Published online Oct 6, 2022. doi: 10.12998/wjcc.v10.i28.10031
Peer-review started: September 15, 2021
First decision: January 22, 2022
Revised: February 15, 2022
Accepted: August 25, 2022
Article in press: August 25, 2022
Published online: October 6, 2022
Processing time: 377 Days and 4 Hours
Parathyroid adenoma (PA) sometimes recurs after surgery, how to improve the surgical success rate of PA is the key to the treatment of this disease.
To investigate the clinical features, diagnosis, and surgical treatment of patients with PA.
Patients who were pathologically confirmed with PA and had undergone surgery for the first time between January 2010 and December 2017 at the Beijing Shijitan Hospital affiliated to Capital Medical University were included in the study. The clinical features, localization diagnosis, and surgical treatment of these patients were analyzed.
Of the 140 patients, 32 were male and 108 were female; 132 cases had one adenoma, and 8 had two adenomas. In addition, 114 cases had clinical symptoms, among which 51, 28, 23, 8, and 4 had urinary system, skeletal system, digestive system, neuromuscular system, and neuropsychiatric symptoms, respectively, while 26 cases had no obvious symptoms. The median level of preoperative parathyroid hormone (PTH) was 201.0 pg/mL. The positive detection rate of technetium-99m sestamibi (Tc-99m MIBI) single-photon emission computed tomography/computed tomography (SPECT/CT), ultrasound examination, and the combined use of Tc-99m MIBI SPECT/CT and ultrasound examination was 92.9%, 85.5%, and 96.4%, respectively. Open surgery was performed in all patients, and PTH was monitored during surgery. The success rate of surgery was 98.6%. After surgery, 21 cases developed hypocalcemia, 1 case developed temporary hoarseness, and 19 cases had transient hypoparathyroidism but there was no permanent hypoparathyroidism, postoperative hemorrhage, or hematoma in the surgical area.
For patients with clinically unexplained skeletal system, urinary system, and neuropsychiatric symptoms, the possibility of PA should be considered. Imaging examinations such as ultrasound and Tc-99m MIBI SPECT/CT could be integrated before surgery to obtain accurate localization diagnosis. Precise preoperative localization, intraoperative PTH monitoring, and delicate surgery to protect the integrity of the PA capsule ensure a minimally invasive and successful surgery.
Core Tip: In this study, we retrospectively analyzed the clinical data of 140 patients with parathyroid adenoma (PA). We found that, for patients with clinically unexplained skeletal system, urinary system, and neuropsychiatric symptoms, the possibility of PA should be considered. Imaging examinations such as ultrasound, technetium-99m sestamibi single-photon emission computed tomography/computed tomography could be integrated before surgery to obtain accurate localization diagnosis. Precise preoperative localization, intraoperative parathyroid hormone monitoring, and delicate surgery to protect the integrity of the PA capsule ensure a minimally invasive and successful surgery.
- Citation: Peng ZX, Qin Y, Bai J, Yin JS, Wei BJ. Analysis of the successful clinical treatment of 140 patients with parathyroid adenoma: A retrospective study. World J Clin Cases 2022; 10(28): 10031-10041
- URL: https://www.wjgnet.com/2307-8960/full/v10/i28/10031.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i28.10031
In recent years, the incidence of primary hyperparathyroidism has gradually increased. In some European countries and the Americas, primary hyperparathyroidism has become the third most common endocrine disease[1]. Due to the widespread application of various examination methods, especially neck ultrasound, the detection rate of parathyroid adenoma (PA) has gradually increased[2-4]. PA secretes parathyroid hormone (PTH) autonomously and is one of the most common causes of primary hyperparathyroidism, accounting for > 85% of the condition. PA can lead to elevated blood calcium in the body, resulting in hypercalcemia and even hypercalcemia crisis, in turn giving rise to symptoms, such as bone pain, fatigue, osteoporosis, muscle pain, nausea, and vomiting. Also, sym
Patients who were pathologically confirmed to have PAs and underwent surgery for the first time between January 2010 and December 2017 in the Beijing Shijitan Hospital affiliated to Capital Medical University were included in this study. The follow-up period was 3 years in all patients, and those who were lost to follow-up were excluded. This study was approved by the Institutional Review Board and Ethics Committee of Beijing Shijitan Hospital, Capital Medical University. According to the Ethics Committee policy, this is an anonymous, retrospective study exempt from obtaining informed consent from the patients.
SPSS 19.0 (IBM, Chicago, IL, United States) software was utilized. All continuous data were tested for normal distribution, and the continuous data conforming to normal distribution were expressed as mean ± SD, while the median (interquartile range) was used for continuous data that did not conform to the normal distribution, and the frequency (percentage) was used for enumeration data. Student’s t-test was used to assess the two-sample data that conformed to the normal distribution. χ2 test was used to compare the rates of the two groups, and P < 0.05 indicated a statistically significant difference.
A total of 140 patients were included, 32 were males with a mean age of 57.1 ± 17.1 years. The mean age of 108 females was 57.5 ± 14.2 years. The male:female ratio was 1.0:3.4.
The majority of patients (114/140) were symptomatic. The proportion of patients with urinary, skeletal, digestive, neuromuscular, and neuropsychiatric symptoms was 36.4%, 20%, 16.4%, 5.7%, and 2.9%, respectively. A total of 26 patients had no obvious symptoms, but they were admitted to the hospital due to high blood calcium or occupation in parathyroid glands observed during ultrasound exa
| Clinical symptoms | Number of patients, n (%) |
| Urinary system symptoms | 51 (36.4) |
| Skeletal system symptoms | 28 (20.0) |
| Digestive system symptoms | 23 (16.4) |
| Neuromuscular system symptoms | 8 (5.7) |
| Psychiatric symptoms | 4 (2.9) |
| Asymptomatic | 26 (18.6) |
All 140 patients underwent laboratory tests to measure blood calcium, blood phosphorus, PTH, alkaline phosphatase (ALP), creatinine (Cr), uric acid (UA), 24 h urinary calcium (24 h-UCa), and 24 h urinary phosphorus (24 h-UP) before surgery. The average values are shown in Table 2.
| Laboratory test | Mean/median | Reference range |
| Blood calcium | 2.84 ± 0.34 mmol/L | 2.2-2.7 mmol/L |
| Blood phosphorus | 0.84 ± 0.29 mmol/L | 0.85-1.51 mmol/L |
| PTH | 201.0 pg/mL (99.8 pg/mL) | 12-88 pg/mL |
| ALP | 97 U/L (20.1 U/L) | 45-125 U/L |
| BUN | 5.20 ± 1.74 mmol/L | 2.86-7.14 mmol/L |
| Cr | 64.81 ± 30.55 μmol/L | 57-97 μmol/L |
| UA | 345.95 ± 94.73 μmol/L | 208-428 μmol/L |
| 24 h-UCa | 8.99 ± 3.49 mmol/24 h | 0-7.5 mmol/24 h |
| 24 h-UP | 15.70 ± 7.46 mmol/24 h | 12.9-42.0 mmol/24 h |
Of the 140 patients with PAs, 132 had one adenoma and 8 had two adenomas. The total number of lesions was 148. The positive detection status of different imaging examinations was as follows: All 140 cases underwent ultrasound examination, in which the intraoperative lesion locations were consistent with the pre-localization in 120 cases. Accurate localization of the lesion site before surgery failed in 20 cases, and the positive detection rate was 85.5% (120/140). Fifty-four cases (54/140) underwent a CT scan with contrast examination, in which the preoperative localization was consistent with that of intraoperative localization in 41 cases; accurate localization of the lesion before surgery failed in 13 cases, and the positive detection rate was 75.9% (41/54). Thirty cases (30/140) underwent a MRI scan with contrast examination, in which 23 cases had the same preoperative localization as during surgery, and accurate localization of the lesion before surgery failed in 7 cases; the positive detection rate was 76.7% (23/30). All 140 cases underwent Tc-99m MIBI SPECT/CT examination, in which 130 cases had the same preoperative localization as during surgery, and accurate localization of the lesion before surgery failed in 10 cases; the positive detection rate was 92.9% (130/140). The combination of ultrasound and Tc-99m MIBI SPECT/CT examination showed that the preoperative localization of 135 patients was consistent with the intraoperative localization, while the lesion was not accurately positioned before surgery in 5 cases; the positive detection rate was 96.4% (Table 3).
| Imaging methods | Number of inspected cases | Exact number of patients | Positive detection rate |
| Ultrasound | 140 | 120 | 85.7% |
| Tc-99m MIBI SPECT/CT | 140 | 130 | 92.9% |
| CT scan with contrast | 54 | 41 | 75.9% |
| MRI with contrast | 30 | 23 | 76.7% |
| Ultrasound + Tc-99m MIBI SPECT/CT | 140 | 135 | 96.4% |
Of 140 patients, 122 (87.1%) had mildly elevated blood calcium without special treatment; 14 (10.0%) had obviously elevated blood calcium but did not have a hypercalcemia crisis (blood calcium ≤ 3.4 mmol/L), all these patients were treated with rehydration therapy (oral or intravenous injection of normal saline) and diuretics; and 4 (2.9%) had hypercalcemia crisis (blood calcium > 3.4 mmo/L), in addition to rehydration therapy and diuresis, they were also treated with pamidronate and calcitonin to lower blood calcium.
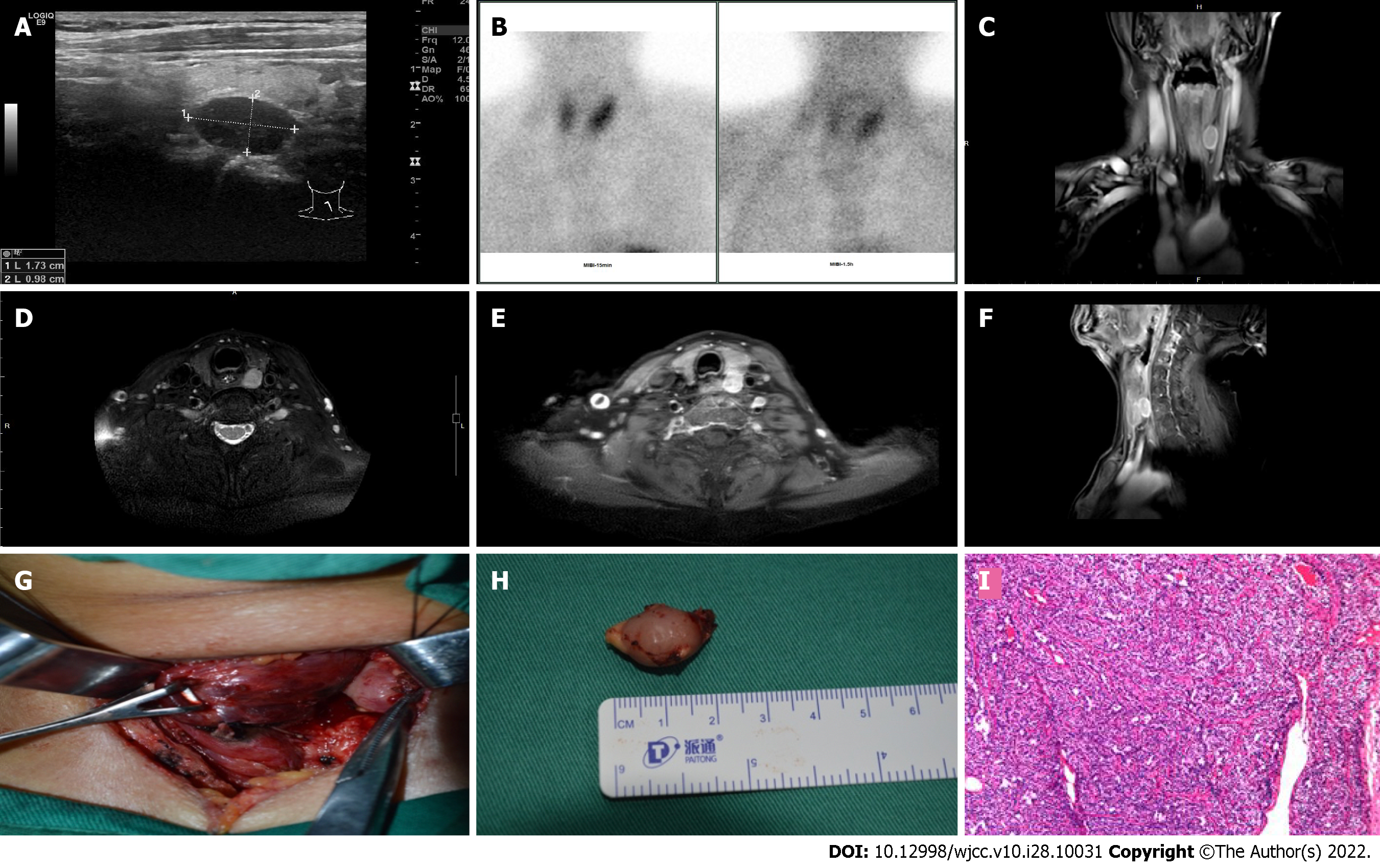
All patients underwent open surgery under general anesthesia. A collar incision was made along the neck dermatoglyphic. The skin and subcutaneous tissue were cut, the skin flap was separated under the platysma muscle, the band muscle was separated along the white line of the neck, the thyroid gland was exposed, and the thyroid lobe was drawn to the trachea. According to the preoperative localization diagnosis, the neck was explored to detect the PA, the recurrent laryngeal nerve was exposed and protected, the integrity of the PA capsule was maintained, and then the PA was removed (Figure 1). PTH was monitored during surgery. The PTH level of the peripheral vein before surgery was used as the baseline. The PTH level of the peripheral vein was detected again at 5 min, 10 min, and 15 min after the adenoma was removed. If the PTH level after resection of the specimen was at least 50% lower than that before resection of the specimen, surgery was deemed successful. If there was no significant change in the PTH level after removal of the specimen, this indicated the presence of residual lesion or multiple lesions, thereby necessitating further exploration of other parts of the neck: the superior sternal fossa, upper mediastinum, carotid sheath, and intra-thyroid gland. All 140 patients underwent intraoperative frozen pathological examination and postoperative routine pathological examination, and the consistency between the two examinations was 100%. Among these patients with PAs, 19 underwent bilateral parathyroid exploration (including 6 cases of non-ipsilateral double adenomas) and 121 cases underwent unilateral parathyroid exploration (including 2 cases of ipsilateral double adenomas) (Table 4). Among 140 patients with PAs, 5 cases had PA combined with papillary thyroid carcinoma; 3 underwent PA resection + total thyroidectomy + central lymph node dissection and 2 cases underwent PA resection + unilateral thyroid gland and isthmus resection + unilateral level VI (central neck) lymph node dissection.
| Surgical procedures | Number of patients, n (%) |
| Unilateral parathyroid exploration | 121 (86.4) |
| Bilateral parathyroid exploration | 19 (13.6) |
Among the 140 cases of PA in this study, 132 cases had one adenoma, including 19 cases of upper left PA, 51 cases of lower left PA, 13 cases of upper right PA, and 45 cases of lower right PA. In addition, there were 4 cases of ectopic PA, of which 3 had an ectopic PA in the upper mediastinum and 1 had an ectopic PA in the thyroid. Moreover, there were 8 cases of double adenomas, including 6 cases of upper left PA combined with upper right PA, 1 case of upper left PA combined with lower left PA, and 1 case of upper right PA combined with lower right PA. The correlations between the findings of the different diagnostic tools and the lesion position are shown in Table 5. Among the four cases of ectopic PA, one case was successfully localized preoperatively by ultrasound, four cases by Tc-99m MIBI SPECT/CT, and two cases each by CT scan with contrast and MRI with contrast.
| Position | Number of patients, n (%) | Ultrasound | Tc-99m MIBI SPECT/CT | CT scan with contrast | MRI with contrast | Ultrasound + Tc-99m MIBI SPECT/CT |
| Upper left PA | 19 (13.6) | 18/19 | 15/19 | 6/7 | 5/5 | 18/19 |
| Lower left PA | 51 (36.4) | 45/51 | 50/51 | 14/16 | 5/6 | 50/51 |
| Upper right PA | 13 (9.3) | 12/13 | 11/13 | 4/5 | 4/4 | 12/13 |
| Lower right PA | 45 (32.1) | 40/45 | 44/45 | 12/14 | 4/5 | 44/45 |
| Upper mediastinal ectopic PA | 3 (2.1) | 0/3 | 3/3 | 2/3 | 2/3 | 3/3 |
| Intrathyroidal ectopic PA | 1 (0.7) | 1/1 | 1/1 | 0/1 | 0/1 | 1/1 |
| Upper left PA combined with upper right PA | 6 (4.3) | 3/6 | 5/6 | 3/6 | 3/4 | 5/6 |
| Upper left PA combined with lower left PA | 1 (0.7) | 1/1 | 0/1 | 0/1 | 0/1 | 1/1 |
| Upper right PA combined with lower right PA | 1 (0.7) | 0/1 | 1/1 | 0/1 | 0/1 | 1/1 |
A total of 21 patients had symptoms of hypocalcemia with numbness of the hands and feet after surgery; the occurrence rate was 15.0%. The calcium supplement program was as follows: If there were mild symptoms of hypocalcemia after surgery, close observation was conducted; if the symptoms were not relieved, oral calcium and vitamin D3 were administered; when the patient had severe symptoms and signs of hypocalcemia, intravenous injection of 10% calcium gluconate and/or oral calcium and vitamin D3 were given simultaneously, and the dose was reduced gradually after the symptoms and signs were relieved until the drug was stopped.
Temporary hoarseness occurred in one case, with an occurrence rate of 0.7%. Nerve nutrient treatment and vasodilator drugs were given for 1 wk, and the hoarseness disappeared after 3 mo.
Nineteen cases had transient hypoparathyroidism after surgery, and the occurrence rate was 13.6%. Although there was no special treatment, the condition returned to normal after 1 wk to 1 mo. Moreover, no postoperative bleeding or hematoma in the surgical area was observed in all 140 patients (Table 6).
| Complications | Number of cases, n (%) |
| Hypocalcemia | 21 (15.0) |
| Hoarse voice | 1 (0.7) |
| Hypoparathyroidism | 19 (13.6) |
| Bleeding or hematoma in the surgical area | 0 (0) |
In all 140 patients with PA, postoperative blood calcium and PTH were significantly lower than those before surgery, and blood phosphorus increased significantly. At 3 years of follow-up, the PTH level and blood calcium of 138 patients had returned to normal. In two patients, the PTH level increased again as observed at the follow-up visit. This was considered to be recurrence of the disease, and the PTH level was restored to the normal value after re-surgery.
We analyzed the clinical records of 140 patients with PA. The overall success rate of surgery in this group of patients was 98.6%, and the treatment outcome was satisfactory.
PA is the most common cause of primary hyperparathyroidism, accounting for approximately 80%-85% of patients with primary hyperparathyroidism[13]. The cohort consisted of more women than men. The age span of patients is large, but it usually occurs between 30 and 60 years of age[14]. Adenomas can be single or multiple and dominated by a single occurrence. Among the cases in this group, 132 were single adenomas, accounting for 94.3% of all patients. Single adenoma was common in the lower parathyroid gland, without any obvious side difference. In this group, among the patients with single adenomas, 32 (22.9%) cases had adenomas in the upper parathyroid gland, and 96 (68.6%) cases had adenomas in the lower parathyroid gland. A single adenoma can also be ectopic, and ectopic sites appear in the thyroid, thymus, posterior esophagus, mediastinum, and carotid artery sheath. In this study, a total of 4 cases had single ectopic PAs, of which 3 were heterotopic in the mediastinum and 1 was heterotopic in the thyroid. Double adenomas are relatively rare, accounting for about 5% of patients with adenomas. These occur on the same side or on both sides, and usually involve both upper parathyroid glands[15]. In this study, 8 cases had double adenomas accounting for 5.7% of the total number of cases, and 6 cases involved bilateral upper parathyroid glands. The size of PAs varied greatly, the smaller ones could be < 1 cm, the larger ones were > 10 cm; the adenomas < 6 mm are termed “microadenomas”[16]. The weight is generally greater than 40 mg[17]; adenomas are solid, yellow or tan, with clear borders and soft round morphology.
The etiology of PA is unclear, and risk factors for the disease include radiation exposure and long-term lithium treatment[18]. Hyperparathyroidism caused by PA gives rise to skeletal system, urinary system, digestive system, neuromuscular system, and neuropsychiatric symptoms. Some patients did not have obvious symptoms before the diagnosis. However, because PA did not cause obvious typical symptoms, and due to the diverse symptoms of PA, patients often first visit orthopedic, urology, gastroenterology, neurology, and psychiatry clinics, leading to misdiagnosis. The key to improving the diagnostic rate is to be alert to the symptoms of PA. If a patient has one or more of the following manifestations, the possibility of PA should be considered: (1) Osteoporosis and bone pain due to unknown reasons; (2) recurrent or active urinary calculi or nephrocalcinosis; (3) unexplained gastrointestinal symptoms, such as nausea, vomiting, anorexia, acid reflux, constipation, and abdominal pain; and (4) unexplained neurological symptoms, such as personality changes and depression.
Preoperative localization diagnosis is a major factor in the success of surgery. As PAs are deeply located, small in size, and soft in texture, local compression symptoms are rarely observed unless the individual is large in size[19], or the PA is ectopically located in the front of the trachea. Moreover, sometimes the PA is ectopic, and there are many sporadic case reports in this regard[20-24]; 4 cases are reported in this study. Therefore, preoperative localization diagnosis is essential.
Currently, there are many detection methods, including ultrasound, CT scan with contrast, MRI with contrast, and Tc-99m MIBI SPECT/CT, for localization diagnosis of PA. Each of these detection methods has its own advantages and disadvantages.
The advantages of ultrasound examination are that it is fast, convenient, non-invasive, reproducible, and has high sensitivity and specificity; therefore, it is the first choice for localization of PAs. The first manifestation in many patients is parathyroid gland-occupying lesions found during ultrasound examination of the neck. All 140 patients in this study underwent neck ultrasonography; most were characterized by clear boundaries, regular morphology, and hypoechoic nodules. However, PAs sometimes undergo changes, such as calcification, cystic change, or cholesterol crystal deposition, which alter their ultrasound performance. Ultrasound examination detects space-occupying lesions in the parathyroid area on the dorsal side of the thyroid gland, but in this area, thyroid nodules may also appear which protrude from the thyroid gland (to the back or outside) or an isolated thyroid gland; hence, careful identification is required. Nodules protruding from the thyroid gland to the rear and outside usually have tissue continuity and blood flow continuity with normal thyroid tissue, while PAs are linearly separated from the thyroid tissue. Moreover, the parathyroid glands consist of large blood vessels that can be identified by color Doppler examination. However, it is difficult to distinguish between isolated thyroid tissues and PA during ultrasound examination. In addition, if the PA occurs ectopically and appears in the upper mediastinum and thyroid, it is difficult to locate it successfully. In this study, 4 patients had ectopic lesions, which could not be positioned by preoperative ultrasound examination. In addition, the experience of the sonographer also affects the accuracy of the diagnosis. In this study, the accuracy of ultrasound localization diagnosis was 85.52%, and hence, ultrasound examination alone cannot be used for preoperative localization diagnosis.
Nuclear medicine examination with Tc-99m MIBI SPECT/CT is currently the most specific method for localization and diagnosis of PAs. The primary mechanism is to use the different excretion rates of Tc-99m by the parathyroid gland and thyroid gland. Dual-phase imaging is also used to determine PAs[25]. The advantage of this method is its high detection rate for ectopic parathyroid tumors. In this study, accurate localization was achieved in 4 cases of ectopic parathyroid tumors. However, Tc-99m MIBI SPECT/CT lacks histological specificity, irrespective if it is PA, thyroid adenoma, thyroid carcinoma, or even nodular goiter; it can show positive findings[26,27]. Therefore, if a patient with PA also has thyroid adenoma, thyroid cancer, or nodular goiter, inaccurate localization is possible. In the present study, 10 patients with preoperative Tc-99m MIBI SPECT/CT showed inaccurate localization of PA.
CT/MRI can provide images of the correlation between PAs, blood vessels, trachea, and esophagus and has significant advantages in judging the association of the lesion with the surrounding tissues and whether there is adhesion. Some investigators have speculated that 4D-CT accurately locates the hyperfunctioning parathyroid glands before surgery (accurate to the quadrant), which was conducive to formulating preoperative plans and improving the success rate of surgery, especially in patients with recurrence[28]. Studies[29-33] have reported that preoperative Choline PET/CT has a high sensitivity and positive predictive value for PA detection in patients with primary hyperparathyroidism and negative or inconclusive conventional imaging results. Bilateral cervical exploration could be avoided in the majority of patients. However, we have no experience on the efficiency of this test as it has not been performed in our institution.
Therefore, each of the above-mentioned imaging methods has advantages and disadvantages. Previous studies have reported that the use of Tc-99m MIBI SPECT/CT is recommended as the primary method for preoperative localization of PAs[6-9]. According to the results of this study, our recom
Due to the etiological characteristics of PAs, approximately 85% of cases are single adenoma lesions. With the continuous improvement in the accuracy of preoperative localization methods and the application of rapid examination and monitoring of intraoperative PTH, the surgical methods for PA have gradually transitioned from the traditional bilateral neck detection surgical method to minimally invasive surgery, which directly removes the diseased gland. In this study, 13 cases of unilateral lesions were observed in the early stage of patients who adopted bilateral neck exploration to prevent residual lesions. Strikingly, with the improved diagnostic accuracy, 119 cases of unilateral lesions in the later stage adopted the minimally invasive surgical method for unilateral neck exploration, and no residual disease was detected. In addition, the integrity of the PA capsule must be ensured during surgery. Once the capsule is ruptured, this leads to planting and local recurrence of the tumor. When the parathyroid tumor is closely related to the thyroid tissue, isolation and removal of the thyroid tissues are necessary. In this study, we focused on protecting the integrity of the PA capsule, avoiding clamping and excessive pulling of the specimens in all cases. Only 2 cases had recurrence after surgery, and blood calcium and PTH levels returned to normal after the second surgery. Intraoperative PTH monitoring improved the success rate of surgery for PA removal. The major factors in the success of minimally invasive surgery were as follows: Precise localization before surgery, fine manipulation during surgery, and imple
The present study has several limitations. Firstly, as this is a retrospective study, it may have some bias and sampling variation. Secondly, this is a single-center study, and the sample size is small; hence, additional multicenter studies with a large sample size are essential.
For patients with clinically unexplained skeletal system symptoms, such as osteoporosis, unexplained urinary system symptoms, such as repeated episodes of urinary tract stones, or nephrocalcinosis, unexplained gastrointestinal symptoms, and unexplained neuropsychiatric symptoms, it is recommended that the possibility of PA should be excluded. Imaging examinations, such as ultrasound and Tc-99m MIBI SPECT/CT could be integrated before surgery to obtain accurate localization diagnosis. Preoperative precise localization, intraoperative PTH monitoring, and delicate surgery are requisites to protect the integrity of the parathyroid tumor capsule and ensure a minimally invasive and successful surgery.
Parathyroid adenoma (PA) sometimes recurs after surgery, how to improve the surgical success rate of PA is the key to the treatment of this disease.
To investigate the clinical features, diagnosis, and surgical treatment of patients with PA.
To summarize the key points to improve the success rate of surgery for PA.
One hundred and forty patients who were pathologically confirmed with PA and had undergone surgery for the first time were included in the study. The clinical features, localization diagnosis, and surgical treatment of these patients were analyzed.
The positive detection rate of technetium-99 m sestamibi (Tc-99m MIBI) single-photon emission computed tomography/computed tomography (SPECT/CT) combined with ultrasound examination was 96.4%. The success rate of surgery was 98.6%.
Imaging examinations such as ultrasound, and Tc-99m MIBI SPECT/CT could be integrated before surgery to obtain accurate localization diagnosis. Precise preoperative localization, intraoperative parathyroid hormone monitoring, and delicate surgery to protect the integrity of the PA capsule ensure a minimally invasive and successful surgery.
To identify more effective diagnostic methods for patients with PAs that cannot be localized preoperatively.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Otorhinolaryngology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Anzola F LK, Colombia; Xu Y, China S-Editor: Chen YL L-Editor: Webster JR P-Editor: Chen YL
| 1. | AACE/AAES Task Force on Primary Hyperparathyroidism. The American Association of Clinical Endocrinologists and the American Association of Endocrine Surgeons position statement on the diagnosis and management of primary hyperparathyroidism. Endocr Pract. 2005;11:49-54. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 144] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 2. | Pal R, Mukherjee S, Bhadada SK, Bhansali A, Puravoor J, Behera A. Persistence of "non-dipping" pattern in blood pressure after curative parathyroidectomy in apparently normotensive patients with symptomatic primary hyperparathyroidism. Minerva Endocrinol. 2020;45:181-188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Karras SN, Koufakis T, Tsekmekidou X, Antonopoulou V, Zebekakis P, Kotsa K. Increased parathyroid hormone is associated with higher fasting glucose in individuals with normocalcemic primary hyperparathyroidism and prediabetes: A pilot study. Diabetes Res Clin Pract. 2020;160:107985. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 20] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Zivaljevic V, Jovanovic M, Diklic A, Zdravkovic V, Djordjevic M, Paunovic I. Differences in primary hyperparathyroidism characteristics between children and adolescents. J Pediatr Surg. 2020;55:1660-1662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 5. | Taniegra ED. Hyperparathyroidism. Am Fam Physician. 2004;69:333-339. [PubMed] |
| 6. | Mihai R, Simon D, Hellman P. Imaging for primary hyperparathyroidism--an evidence-based analysis. Langenbecks Arch Surg. 2009;394:765-784. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 108] [Cited by in RCA: 94] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 7. | Cheung K, Wang TS, Farrokhyar F, Roman SA, Sosa JA. A meta-analysis of preoperative localization techniques for patients with primary hyperparathyroidism. Ann Surg Oncol. 2012;19:577-583. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 248] [Cited by in RCA: 255] [Article Influence: 18.2] [Reference Citation Analysis (0)] |
| 8. | Eslamy HK, Ziessman HA. Parathyroid scintigraphy in patients with primary hyperparathyroidism: 99mTc sestamibi SPECT and SPECT/CT. Radiographics. 2008;28:1461-1476. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 94] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 9. | Lew JI, Solorzano CC. Surgical management of primary hyperparathyroidism: state of the art. Surg Clin North Am. 2009;89:1205-1225. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 70] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 10. | Wilhelm SM, Wang TS, Ruan DT, Lee JA, Asa SL, Duh QY, Doherty GM, Herrera MF, Pasieka JL, Perrier ND, Silverberg SJ, Solórzano CC, Sturgeon C, Tublin ME, Udelsman R, Carty SE. The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism. JAMA Surg. 2016;151:959-968. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 578] [Cited by in RCA: 612] [Article Influence: 68.0] [Reference Citation Analysis (0)] |
| 11. | Catalfamo A, Famà F, Pergolizzi FP, Bartolo V, Rizzo AG, Marullo M, Fabiano V, Cancellieri A, Melita G, Portinari M, Donatini G, Makay O, Carcoforo P, Dionigi G. Management of undetectable and lost parathyroid adenoma. Ann Thyroid. 2018;3:1-1.. [DOI] [Full Text] |
| 12. | Agarwal A, Pradhan R. Failed parathyroidectomy: The road ahead. Indian J Endocrinol Metab. 2012;16:S221-S223. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Marcocci C, Cetani F. Clinical practice. Primary hyperparathyroidism. N Engl J Med. 2011;365:2389-2397. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 230] [Cited by in RCA: 210] [Article Influence: 15.0] [Reference Citation Analysis (33)] |
| 14. | Lu R, Zhao W, Yin L, Guo R, Wei B, Jin M, Zhou X, Zhang C, Lv X. Efficacy of ultrasonography and Tc-99m MIBI SPECT/CT in preoperative localization of parathyroid adenomas causing primary hyperthyroidism. BMC Med Imaging. 2021;21:87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 15. | Guilmette J, Sadow PM. Parathyroid Pathology. Surg Pathol Clin. 2019;12:1007-1019. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 36] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 16. | Oberger Marques JV, Moreira CA. Primary hyperparathyroidism. Best Pract Res Clin Rheumatol. 2020;34:101514. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 18] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 17. | Erickson LA, Mete O. Immunohistochemistry in Diagnostic Parathyroid Pathology. Endocr Pathol. 2018;29:113-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 64] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 18. | Gebauer J, Higham C, Langer T, Denzer C, Brabant G. Long-Term Endocrine and Metabolic Consequences of Cancer Treatment: A Systematic Review. Endocr Rev. 2019;40:711-767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 94] [Article Influence: 15.7] [Reference Citation Analysis (0)] |
| 19. | Al-Hassan MS, Mekhaimar M, El Ansari W, Darweesh A, Abdelaal A. Giant parathyroid adenoma: a case report and review of the literature. J Med Case Rep. 2019;13:332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 20. | Iyer S, Simon M, Tan C, Gesner L, Viggiano J, Chhabra S. Retro-tracheal parathyroid adenoma: A rare location of a common pathology. Radiol Case Rep. 2020;15:672-674. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Yokota K, Kurihara I, Matsusaka Y, Emoto K, Hishida T, Oshida T, Kobayashi S, Murai-Takeda A, Miyashita K, Matsuda K, Nakagomi T, Itoh H. Mediastinal Cystic Parathyroid Adenoma Diagnosed by Somatostatin Receptor Scintigraphy. Intern Med. 2021;60:1555-1560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 22. | Abusabeib A, Bhat H, El Ansari W, Al Hassan MS, Abdelaal A. Right ectopic paraesophageal parathyroid adenoma with refractory hypercalcemia in pregnancy: A case report and review of the literature. Int J Surg Case Rep. 2020;77:229-234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 23. | Ng FH, Yung KS, Luk WH. Ectopic Submandibular Parathyroid Adenoma by Tc-99m Sestamibi SPECT/CT Localization. J Clin Imaging Sci. 2020;10:61. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 24. | Seo Y, Song K, Choi HS, Suh J, Kwon A, Chae HW, Kim HS. A case of primary hyperparathyroidism due to an intrathymic ectopic parathyroid adenoma in a 15-year-old boy. Ann Pediatr Endocrinol Metab. 2020;25:187-191. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Mohebati A, Shaha AR. Imaging techniques in parathyroid surgery for primary hyperparathyroidism. Am J Otolaryngol. 2012;33:457-468. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 63] [Cited by in RCA: 65] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 26. | Rubello D, Toniato A, Pelizzo MR, Casara D. Papillary thyroid carcinoma associated with parathyroid adenoma detected by pertechnetate-MIBI subtraction scintigraphy. Clin Nucl Med. 2000;25:898-900. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Wei B, Shen H, Tong G, Wang R, Chang H. [Efficiency of (99)Tc(m)-sestamibi in diagnosis of parathyroid diseases with primary hyperparathyroidism]. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. 2015;50:123-126. [PubMed] |
| 28. | Rodgers SE, Hunter GJ, Hamberg LM, Schellingerhout D, Doherty DB, Ayers GD, Shapiro SE, Edeiken BS, Truong MT, Evans DB, Lee JE, Perrier ND. Improved preoperative planning for directed parathyroidectomy with 4-dimensional computed tomography. Surgery. 2006;140:932-40; discussion 940. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 310] [Cited by in RCA: 277] [Article Influence: 14.6] [Reference Citation Analysis (0)] |
| 29. | Quak E, Blanchard D, Houdu B, Le Roux Y, Ciappuccini R, Lireux B, de Raucourt D, Grellard JM, Licaj I, Bardet S, Reznik Y, Clarisse B, Aide N. F18-choline PET/CT guided surgery in primary hyperparathyroidism when ultrasound and MIBI SPECT/CT are negative or inconclusive: the APACH1 study. Eur J Nucl Med Mol Imaging. 2018;45:658-666. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 65] [Cited by in RCA: 78] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 30. | Parvinian A, Martin-Macintosh EL, Goenka AH, Durski JM, Mullan BP, Kemp BJ, Johnson GB. 11C-Choline PET/CT for Detection and Localization of Parathyroid Adenomas. AJR Am J Roentgenol. 2018;210:418-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 29] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 31. | Whitman J, Allen IE, Bergsland EK, Suh I, Hope TA. Assessment and Comparison of 18F-Fluorocholine PET and 99mTc-Sestamibi Scans in Identifying Parathyroid Adenomas: A Metaanalysis. J Nucl Med. 2021;62:1285-1291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 16] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 32. | Treglia G, Piccardo A, Imperiale A, Strobel K, Kaufmann PA, Prior JO, Giovanella L. Diagnostic performance of choline PET for detection of hyperfunctioning parathyroid glands in hyperparathyroidism: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging. 2019;46:751-765. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 97] [Cited by in RCA: 130] [Article Influence: 18.6] [Reference Citation Analysis (0)] |
| 33. | Prabhu M, Damle NA. Fluorocholine PET Imaging of Parathyroid Disease. Indian J Endocrinol Metab. 2018;22:535-541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 1.9] [Reference Citation Analysis (0)] |