Published online Sep 26, 2022. doi: 10.12998/wjcc.v10.i27.9798
Peer-review started: March 30, 2022
First decision: May 30, 2022
Revised: March 30, 2022
Accepted: August 16, 2022
Article in press: August 16, 2022
Published online: September 26, 2022
Processing time: 162 Days and 23.7 Hours
Solitary fibrous tumor (SFT) is a rare mesenchymal neoplasm. SFT derived from the renal pelvis is an exceedingly rare entity. In this study, we report a case of renal pelvis SFT and review the relevant literature on this rare tumor.
A 76-year-old man was hospitalized due to right lumbar and abdominal pain. Abdominal computed tomography showed a hypervascular space-occupying renal lesion, sized 2.3 cm × 1.8 cm. Based on the computed tomography findings, the patient was diagnosed with right renal pelvis tumor and underwent neph
We report a rare case of SFT derived from the renal pelvis and discuss the imaging and histopathological features that distinguish renal pelvis SFT from other renal pelvis tumors.
Core Tip: Extrapleural solitary fibrous tumor is an extremely rare mesenchymal neoplasm, especially in cases of origination from the renal pelvis. We report a rare case of renal pelvis solitary fibrous tumor and discuss the detailed radiologic and pathologic findings. The differential diagnosis of renal pelvis solitary fibrous tumor is discussed based on literature review.
- Citation: Liu M, Zheng C, Wang J, Wang JX, He L. Solitary fibrous tumor of the renal pelvis: A case report. World J Clin Cases 2022; 10(27): 9798-9804
- URL: https://www.wjgnet.com/2307-8960/full/v10/i27/9798.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i27.9798
Solitary fibrous tumors (SFTs) were reported for the first time by Wagner et al[1] in 1870. As hemangiopericytomas, SFTs are usually benign and arise from mesenchymal spindle cells, typically of the pleura. Extrapleural SFTs are relatively rare[2]. Although several cases of SFT have been reported, the cause of SFT remains unknown[3]. Most of the SFTs are benign lesions with slow progress, but some have malignant potential[4]. Renal pelvis SFT is an extremely rare entity, with only 11 cases reported in the published literature[5]. Renal pelvis SFT is liable to be misdiagnosed as renal cell carcinoma (RCC), upper-tract urothelial cancers (UTUCs) or renal angiomyolipoma (RAML). The diagnosis and treatment of renal pelvis SFT is challenging. In this work, we report a rare case of renal pelvis SFT. In addition, we review the relevant literature to facilitate accurate diagnosis and treatment of renal pelvis SFT.
A 76-year-old man (height: 167 cm; weight: 70 kg) presented in our hospital for persistent right lumbar and abdominal pain.
The right lumbar and abdominal pain had persisted for more than 3 years and gradually aggravated in the last 3 mo. There was no associated nausea or vomiting.
The illness history of the patient was unremarkable.
The patient had no specific personal or family history of illnesses.
The vital parameters of the patient on the day of admission were as follows: body temperature, 36.3 °C; heart rate, 80 beats per min; respiratory rate, 18 breaths per min; blood pressure, 125/80 mmHg; and oxygen saturation in room air, 98%. There was mild tenderness in the left lumbar and abdominal area.
Urinalysis, routine blood tests, coagulation indices, blood urea nitrogen, and liver function were normal. Urinary cytology revealed no heterocytes.
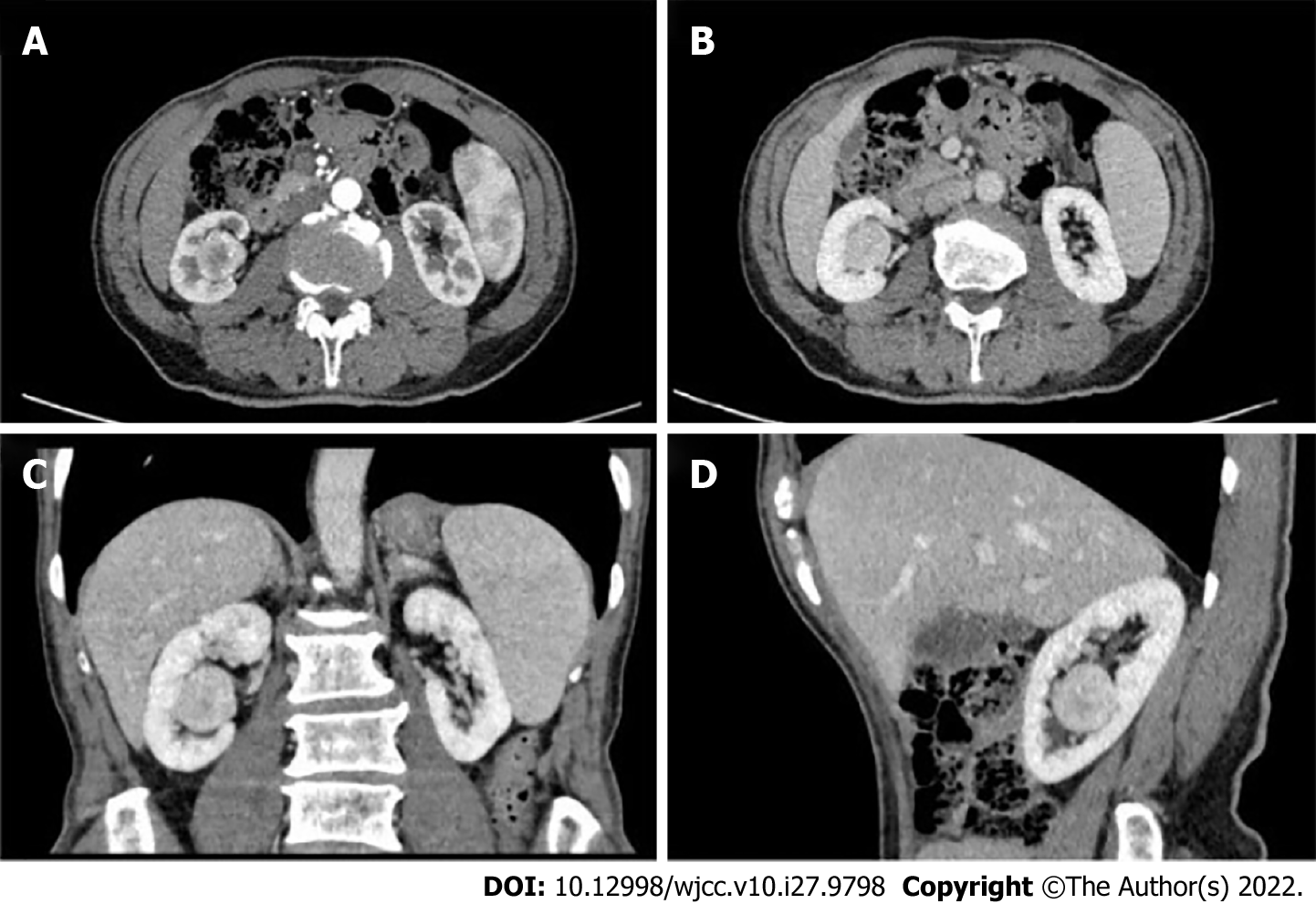
Abdominal contrast-enhanced computed tomography (CT) showed a right renal intrapelvic hyper
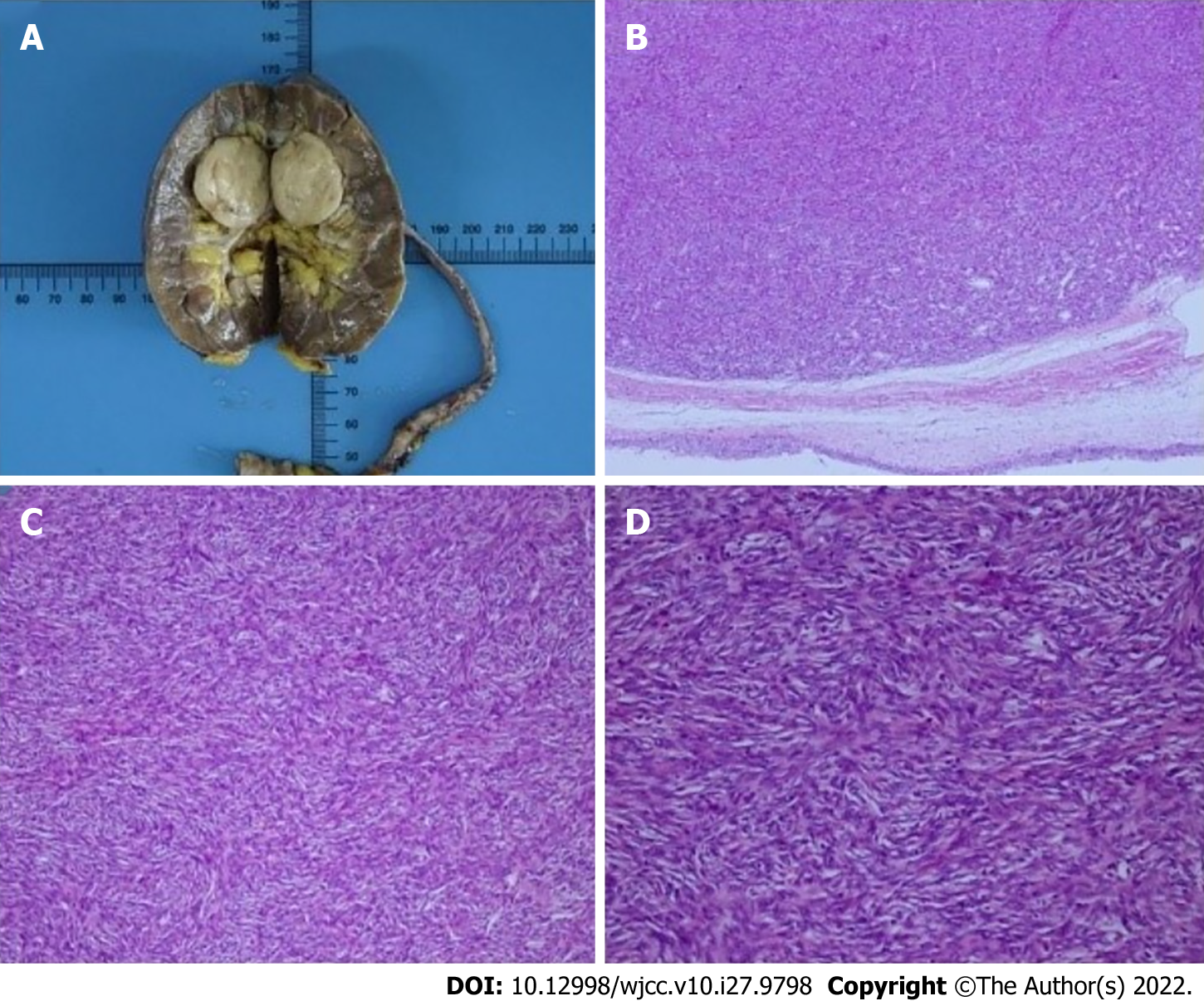
Histopathological findings identified the tumor as renal pelvis SFT (Figure 2). The size of the tumor was 2.7 cm × 2.5 cm × 1.6 cm. The mitotic image of the tumor was higher than 4/10 high power field. There were no signs of neurovascular invasion by tumor cells.
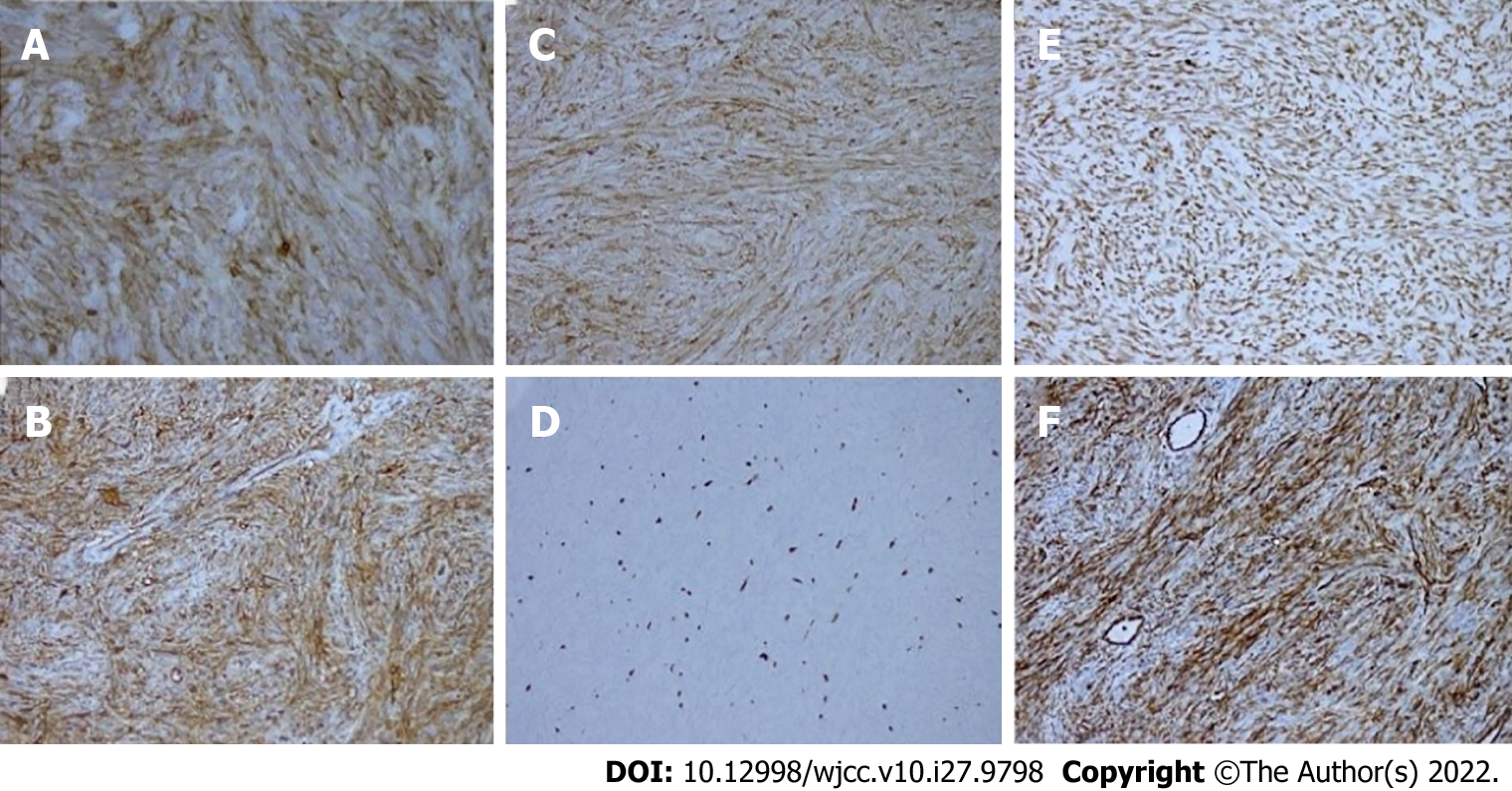
Immunohistochemical results were as follows: CD34 (+), desmin (-), H-caldesmon (-), SMA (+), STAT6 (+), vimentin (+), Bcl-2 (+), CD117 (-), Dog-1 (-), HMB45 (-), S-100 (-), Ki-67 (+10%), CD99 (+) and EMA (-). The immunohistochemical results confirmed the diagnosis of renal pelvis SFT (Figure 3).
The patient was diagnosed with left renal pelvis tumor.
After weighing different treatment options, the patient underwent laparoscopic right nephroureterectomy.
The patient recovered well after the operation and was discharged after 5 d. The outcome was satisfactory, and there were no signs of recurrence during the 3-year follow-up.
SFTs are rare mesenchymal tumors accounting for < 2% of all soft tissue tumors with an estimated annual incidence of 2 cases per million population[6]. The age of reported cases of SFT patients ranges between 4 years and 85 years, and there is no clear predilection for any particular sex[3]. SFTs mainly occur in the pleura. However, SFTs have also been reported at extrapulmonary sites, such as the liver, mediastinum, breast, lung, meninges, and urogenital organs[7]. According to previous reports, 15% of SFTs originating in the kidneys are located in the renal capsule, 6% are located around the pelvis, 3% are located in the renal pelvis, and 76% do not have a clear site of origin[8]. The first case of renal pelvis SFT was reported by Yazaki et al[9] in 2001. Until now, only 15 cases of renal pelvis SFTs have been reported. Renal pelvis SFT cases are summarized in Table 1.
| No | Ref. | Age/Sex/Side | Size | Treatment |
| 1 | Yazaki et al[9] | 70/M/R | 6 cm × 4.5 cm × 4 cm | Radical nephrectomy |
| 2 | Margo et al[20] | 31/F/R | Approximately 8.6 cm | Radical nephrectomy |
| 3 | Marzi et al[21] | 72/F/L | Approximately 19 cm | Radical nephrectomy |
| 4 | Sasaki et al[22] | 48/M/R | 28 cm × 18 cm × 10 cm | Radical nephrectomy |
| 5 | Usuba et al[16] | 50/M/L | 17 cm × 11 cm × 8 cm | Radical nephrectomy |
| 6 | Zhang et al[5] | 45/F/L | 4 cm × 2.5 cm × 2 cm | Radical nephrectomy |
| 7 | Hirano et al[23] | 75/F/L | 4.5 cm × 3.5 cm | Radical nephrectomy |
| 8 | Naveen et al[24] | 52/F/R | 17 cm × 10 cm × 10 cm | Radical nephrectomy |
| 9 | Dong et al[25] | 71/F/L | 4 cm × 3.5 cm × 4 cm | Radical nephrectomy |
| 10 | Mearini et al[26] | 17/F/L | 17 cm × 9.8 cm × 12 cm | Radical nephrectomy |
| 11 | Wang et al[27] | 66/F/R | 23 cm × 18 cm × 12 cm | Radical nephrectomy |
| 12 | Cheung et al[2] | 49/F/L | 19 cm × 12 cm × 10 cm | Radical nephrectomy |
| 13 | Fursevich et al[14] | 66/F/L | 9.3 cm × 7.9 cm × 9.4 cm | Radical nephrectomy |
| 14 | Bacalbasa et al[1] | 49/M/R | 15 cm × 15 cm × 10 cm | Radical nephrectomy |
| 15 | Luca et al[3] | 52/F/R | 7.4 cm × 6.3 cm × 5.8 cm | Radical nephrectomy |
Renal pelvis SFTs need to be differentiated from the more common renal pelvis tumors such as RCC, RAMLs, and UTUCs. Contrast-enhanced CT is the main method for the diagnosis of RCCs[10]. RCC is characterized by abundant blood supply, and tumor blood vessels and tumor staining can be observed on renal angiography. Contrast enhancement of renal pelvis SFTs is much lower than that of RCCs. UTUCs are another kind of common renal pelvis malignant tumor. Patients with UTUCs typically have a history of hematuria[11]. In contrast, symptoms of renal pelvis SFTs are mostly due to pressure effect of the lesion, and these patients rarely develop urinary symptoms. The UTUCs show signs of infiltrative growth in CT images. Compared with UTUCs, renal pelvis SFT appears as a well-defined, heterogeneous or homogeneous mass showing moderate to marked contrast-enhancement. RAML is the most common renal benign tumor. Most RAMLs exhibit mixed density on CT imaging, due to the complex fatty vascular components.
In addition to RCCs, UTUCs, and RAMLs, there are also some rare tumor types including hemangiopericytomas, renal pelvis fibroepithelial polyps, fibromas, renal leiomyoma and inflammatory myofibroblastic tumors[12]. The imaging characteristics of renal pelvis SFTs are usually indistinguishable from these rare tumors, and the differential diagnosis is based on immunohistochemistry[13].
According to the literature, some renal pelvis SFTs show areas of calcification, cystic change or necrosis[14]. These changes indicate the aggressive nature of the tumor and poor prognosis.
In this case, the surgical method was laparoscopic right kidney and ureterectomy. There are currently no treatment guidelines for renal pelvis SFTs, but radical resection is generally chosen. Whether preoperative biopsy or nephron preservation surgery can improve the treatment efficacy and prognosis is not clear. For most cases of SFT, due to the malignant potential of SFTs and lack of recurrence after radical nephrectomy, a complete removal is recommended[15].
Immunohistochemistry plays a key role in arriving at a definitive diagnosis. SFTs stain positive for CD34, CD99 and Bcl-2. STAT6 is also an antibody with high sensitivity for SFT diagnosis. These surface antigens are useful diagnostic markers of SFT[3]. It has been reported that CD34 and Bcl-2 negativity may indicate increased malignant potential[16]. Although STAT6 is expressed in most SFTs, SFTs located in the renal pelvis have not been evaluated. Whether STAT6-negative status increases the malignant potential of renal pelvis SFTs is unknown. In this case, tumor tissue stained positive for CD34, vimentin, Bcl-2, STAT6 and CD99. It was considered as a benign renal SFT, and there was no local or distant metastasis after 3 years of follow-up. However, benign renal pelvis SFT may also have the ability for distant metastasis. Therefore, renal pelvis SFT is considered to be a “moderately malignant tumor that rarely metastasizes.” Metastasis may occur in the lungs, liver and bones[17]. There are also reports of retroperitoneal recurrence[18]. Rarely, the SFTs can also cause paraneoplastic syndromes such as Doege-Potter syndrome[19]. Hence, all renal pelvis SFT patients need long-term follow-up and regular review, such as abdominal and lung CT.
We reported a rare case of renal pelvis SFT. Compared to the previously reported renal pelvis SFT tumors, the tumor in our patient was small in size and localized in the renal pelvis. Clinicians should pay attention to clarifying the source of kidney SFT and differentiate it from other renal pelvis cancers, so as to reduce the occurrence of misdiagnosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Bellini MI, Italy; Sahin TK, Turkey; Straksyte V, Lithuania S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Bacalbasa N, Balescu I, Jinescu G, Marcu M, Contolenco A, Pop D, Dobritoiu D, Ionescu O, Ionescu P, Stoica C. Fat-forming Solitary Fibrous Tumor of the Kidney - A Case Report and Literature Review. In Vivo. 2018;32:649-652. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 2. | Cheung F, Talanki VR, Liu J, Davis JE, Waltzer WC, Corcoran AT. Metachronous Malignant Solitary Fibrous Tumor of Kidney: Case Report and Review of Literature. Urol Case Rep. 2016;4:45-47. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | De Luca L, Creta M, Barone B, Crocetto F, Cieri M, Campanino MR, Insabato L, Mangiapia F, Fusco F, Imbimbo C, Mirone V, Longo N. A case of incidentally discovered solitary fibrous tumor of the kidney: A case study. Mol Clin Oncol. 2020;13:39. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Yan XJ, Zheng C, Wang J. Transcatheter arterial embolization of malignant pelvic solitary fibrous tumor: case report and literature review. Translational Cancer Research. 2021;10(11):4979-4987. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Zhang Q, Qin J, Li Y, Wu T. Primary solitary fibrous tumor of kidney: A case report and literature review. Urol Case Rep. 2019;23:92-94. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Zhou SY, Zhan R, Qiao ZG, Wu JZ. Giant solitary fibrous tumor: A clinically silent tumor. Asian Journal of Surgery. 2021;44(8):1085-1086. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 7. | Zaghbib S, Chakroun M, Essid MA, Saadi A, Bouzouita A, Derouiche A, Slama MRB, Ayed H, Chebil M. Solitary fibrous tumor of the kidney: A case report. Int J Surg Case Rep. 2019;62:112-114. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Kopel J, Sharma P, Warriach I. A solitary fibrous tumor of the kidney. Urol Case Rep. 2020;28:101072. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Yazaki T, Satoh S, Iizumi T, Umeda T, Yamaguchi Y. Solitary fibrous tumor of renal pelvis. International journal of urology: official journal of the Japanese Urological Association. 2001;8(9):504-508. [RCA] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Chen M, Yin F, Yu Y, Zhang H, Wen G. CT-based multi-phase Radiomic models for differentiating clear cell renal cell carcinoma. Cancer Imaging. 2021;21:42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 18] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 11. | Sahin TK, Aladag E, Setterzade E, Guven GS, Haznedaroglu IC, Aksu S. Spontaneous subepithelial hemorrhage of renal pelvis and ureter (Antopol-Goldman lesion) in hemophilia A patient with inhibitor: Case report and review of the literature. Medicine (Baltimore). 2020;99:e20851. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 12. | Khater N, Khauli R, Shahait M, Degheili J, Khalifeh I, Aoun J. Solitary fibrous tumors of the kidneys: presentation, evaluation, and treatment. Urol Int. 2013;91:373-383. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Raman SP, Hruban RH, Fishman EK. Beyond renal cell carcinoma: rare and unusual renal masses. Abdom Imaging. 2012;37:873-884. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 30] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | Fursevich D, Derrick E, O'Dell MC, Vuyyuru S, Burt J. Solitary Fibrous Tumor of the Kidney: A Case Report and Literature Review. Cureus. 2016;8:e490. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 15. | Kuroda N, Ohe C, Sakaida N, Uemura Y, Inoue K, Nagashima Y, Hes O, Michal M. Solitary fibrous tumor of the kidney with focus on clinical and pathobiological aspects. Int J Clin Exp Pathol. 2014;7:2737-2742. [PubMed] |
| 16. | Usuba W, Sasaki H, Yoshie H, Kitajima K, Kudo H, Nakazawa R, Sato Y, Takagi M, Chikaraishi T. Solitary Fibrous Tumor of the Kidney Developing Local Recurrence. Case Rep Urol. 2016;2016:2426874. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Dozier J, Jameel Z, McCain DA, Hassoun P, Bamboat ZM. Massive malignant solitary fibrous tumor arising from the bladder serosa: a case report. J Med Case Rep. 2015;9:46. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 16] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 18. | Manica M, Roscigno M, Naspro R, Sodano M, Milesi L, Gianatti A, Da Pozzo LF. Recurrent retroperitoneal solitary fibrous tumor: a case report. Tumori. 2021;107:NP11-NP14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 19. | Mohammed T, Ozcan G, Siddique AS, Araneta RN, Slater DE, Khan A. Doege-Potter Syndrome with a Benign Solitary Fibrous Tumor: A Case Report and Literature Review. Case Reports in Oncology. 2021;14(1):470-476. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 20. | Magro G, Cavallaro V, Torrisi A, Lopes M, Dell'Albani M, Lanzafame S. Intrarenal solitary fibrous tumor of the kidney report of a case with emphasis on the differential diagnosis in the wide spectrum of monomorphous spindle cell tumors of the kidney. Pathol Res Pract. 2002;198:37-43. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Marzi M, D'Alpaos M, Piras P, Paiusco A, Minervini MS, Di Zitti P. [Solitary fibrous tumor of the kidney. A propos of a case]. Urologia. 2009;76:112-114. [PubMed] |
| 22. | Sasaki H, Kurihara T, Katsuoka Y, Nakano T, Yoshioka M, Miyano S, Sato Y, Uejima I, Hoshikawa M, Takagi M, Chikaraishi T. Distant metastasis from benign solitary fibrous tumor of the kidney. Case Rep Nephrol Urol. 2013;3:1-8. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Hirano D, Mashiko A, Murata Y, Satoh K, Ichinose T, Takahashi S, Jike T, Sugitani M. A case of solitary fibrous tumor of the kidney: an immunohistochemical and ultrastructural study with a review of the literature. Med Mol Morphol. 2009;42:239-244. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 20] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 24. | Naveen HN, Nelivigi GN, Venkatesh GK, Suriraju V. A case of solitary fibrous tumor of the kidney. Urol Ann. 2011;3:158-160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Dong B, Zhang JJ, Wang G. Renal solitary fibrous tumour: A rare pathological entity. Cuaj-Canadian Urological Association Journal. 2014;8(9-10):E657-E9. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 26. | Mearini E, Cochetti G, Barillaro F, Fatigoni S, Roila F. Renal malignant solitary fibrous tumor with single lymph node involvement: report of unusual metastasis and review of the literature. Onco Targets Ther. 2014;7:679-685. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 27. | Wang H, Liao Q, Liao X, Wen G, Li Z, Lin C, Zhao L. A huge malignant solitary fibrous tumor of kidney: case report and review of the literature. Diagn Pathol. 2014;9:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |