1β/KCC2 signaling during early development. BMC Med. 2022;20:235. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 12. | Fania L, Didona D, Di Pietro FR, Verkhovskaia S, Morese R, Paolino G, Donati M, Ricci F, Coco V, Candi E, Abeni D, Dellambra E. Cutaneous Squamous Cell Carcinoma: From Pathophysiology to Novel Therapeutic Approaches. Biomedicines. 2021;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 145] [Article Influence: 36.3] [Reference Citation Analysis (0)] |
| 13. | Paolino G, Donati M, Didona D, Mercuri SR, Cantisani C. Histology of Non-Melanoma Skin Cancers: An Update. Biomedicines. 2017;5. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 63] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 14. | Lin SD, Chang KP, Lu DK, Lee SS, Lin TM, Tsai CC, Lai CS. Endoscope-assisted management of varicose veins in the posterior thigh, popliteal fossa, and calf area. Ann Plast Surg. 2002;48:10-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Lin TS, Jeng SF, Chiang YC. Resurfacing with full-thickness skin graft after debulking procedure for bulky flap of the hand. J Trauma. 2008;65:123-126. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Dessy LA, Figus A, Fioramonti P, Mazzocchi M, Scuderi N. Reconstruction of anterior auricular conchal defect after malignancy excision: revolving-door flap versus full-thickness skin graft. J Plast Reconstr Aesthet Surg. 2010;63:746-752. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 50] [Article Influence: 3.3] [Reference Citation Analysis (0)] |