Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.9156
Peer-review started: April 28, 2022
First decision: June 8, 2022
Revised: June 13, 2022
Accepted: August 1, 2022
Article in press: August 1, 2022
Published online: September 6, 2022
Processing time: 120 Days and 3 Hours
Simple hepatic cysts are commonly occurring lesions that are usually asym
A 72-year-old woman diagnosed with adenocarcinoma of duodenal papilla underwent pancreatoduodenectomy with Child reconstruction. She then suffered repeated occurrences of bacteremia and hepatic cyst infection for 3 years. Blood cultures were positive for Klebsiella pneumoniae and Escherichia coli a total of 7 times and 4 times, respectively. During the early stage, we suspected that post
Biliary reconstruction inducing hepatic cyst infection is easily misdiagnosed as biliary reflux infection, Repeated imaging examination is a method for identifying the infected focus.
Core Tip: Biliary reconstruction can induce repeated hepatic cyst infection for multiple cysts. Repeated imaging examination is a good method for identifying the infected focus. Antimicrobial treatment and percutaneous cyst drainage are simple and effective method to control infection.
- Citation: Zhang K, Zhang HL, Guo JQ, Tu CY, Lv XL, Zhu JD. Repeated bacteremia and hepatic cyst infection lasting 3 years following pancreatoduodenectomy: A case report. World J Clin Cases 2022; 10(25): 9156-9161
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/9156.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.9156
Simple hepatic cysts are common lesions that are usually asymptomatic and require no treatment, with only 5% of patients suffering from bleeding, rupture, infection, or other complications[1]. A reason that predisposes individuals to asymptomatic hepatic cyst infection is history of biliary surgery, and communication between the biliary tract and cysts has been observed in some cases[2,3]. We report a case of hepatic cyst infection following pancreatoduodenectomy, in which repeated fever lasted for almost 3 years, and two cysts were infected successively. Treatment with antimicrobials was provided, and percutaneous cyst drainage was performed. The patient did not experience another relapse event for over 4 years.
A 72-year-old woman suffered from repeated fever, nausea and vomiting for 3 years following pancreatoduodenectomy, which had been aggravated for 2 d prior to her presentation at the hospital.
The patient presented with a complaint of repeated fever, sometimes accompanied by nausea and vomiting following pancreatoduodenectomy for 3 years. No associated abdominal pain, diarrhea, or melena was observed. Similar symptoms appeared repeatedly, once every 1-2 mo, with fever symptoms that gradually resolved 3-5 d after antibiotic treatment. Two days later, she became febrile again. The use of oral moxifloxacin tablets could not control the infection, and her body temperature reached 39.8 °C.
The patient underwent pancreatoduodenectomy with child reconstruction for adenocarcinoma of duodenal papilla 3 years prior. Histological analysis revealed a moderately differentiated adenocarcinoma at stage T2N0M0, Ia. The patient recovered well and was followed-up regularly. No evidence of local recurrence or distant metastasis was noted within 3 years after surgery. Multiple cysts of the liver were detected over more than 40 years but were asymptomatic. She also had hypertension, which was controlled with medication for more than 20 years.
The patient’s temperature was 39.8 °C, heart rate was 92 bpm, and blood pressure was 145/92 mmHg. Physical examination revealed yellowish skin and icteric sclera. The abdomen was soft with no abdominal pain or rebound pain.
Laboratory findings revealed a white cell count of 8900/µL (reference value, 4000 to 10000/µL), neutrophil ratio of 90%, serum C-reactive protein concentration of 126 mg/dL (reference value, < 8 mg/dL), serum gamma glutamic transpeptidase concentration (GGT) of 158 IU/L (reference value, 8 to 50 IU/L), serum alkaline phosphatase concentration (ALP) of 576 IU/L (reference value, 40 to 150 IU/L), serum total bilirubin (TBIL) level of 95 µmol/L (reference value, 3 to 22 µmol/L), serum direct bilirubin (DBIL) level of 76.5 µmol/L (reference value, 0 to 7 µmol/L), serum aspartate aminotransferase concentration (AST) of 55 IU/L (reference value, 15 to 40 IU/L), and serum alanine aminotransferase concentration (ALT) of 115 IU/L (reference value, 7 to 40 IU/L). In the past 3 years, blood culture was positive for Klebsiella pneumoniae and Escherichia coli 7 times and 4 times, respectively.
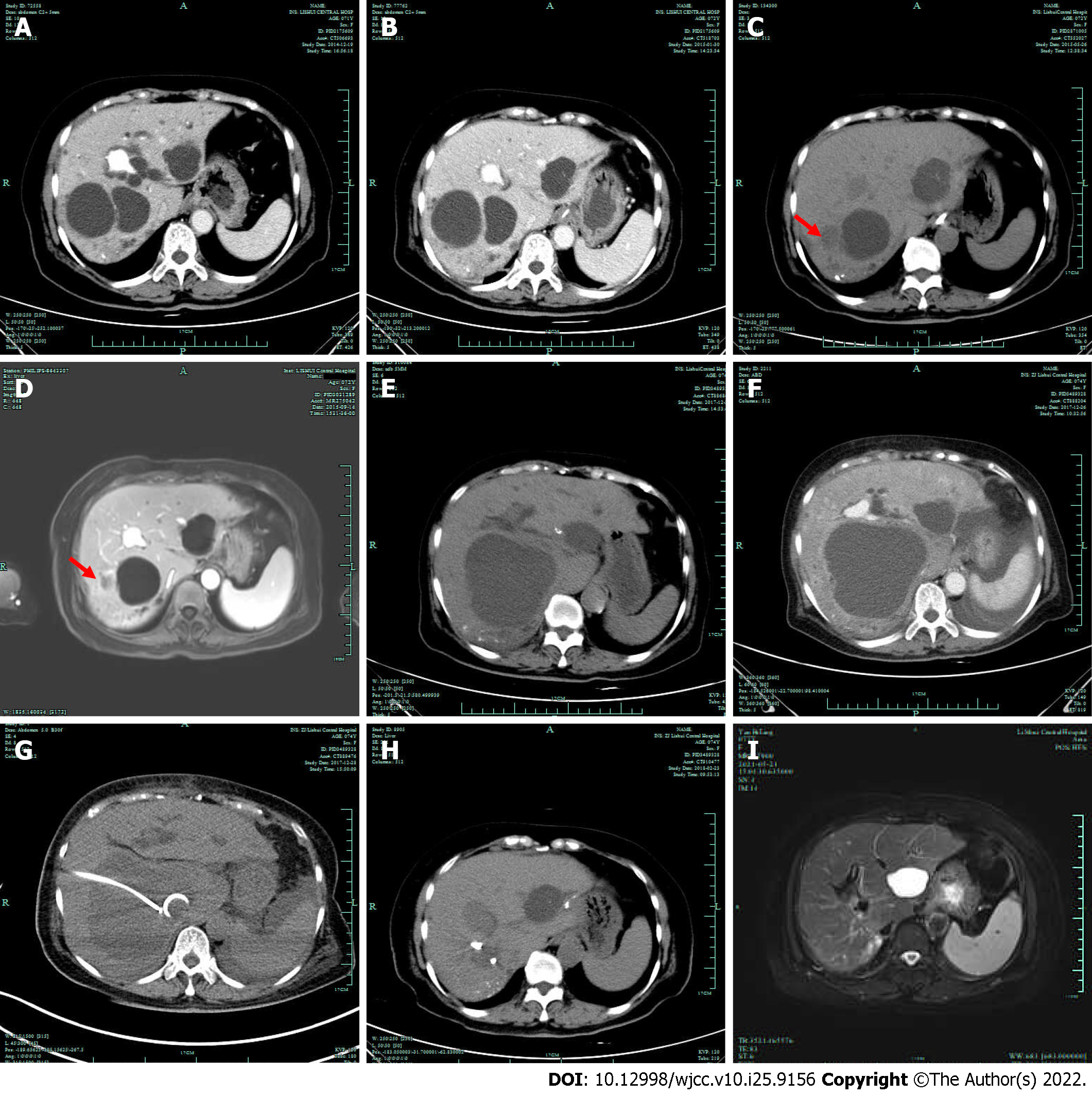
Preoperative computed tomography (CT) showed several asymptomatic hepatic cysts (Figure 1A). Abdominal CT performed 2 mo postoperatively did not reveal signs of hepatic cyst infection, such as an enhanced thickened wall, edema of the perilesional hepatic parenchyma or a significant increase in cyst diameter (Figure 1B). Abdominal CT performed 5 mo postoperatively (Figure 1C) and Magnetic Resonance Imaging (MRI) performed 9 mo postoperatively (Figure 1D) both showed that the cyst on the lateral side of the right liver had significantly decreased in size, and the wall of the cyst was slightly thickened. The interior cyst appeared slightly enlarged, but it had a thin smooth wall and homogenous contents, and no edema was observed in the surrounding liver tissue. Three years postoperatively, a CT plain scan showed that the cyst on the lateral side of the right liver had disappeared and that the cyst on the inner side of the right lobe had obviously increased in size. Mild dilatation of the intrahepatic bile duct was also noted (Figure 1E).
Enhanced CT revealed that the cyst on the inner side of the right lobe had obviously increased in size, had a thick wall and was surrounded by edema, with less pleural and peritoneal effusion (Figure 1F). The cyst showed obvious infection. The blood culture was positive for Klebsiella pneumoniae at this time.
Based on the patient history, laboratory examinations, and imaging examinations, the final diagnosis was cyst infection and infection of the biliary tract combined with bacteremia.
We initially administered empiric antibiotics (cefoperazone/sulbactam 2 g q8 h), and then we did percutaneous transhepatic cyst drainage under CT guidance (Figure 1G). The cyst fluid appeared yellowish-brown and milky, which indicated infection with biliary communication. The body temperature gradually decreased to normal 4 d after drainage. She was discharged 14 d after drainage.
Two months after drainage was performed, the infected cyst had disappeared, and the drainage tube was removed (Figure 1H). No recurrence was observed during the 4 years after drainage (Figure 1I). At present, it has been more than 7 years since the operation, and the patient has not suffered from cyst infection or fever in more than 4 years.
Simple hepatic cysts are common and usually asymptomatic, only rarely causing symptoms and complications, such as infection, intracystic hemorrhage, rupture and obstructive jaundice[3]. As far as we know, no previous case reports have described hepatic cyst infection lasting over 3 years. There were two infected cysts in this case; the first was cured after long-term antibiotic therapy, but the diameter of the second cyst increased significantly after infection, and the cyst had to be treated by drainage. This finding led us to wonder why the fever related to the second cyst infection was difficult to control with antibiotics alone. The main reason was that this cyst was large and compressed the bile duct and caused obstructive jaundice and severe infection along with cholangitis and bacteremia.
Due to the abnormal levels of the serum AST, ALT, ALP, and GTP, as well as the presence of fever and other evidence of an inflammatory response in the laboratory tests, such as an increased WBC count and CRP level, and because the patient had no history of liver cyst infection prior to surgery, we believed that the cause of the patient’s recurrent fever was cholangitis, which often occurs after pancreaticoduodenectomy. When the Oddi sphincter is resected after pancreaticoduodenectomy, the incidence of postoperative cholangitis ranges from 6%-25%[4-6]. However, it was later confirmed to be a hepatic cyst infection. The patient’s repeated episodes of fever did not recur after the infected cyst was drained.
The diagnosis of hepatic cyst infection usually needs to be confirmed with imaging findings, such as internal heterogeneity, liquid debris level, thickened wall and edge enhancement with peripheral edema[7]. However, in the early stage of infection, imaging examination may not always show positive results. In fact, changes in the cystic contents may not occur for at least one month after infection[8]. This patient did not exhibit imaging abnormalities until 4 mo after the first fever. Therefore, repeated imaging examinations should be performed in suspected patients.
In general, bacterial infection of a hepatic cyst may arise from the bile duct, the portal vein, hematogenous transmission, direct invasion of a nearby infected focus, or trauma[3]. The main route of infection is supposed to be biliary tract approach, as communication between the cyst and the bile duct has been frequently observed[2,3,9], and the causative bacteria are mostly intestinal bacteria such as Klebsiella pneumoniae and Escherichia coli[10]. This patient had no history of infected liver cysts prior to pancreatoduodenectomy, so biliary reconstruction may be the cause of the infection.
Antimicrobial treatment alone is not sufficient to completely resolve cyst infection and prevent its recurrence, with 64% of patients requiring puncture drainage or surgical treatment[11]. Our case shows that antimicrobial treatment alone may cure hepatic cyst infection, but it requires long-term administration and repeated treatment, whereas antimicrobial treatment combined with percutaneous cyst drainage can control the infection quickly. If we had performed puncture and drainage earlier, the patient might not have needed such a long duration of antibacterial treatment.
Therefore, biliary reconstruction should be considered a risk factor for hepatic cyst infection. We suggest that hepatic cyst infection be treated with antibiotics followed by puncture and drainage. Of course, for multiple cysts, it is also important to identify which cysts are infected.
Biliary reconstruction can induce hepatic cyst infection, which is easily misdiagnosed as biliary reflux infection, and it can be difficult to identify the infected focus during the early stage when multiple cysts are present. Repeated imaging examination is a good method for identifying the infected focus. Antimicrobial treatment and percutaneous cyst drainage represent a simple and effective method to control infection.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Apiratwarakul K, Thailand; Sivanand N, India S-Editor: Chen YL L-Editor: A P-Editor: Chen YL
| 1. | Gaines PA, Sampson MA. The prevalence and characterization of simple hepatic cysts by ultrasound examination. Br J Radiol. 1989;62:335-337. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 144] [Cited by in RCA: 117] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 2. | Kudou K, Ninomiya M, Iguchi T, Harimoto N, Itoh S, Harada N, Takeishi K, Yamashita Y, Yoshizumi T, Soejima Y, Ikeda T, Shirabe K, Maehara Y. Cystic liver infection after living donor liver transplantation: a case report. Case Rep Gastroenterol. 2014;8:169-174. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Mizumoto Y, Mizuno S, Nakai Y, Tanaka E, Suzuki T, Noguchi K, Nakamura T, Sato T, Ishigaki K, Takeda T, Hakuta R, Saito K, Uchino R, Takahara N, Kogure H, Tada M, Koike K. Cholangitis complicated by infection of a simple hepatic cyst. Clin J Gastroenterol. 2018;11:493-496. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 4. | Ito Y, Abe Y, Kitago M, Itano O, Kitagawa Y. Predictive factors of late cholangitis in patients undergoing pancreaticoduodenectomy. World J Surg Oncol. 2018;16:19. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 5. | Malgras B, Duron S, Gaujoux S, Dokmak S, Aussilhou B, Rebours V, Palazzo M, Belghiti J, Sauvanet A. Early biliary complications following pancreaticoduodenectomy: prevalence and risk factors. HPB (Oxford). 2016;18:367-374. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 6. | Imai H, Osada S, Tanahashi T, Sasaki Y, Tanaka Y, Okumura N, Matsuhashi N, Nonaka K, Nagase M, Takahashi T, Yamaguchi K, Yoshida K. Retrospective evaluation of the clinical necessity of external biliary drainage after pancreaticoduodenectomy. Hepatogastroenterology. 2013;60:2119-2124. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 7. | Morii K, Yamamoto T, Nakamura S, Okushin H. Infectious Hepatic Cyst: An Underestimated Complication. Intern Med. 2018;57:2123-2129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Shoji F, Kitamura M, Shirabe K, Kai H, Akiyoshi T, Sugimachi K. Infected hepatic cyst in a patient with multiple hepatic cysts: report of a case diagnosed by change of ultrasonographic findings. Eur J Gastroenterol Hepatol. 2000;12:703-705. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Klingler PJ, Gadenstätter M, Schmid T, Bodner E, Schwelberger HG. Treatment of hepatic cysts in the era of laparoscopic surgery. Br J Surg. 1997;84:438-444. [PubMed] |
| 10. | Mori E, Akai Y, Matsumoto T, Kawaratani H, Horii M, Iwano M, Uemura S, Nonomura A, Fukui H, Saito Y. Hepatic cyst infection in a healthy older male. BMJ Case Rep. 2012;2012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Lantinga MA, Geudens A, Gevers TJ, Drenth JP. Systematic review: the management of hepatic cyst infection. Aliment Pharmacol Ther. 2015;41:253-261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 25] [Article Influence: 2.5] [Reference Citation Analysis (0)] |