Published online Sep 6, 2022. doi: 10.12998/wjcc.v10.i25.8954
Peer-review started: January 23, 2022
First decision: May 11, 2022
Revised: May 19, 2022
Accepted: July 27, 2022
Article in press: July 27, 2022
Published online: September 6, 2022
Processing time: 214 Days and 18.5 Hours
Quadricuspid aortic valve (QAV) is a very rare congenital cardiac defect with the incidence of 0.0125%-0.033% (< 0.05%) predominantly causing aortic regur
A 60-year-old female patient was referred for transthoracic ultrasound of the heart as part of a routine examination in the treatment of arterial hypertension. She did not have any significant symptoms. QAV was confirmed and there were no elements of valve stenosis with moderate aortic regurgitation. At first, it seemed that in the projection of the presumed left coronary cusp, there were two smaller and equally large cusps along with two larger and normally developed cusps. Cardiac CT imaging was performed to obtain an even more precise valve morphology and it showed that the location of the supernumerary cusp is between the right and left coronary cusp, with visible central malcoaptation of the cusps. Also, coronary computed angiography confirmed the right-type of myocardial bridging at the distal segment of the left anterior descending coronary artery. Significant valve dysfunction often occurs in middle-aged patients and results in surgical treatment, therefore, a 1-year transthoracic echocardiogram control examination and follow-up was recommended to our patient.
This case highlights the importance of diagnosing QAV since it leads to progressive valve dysfunction and can be associated with other congenital heart defects which is important to detect, emphasizing the role of cardiac CT and MRI.
Core Tip: The recognition of quadricuspid aortic valve (QAV) has clinical significance as it leads to progressive aortic valve dysfunction (aortic regurgitation in the majority), which can be severe enough for surgical correction and can be associated with other congenital heart defects - in our case, right-ventricular type of myocardial bridging at the distal segment of the left anterior descending coronary artery. Therefore, these patients require appropriate diagnosis, careful clinical evaluation and follow-up in order to be properly treated. Cardiac computed tomography, as well as magnetic resonance, is a useful imaging modality for comprehensively assessing of QAV.
- Citation: Sopek Merkaš I, Lakušić N, Paar MH. Quadricuspid aortic valve and right ventricular type of myocardial bridging in an asymptomatic middle-aged woman: A case report. World J Clin Cases 2022; 10(25): 8954-8961
- URL: https://www.wjgnet.com/2307-8960/full/v10/i25/8954.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i25.8954
Except for the mitral valve which morphologically has two leaflets, the other three heart valves are normally trileaflet. The aortic and pulmonary valves are known as semilunar valves. Semilunar valve formation begins during the 4th week of gestation. The improper fusion or the incomplete dedifferentiation of endocardial cushions is responsible for the formation of anatomically and structurally congenitally abnormal aortic valves[1]. The most common pathophysiological variant seen in everyday clinical practice is bicuspid aortic valve, occurring in 1%-2% of the population, with a 2:1 predominance among men[2]. Unicuspid aortic valve is also one of the variants of congenital valvular defect with an incidence of 0.02% in the general population[3]. The rarest pathophysiological variant in clinical practice is the QAV with a very low incidence of 0.0125%-0.033% in the general population[4]. Each of the described pathophysiological defects of the aortic valve is more prone to accelerated degeneration in the form of stenosis and/or insufficiency in comparison with morphologically normal tricuspid aortic valve and it is treated mostly by surgery or with transcatheter intervention.
A 60-year-old female patient was referred for transthoracic ultrasound of the heart as part of a routine examination because of long-term arterial hypertension treatment. In daily life she reported no significant symptoms in the form of shortness of breath, chest pain or headache. She did not experience syncope or dizziness.
The patient had well-regulated arterial hypertension managed with a combination of losartan and hydrochlorothiazide (50/12.5 mg). Cholesterol levels were within range managed with a low dose statin therapy (atorvastatin 10 mg).
Apart from arterial hypertension for the last 10 years and dyslipidemia that was treated for 2 years, the patient does not have other chronic diseases. In the family, there were no sudden deaths or known cardiovascular diseases.
There are no documented cardiovascular illnesses in the family.
Blood pressure was 120/75 mmHg, heart rate 68/min. Heart murmur was not described in clinical status and there were no clinical signs of heart failure (no edema of limbs, without lung crackles). Abdomen was not painful and liver and spleen were not enlarged.
Complete blood count was normal, as well as biochemistry and urine analysis. Cholesterol was 5.0 mmol/L and LDL-cholesterol 2.2 mmol/L. Electrocardiogram showed normal sinus rhythm 71/min with no elements of left ventricular hypertrophy (LVH).
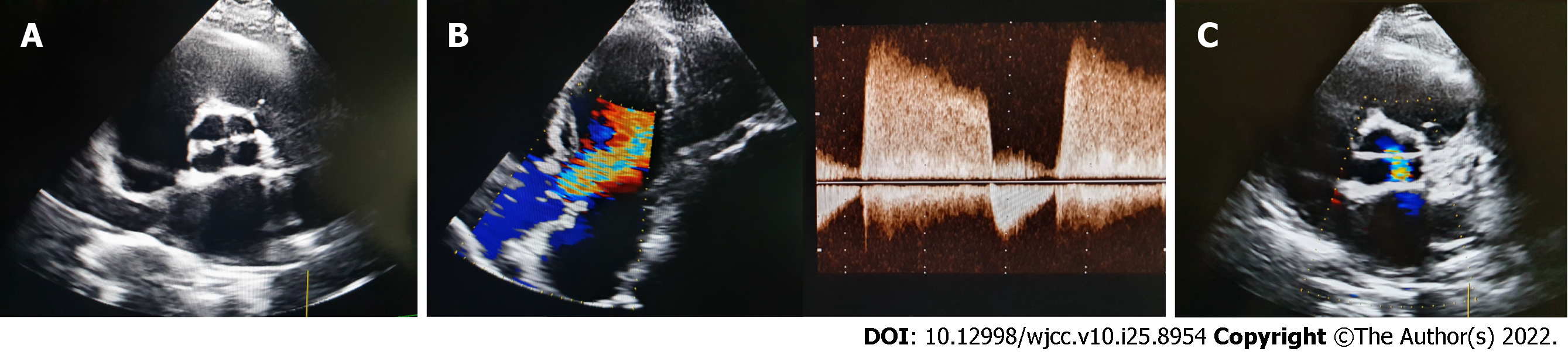
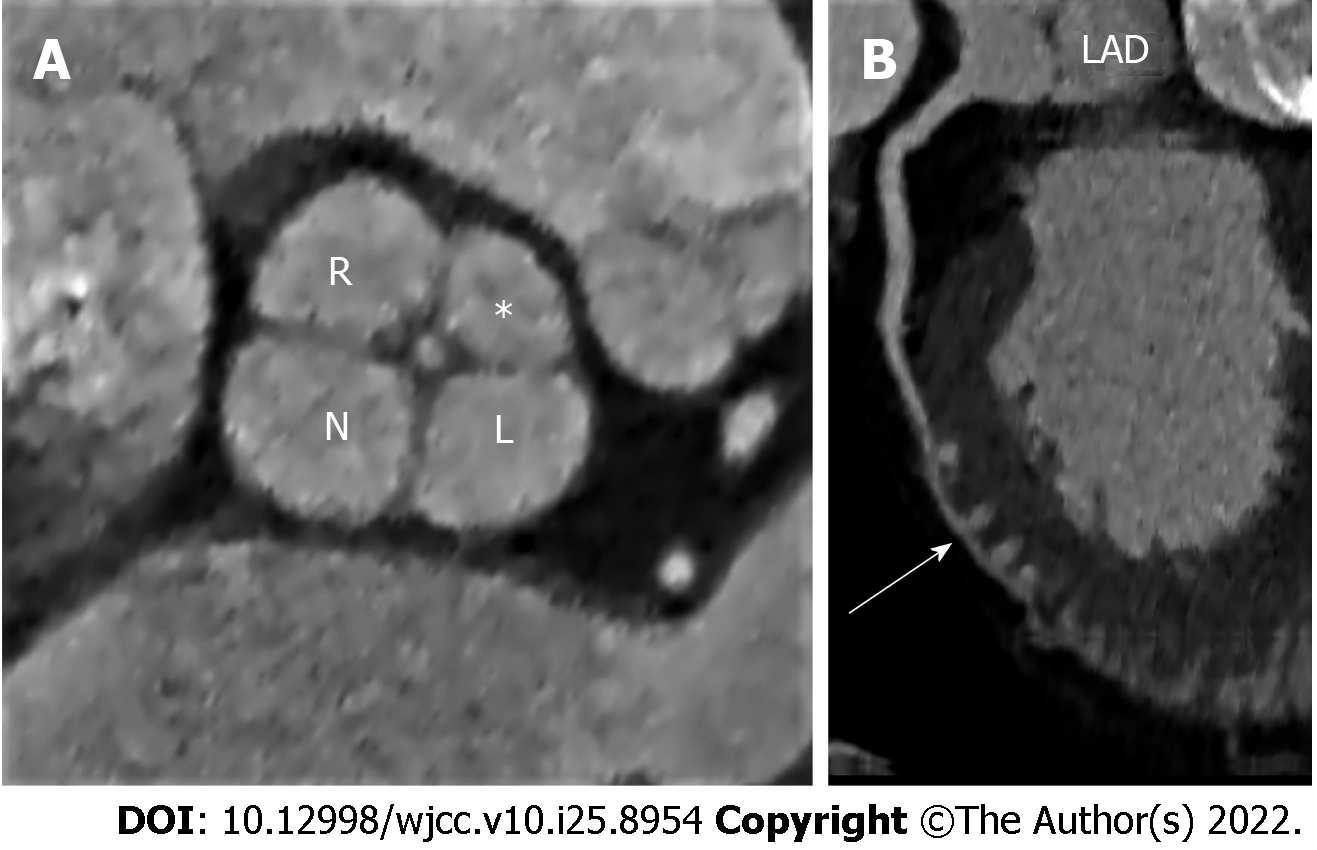
Transthoracic echocardiogram (TTE) verified normal dimensions of left ventricle (LV) (left ventricular end-diastolic diameter - LVDd 5.1 cm; end-diastolic volume - EDV 118 mL), without LVH (wall thickness 0.9 cm, LVmass 165 g), no regional wall motion abnormalities, with normal global systolic function [LV ejection fraction (EF) - Teichholz 66%, Simpson biplane 65%] and second-degree diastolic dysfunction of the LV (E/A 1.2, dt 220 ms, E/e' 10, during Valsalva maneuver E/A 0.6). Mitral valve function was normal and there were no indirect signs of pulmonary hypertension while resting. The aorta was of normal diameter at all levels (annulus, bulbus, sinotubular junction, ascending segment, and arcus). QAV was verified and at first it seemed that in the projection of the presumed left coronary cusp, there were two smaller and equally large cusps along with two larger and normally developed cusps (Figure 1A). There were no elements of QAV stenosis (aortic valve area planimetric — 3 cm2) with moderate aortic regurgitation (vena contracta 5 mm, pressure half time — PHT 499 ms, retrograde pressure gradient 45 mmHg, according to the depth of the jet in LV angio 3+, reversal flow in descending aorta 0.14 m/s), (Figure 1B and C, Video). Ascending aorta measured 27 mm. The diagnostic algorithm was then extended with multislice computed tomography (MSCT) imaging to obtain an even more precise QAV morphology and it showed that the location of the supernumerary cusp (asterisk) is between the right and left coronary cusp, with visible central malcoaptation of the cusps (Figure 2A). Coronary CT angiography (CCTA) confirmed the right ventricular type of myocardial bridging at the distal segment of the left anterior descending (LAD) coronary artery (Figure 2B). In this type of myocardial bridging, an intramuscular artery segment is running in the right ventricular anterior wall or in the right ventricular cavity[5]. Other possible associated pathologies such as abnormally located coronary ostia, patent foramen ovale, etc were excluded. Since the patient was asymptomatic, the medicament therapy remained the same. A 1-year TTE control examination was recommended.
The final diagnosis of the presented case is QAV with the location of the supernumerary cusp (asterisk) between the right and left coronary cusp and associated anomaly of the right-ventricular type of myocardial bridging at the distal segment of the LAD.
The recommendation of medicament therapy for arterial hypertension and dyslipidemia remained the same. It was explained to the patient that QAV can lead to progressive valve dysfunction (in this case insufficiency) which can lead to surgical aortic valve replacement. Also, she was instructed to pay attention to possible symptoms - dyspnea, chest discomfort, palpitations, syncope, edema of the legs, etc. It is unclear whether patients with QAVs have increased risk for infective endocarditis, though it has been reported, and antibiotic prophylaxis against infective endocarditis in the QAV patients with unequal-sized cusps is suggested[6] in the case of dental, respiratory tract procedures, gastrointestinal or urogenital procedures. In ESC guidelines there is currently no recommendation regarding infective endocarditis prophylaxis for these patients[7].
A 1-year TTE control examination was recommended. At the control examination the patient was stable, still asymptomatic and without valvular disease progression.
QAV was first described in 1862 by Balington[8]. In the PubMed database QAV was first mentioned in 1958[9]. QAV is an extremely rare congenital anomaly and depending on the observed population the incidence of QAV ranges from 0.0125%-0.033% in the general population[4], 0.00028%-0.00033% in the autopsy series, 0.0059%-0.0065% for patients undergoing TTE and 0.05%-0.1% for patients undergoing aortic valve replacement due to aortic regurgitation[6].
The mechanisms of QAV development remain unclear. Abnormal septation of the conotruncus and abnormal septation of one of the endocardial cushions as a result of an inflammatory episode is a possible pathophysiological mechanism of QAV development[6].
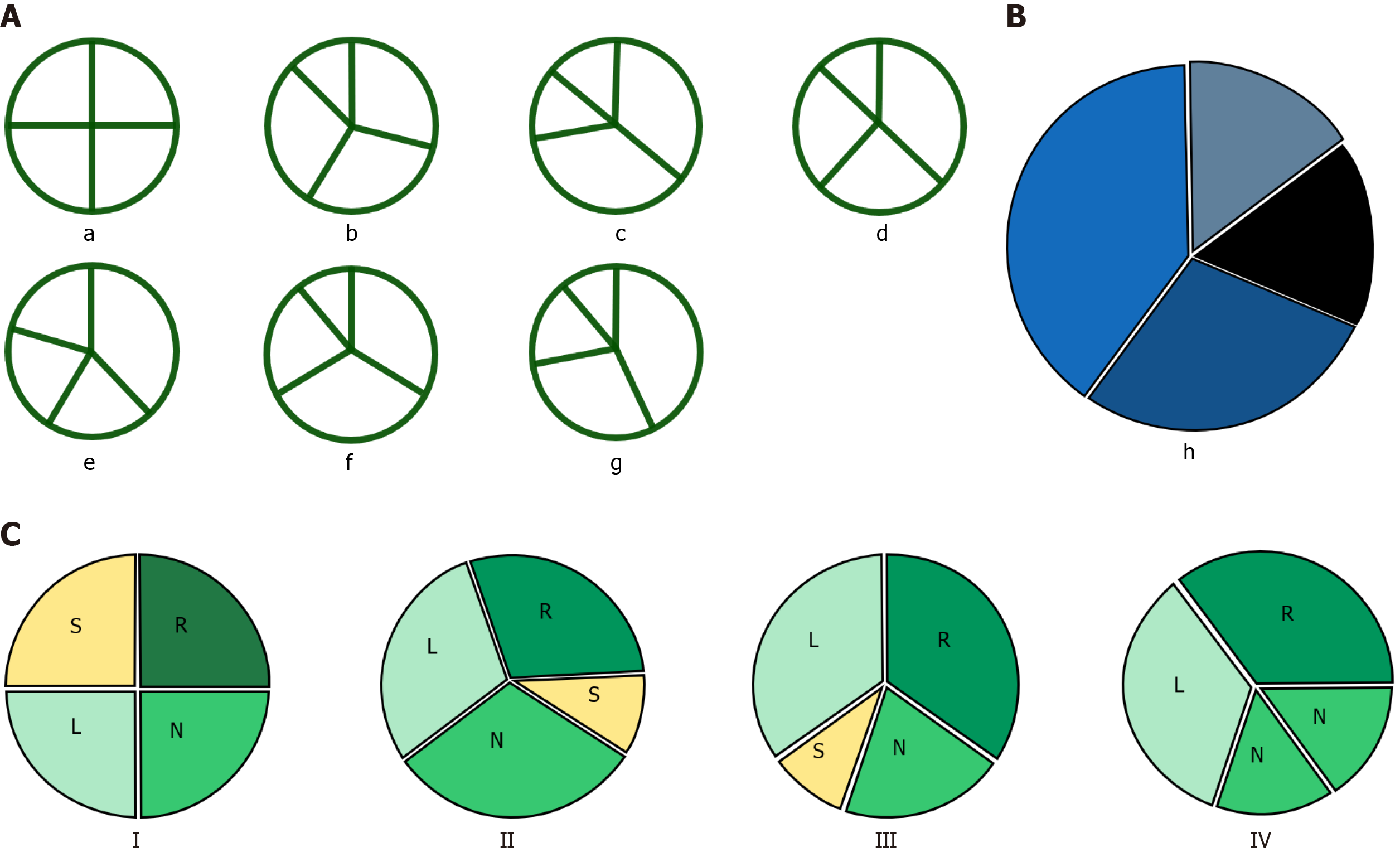
There are several QAV classification schemes according to the morphology of the cusps. The Hurwitz and Roberts classify and divide QAV into 7 types from A to G based on the relative size of the supernumerary cusp (Figure 3A)[10]. Type A, B and C represent more than 85% of the cases. At first, according to the TTE, we considered that our patient has a type C morphology of QAV (two equal larger cusps and two equal smaller cusps). However, CT confirmed type B form of QAV (three equal-sized cusps and one smaller cusp). Vali et al[11] supplemented the original Hurwitz and Roberts classification with type H of QAV (Figure 3B). Furthermore, Nakamura et al[12] designed a simplified classification by focusing on the position of the supernumerary cusp (Figure 3C) where our patient falls in Type I (supernumerary cusp between the left and right coronary cusps).
QAV commonly occurs as an isolated defect but has been associated with the aortic dilatation[13] as well as other congenital heart defects such as patent foramen ovale[14] and ductus arteriosus[15], atrial and ventricular septal defect[16,17], subaortic stenosis[18], hypertrophic cardiomyopathy[19], etc (Table 1). Coronary ostium and anomalies of the coronary arteries are the most frequently associated disorders in patients with QAV. For example, malformation and displacement of coronary ostia is found in 10% of patients with a QAV[6]. Thus, CCTA confirmed that our patient has the right-ventricular type of myocardial bridging at the distal segment of the LAD coronary artery. Myocardial bridging is a congenital coronary anomaly, mostly benign and asymptomatic. However, it can be associated with myocardial ischemia, exertional angina, ventricular arrhythmias, acute coronary syndrome, sudden death, etc. Symptoms may appear in case of LVH, vasospasm, diastolic and microvascular dysfunction. The prevalence varies considerably depending on the diagnostic method used (CCTA — 25%, coronary angiography — 0.5%-16%) and emphasizes the difference of significant functional findings from an anatomic finding[20].
| Atrial septal defect |
| Ventricular septal defect |
| Patent ductus arteriosus |
| Mitral valve regurgitation |
| Mitral valve prolapse |
| Sinus of Valsalva fistula |
| Subaortic fibromuscular stenosis |
| Hypertrophic non-obstructive cardiomyopathy |
| Transposition of the great arteries |
| Tetralogy of Fallot |
| Ehlers-Danlos syndrome |
| Coronary artery and coronary ostium anomalies |
Aortic valvular insufficiency is commonly observed in QAV. It occurs secondary to a central orifice formed from malcoaptation of the four valvular leaflets[6,21,22]. In addition to aortic, associated mitral regurgitation is possible[23].
The basic diagnostic method of detecting QAV is TTE with further confirmation of the diagnosis using transesophageal echocardiography (TEE). TEE is a more sensitive method than TTE and it can additionally visualize the coronary ostia. However, echocardiography is a subjective method — it is operator-dependent and its diagnostic value depends on several factors (e.g., suboptimal acoustic windows, subject body habitus, and in cases of uncertain valvular anatomy, differential diagnosis[24] (Table 2) and may require additional imaging)[25]. MSCT and MRI are complementary methods in detecting possible associated anomalies and differential diagnosis[12,25,26].
| Tumor of the valve |
| Valvular degeneration (with possible calcification) |
| Thrombus |
| Vegetations |
Multiple clinical courses are possible for patients with QAV. At a younger age (< 20 years), patients usually have no difficulties and the anomaly is accidentally found at routine TTE examinations. Significant QAV dysfunction often occurs in middle-aged patients and results in a surgical treatment. About one-third of the patients with QAV require aortic valve surgery[26] and patients’ complaints are mostly related to congestive heart failure (CHF) symptoms due to stenosis and/or significant valve insufficiency[27].
Treatment of severe dysfunctional QAV (stenosis and/or insufficiency) includes aortic valve repair (required skill and experience of a cardiac surgeon), surgical aortic valve replacement and transcatheter aortic valve replacement[28-32].
QAV is a very rare congenital cardiac defect. It is often detected accidentally at a routine TTE exa
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Croatia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Hong X, China; Vyshka G, Albania S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Gong ZM
| 1. | Anderson RH, Webb S, Brown NA, Lamers W, Moorman A. Development of the heart: (3) formation of the ventricular outflow tracts, arterial valves, and intrapericardial arterial trunks. Heart. 2003;89:1110-1118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 162] [Cited by in RCA: 139] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 2. | Malouf JF, Edwards WD, Tajik AJ, Seward J. Functional anatomy of the heart. In: Fuster V, O’Rourke RA, Walsh RA, editors. Hurst’s The Heart, 12th ed. New York: McGraw-Hill Companies, Inc; 2008. |
| 3. | Novaro GM, Mishra M, Griffin BP. Incidence and echocardiographic features of congenital unicuspid aortic valve in an adult population. J Heart Valve Dis. 2003;12:674-678. [PubMed] |
| 4. | Feldman BJ, Khandheria BK, Warnes CA, Seward JB, Taylor CL, Tajik AJ. Incidence, description and functional assessment of isolated quadricuspid aortic valves. Am J Cardiol. 1990;65:937-938. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 131] [Cited by in RCA: 136] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Konen E, Goitein O, Sternik L, Eshet Y, Shemesh J, Di Segni E. The prevalence and anatomical patterns of intramuscular coronary arteries: a coronary computed tomography angiographic study. J Am Coll Cardiol. 2007;49:587-593. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 124] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 6. | Yuan SM. Quadricuspid Aortic Valve: A Comprehensive Review. Braz J Cardiovasc Surg. 2016;31:454-460. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 38] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 7. | Habib G, Lancellotti P, Antunes MJ, Bongiorni MG, Casalta JP, Del Zotti F, Dulgheru R, El Khoury G, Erba PA, Iung B, Miro JM, Mulder BJ, Plonska-Gosciniak E, Price S, Roos-Hesselink J, Snygg-Martin U, Thuny F, Tornos Mas P, Vilacosta I, Zamorano JL; ESC Scientific Document Group. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur Heart J. 2015;36:3075-3128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2661] [Cited by in RCA: 3346] [Article Influence: 334.6] [Reference Citation Analysis (0)] |
| 8. | Tai JM, Laghari AH, Gill CT. Quadricuspid aortic valve with aortic regurgitation: a rare echocardiographic finding. BMJ Case Rep. 2013;2013. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | McCOLL I. Pericarditis due to a mycotic aneurysm in subacute bacterial endocarditis; report of a case affecting congenitally stenosed quadricuspid aortic valve. Guys Hosp Rep. 1958;107:34-47. [PubMed] |
| 10. | Hurwitz LE, Roberts WC. Quadricuspid semilunar valve. Am J Cardiol. 1973;31:623-626. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 240] [Cited by in RCA: 260] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 11. | Vali Y, Rajendra R, Nishtar S. A previously undescribed type of quadricuspid aortic valve: type H. J Heart Valve Dis. 2010;19:792-793. [PubMed] |
| 12. | Nakamura Y, Taniguchi I, Saiki M, Morimoto K, Yamaga T. Quadricuspid aortic valve associated with aortic stenosis and regurgitation. Jpn J Thorac Cardiovasc Surg. 2001;49:714-716. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 49] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Tsang MY, Abudiab MM, Ammash NM, Naqvi TZ, Edwards WD, Nkomo VT, Pellikka PA. Quadricuspid Aortic Valve: Characteristics, Associated Structural Cardiovascular Abnormalities, and Clinical Outcomes. Circulation. 2016;133:312-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 69] [Cited by in RCA: 101] [Article Influence: 11.2] [Reference Citation Analysis (0)] |
| 14. | Honda A, Tahara N, Shojima T, Fukumoto Y. Multimodal imaging of quadricuspid aortic valve in elderly patient. Eur Heart J Case Rep. 2021;5:ytab344. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 15. | Seol SH, Kim U, Cho HJ, Kim DK, Kim DI, Kim DS. Quadricuspid aortic valve with patent ductus arteriosus. Tex Heart Inst J. 2010;37:726-727. [PubMed] |
| 16. | Sousa L, Pinto F, Nogueira G, Kaku S, Antunes AM. Quadricuspid aortic valve and atrial septal defect. Rev Port Cardiol. 2001;20:329-330. [PubMed] |
| 17. | Demirkol S, Balta S, Arslan Z, Unlu M, Kucuk U, Iyisoy A. Association of quadricuspid aortic valve and ventricular septal defect in a patient who had undergone atrial septal defect surgery. Kardiol Pol. 2013;71:546. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Iglesias A, Oliver J, Muñoz JE, Nuñez L. Quadricuspid aortic valve associated with fibromuscular subaortic stenosis and aortic regurgitation treated by conservative surgery. Chest. 1981;80:327-328. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 27] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 19. | Janssens U, Klues HG, Hanrath P. Congenital quadricuspid aortic valve anomaly associated with hypertrophic non-obstructive cardiomyopathy: a case report and review of the literature. Heart. 1997;78:83-87. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 60] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 20. | Kanwal A, Shah AB. Myocardial bridging in adults. American College of Cardiology 2020. Available from: https://www.acc.org/Latest-in-cardiology/articles/2020/08/04/08/48/myocardial-bridging-in-adults. |
| 21. | Godefroid O, Colles P, Vercauteren S, Louagie Y, Marchandise B. Quadricuspid aortic valve: a rare etiology of aortic regurgitation. Eur J Echocardiogr. 2006;7:168-170. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 23] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Vasudev R, Shah P, Bikkina M, Shamoon F. Quadricuspid Aortic Valve: A Rare Congenital Cause of Aortic Insufficiency. J Clin Imaging Sci. 2016;6:10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 23. | Zhu J, Zhang J, Wu S, Zhang Y, Ding F, Mei J. Congenital quadricuspid aortic valve associated with aortic insufficiency and mitral regurgitation. J Cardiothorac Surg. 2013;8:87. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Franco A, Gabriel S, Ruehm SG. The quadricuspid aortic valve. J Radiol Case Rep. 2014;8:25-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Saith S, Saith S, Murthy A. Quadricuspid Aortic Valve: An Introduction for Clinicians. Cardiol Res. 2022;13:2-10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 15] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 26. | Manuel AM, Ladeiras-Lopes R, Ribeiro J, Ferreira ND, Faria R, Carvalho M, Ferreira W, Ferraz R, Gonçalves F, Batista A, Gonçalves C, Pires-Morais G, Rodrigues A, Sampaio F, Teixeira M, Braga P, Fontes-Carvalho R. Prevalence, multimodality imaging characterization, and mid-term prognosis of quadricuspid aortic valves: an analysis of eight cases, based on 160 004 exams performed during 12 years in a tertiary care hospital. Eur Heart J Cardiovasc Imaging. 2021;22:765-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 27. | Jagannath AD, Johri AM, Liberthson R, Larobina M, Passeri J, Tighe D, Agnihotri AK. Quadricuspid aortic valve: a report of 12 cases and a review of the literature. Echocardiography. 2011;28:1035-1040. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 28. | Schmidt KI, Jeserich M, Aicher D, Schäfers HJ. Tricuspidization of the quadricuspid aortic valve. Ann Thorac Surg. 2008;85:1087-1089. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 29. | Song MG, Yang HS, Lee DH, Shin JK, Chee HK, Kim JS. Mid-term results in patients having tricuspidization of the quadricuspid aortic valve. J Cardiothorac Surg. 2014;9:29. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 30. | Langer F, Aicher D, Kissinger A, Wendler O, Lausberg H, Fries R, Schäfers HJ. Aortic valve repair using a differentiated surgical strategy. Circulation. 2004;110:II67-II73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 49] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 31. | Idrees JJ, Roselli EE, Arafat A, Johnston DR, Svensson LG, Sabik JF 3rd, Pettersson GB. Outcomes after repair or replacement of dysfunctional quadricuspid aortic valve. J Thorac Cardiovasc Surg. 2015;150:79-82. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 44] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 32. | Zhou D, Fan J, Liu X, Wang J. The First Two Cases of Long-Term Outcomes After Transcatheter Aortic Valve Replacement in Patients With Quadricuspid Aortic Valve. J Invasive Cardiol. 2021;33:E839-E840. [PubMed] |
| 33. | Song I, Park JA, Choi BH, Ko SM, Shin JK, Chee HK, Kim JS. Morphological and Functional Evaluation of Quadricuspid Aortic Valves Using Cardiac Computed Tomography. Korean J Radiol. 2016;17:463-471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.4] [Reference Citation Analysis (0)] |