Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.7931
Peer-review started: November 3, 2021
First decision: November 19, 2021
Revised: December 15, 2021
Accepted: June 27, 2022
Article in press: June 27, 2022
Published online: August 6, 2022
Processing time: 260 Days and 16.3 Hours
Primary hypertension is a common clinical disease. Pheochromocytoma and paraganglioma is a rare cause of secondary hypertension. The diagnosis of the latter is still difficult, and the relationship between the two is not clear. The successful diagnosis of this case confirmed that standardized etiological investigation of secondary hypertension is necessary, contributes to the accurate diagnosis of rare diseases, and is conducive to the formulation or optimization of treatment plans. It shows an example of the coexistence of primary hypertension and secondary hypertension.
The patient was a 54-year-old male and was hospitalized with high blood pressure for 4 years. The patient’s blood pressure was measured at 150/100 mmHg during physical examination 4 years ago and had no paroxysmal or persistent elevated blood pressure, no typical triad of headache, palpitation, and sweating, without postural hypotension. After taking nifedipine sustained release tablets intermittently, the blood pressure did not meet the standard. Physical examination revealed blood pressure of 180/120 mmHg. There was no abnor
Subclinical paraganglioma and primary hypertension can coexist. The holistic thinking in clinical practice is helpful to the early diagnosis of rare diseases.
Core Tip: Pheochromocytoma and paraganglioma (PPGL) is a rare cause of secondary hypertension, and early and accurate diagnosis is still facing challenges. A case of subclinical paraganglioma (PGL) complicated with essential hypertension was analyzed retrospectively. A typical and subclinical pheochromocytoma and PGL should be paid more attention due to the lack of clinical features. At the same time, standardized etiological investigation of secondary hypertension is also an indispensable part of an accurate diagnosis. Clinical practice has proven that subclinical PGL and essential hypertension are two independent diseases that can coexist. After reviewing the literature, it is considered that genetic susceptibility is the same pathogenic factor.
- Citation: Wei JH, Yan HL. Primary hypertension in a postoperative paraganglioma patient: A case report. World J Clin Cases 2022; 10(22): 7931-7935
- URL: https://www.wjgnet.com/2307-8960/full/v10/i22/7931.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i22.7931
Paraganglioma (PGL) is a rare cause of secondary hypertension that is manifested as a hypertensive crisis and easily leads to target organ damage. The reported prevalence of pheochromocytoma and paraganglioma (PPGL) is 0.2%–0.6%[1], with an incidence closely related to a germline gene mutation[2]. Surgery is the first option after diagnosis, resulting in a generally normal postoperative blood pressure. In this study, we present our findings on a confirmed case of combined postoperative PGL and primary hypertension.
A 54-year-old male had high blood pressure for 5 mo.
The patient’s blood pressure was 186/100 mmHg at a physical examination 5 mo ago without discomfort. However, taking a 20 mg nifedipine sustained-release tablet once daily did not normalize his blood pressure. He had stopped the medication 3 mo prior to the time of admission. Since the disease onset, he had maintained a good diet and slept without snoring.
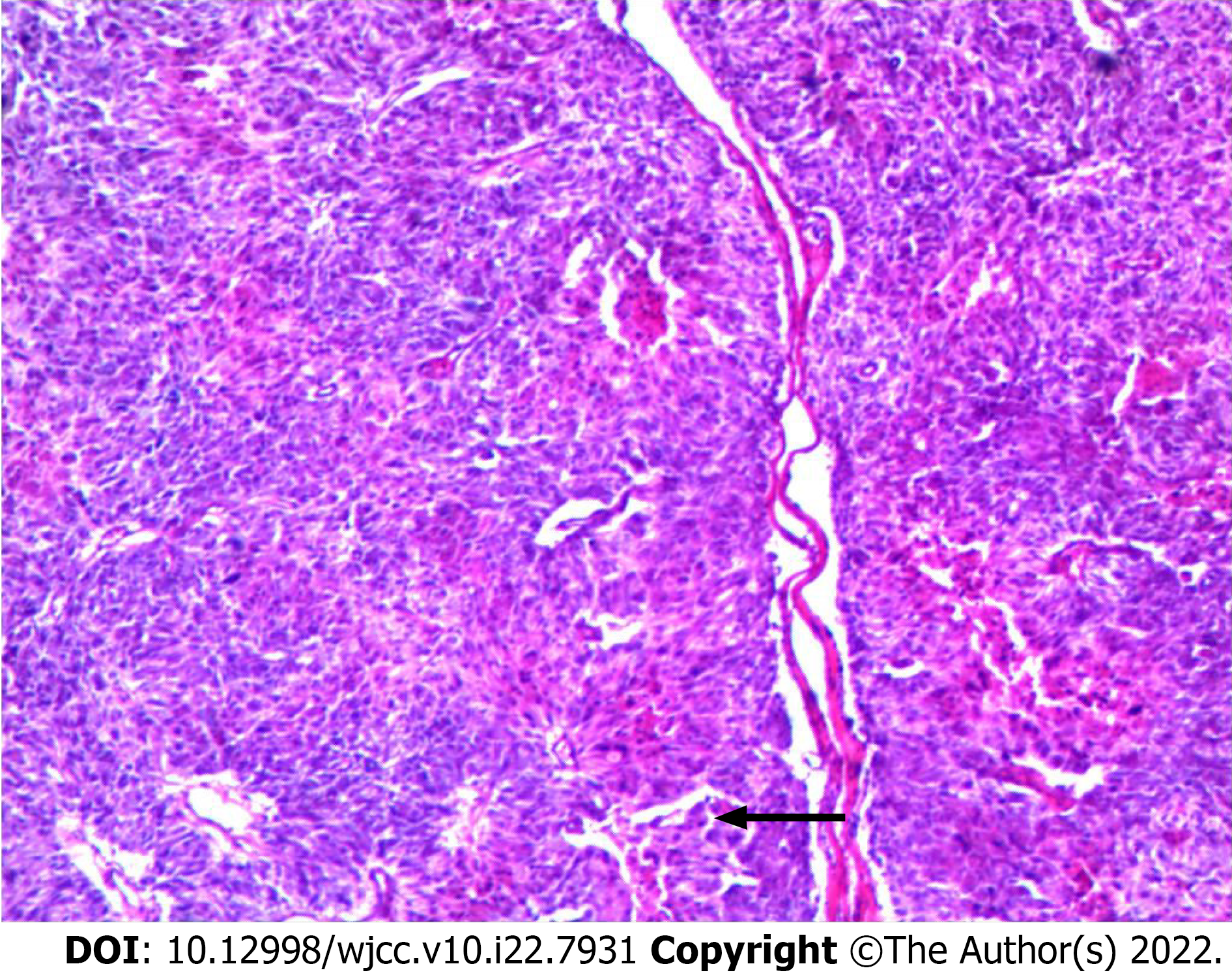
He had a history of PGL resection (Figure 1) and postoperative pathological diagnosis of PGL (Figure 2).
He had a history of passive smoking, and family history of hypertension, but no PPGL.
The physical examination at admission revealed a body temperature of 36.4 °C, pulse of 86 beats/min, breathing of 18 breaths/min, blood pressure of 188/108 mmHg, waist circumference of 96 cm, body mass index of 27.8 kg/m2, clear mind, good spirit, and no murmur in neck and umbilical blood vessels. No abnormality was detected in the heart, lungs, and abdomen. No edema was found in both lower limbs, and positive nervous system signs were observed.
Laboratory examinations revealed normal macrobiochemical parameters, thyroid function, parathyroid hormone levels, cortisol and adrenocorticotropic hormone levels, and rhythm as well as normal prolactin, antinuclear antibody spectrum, and 24-h urine protein levels. Blood aldosterone and renin were determined by chemiluminescence measurements (11.31). Metanephrine was 31.9 ng/L (reference range < 96.60 ng/L), detected by liquid chromatography-tandem mass spectrometry. Normetanephrine was 68.9 ng/L (reference range < 163.00 ng/L).
Adrenal and renal artery computed tomography: Bilateral adrenal hyperplasia and right renal artery stenosis. Brain magnetic resonance imaging and chest, abdomen, and pelvic computed tomography were normal.
(1) Postoperative PGL; and (2) Primary hypertension with hypertensive retinopathy stage 2.
Felodipine sustained-release tablet of 5 mg was administered once daily combined with olmesar
The patient had no symptoms. At the last follow-up examination on April 23, 2021, the blood pressure was normal and stable.
Hypertension was defined as systolic blood pressure ≥ 140 mmHg and/or diastolic pressure ≥ 90 mmHg measured three times on a different day in the absence of antihypertensive medications. Secondary hypertension refers to hypertension caused by certain diseases or causes, accounting for about 5% of all hypertension, is characterized by endocrine dysfunction, such as primary aldosteronism and PPGL[3]. PGL patients, accounting for 15%–20% of all PPGL cases, have normal blood pressure without symptoms. They are distributed in the abdomen, chest, pelvic, neck, and brain tissue, especially in the retroperitoneum. A malignant tendency of PGL development has been reported, with a malignant transformation rate of 24%–50%[4]. No typical clinical manifestation of PPGL was observed in the present case.
The blood metanephrine was normal, and only the abdominal computed tomography revealed a left retroperitoneal mass. Importantly, postoperative pathological diagnosis of PGL should be differentiated from adrenocortical eosinophilic and low-grade neuroendocrine tumors[5]. The main difference among the three tumors is the intensity of the neuroendocrine markers; hence, we considered it was nonfunctional subclinical PGL, which was consistent with the results of previous studies[6,7]. PGL is curable secondary hypertension in which resection is to be performed after the diagnosis, which results in achieving normal postoperative blood pressure. This case completely differed from PPGL, with symptoms and positive examination results. It had high concealment, with no PPGL triad of headache, palpitation, sweating, and hypertension, and the specific marker of blood metanephrine was normal. The increase in the blood pressure occurred 3 years after the PGL operation.
Differential diagnosis and screening of PGL metastasis were performed based on the specific medical history, clinical manifestations, etiology of secondary hypertension, distribution of PGL, and the site of metastasis. Renal parenchymal hypertension, renovascular hypertension, primary aldosteronism, sleep apnea hypopnea syndrome, hypercortisolism, pituitary tumors, thyroid and parathyroid dysfunction, pharmacogenic hypertension, and connective tissue disorders, such as vasculitis and systemic sclerosis, were excluded[8,9]. No recurrence or metastasis was observed in PGL, and the diagnosis of primary hypertension was clear.
Meanwhile, because of the lack of family history of hypertension, middle age, short course of disease, mild target organ damage, and PGL history, this case was different from the commonly known primary hypertension. High blood pressure occurred after the PGL operation. The diagnosis of the combination of postoperative PGL and primary hypertension was confirmed by recurrence and metastasis screening. After reviewing the literature[9], the diagnosis of postoperative PGL was clear albeit rare in clinical practice. No related report was available of subclinical postoperative PGL and primary hypertension, and thus we had to make the differential diagnosis. This case has deepened the clinician’s under
Despite its rare occurrence, postoperative PGL patients can develop primary hypertension. The screening, diagnosis, and differential diagnosis of PPGL should be performed in cases with adrenal incidentaloma, retroperitoneal mass, or carotid body tumor. Pathological diagnosis is the gold standard for PPGL diagnosis.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Moshref L, Saudi Arabia; Moshref RH, Saudi Arabia S-Editor: Xing YX L-Editor: Filipodia P-Editor: Xing YX
| 1. | Endocrinology CSo; Association CM. Expert consensus on the diagnosis and treatment of pheochromocytoma and paraganglioma (2020). Zhonghua Neifenmi Daixie Zazhi. 2020;36:737-750. [DOI] [Full Text] |
| 2. | Zhang F, Kan W. New advances in genomics of pheochromocytomas and paragangliomas. World J Clin Oncol. 2018;45:969-972. [DOI] [Full Text] |
| 3. | Chen X, Cui Z, Lin J. Comment and key-points translation of International Society of Hypertension global hypertension practical guideline. Zhongguo Yixue Qianyan Zazhi. 2020;12:54-60. [DOI] [Full Text] |
| 4. | Ge J, Xu Y, Wang C. People's Medical Publishing House. J Intern Med. 710-712. [DOI] [Full Text] |
| 5. | Tong A, Li H. Neuroendocrine Neoplasias Related to Hypertension: Current Status and Progress. Xiehe Yixue Zazhi. 2020;11:361-364. [DOI] [Full Text] |
| 6. | Wang L, Ma R, Chang H. Clinicopathological analysis of adrenal pheochromocytoma. Linchuang Zhongliuxue Zazhi. 2020;25: 257-260. [DOI] [Full Text] |
| 7. | Eisenhofer G, Prejbisz A, Peitzsch M, Pamporaki C, Masjkur J, Rogowski-Lehmann N, Langton K, Tsourdi E, Pęczkowska M, Fliedner S, Deutschbein T, Megerle F, Timmers HJLM, Sinnott R, Beuschlein F, Fassnacht M, Januszewicz A, Lenders JWM. Biochemical Diagnosis of Chromaffin Cell Tumors in Patients at High and Low Risk of Disease: Plasma vs Urinary Free or Deconjugated O-Methylated Catecholamine Metabolites. Clin Chem. 2018;64:1646-1656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 75] [Cited by in RCA: 129] [Article Influence: 18.4] [Reference Citation Analysis (0)] |
| 8. | Li N. Clinical diagnosis and treatment of secondary hypertension. Zhonghua Gaoxueya Zazhi. 2014;22:516-518. [DOI] [Full Text] |
| 9. | Committee CHPaTGR; (China) HA, Cardiology HPCoCMDAoCAo, Exchanges HBoCAftPoIH, Society HBoCG. Chinese guidelines for the management of hypertensionWriting Group of 2018. Zhongguo Xinxueguan Zazhi. 2019;24:24-56. [DOI] [Full Text] |