Published online Oct 16, 2022. doi: 10.12998/wjcc.v10.i29.10689
Peer-review started: May 11, 2022
First decision: July 12, 2022
Revised: July 15, 2022
Accepted: August 30, 2022
Article in press: August 30, 2022
Published online: October 16, 2022
Processing time: 141 Days and 1.9 Hours
Intravesical explosion during transurethral resection of bladder tumor (TUR-BT) is a very rare complication, and it may result in rupture of the bladder, which us
This paper reports a case of intravesical explosion during TUR-BT. Combined with the literature review, the risk factors are analyzed and measures of pre
Although rare, intravesical explosions can cause serious consequences, and the loud explosion can also lead to a profound psychological shadow on the patient. Urologists must be aware of this potential complication. Careful operative tech
Core Tip: Transurethral resection of bladder tumor (TUR-BT) is the most common operation performed for non-muscle invasive bladder cancer. Although it is considered as a safe and minimally invasive procedure, occasionally life-threatening complications may be seen. Intravesical explosion is a very rare comp
- Citation: Xu CB, Jia DS, Pan ZS. Intravesical explosion during transurethral resection of bladder tumor: A case report. World J Clin Cases 2022; 10(29): 10689-10694
- URL: https://www.wjgnet.com/2307-8960/full/v10/i29/10689.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i29.10689
Transurethral resection of bladder tumor (TUR-BT) is the most common operation performed for non-muscle invasive bladder cancer. Although it is considered as a safe and minimally invasive procedure, occasionally life-threatening complications may be seen. Intravesical explosion, which was first reported in 1926 by Cassuto[1], is a very rare complication that can cause serious consequences, and the loud explosion can also lead to a profound psychological shadow on the patient. It may result in rupture of the bladder and has received special attention in consensus on safety of TUR-BT[2]. If bladder explosion happens and is not diagnosed and treated timely, it will cause serious consequences. Here, we present a case of intravesical explosion during TUR-BT leading to bladder rupture to remind urologists of this rare complication with suggestions on how to manage and prevent this complication.
A 44-year-old man was admitted to the hospital with painless gross haematuria that had persisted for 1 wk.
The patient experienced haematuria throughout urination, with blood clots, but without dysuria, frequent or urgent urination, or lower back pain.
The patient had a history of hypertension.
The patient had no personal and family history.
There was no specific physical examination.
Routine urine test and microscopic examination showed plenty of red cells.
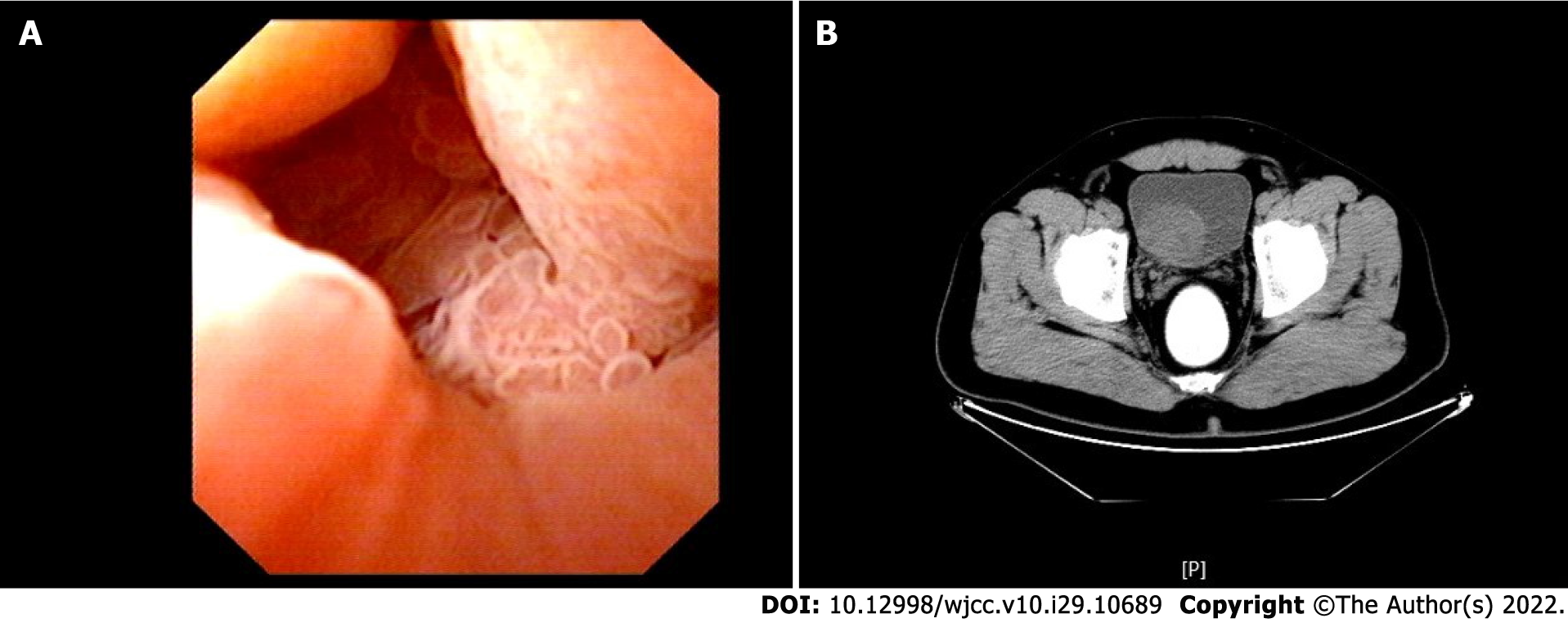
Ultrasound showed multiple irregular, heterogeneous, slightly high echoes in the bladder, of which the smallest was located in the left bladder wall (approximately 7 mm × 5 mm in size) and the largest one in the right posterior wall (approximately 61 mm × 47 mm in size). Colour Doppler flow imaging detected obvious blood flow signals within the region. Cystoscopy identified many cauliflower-like tumors in the left apical and posterior walls of the bladder (Figure 1A), the largest of which was in the posterior wall of the bladder, with local necrosis and bleeding. Computed tomography (CT) examination showed a tumor in the right lateral wall of the bladder (Figure 1B). Despite its size, this could not be visualised entirely because of its location. There was no obvious abnormality in the ureteral orifice.
Pathological examination indicated possible high-grade urothelial carcinoma. The recommended surgical procedure was radical cystectomy combined with urinary diversion. However, the patient was still young and was unwilling to undergo cystectomy. Therefore, after some discussion, we performed a TUR-BT.
The patient was placed under general anaesthesia. An Olympus F24 plasma resectoscope was used intraoperatively. We used 0.9% warm normal saline as a flushing solution, and the monopolar electrocautery current was set at 120 W for coagulation and 280 W for cutting. The tumor was located and found to have a wide base and an extensive range. Resection was performed using step-by-step electroexcision. However, the surgical field of vision was poor because of the large tumor size and its abundant blood supply, which resulted in substantial haemorrhage. There was also an accumulation of resected tumor tissue in the bladder. The excised tissue was repeatedly rinsed using Ellikrinser. After approximately 120 min, we encountered difficulty accessing the tumor tissue in the apical wall of the bladder with the electric cutting ring. The assistant pressed down on the abdomen for assistance, and an explosive bang sound was emitted from the lower abdomen, leading to the blurring of the field of vision of the resectoscope and failure of bladder filling. We surmised this to be a bladder rupture, and an exploratory laparotomy was performed immediately. During this procedure, the bladder was broken into several irregular pieces, with irregular wound margins, a lacerated appearance, and active bleeding. The rupture was traced to the abdominal cavity. Approximately 300 mL of light red liquid was sucked out of the abdominal cavity. No obvious damage was found to the intestines or other abdominal structures, but a large number of blood clots were found in the bladder. Following careful exploration of the bleeding sites and complete haemostasis, the residual tumor tissue was completely resected, after which the bladder was checked carefully. No other lesions were found, and the urine spraying at the bilateral ureteral orifices showed no abnormality. After trimming the wound margin of the bladder and confirming that there was no further bleeding, the muscular layer and serosa layer were continuously sutured with 2.0 absorbable sutures. A test of bladder infusion showed no suture leakage. The pelvic and abdominal drainage tubes were placed, and the incision closed.
The drainage tubes were removed after 1 wk, and the urinary tube after 2 wk. There were no abnormalities in urinary function. The patient received two cycles of gemcitabine and cisplatin chemotherapy combined with regular intravesical gemcitabine. Both CT and cystoscopy at the 3-mo postoperative review revealed no abnormalities of the bladder or abdominal cavity. The patient had three recurrences of bladder tumors in the next 3 years and was treated in each instance by TUR-BT because of the smaller size of the tumors. The patient has received regular follow-ups up to the present time without further tumor recurrence.
Intravesical explosion is rare in TUR of the prostate (TURP) with a low incidence during TUR-BT. We conducted a Chinese and English literature review through the PubMed database and the Wanfang database for research on bladder explosions up to December 2021. Only three papers related to TUR-BT, and the rest related to TURP. TUR-BT and TURP are both transurethral procedures for conditions with similar causes, clinical manifestations, treatments, and preventative measures. Martov et al[3] investigated 5401 cases of intraoperative and postoperative complications of TURP, and one case of bladder gas explosion was found. This case developed into bladder rupture. Liu et al[4] conducted a retrospective analysis of the surgical data from 1950 cases of benign prostatic hyperplasia and found four cases of bladder gas explosion followed by bladder repair, amounting to an incidence of < 0.2%. In most cases, bladder gas explosion is characterised by a dull explosive sound in the middle to late stage of the operation, without obvious damage to the bladder and with no special treatment required. In instances where a mild injury occurs, it is in the form of congestion and slight tearing and bleeding of the bladder mucosa, which can be treated by electrosurgical resection and haemostasis. When a severe injury occurs, it is predominantly bladder rupture. Intraperitoneal injury is more common than extraperitoneal[5,6]. At this time, there are no reports in the literature of abdominal involvement or major vascular injury induced by bladder gas explosion. However, Seitz et al[7] have reported a case requiring expanded excision of the bladder due to poor blood supply at the bladder wound margin. In another case, the bladder repair was further complicated by bladder dehiscence due to the severe damage and this had required a second repair[8]. Additionally, improper treatment of fluid and electrolyte disorders can lead to patient mortality[9]. Therefore, in cases of bladder rupture, open or laparoscopic bladder repair must be performed on time, with additional attention paid to any injury of the intestinal tract or surrounding structures. As suggested by Georgios et al[10], laparoscopic repair of the bladder has the advantages of reducing surgical trauma, enabling easy aspiration of fluid in the abdominal cavity, and facilitating more comprehensive observation of the abdominal organs. However, open surgery is more advantageous for cases with large, irregular, and numerous bladder lacerations. Another serious problem of intravesical explosion is seeding of the tumor cells caused by intraperitoneal bladder rupture. Bus et al[11] reported the first case of tumor seeding to both adnexa in a patient with low grade urotherlial cancer conservatively treated by TUR-BT that had intraperitoneal perforation.
An intravesical explosion is a violent chemical reaction of combustible gas under specific conditions. Bladder rupture may occur when the volume of gas and liquid that the bladder contains exceeds its maximum capacity. A gas explosion requires certain physical and chemical conditions, including a combustion agent (e.g., hydrogen), an oxidant (e.g., oxygen), and an ignition source (e.g., an electric spark). During transurethral surgery, the heat of electroexcision may induce cellular inflammation, rupture, and gasification. The water content of the cells can then evaporate, leading surgical electrocoagulation to deform proteins and destroy cell walls[12]. Ning et al[13] analysed the gas produced by electrocautery of tissues through in vitro experiments and found its composition to include 40%-50% hydrogen and less than 3% oxygen. Similar results have been reported by Davis[14]. These concentrations of gases are not sufficient to produce an explosion, suggesting that electroexcision or electric coagulation alone does not cause intravesical explosions. It has been proposed that with a 40% volume ratio of hydrogen in the combustible gas generated by electroexcision, 11.4%-90.6% oxygen is required to induce a hydrogen explosion. Therefore, the accidental intraoperative introduction of air via a poorly sealed endoscopic sheath, through the flushing tube during the continuous bladder irrigation, or during repeated rinsing with Ellik, can provide sufficient oxidant for the gas to become explosive. The gas in the bladder accumulates when the operation is lengthy. In the present case, surgery was prolonged because of the large tumor size, massive haemorrhage, quantity of resected tissue, and repeated rinsing to clear the visual field. Air was introduced into the bladder during rinsing, resulting in the internal oxygen concentration required for a hydrogen explosion. Hydrogen has an extremely low minimum ignition energy of 0.019 mJ[15]. The electric spark produced by electroexcision using an electric cutting ring or electric coagulation may ignite the mixed gases. The energy released by an explosion will determine the extent of the damage. Bladder rupture occurs when the pressure generated by the explosion exceeds that which can be borne by the bladder wall. Multiple trabeculations and bladder diverticulum have been identified as risk factors for bladder explosion and rupture[16]. Presently, most scholars believe that the flushing solution does not affect bladder explosion, with no reported cases being caused by mannitol, glucose, or normal saline. Additionally, neither intraspinal anaesthesia nor general anaesthesia has any obvious relationship with bladder explosion. However, Hirai et al[17] have reported a case of bladder explosion caused by anaesthesia by nitrous oxide (N2O) inhalation. This was due to the flammable and explosive nature of N2O in confined spaces (such as the bladder).
In addition to the aforementioned objective contributors, there may also be human factors involved in bladder explosion. These can include the habits, safety awareness, and experience and personality of the surgeon. For instance, some surgeons are used to performing cystostomies before complex TURs. This can certainly increase the risk of bladder tumor dissemination but can avoid the accumulation of gas in the bladder[18]. Some surgeons adhere to the principle that safety is the top priority and adhere rigidly to the operation specifications. They may avoid the introduction of air and carefully observe any gas accumulation in the bladder intraoperatively, ensuring that it is discharged before there is excessive build-up. Other surgeons may have insufficient surgical experience or poor safety awareness. They may be impatient, make rash decisions during operations, or ignore surgical specifications.
Our literature review suggests a lower incidence of bladder explosions in TUR-BT than in TURP. When removing tumors in the trigone, lateral, and posterior walls of the bladder, keeping an adequate distance from the gas accumulation area of the anterior wall may reduce the risk of bladder explosion. Operations may be disturbed by bubbles when removing tumors from the anterior and apical walls. When this occurs, surgeons usually discharge the gas or change the body position to avoid bubble interference during TUR-BT. However, the prostate has a relatively fixed position in TURP, and removal of the tissue at the 12 o’clock position carries a high risk of disturbing gas accumulated in the anterior wall of the bladder and causing an explosion. Hence, the conditions necessary for bladder explosion are less frequently met during TUR-BT, resulting in a lower incidence.
Special precautions should be taken to avoid bladder explosion during transurethral surgery. First, the risk of explosion can be reduced with the use of low or medium power as this reduces the energy of the ignition source and lowers the local temperature during the electroexcision and electrocoagulation processes. Second, to carefully check for gas mixing in the flushing solution and to minimise the flushing times, maintaining a tight connection on the endoscopic sheath is important. The Ellik should be filled with normal saline during each flushing. Third, despite the inevitable generation of combustible gas, bladder explosion can be avoided by discharging the build-up of gas within the bladder promptly. An appropriate method for achieving this has been proposed in previous research[19]. The procedure is to tilt the resectoscope towards the top of the bladder and align it with the bubbles, close the exhalant canal, unplug the water inlet, and open the water inlet control valve to discharge the bubbles. Fourth, the duration of electroexcision should be kept to a minimum to reduce gas production, and this is best achieved through the adoption of punctate electroexcision and electrocoagulation to avoid blind inch-by-inch electrocoagulation. Fifth, the surgical position can be adjusted according to the intraoperative situation to change the bubble position. In this way, the surgeon can avoid contact between the gas bubbles and the electric spark produced by the electric cutting ring. Lastly, it is critical to be fully conversant with the operation indications and to conduct a thorough assessment of the surgical difficulty and risks. In our case, bladder explosion occurred because TUR of the bladder was an inappropriate treatment given the large tumor size. This led to the generation of a considerable amount of flammable gas because of the duration of the operation and the introduction of a great deal of air during repeated flushing. After this bladder explosion incident, our team conducted a systematic analysis and evaluation to improve operational details and raise surgeons’ awareness of the risk of such events. There have been no further intravesical explosions at our institution since this case.
Although rare, intravesical explosions can cause serious consequences, and the loud explosion can also lead to a profound psychological shadow on the patient. Urologists must be aware of this potential complication. Careful operative techniques and special precautions can reduce the risk of this complication.
Provenance and peer review: Unsolicited article; Externally peer reviewed
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hakimi T, Afghanistan; Markic D, Croatia S-Editor: Wang JJ L-Editor: Wang TQ P-Editor: Wang JJ
| 2. | Wang XH, Qi L, He DL. Consensus on safety of transurethral plasma resection of bladder tumors. J Modern Urol. 2018;23:895-901. [DOI] [Full Text] |
| 3. | Martov AG, Kornienko SI, Gushchin BL, Ergakov DV, Sazonov OA. [Intraoperative urological complications in transurethral surgical interventions on the prostate for benign hyperplasia]. Urologiia. 2005;3-8. [PubMed] |
| 4. | Liu HQ, Chen YS, Zou B, Kong J, Tao LS, Zhu GB. Serious complications of transurethral resection of the prostate. Chin J Urol. 2016;37:515-518. [DOI] [Full Text] |
| 5. | Di Tonno F, Fusaro V, Bertoldin R, Lavelli D. Bladder explosion during transurethral resection of the prostate. Urol Int. 2003;71:108-109. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Dublin N, Razack AH, Loh CS. Intravesical explosion during transurethral resection of the prostate. ANZ J Surg. 2001;71:384-385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Seitz M, Soljanik I, Stanislaus P, Sroka R, Stief C. Explosive gas formation during transurethral resection of the prostate (TURP). Eur J Med Res. 2008;13:399-400. [PubMed] |
| 8. | Ribeiro da Silva MN, Lopes Neto AC, Zambon JP, Verotti MJ, Wroclawski ER. Vesical explosion during transurethral resection of the prostate: report of a case. Arch Esp Urol. 2006;59:651-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 9. | Vacchiano G, Rocca A, Compagna R, Zamboli AGI, Cirillo V, Di Domenico L, Di Nardo V, Servillo G, Amato B. Transurethral Resection of the Prostate, Bladder Explosion and Hyponatremic Encephalopathy: A Rare Case Report of Malpractice. Open Med (Wars). 2017;12:50-57. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 10. | Georgios K, Evangelos B, Helai H, Ioannis G. Intravesical explosion during transurethral electrosurgery. Scott Med J. 2015;60:e25-e26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Bus MT, Cordeiro ER, Anastasiadis A, Klioueva NM, de la Rosette JJ, de Reijke TM. Urothelial carcinoma in both adnexa following perforation during transurethral resection of a non-muscle-invasive bladder tumor: a case report and literature review. Expert Rev Anticancer Ther. 2012;12:1529-1536. [PubMed] [DOI] [Full Text] |
| 12. | Liu S, Liu YH. High frequency electrotome and safe clinical use. Chin J Pract Sur. 2005;25:383-384. |
| 13. | Ning TC Jr, Atkins DM, Murphy RC. Bladder explosions during transurethral surgery. J Urol. 1975;114:536-539. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Davis TR. The composition and origin of the gas produced during urological endoscopic resections. Br J Urol. 1983;55:294-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 15. | He LQ. Gas combustion. In: Fire combustion science. Beijing: China Machine Press, 2014: 129-143. |
| 16. | Vincent DP. Bladder explosion during transurethral resection of prostate: Bladder diverticula as an additional risk factor. Urol Ann. 2017;9:68-70. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 17. | Hirai E, Tokumine J, Lefor AK, Ogura S, Kawamata M. Bladder Explosion during Transurethral Resection of the Prostate with Nitrous Oxide Inhalation. Case Rep Anesthesiol. 2015;2015:464562. [PubMed] [DOI] [Full Text] |
| 18. | Chang SS, Boorjian SA, Chou R, Clark PE, Daneshmand S, Konety BR, Pruthi R, Quale DZ, Ritch CR, Seigne JD, Skinner EC, Smith ND, McKiernan JM. Diagnosis and Treatment of Non-Muscle Invasive Bladder Cancer: AUA/SUO Guideline. J Urol. 2016;196:1021-1029. [PubMed] [DOI] [Full Text] |
| 19. | Takeshita H, Moriyama S, Chiba K, Noro A. A simple technique for evacuating air bubbles with scum from the bladder dome during transurethral resection of bladder tumor. Wideochir Inne Tech Maloinwazyjne. 2014;9:619-622. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |