Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.7973
Peer-review started: January 2, 2022
First decision: April 8, 2022
Revised: May 16, 2022
Accepted: June 26, 2022
Article in press: June 26, 2022
Published online: August 6, 2022
Processing time: 200 Days and 19.1 Hours
Delayed arterial symptomatic epidural hematoma (SEH) on the 14th day after posterior lumbar interbody fusion (PLIF) is rare but it may lead to severe complications if not identified and treated in a timely manner. After diagnosis of the current case, early surgical removal of the hematoma and strict hemostasis treatment was accomplished. This case report highlights the importance of swift diagnosis and treatment in SEH patients.
A 41-year-old male patient with a single-segment lumbar disc herniation underwent left-side PLIF. On the 14th post-operative day, the patient complained of lumbar incision pain with sudden onset accompanied by left limb radiation pain and aggravated cauda equina symptoms. Magnetic resonance imaging examination and a puncture blood draw at the incision site confirmed a delayed arterial SEH. Emergency surgical removal of the hematoma and hemostasis was performed. About 70 mL of hematoma was found in the left incision. Continuous bleeding was found in the anterior branch of the transverse process of the 4th lumbar artery in the muscle area about 2 cm below the transverse process of the 4th lumbar vertebra. A blood jet of about 10 cm in height was observed and bipolar electrocoagulation was used to stop the bleeding. Post-operative lumbar incision pain and left lower limb pain were relieved immediately and gradually disappeared. There was no recurrence during the 12-mo follow-up.
For delayed arterial SEH on the 14th day after PLIF, preventive measures including pre-, intra- and post-operative prevention should be implemented.
Core Tip: Posterior lumbar interbody fusion (PLIF) is a standard surgical method for the treatment of lumbar disc herniation. Delayed arterial symptomatic epidural hematoma is an infrequent complication after lumbar spine surgery, occurring with extreme rarity as late as the 14th day after PLIF. Without timely diagnosis and treatment, clinical consequences could be severe. Once the complication had been found in the present case, early surgical hematoma removal and strict hemostasis treatment were required.
- Citation: Hao SS, Gao ZF, Li HK, Liu S, Dong SL, Chen HL, Zhang ZF. Delayed arterial symptomatic epidural hematoma on the 14th day after posterior lumbar interbody fusion: A case report. World J Clin Cases 2022; 10(22): 7973-7981
- URL: https://www.wjgnet.com/2307-8960/full/v10/i22/7973.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i22.7973
Epidural hematoma (EH) is a common complication following posterior lumbar surgery. It has been reported that EH could be detected by imaging in approximately 33%-100% of patient’s post-operation[1] with most showing no clinical symptoms. Indeed, the incidence of asymptomatic EH may be as high as 58%[2]. Clinical symptoms of lumbar symptomatic epidural hematoma (SEH) include sudden severe spontaneous waist pain following lumbar spine surgery with compression symptoms after a few minutes to a few days and sphincter dysfunction below the site of the pain. In extreme cases, paraplegia may develop. The aforementioned are the typical clinical features of EH usually occurring within 72 h of surgery and SEH occurring 5 to 16 h after surgery. When SEH occurs more than 72 h post-surgery, it can be defined as a delayed SEH[3] which has an incidence rate of 0.17%[4]. Posterior lumbar interbody fusion (PLIF) is a surgical treatment for lumbar disc herniation, and delayed arterial SEH after PLIF is an infrequent and severe complication. Cases of delayed arterial SEH occurring on the 14th day after PLIF are extremely rare, highlighting the importance of raising clinicians’ awareness about their diagnosis and treatment.
The current report describes the treatment of a sporadic rare patient with delayed arterial SEH on the 14th day after PLIF. This case represents the first patient with SEH following PLIF observed by orthopedic doctors and anesthesiologists in our hospital for decades. Given the rarity of this condition, a comprehensive review and analysis of the existing literature was conducted. The aim of this case report is to analyze the possible causes of delayed arterial SEH, introduce treatment methods and explore preventive measures. Meanwhile, we hope to encourage other clinicians to increase their vigilance against delayed arterial SEH after PLIF and provide some references for the diagnosis and treatment of this serious complication.
A 41-year-old male patient, 174 cm tall and weighing 85 kg, was admitted to our hospital with the chief complaint of "left lower limb pain for more than 7 mo and worsening over the previous 20 d".
The patient developed left calf pain due to fatigue for more than 7 mo with numbness of his left hip and foot and limited mobility. The symptoms gradually worsened. Bed rest, physical therapy and drug therapy brought no relief. The above symptoms had worsened during the 20 d prior to admission.
The patient had a 2-year history of hypertension for which he usually received "amlodipine besylate tablets" (5 mg po. qd.).
The patient was a 41-year-old Chinese man, non-smoker with a blood type O and rhesus positive.
Oral history revealed poor spirit, poor sleep, average diet, stool dysfunction and regular urination. Physiological curvature of the lumbar spine was present without kyphosis, scoliosis or lordosis and with a reduced degree of motion. Left lower limb muscle strength was a level 4, and right was a level 5. The muscle tension of both lower limbs was normal. The patient reported feeling weakness in the left hip, left calf and left foot while the right limb was normal. The left knee-tendon reflex was weaker while the right was normal. The left Bragard sign was positive while the right was negative. Babinski’s sign was negative on both sides. There was no edema in either lower limb and normal blood supply.
Coagulation function test: Prothrombin time (PT): 11.30 s; PT%: 93.00%; international normalized ratio (INR): 1.04; fibrinogen C (FC): 3.5 g/L; activated partial thromboplastin time (APTT): 39.80 s; thrombin time (TT): 15.69 s and fibrin (original) degradation product (FDP): 1.04 μg/mL. These results were all within normal ranges.
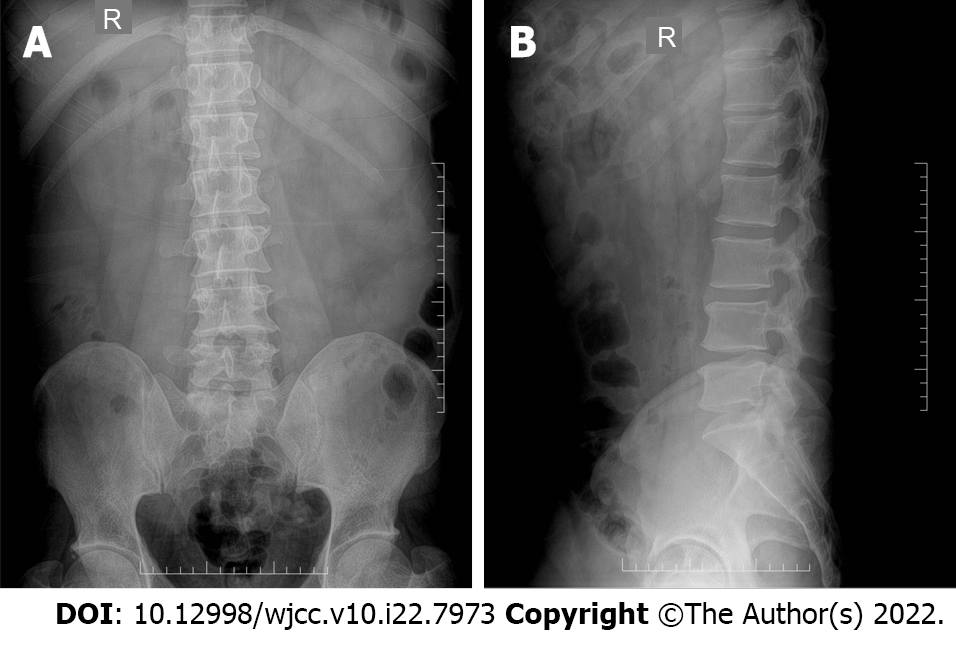
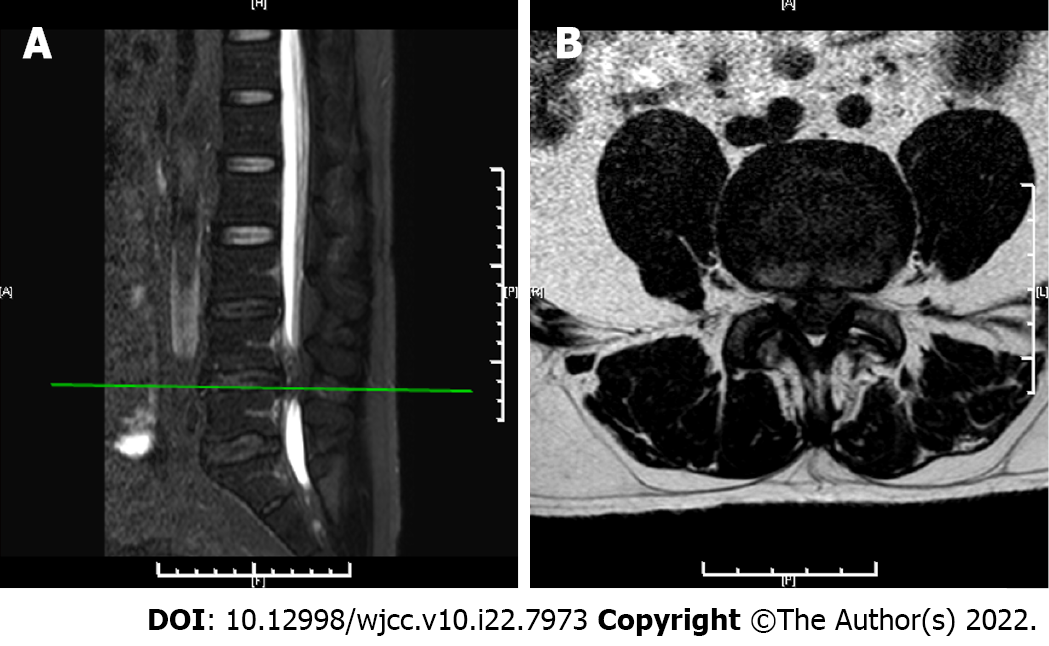
X-ray examination showed that the intervertebral space of the 4th/5th lumbar vertebrae had shrunk (Figure 1). Computed tomography (CT) scan indicated a herniated disc of the 4th/5th lumbar vertebrae (Figure 2). Magnetic resonance imaging (MRI) revealed a herniated disc of the 4th/5th lumbar vertebrae (Figure 3).
Patient diagnosis: (1) Lumbar disc herniation with cauda equina injury; and (2) Hypertension.
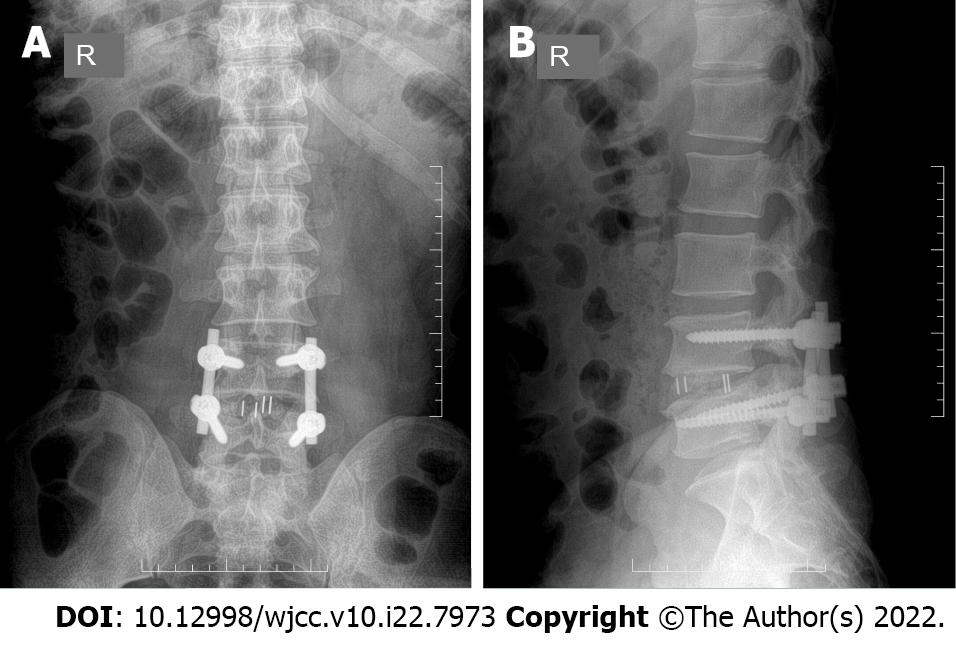
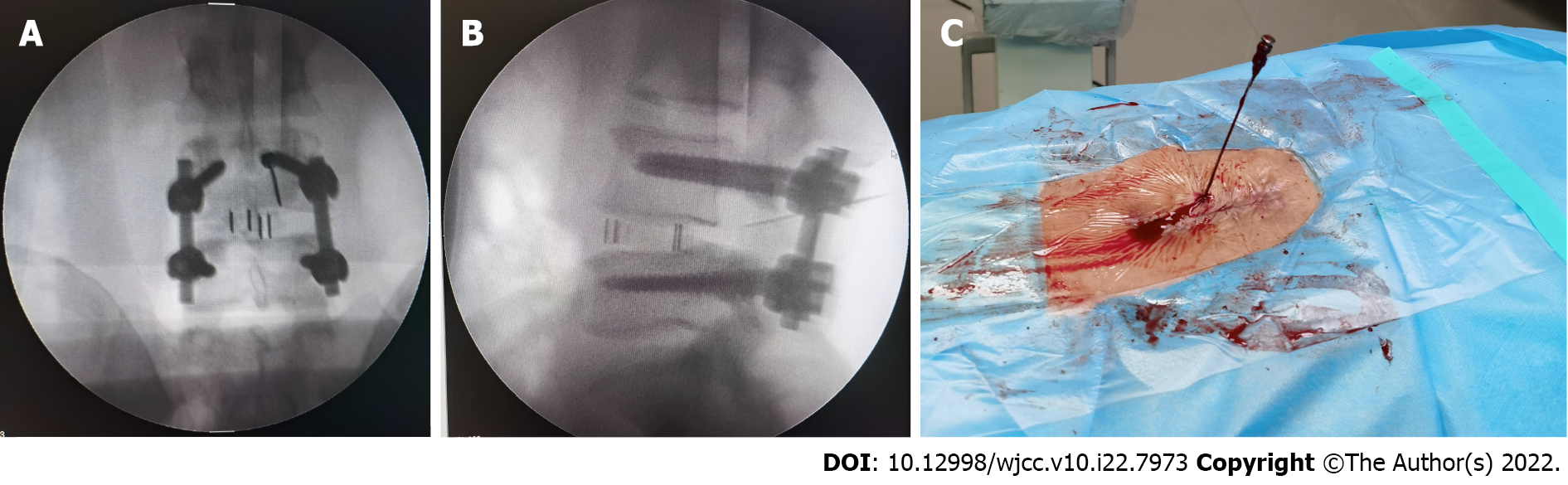
After pre-operative preparation, the patient underwent a successful surgery of "left-side PLIF" on the 4th day after admission. The operation time was 120 min with an intra-operative blood loss of 600 mL, placement of 2 drainage tubes and no blood transfusion. The patient's left calf pain and left hip and foot numbness were significantly reduced post-operatively. Within the 24 h post-operative period, low-molecular-weight heparin was used for anti-coagulation to prevent deep vein thrombosis (DVT). Coagulation function test on the 1st post-operative day showed PT: 12.80 s; PT%: 76.00%; INR: 1.18; FC: 3.48 g/L; APTT: 33.40 s; TT: 15.13 s and FDP: 1.04 μg/mL. These results were similar to those of the pre-operative coagulation function test. After the operation, the drainage tube was unobstructed and drainage volume gradually decreased: 1st post-operative day: 120 mL; 2nd post-operative day: 80 mL; and 3rd post-operative day: 40 mL before drainage tube removal on the 3rd post-operative day. After pulling out the drainage tube, the pain and numbness of the left lower limb were gradually alleviated. Re-examination of lumbar spine X-rays on the 4th post-operative day indicated satisfactory positions of the lumbar spine fixation and fusion cage (Figure 4).
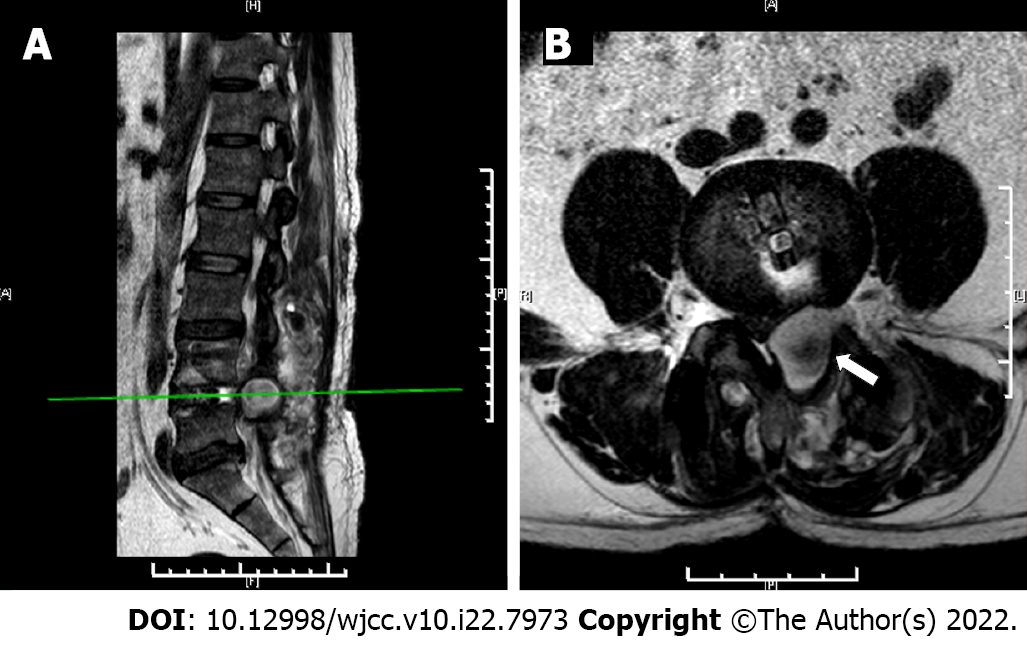
On the 14th post-operative day, the patient reported sudden incision pain. Physical examination revealed no noticeable swelling and redness at the waist incision but evident tenderness. The pain was partially relieved by applying analgesics. On the 15th post-operative day, the patient experienced increased pain at the waist incision, accompanied by symptoms similar to those before the operation including left calf pain, left hip and foot numbness and stool dysfunction. Physical examination revealed a slight swelling of the skin at the incision with pain and aggravation of lower limb pain on pressure. The left Bragard sign was positive while the right was negative. The MRI scan revealed abnormal signals in the left area of the 4th/5th lumbar vertebral body with possible hematoma formation (Figure 5). After departmental consultation, the possibility of a delayed post-operative SEH was indicated. It was considered that the patient experienced symptoms of spinal cord and nerve compression due to possible hematoma formation in the lumbar incision. Immediate puncture of the hematoma with tube placement for drainage was scheduled. This minimally invasive operation was designed to allow the hematoma to be drained and the patient's symptoms to be relieved without significant impact on the incision. Puncture treatment was performed under C-arm X-ray machine fluoroscopy. When the puncture needle broke through the muscle tissue, bright red blood could be seen gushing out of the puncture needle core with continuous pulsation (Figure 6). The diagnosis of delayed arterial SEH after PLIF was confirmed.
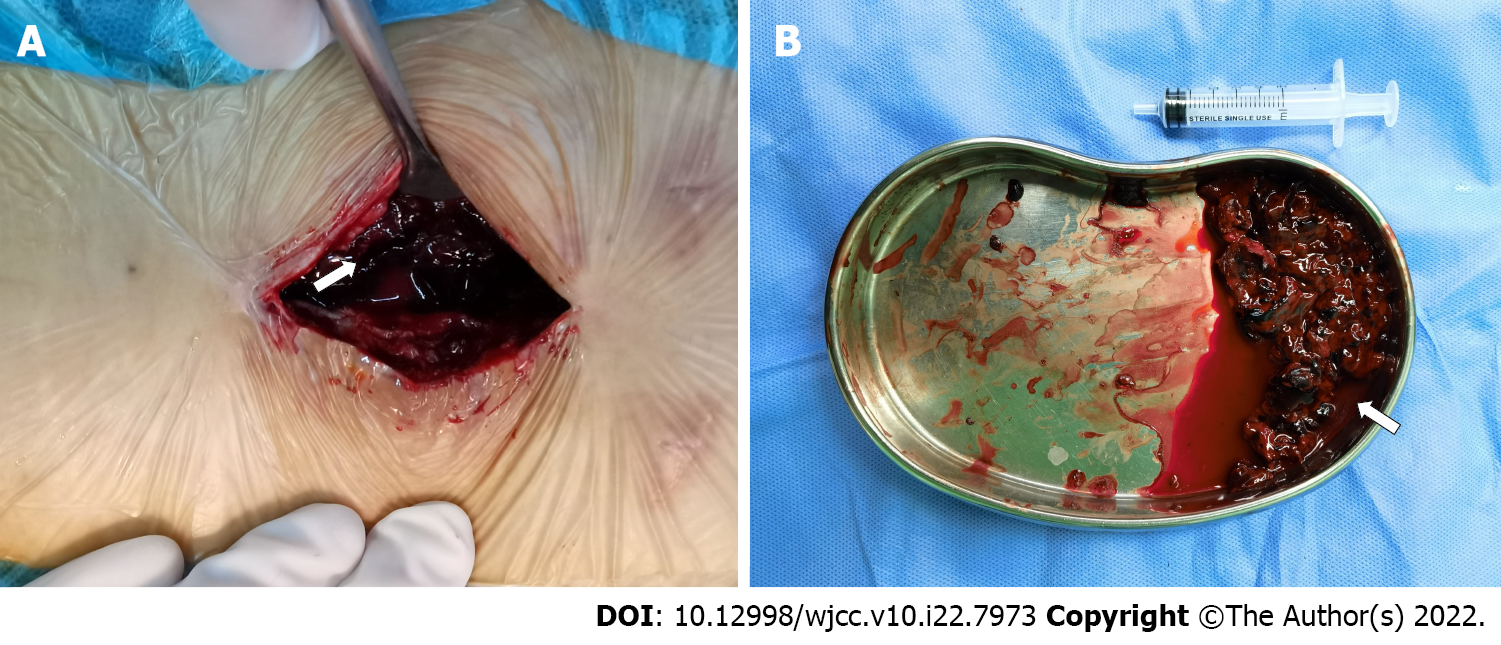
Emergency surgery was performed to stop the bleeding and remove the hematoma. During the 2nd operation, a large hematoma in the left incision with compression around the nerve root became apparent. After the removal of about 70 mL of blood clot (Figure 7), a small artery, an anterior branch of the transverse process of the 4th lumbar artery, was found to be the source of continuous bleeding. The artery location was in the muscle tissue area about 2 cm below the transverse process of the 4th lumbar vertebra on the left. The pressure of the gushing blood was high and the height of the bleeding jet reached about 10 cm. Careful bipolar coagulation was used to stop the bleeding and hemostatic gelatin sponge was packed to enhance the hemostatic effect. After flushing of the surgical incision and ensuring of no bleeding point in the incision, it was sutured with placement of a drainage tube. The outcome of the operation was very successful. The operation time was 75 min with intra-operative blood loss of 100 mL. The patient’s pain and numbness were significantly reduced after the operation. Within 24 h, low-molecular-weight heparin was used for anti-coagulation to prevent DVT.
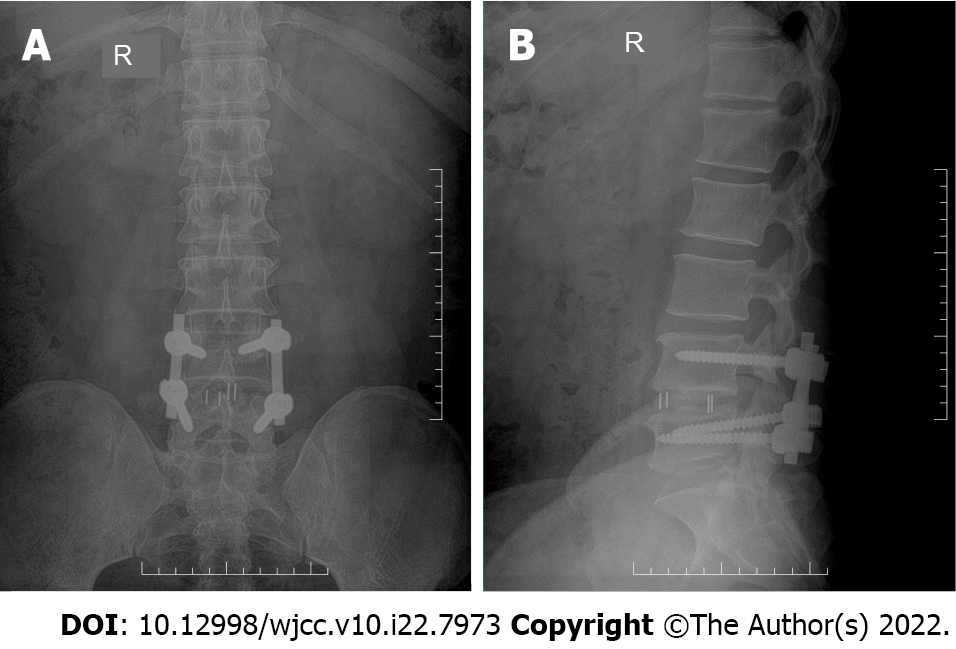
A coagulation function test on the 1st day after the 2nd operation showed PT: 11.60 s; PT%: 89.00%; INR: 1.07; FC: 3.41 g/L; APTT: 38.30 s and TT: 16.97 s, which were similar to those of the previous two laboratory tests. The drainage tube was unobstructed and drainage volume gradually decreased: (1) Post-operative day: 90 mL; (2) Post-operative day: 60 mL; and (3) Post-operative day: 30 mL before drainage tube removal on the 3rd post-operative day. Waist incision and left lower limb pain continued to decline, and reached zero at the 12th day after the 2nd operation, when the patient was discharged. Only mild left foot and left hip numbness and mild symptoms of stool dysfunction remained. Stool dysfunction was relieved 2 mo after discharge and left foot and hip numbness vanished after 6 mo. There was no recurrence of symptoms on 9 and 12 mo follow-ups (Figures 8 and 9). The patient expressed satisfaction with his treatment.
PLIF is a standard surgical method for the treatment of lumbar disc herniation. Bleeding was inevitable at the post-operative decompression site and EH was estimated to form at the decompression or adjacent segment[5]. As the localized space is enlarged after PLIF, nerve compression symptoms generally do not occur. However, SEH represents a particular type of EH accompanied by symptoms of spinal cord or nerve compression. Clinical manifestations include severe swelling and pain at the waist incision, inability to lie flat, pain not wholly responsive to analgesics and irritability. In addition, some patients experience radicular pain, low muscle strength and reduced sensation in the lower limbs with severe cases being complicated by cauda equina syndrome and even paraplegia. SEH after PLIF is an infrequent and severe complication with severe consequences contingent on failure to diagnose and treat the condition in a timely manner. Therefore, early diagnosis and surgery are critical for the treatment of SEH[6]. Delayed arterial SEH on the 14th day after PLIF is a very rare and severe complication. The current case report is designed to raise awareness of this complication among other spinal doctors and provide references for diagnosis, treatment and prevention.
A literature review revealed diverse views on the causes of post-operative EH or SEH. Kao et al[7] believed that the use of an intra-operative gelatin sponge was a risk factor for EH. Kou et al[3] reported that multi-segment spinal surgery increased the risk of epidural venous plexus injury, leading to the formation of EH. Post-operative blockage of the wound drainage tube has also been proposed as a contributory factor[8], as have multi-segment decompression, improper use of hemostatic materials, abnormal drainage, use of anti-coagulants and incomplete hemostasis and spinal revision surgery[9]. Sokolowski et al[5] suggested that the use of low-molecular-weight heparin after surgery might increase the risk of EH, albeit that most examples of EH were asymptomatic and required no treatment. However, it has also been reported that early administration of low-molecular-weight heparin does not increase the risk of EH if lumbar spine surgery was accompanied by hemostasis and adequate drainage[10]. An EH multiple regression model analysis showed that the pre-surgery risk factors were age > 65 years and revision surgery, and the risk factors during surgery were surgery time > 120 min, blood loss > 600 mL and intra-operative infusion of frozen plasma[11]. It is clear that further research is required to fully identify the specific causes of EH or SEH. However, each of the reasons mentioned above is a possible factor, indicating the need for vigilance in clinical work.
Both veins and arteries can contribute to bleeding during SEH. Rupture of the epidural venous plexus (Batson venous plexus) has been suggested as a cause of bleeding[12], as has local arterial rupture since the speed and quantity of blood produced are commensurate with the rapid clinical progression of SEH[13]. Hu et al[14] reported a case of delayed arterial SEH caused by delayed lumbar perforating arterial bleeding in the 2nd week after PLIF. The patient experienced unbearable soreness and discomfort in the lumbosacral area and a burning sensation on urination. After 5 h, he experienced increased numbness in both lower limbs, and was unable to move below the ankles and control urination. Emergency surgery was performed to remove the hematoma and stop the bleeding, after which the patient's lower limb muscle strength gradually recovered after the 2nd post-operative week, stool function recovered after the 1st month and urine function recovered after the 7th month.
The current case involved bleeding from the anterior branch of the transverse process of the 4th lumbar artery. The vessel issued close to the lower edge of the root of the upper transverse process and ran slightly to the ventral side from the inside to the outside, passed through the transverse process and travelled outward and downward to enter the muscle fascia tissue. This was consistent with the bleeding site we found during the 2nd operation. Intra-operative exposure of the transverse process beyond the boundary of its lower edge might damage the artery. Moreover, when using intra-operative bipolar coagulation to stop bleeding, it should be administered close to the root of the lower edge of the transverse process to avoid damaging the nerve roots in the exit area of the deep intervertebral foramina[15]. Our patient's pain and neurological symptoms were alleviated immediately after the operation and had disappeared completely by the 12th post-operative day. The patient's stool dysfunction disappeared after the 2nd month and the left foot and hip numbness disappeared after the 6th month. There was no recurrence by the 12 mo of follow-up. It can be seen that the symptoms of delayed arterial SEH caused by the rupture of lumbar arteries were severe and the recovery process prolonged.
We consider that there are three main reasons why this severe complication might have affected the present case. Firstly, post-operative administration of anti-coagulant drugs to reduce the incidence of DVT in patients after lumbar surgery may be a factor. Low-molecular-weight heparin is a drug of choice which reduces the incidence of DVT after spinal surgery but also carries a low risk of EH and other bleeding events[16]. Generally, post-operative application of anti-coagulant drugs does not increase the risk of EH and SEH in our clinical experience, but which drugs produce the most favorable outcomes and whether the use of such drugs can confer an increased risk of SEH remain unclear. Secondly, hypertension may contribute to the increased fragility of blood vessels. The current patient had a 2-year history of hypertension and fluctuations of blood pressure may have caused rupture and hemorrhage of local arterioles. Thirdly, an increase in abdominal pressure due to constipation and cough after surgery may cause fluctuations in arterial pressure contributing to the likelihood of rupture and bleeding. All of the above factors may have interacted to cause SEH or one factor may predominate due to the changes in local tissue structure and vertebral body mechanics after PLIF. The mobility of the lumbar spine was reduced and restrictions in the range of motion might cause damage and rupture of the small artery vessels. Initial local accumulation of blood was cleared by the body on spontaneous cessation of bleeding but changes in biomechanics and long-term stress damage might cause repeated rupture of small blood vessels, forming hematoma and eventually SEH[17].
Delayed arterial SEH is a rare and severe complication which requires prompt diagnosis and emergency surgical treatment. We identify three main items for diagnosis. Firstly, sudden onset of clinical symptoms, such as sudden lumbar incision pain and progressive aggravation accompanied by symptoms of compression of lower limb nerve function and impaired cauda equina nerve function. Secondly, MRI scans reveal the location, scope, size of the hematoma and changes following compression of the dural sac. A preliminary prognosis could be made by analyzing the size of the hematoma and the degree of nerve displacement. Thirdly, a punctured blood draw from the surgical incision site not only confirms the diagnosis but if bright red blood with continuous pulsation from the needle core is found, it will help to reduce the patient's symptoms of nerve involvement. Therefore, we recommend the uses of MRI scanning and puncture blood operation, although the patient's clinical symptoms remain the most valuable diagnosis. On presentation of the symptoms, the operation should be performed quickly following discussion with the patient. Surgical treatment aims to remove the hematoma and stop the bleeding but also relieves the patient's lumbar incision pain and nerve involvement symptoms.
Early detection, diagnosis and treatment are essential for preventing delayed arterial SEH. Further measures are required to prevent its recurrence. We have combined our clinical experience with our survey of the literature to summarize pre-, intra- and post-operative preventive methods[18]. Firstly, pre-operative prevention includes improved laboratory tests, imaging and control of primary diseases. Secondly, intra-operative prevention includes strict hemostasis[19]. For example, bone wax could be used to stop bleeding during bone oozing, bipolar coagulation or gauze compression during venous bleeding and bipolar coagulation during arterial bleeding. Thirdly, post-operative prevention includes placement of a drainage tube through the incision which must remain unobstructed, monitoring and control of blood pressure, anti-tussive action, avoidance of frequent changes in body position, prevention of constipation and the rational use of anti-coagulant drugs.
In summary, delayed arterial SEH is an infrequent complication after lumbar spine surgery and is extremely rare as late as the 14th day after PLIF. Serious consequences are likely in the absence if there is timely discovery and treatment. We hope, by our research regarding this case, to increase clinicians’ understanding and vigilance regarding this condition and also to provide some reference material for diagnosis, treatment and prevention.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Belosludtseva NV, Russia; Subramanian A, India S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | Ikuta K, Tono O, Tanaka T, Arima J, Nakano S, Sasaki K, Oga M. Evaluation of postoperative spinal epidural hematoma after microendoscopic posterior decompression for lumbar spinal stenosis: a clinical and magnetic resonance imaging study. J Neurosurg Spine. 2006;5:404-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 58] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 2. | Glotzbecker MP, Bono CM, Wood KB, Harris MB. Postoperative spinal epidural hematoma: a systematic review. Spine (Phila Pa 1976). 2010;35:E413-E420. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 142] [Cited by in RCA: 114] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 3. | Kou J, Fischgrund J, Biddinger A, Herkowitz H. Risk factors for spinal epidural hematoma after spinal surgery. Spine (Phila Pa 1976). 2002;27:1670-1673. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 241] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 4. | Uribe J, Moza K, Jimenez O, Green B, Levi AD. Delayed postoperative spinal epidural hematomas. Spine J. 2003;3:125-129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 101] [Cited by in RCA: 102] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 5. | Sokolowski MJ, Garvey TA, Perl J 2nd, Sokolowski MS, Cho W, Mehbod AA, Dykes DC, Transfeldt EE. Prospective study of postoperative lumbar epidural hematoma: incidence and risk factors. Spine (Phila Pa 1976). 2008;33:108-113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 121] [Cited by in RCA: 127] [Article Influence: 7.5] [Reference Citation Analysis (0)] |
| 6. | Zhang Z, Zhao WD, Wu DS, Zhao DL. The diagnosis and treatment of epidural hematomas after lumbar surgery. The J Cervicodynia Lumbodynia. 2013;34:133-135. [DOI] [Full Text] |
| 7. | Kao FC, Tsai TT, Chen LH, Lai PL, Fu TS, Niu CC, Ho NY, Chen WJ, Chang CJ. Symptomatic epidural hematoma after lumbar decompression surgery. Eur Spine J. 2015;24:348-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 92] [Article Influence: 8.4] [Reference Citation Analysis (0)] |
| 8. | Mirzai H, Eminoglu M, Orguc S. Are drains useful for lumbar disc surgery? J Spinal Disord Tech. 2006;19:171-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 76] [Cited by in RCA: 95] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 9. | Hong J, Liu Q, Huang L, Wu N, Ao Q, Gong X. Analysis and prevention of spinal epidural hematoma following lumbar spine decompression and internal fixation. J Clin Orthop. 2015;18:414-417. [DOI] [Full Text] |
| 10. | Dong Z, Xu J, Zhang B, Wu J, Gao Y, Wang Z, Ding W. Association of low molecular weight heparin anticoagulation and epidural hematoma formation application after lumbar surgery. The J Cervicodynia Lumbodynia. 2015;36:138-140. [DOI] [Full Text] |
| 11. | Wang Q, Zhang L, Ji Q, Wang X, Sun C. Postoperative lumbar spinal epidural hematoma: risk factors and clinical outcomes. Zhonguo Jizhu Jisui Zazhi. 2015;25:815-819. [DOI] [Full Text] |
| 12. | Groen RJ, Ponssen H. The spontaneous spinal epidural hematoma. A study of the etiology. J Neurol Sci. 1990;98:121-138. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 238] [Cited by in RCA: 226] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 13. | Liu C, Liang S, Wei J, Huang S, Chen W. Early diagnosis and treatment of epidural hematoma after lumbar spine surgery. The J Cervicodynia Lumbodynia. 2011;32:134-135. [DOI] [Full Text] |
| 14. | Hu Z, Yu X, Yang J, Jiao Y. A case of sudden epidural hematoma 2 wk after lumbar spine surgery and review of related literature. Zhongguo Jiaoxing Waike Zazhi. 2018;26:861-863. |
| 15. | Cheng Y, Sun Z, Li R, Fang Q, Wang G, Ren J. Observation of lumbar zygapophyseal joints adjacent arterials by anatomy and DSA. Zhonghua Yixue Zazhi. 2015;95:2198-2201. [DOI] [Full Text] |
| 16. | Yi W, Liang B, Chen F, Qiu D, Wei J, Wei M, Chu Y, Li S, Ji D. Risk factors for early lower extremity deep venous thrombosis after posterior lumbar interbody fusion. Zhonguo Jizhu Jisui Zazhi. 2017;27:823-828. [DOI] [Full Text] |
| 17. | Li J, Wei C, Zheng C, Liu J. Delayed organized epidural hematoma after lumbar surgery: one case report. J Med Imaging. 2019;29:2178-2179. |
| 18. | Wang LF, Li XB, Wang CL, Chang HR, Liu KY, Chen T, Meng XZ. Research progress of symptomatic spinal epidural hematoma after posterior lumbar surgery. Shiyong Guke Zazhi. 2018;24:438-440. |
| 19. | Chen J, Qi Q, Guo Z, Li W, Zeng Y, Sun C. The management of symptomatic epidural hematoma after the posterior lumbar surgery. Zhonguo Jizhu Jisui Zazhi. 2015;25:733-738. [DOI] [Full Text] |