Published online Aug 6, 2022. doi: 10.12998/wjcc.v10.i22.7738
Peer-review started: January 29, 2022
First decision: May 11, 2022
Revised: May 21, 2022
Accepted: June 17, 2022
Article in press: June 17, 2022
Published online: August 6, 2022
Processing time: 173 Days and 16.2 Hours
A low survival rate in patients with cardiac arrest is associated with failure to recognize the condition in its initial stage. Therefore, recognizing the warning symptoms of cardiac arrest in the early stage may play an important role in survival.
To investigate the warning symptoms of cardiac arrest and to determine the correlation between the symptoms and outcomes.
We included all adult patients with all-cause cardiac arrest who visited Peking University Third Hospital or Beijing Friendship Hospital between January 2012 and December 2014. Data on population, symptoms, resuscitation parameters, and outcomes were analysed.
Of the 1021 patients in the study, 65.9% had symptoms that presented before cardiac arrest, 25.2% achieved restoration of spontaneous circulation (ROSC), and 7.2% survived to discharge. The patients with symptoms had higher rates of an initial shockable rhythm (12.2% vs 7.5%, P = 0.020), ROSC (29.1% vs 17.5%, P = 0.001) and survival (9.2% vs 2.6%, P = 0.001) than patients without symptoms. Compared with the out-of-hospital cardiac arrest (OHCA) without symptoms subgroup, the OHCA with symptoms subgroup had a higher rate of calls before arrest (81.6% vs 0.0%, P < 0.001), health care provider-witnessed arrest (13.0% vs 1.4%, P = 0.001) and bystander cardiopulmonary resuscitation (15.5% vs 4.9%, P = 0.002); a shorter no flow time (11.7% vs 2.8%, P = 0.002); and a higher ROSC rate (23.8% vs 13.2%, P = 0.011). Compared to the in-hospital cardiac arrest (IHCA) without symptoms subgroup, the IHCA with symptoms subgroup had a higher mean age (66.2 ± 15.2 vs 62.5 ± 16.3 years, P = 0.005), ROSC (32.0% vs 20.6%, P = 0.003), and survival rates (10.6% vs 2.5%, P < 0.001). The top five warning symptoms were dyspnea (48.7%), chest pain (18.3%), unconsciousness (15.2%), paralysis (4.3%), and vomiting (4.0%). Chest pain (20.9% vs 12.7%, P = 0.011), cardiac etiology (44.3% vs 1.5%, P < 0.001) and survival (33.9% vs 16.7%, P = 0.001) were more common in males, whereas dyspnea (54.9% vs 45.9%, P = 0.029) and a non-cardiac etiology (53.3% vs 41.7%, P = 0.003) were more common in females.
Most patients had warning symptoms before cardiac arrest. Dyspnea, chest pain, and uncon
Core Tip: This was a retrospective study to investigate the correlation between the symptoms and the outcomes in cardiac arrest patients. A total of 65.9% of patients had symptoms before arrest. Dyspnea, chest pain, and unconsciousness were the most common symptoms. The patients with symptoms had a higher rate of initial shockable rhythm, restoration of spontaneous circulation (ROSC) and survival than patients without symptoms. The out-of-hospital cardiac arrest symptoms subgroup had a higher rate of bystander cardiopulmonary resuscitation, a shorter no flow time, and a higher ROSC rate. The in-hospital cardiac arrest symptoms subgroup had higher ROSC and survival rates. Immediate recognition of symptoms and activation of the emergency medical system could prevent resuscitation delay and improve the survival rate.
- Citation: Zheng K, Bai Y, Zhai QR, Du LF, Ge HX, Wang GX, Ma QB. Correlation between the warning symptoms and prognosis of cardiac arrest. World J Clin Cases 2022; 10(22): 7738-7748
- URL: https://www.wjgnet.com/2307-8960/full/v10/i22/7738.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i22.7738
Sudden cardiac arrest (SCA) is commonly defined as an unexpected loss of pulse, which causes the patient to rapidly collapse. SCA has become a major issue in the field of emergency medicine over the past decades[1]. SCA patients may survive with timely cardiopulmonary resuscitation (CPR). Patients in the end-stage of cardiac arrest and those with pre-existing illnesses, such as terminal cancer, nonresponding pneumonia, end-stage cirrhosis, or massive cerebral hemorrhage, are generally untreatable, so cardiac arrest is predictable and death is inevitable[2]. However, if a patient is not in the end stage, regardless of the etiology and location of the cardiac arrest, high-quality basic life support and advanced cardiovascular life support could save the patient’s life[3].
Important progress has been made in resuscitation science over the last two decades. Smartphone applications can be used to activate the emergency response system[4,5]. There are more specific recommendations for high-quality chest compression, including an adequate compression rate and depth, full chest recoil, and the minimization of interruptions. Extracorporeal CPR may be considered for select cardiac arrest patients[6]. However, despite major progress in public-access defibrillation and resuscitation techniques, survival after SCA remains very low, at approximately 10% in developed countries and less than 1% in China and other developing countries[7,8]. The unpredictability of SCA is a primary problem that increases the difficulty of treatment and reduces the survival rate[7].
Over 60% of SCA events occur under in hospitalized patients under monitoring[7,9]. In a hospital, health care providers can arrive at the site within a few minutes, and the rapid response team can begin treatment immediately, which may contribute to the higher survival rate of in-hospital cardiac arrest (IHCA) patients[10]. In contrast, many SCA events occur outside the hospital and is known as out-of-hospital cardiac arrest (OHCA). In these situations, bystanders are usually not trained in CPR[11]. An immediately activated emergency response system is the first part of the “chain of survival” for OHCA patients, as emphasized by CPR guidelines in recent years[12]. However, most patients who experience cardiac arrest in public do not receive adequate treatment in China. The most common public response is “wait and see”, and treatment initiation by emergency medical services (EMS) can also be influenced by factors such as traffic jams and response time, that is, the time from answering the call to EMS arrival on site, which is largely determined by the availability of dispatching resources[8]. All the above can result in missing the ideal time to rescue a cardiac arrest patient. Thus, the rate of survival to discharge in OHCA patients in China has remained low for many years.
Regardless of OHCA or IHCA, clinicians need to develop methods to identify high-risk patients who suffer cardiac arrest. Warning symptoms are defined as signs that appear before SCA and have a causal relationship, including chest pain, dyspnea, palpitation, unconsciousness, and paralysis[13].
We hypothesized that different etiologies of SCA correlate with certain symptoms and that the immediate and correct recognition of symptoms and etiology can improve patient survival. We sought to investigate the characteristics of the warning symptoms of cardiac arrest, and to determine the correlation between cardiac arrest symptoms and patient prognosis.
Two medical centers participated in this study: Perking University Third Hospital and Beijing Friendship Hospital. Both are general hospitals, and the number of emergency visits exceeds 10000 per year in each of the two hospitals, which is the highest in Beijing.
We included all adult patients with all-cause cardiac arrest who visited Perking University Third Hospital or Beijing Friendship Hospital between January 2012 and December 2014. The exclusion criteria were as follows: Younger than 18 years old, showing obvious signs of irreversible disease (e.g., terminal cancer) and have a Do Not Resuscitate (DNR) declaration. Using the personal identification number provided to all emergency patients, electronic medical records in the hospital information systems were reviewed.
Data on patient characteristics, including pre-existing illnesses, warning symptoms within 24 h before SCA, call for EMS, the presence of a witness at the scene, time from cardiac arrest to contact with a health care provider, time from cardiac arrest to effective CPR (as defined by trained public rescuer or health care provider), initial rhythm, administration of defibrillation, restoration of spontaneous circulation (ROSC) (defined as a brief ROSC that provides evidence of more than an occasional gasp), and survival to discharge, were obtained. This study was approved by the Peking University Third Hospital Medical Science Research Ethics Committee.
Continuous variables are presented as the mean ± SD and were compared using a t-test. Categorical variables are presented as numbers (%) and were compared using the chi-square test or Fisher’s exact test as appropriate. A P value < 0.05 was considered statistically significant. All data were analysed using the statistical software package SPSS (IBM Corp. IBM SPSS Statistics for Windows, Version 25.0. Armonk, New York, United States).
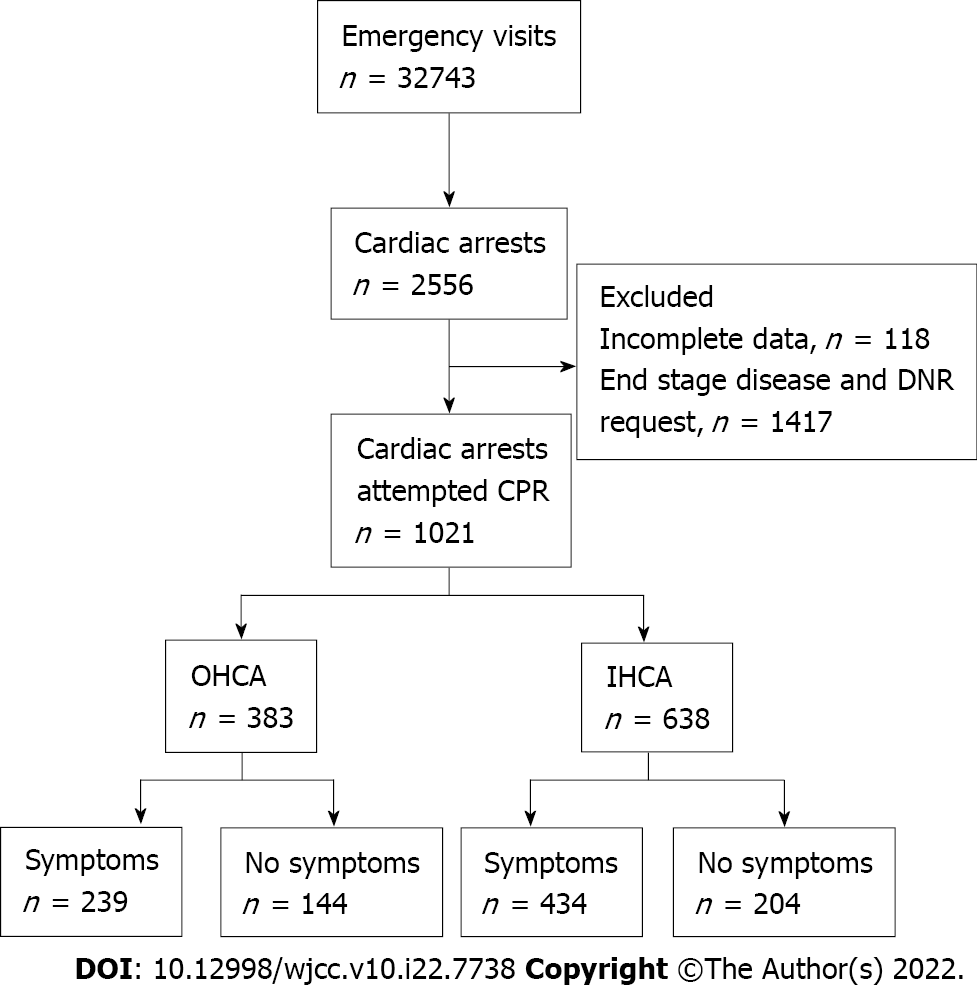
During the 36-mo study period, a total of 32743 patients visited the emergency departments. Of these patients, 2556 suffered cardiac arrest. One hundred eighteen patients were excluded because of incomplete information, and an additional 1417 were excluded for end-stage disease or DNR requests. A total of 1021 patients were ultimately included in this study. Among the included patients, 673 (65.9%) had warning symptoms, and 348 (34.1%) patients had no symptoms (Figure 1).
The included patients had a mean age of 64.1 ± 16.7 years; 68.4% were male, 37.8% had a cardiac etiology, 10.6% had an initial shockable rhythm, 25.2% achieved ROSC, and 7.0% survived to discharge. Of the 1021 patients, 770 (75.4%) had pre-existing illnesses. The top five pre-existing illnesses were hypertension (33.6%), coronary heart disease (23.3%), diabetes (20.0%), cerebral vascular disease (13.7%), and malignancy (8.8%). Other pre-existing illnesses included chronic kidney disease, chronic obstructive pulmonary disease, asthma, interstitial lung disease, valvular heart disease, cardiomyopathy, and cirrhosis.
The patients with symptoms had a higher mean age (65.2 ± 16.2 vs 61.8 ± 17.4 years, P = 0.002) and had higher rates of initial shockable rhythm (12.2% vs 7.5%, P = 0.020), ROSC (29.1% vs 17.5%, P = 0.001) and survival (9.2% vs. 2.6%, P = 0.001) than the patients without symptoms. Regarding other factors, such as sex, pre-existing illnesses, arrest location and etiology, there were no significant differences between the two groups (Table 1).
| All (n = 1021) | No symptoms (n = 348) | Symptoms (n = 673) | P value | |
| Age, mean ± SD | 64.1 ± 16.7 | 61.8 ± 17.4 | 65.2 ± 16.2 | 0.002a |
| Male, n (%) | 698 (68.4) | 238 (68.4) | 460 (68.4) | 0.990 |
| Pre-existing illness, n (%) | ||||
| Hypertension | 343 (33.6) | 120 (31.3) | 223 (33.1) | 0.666 |
| Coronary heart disease | 238 (23.3) | 72 (18.8) | 166 (24.7) | 0.154 |
| Diabetes | 204 (20.0) | 67 (17.4) | 137 (20.4) | 0.676 |
| Cerebral vascular disease | 140 (13.7) | 40 (10.4) | 100 (14.9) | 0.139 |
| Malignancy | 90 (8.8) | 27 (7.0) | 63 (9.4) | 0.392 |
| 1 pre-existing illness | 341 (33.4) | 105 (24.7) | 236 (35.1) | 0.116 |
| 2 pre-existing illnesses | 209 (20.5) | 74 (19.3) | 135 (20.1) | 0.651 |
| ≥ 3 pre-existing illnesses | 83 (8.1) | 24 (6.3) | 59 (8.8) | 0.300 |
| Location of SCA, n (%) | 0.066 | |||
| Out of hospital | 383 (37.5) | 144 (41.4) | 239 (35.5) | |
| In hospital | 638 (62.5) | 204 (58.6) | 434 (64.5) | |
| Initial shockable rhythm, n (%) | 108 (10.6) | 26 (7.5) | 82 (12.2) | 0.020a |
| Cardiac etiology, n (%) | 386 (37.8) | 122 (35.1) | 264 (39.2) | 0.193 |
| ROSC, n (%) | 257 (25.2) | 61 (17.5) | 196 (29.1) | < 0.001a |
| Survival to discharge, n (%) | 71 (7.0) | 9 (2.6) | 62 (9.2) | < 0.001a |
Patients were divided into OHCA or IHCA groups according to the cardiac arrest location, and then each group was divided into subgroups according to the presence or absence of symptoms (Table 2). The OHCA with symptoms subgroup had higher proportions of calls before arrest (81.6% vs 0.0%, P < 0.001), health care provider-witnessed arrest (13.0% vs 1.4%, P = 0.001), bystander CPR administration (15.5% vs 4.9%, P = 0.002), no flow time for 1 to 4 min (11.7% vs 2.8%, P = 0.002), and ROSC (23.8% vs 13.2%, P = 0.011) than the OHCA without symptoms subgroup. In comparison to the IHCA without symptoms subgroup, the IHCA with symptoms group had a higher mean age (66.2 ± 15.2 vs 62.5 ± 16.3 years, P = 0.005) and higher proportions of ROSC (32.0% vs 20.6%, P = 0.003) and survival to discharge (10.6% vs 2.5%, P < 0.001); there were no significant differences in any resuscitation parameters.
| OHCA | IHCA | |||||
| No symptoms (n = 144) | Symptoms (n = 239) | P value | No symptoms (n = 204) | Symptoms (n = 434) | P value | |
| Age, (mean ± SD) | 60.8 ± 18.8 | 63.4 ± 17.7 | 0.174 | 62.5 ± 16.3 | 66.2 ± 15.2 | 0.005a |
| Male, n (%) | 106 (73.6) | 175 (73.2) | 0.933 | 132 (64.7) | 285 (65.7) | 0.812 |
| Call before arrest, n (%) | 0 (0.0) | 195 (81.6) | < 0.001a | — | — | — |
| Witness of cardiac arrest, n (%) | < 0.001a | 0.299 | ||||
| None | 14 (9.7) | 22 (9.2) | 0.867 | 0 (0.0) | 0 (0.0) | |
| Family member | 128 (88.9) | 186 (77.8) | 0.006a | 10 (4.9) | 14 (3.2) | |
| Health care provider | 2 (1.4) | 31 (13.0) | < 0.001a | 194 (95.1) | 420 (96.8) | |
| Bystander CPR, n (%) | 7 (4.9) | 37 (15.5) | 0.002a | 194 (95.1) | 420 (96.8) | 0.299 |
| No flow time, n (%) | 0.002a | 0.189 | ||||
| 1 to 4 min | 4 (2.8) | 28 (11.7) | 0.002a | 204 (100.0) | 427 (98.4) | |
| 5 to 10 min | 4 (2.8) | 16 (6.7) | 0.095 | 0 (0.0) | 3 (0.7) | |
| > 10 min | 136 (94.4) | 195 (81.6) | < 0.001a | 0 (0.0) | 4 (0.9) | |
| Initial shockable rhythm, n (%) | 7 (4.9) | 19 (7.9) | 0.244 | 19 (9.3) | 63 (14.5) | 0.067 |
| Cardiac etiology, n (%) | 77 (53.5) | 140 (58.6) | 0.329 | 45 (22.1) | 124 (28.6) | 0.082 |
| ROSC, n (%) | 19 (13.2) | 57 (23.8) | 0.011a | 42 (20.6) | 139 (32.0) | 0.003a |
| Survival to discharge, n (%) | 49 (2.8) | 16 (6.7) | 0.095 | 5 (2.5) | 46 (10.6) | < 0.001a |
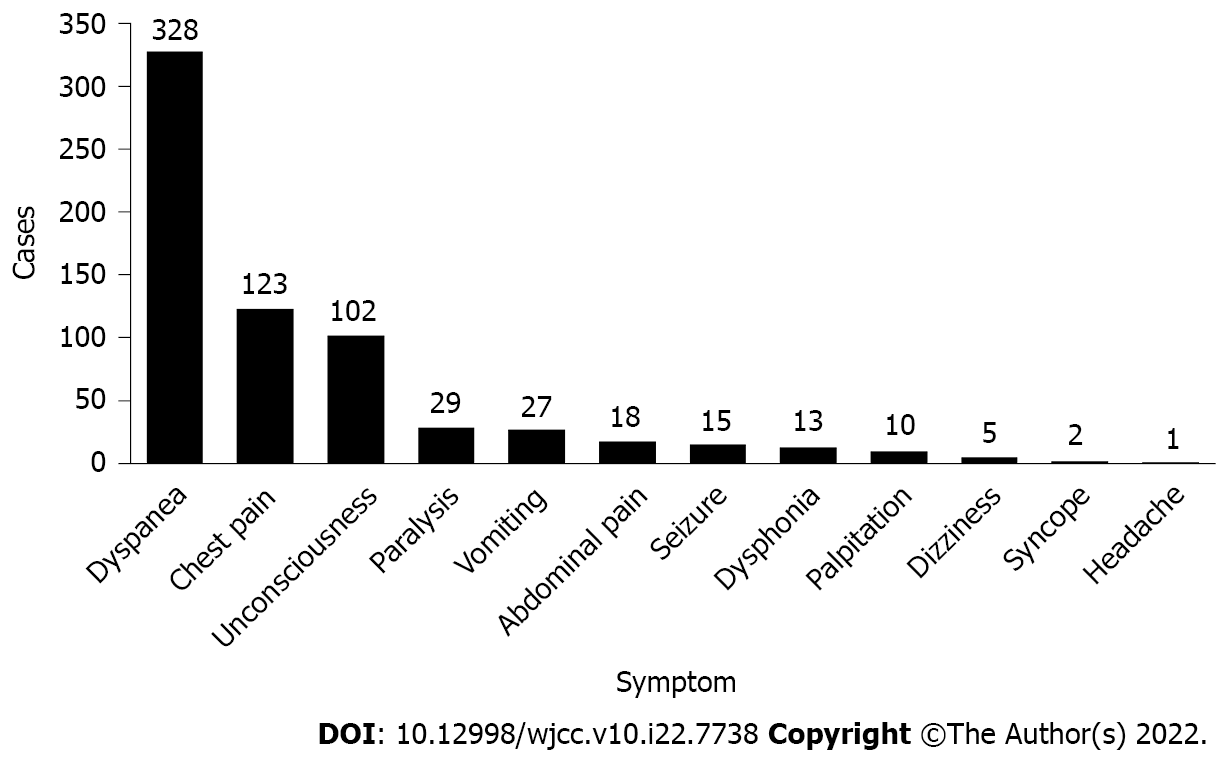
Six hundred seventy-three patients (65.9%) had warning symptoms before SCA. The top five symptoms were dyspnea (48.7%), chest pain (18.3%), unconsciousness (15.2%), paralysis (4.3%), and vomiting (4.0%). Other symptoms included abdominal pain, seizure, dysphonia, palpitation, dizziness, syncope, and headache (Figure 2).
Four hundred sixty male patients had warning symptoms. The top three symptoms were dyspnea (45.9%), chest pain (20.9%) and unconsciousness (14.6%). Two hundred thirteen female patients had warning symptoms. The top three symptoms were dyspnea (54.9%), unconsciousness (16.4%) and chest pain (12.7%). Chest pain was more common in males (20.9% vs 12.7%, P = 0.011), whereas dyspnea was more common in females (54.9% vs 45.9%, P = 0.029). There was no significant difference in the other symptoms between the two groups (Table 3).
| Symptom, n (%) | Sex | Age | Etiology | Outcome | ||||||||
| Male (n = 460) | Female (n = 213) | P value | < 60 yr (n = 225) | ≥ 60 yr (n = 448) | P value | Cardiac (n = 264) | Noncardiac (n = 409) | P value | Survival to discharge (n = 62) | Death to discharge (n = 611) | P value | |
| Dyspnea | 211 (45.9) | 117 (54.9) | 0.029a | 101 (44.9) | 227 (50.7) | 0.157 | 110 (41.7) | 218 (53.3) | 0.003a | 27 (43.5) | 301 (49.3) | 0.391 |
| Chest pain | 96 (20.9) | 27 (12.7) | 0.011a | 50 (22.2) | 73 (16.3) | 0.061 | 117 (44.3) | 6 (1.5) | < 0.001a | 21 (33.9) | 102 (16.7) | 0.001a |
| Unconsciousness | 67 (14.6) | 35 (16.4) | 0.530 | 38 (16.9) | 64 (14.3) | 0.374 | 19 (7.2) | 83 (20.3) | < 0.001a | 8 (12.9) | 94 (15.4) | 0.604 |
| Paralysis | 23 (5.0) | 6 (2.8) | 0.195 | 9 (4.0) | 20 (4.5) | 0.780 | 3 (1.1) | 26 (6.4) | 0.001a | 3 (4.8) | 26 (4.3) | 0.829 |
| Vomiting | 20 (4.3) | 7 (3.3) | 0.514 | 7 (3.1) | 20 (4.5) | 0.399 | 5 (1.9) | 22 (5.4) | 0.025a | 1 (1.6) | 26 (4.3) | 0.312 |
| Abdominal pain | 10 (2.2) | 8 (3.8) | 0.237 | 4 (1.8) | 14 (3.1) | 0.307 | 2 (0.8) | 16 (3.9) | 0.013a | 0 (0.0) | 18 (2.9) | 0.171 |
| Seizure | 13 (2.8) | 2 (0.9) | 0.123 | 6 (2.7) | 9 (2.0) | 0.586 | 3 (1.1) | 12 (2.9) | 0.123 | 2 (3.2) | 13 (2.1) | 0.577 |
| Dysphonia | 6 (1.3) | 7 (3.3) | 0.082 | 4 (1.8) | 9 (2.0) | 0.837 | 1 (0.4) | 12 (2.9) | 0.019a | 0 (0.0) | 13 (2.1) | 0.246 |
| Palpitation | 8 (1.7) | 2 (0.9) | 0.425 | 3 (1.3) | 7 (1.6) | 0.817 | 4 (1.5) | 6 (1.5) | 0.960 | 0 (0.0) | 10 (1.6) | 0.310 |
| Dizziness | 4 (0.9) | 1 (0.5) | 0.574 | 2 (0.9) | 3 (0.7) | 0.755 | 0 (0.0) | 5 (1.2) | 0.071 | 0 (0.0) | 5 (0.8) | 0.475 |
| Syncope | 1 (0.2) | 1 (0.5) | 0.576 | 0 (0.0) | 2 (0.4) | 0.316 | 0 (0.0) | 2 (0.5) | 0.255 | 0 (0.0) | 2 (0.3) | 0.652 |
| Headache | 1 (0.2) | 0 (0.0) | 0.496 | 1 (0.4) | 0 (0.0) | 0.158 | 0 (0.0) | 1 (0.2) | 0.421 | 0 (0.0) | 1 (0.2) | 0.750 |
Among the patients who were younger than 60 years old, 225 patients had warning symptoms. The top three symptoms were dyspnea (44.9%), chest pain (22.2%) and unconsciousness (16.9%). Among the patients who were aged 60 years and older, 448 patients had warning symptoms. The top three symptoms were dyspnea (50.7%), chest pain (16.3%) and unconsciousness (14.3%). No significant difference was observed in these age groups (Table 3).
Two hundred sixty-four patients with a cardiac etiology had warning symptoms. The top three symptoms were chest pain (44.3%), dyspnea (41.7%) and unconsciousness (7.2%). Four hundred nine patients with a noncardiac etiology had warning symptoms. The top three symptoms were dyspnea (53.3%), unconsciousness (20.3%) and paralysis (6.4%). Symptoms of dyspnea (53.3% vs 41.7%, P = 0.003), unconsciousness (20.3% vs 7.2%, P < 0.001), paralysis (6.4% vs 1.1%, P = 0.001), vomiting (5.4% vs 1.9%, P = 0.025), abdominal pain (3.9% vs 0.8%, P = 0.013) and dysphonia (2.9% vs 0.4%, P = 0.019) were more common in the noncardiac etiology group. In contrast, chest pain was more common in the cardiac etiology group (44.3% vs 1.5%, P < 0.001). There were no significant differences in other symptoms between the two groups (Table 3).
Sixty-two surviving patients had warning symptoms. The top three symptoms were (43.5%), chest pain (33.9%) and unconsciousness (12.9%). Among the 621 patients who did not survive, the top three symptoms were dyspnea (49.3%), chest pain (16.7%) and unconsciousness (15.4%). Chest pain was more common in the surviving patients (33.9% vs 16.7%, P = 0.001). There were no significant differences in the other symptoms between the two groups (Table 3).
Most patients had warning symptoms before SCA. Warning symptoms frequently occurred before SCA, and most symptoms recurred during the 24-hour period before SCA[13]. Unfortunately, more than two-thirds of patients and their families ignore the symptoms until cardiac arrest occurs[14]. In our study, it was remarkable that 65.9% of the patients had warning symptoms. Once warning symptoms appear, immediate activation of EMS could help patients receive treatment as early as possible. Emergency calls before patient collapse was associated with an increase in the proportions of EMS-witnessed cases and survival[4]. In our study, it was remarkable that the patients with symptoms had a better prognosis. The rate of bystander CPR in China is less than 20%. Most victims received appropriate treatment only when EMS personnel arrived at the scene[15]. In the large cities of China, the average time from the emergency call to EMS arrival was 10 minutes[8]. Due to the low rate of bystander CPR and lack of CPR knowledge, improving the public’s immediate recognition of cardiac arrest and activation of emergency response are the most important components of OHCA survival in China. In our study, we found that the OHCA patients with symptoms subgroup had higher proportions of emergency calls before arrest, health care provider-witnessed arrest and no flow time for 1 to 4 minutes. This means that if people could promptly recognize the warning symptoms of cardiac arrest and call EMS immediately, most patients could be treated as early as possible, which may improve the prognosis of cardiac arrest.
Pre-existing illnesses are generally associated with unfavorable outcomes[16]. However, the correlation between pre-existing illnesses and warning symptoms is not clear[13]. In our study, more than 50% of the patients had pre-existing illnesses, regardless of the presence of symptoms. Hypertension and coronary heart disease were the most common pre-existing illnesses. This discovery indicated that patients with cardiovascular illnesses had a high risk of cardiac arrest and thus should be the focus in hospitals. It should be noted that there was no relationship between pre-existing illnesses and warning symptoms, nor were there significant differences between patients with and without warning symptoms.
In our study, dyspnea, chest pain and unconsciousness were the top three warning symptoms, which accounted for 82.2% of symptoms, and dyspnea, at 48.7%, was the most common. Other studies also reported that these three symptoms were the most common complaints of all the patients who experienced cardiac arrest[13,17]. Therefore, health care providers should focus on patients with these symptoms, do their best to recognize critically ill patients in the triage area, and treat them in the appropriate medical units.
In males and females, dyspnea, chest pain, and unconsciousness were the top three most common warning symptoms, but the presence of a pre-existing illness may induce different clinical manifestations; for example, acute myocardial infarction usually presents as chest pain in males but not in females[18-20]. Our results were typical in that chest pain was more common in male patients. Based on these results, more information about other clinical manifestations should be collected, including electrocardiogram findings and myocardial injury markers, to make a correct diagnosis, especially in female patients with suspected acute myocardial infarction but without typical ischemic chest pain.
Younger patients (younger than 60 years of age) and elderly patients (older than 60 years of age) are known to have different disease spectra[7,21,22]. In our study, there were no differences in the warning symptoms that presented in the younger patients compared to the elderly patients; however, because of more comorbidities and longer disease durations, elderly patients usually received more attention from health care providers when they visit emergency departments. In contrast, younger patients received less attention because of their health histories and lack of regular health check-ups. As this may result in misdiagnosis, which can have serious consequences, more attention should be given to younger SCA patients in emergency departments.
The etiology of cardiac arrest was categorized as cardiac or noncardiac. The most common cardiac etiologies were acute myocardial infarction and heart failure, both of which include chest pain and dyspnea[7,23,24]. In our study, chest pain and dyspnea were the most important warning symptoms in patients with a cardiogenic etiology, accounting for 86.0% of all symptoms. In contrast, noncardiac etiologies include several diseases that include a variety of clinical manifestations, such as dyspnea, unconsciousness, paralysis, vomiting, and abdominal pain[17,25]. During CPR, the health care provider should give special treatment for the specific etiology if it is known[22,26-28]. That is, analyzing a patient’s symptoms to make an initial diagnosis and initiating appropriate treatment measures may be helpful in improving the ROSC rate. It is worth noting, however, that dyspnea was common in SCA due to both cardiac and noncardiac etiologies (41.7% vs 53.3%), with a variety of mechanisms contributing to the dyspnea in different situations, such as shock or poisoning. Therefore, when managing patients with dyspnea as a warning symptom, additional clinical information should be collected for the differential diagnosis.
In this study, chest pain was the most common warning symptom of SCA with a cardiac etiology, and patients with chest pain had a higher rate of survival. Considering that acute myocardial infarction is the most common cardiac cause of cardiac arrest, which is the primary cause of malignant arrhythmia, including ventricular fibrillation and pulseless ventricular tachycardia, early defibrillation can terminate arrhythmia, and ROSC can be achieved[29-31]. Consequently, when treating cardiac arrest patients with chest pain, a warning symptom, evaluating their initial rhythm and administering defibrillation to restore rhythm as soon as possible during CPR is an important method of improving the survival rate.
In this study, most patients had warning symptoms before cardiac arrest. Dyspnea, chest pain and unconsciousness were the most common symptoms, and patterns of symptoms differed by etiology and sex. The characteristics of the warning symptoms may be helpful in identifying the etiology and allowing the initiation of targeted treatment during CPR. Early warning signs of cardiac arrest were similar in patients of different ages, and clinicians should focus on younger patients as well as elderly patients. Finally, because of the low rate of bystander CPR and their lack of CPR knowledge, immediate recognition of cardiac arrest and activation of EMS should prevent CPR delay and increase the survival rate of OHCA patients.
The characteristics of early warning symptoms need further research. Especially the point of time, frequency and severity of warning symptoms before cardiac arrest occur.
Most patients had warning symptoms before cardiac arrest. Dyspnea, chest pain, and unconsciousness were the most common symptoms. The characteristics of the warning symptoms may be helpful in identifying the etiology and allowing the initiation of targeted treatment during cardiopulmonary resuscitation.
A total of 65.9% of patients had symptoms before arrest. Dyspnea, chest pain, and unconsciousness were the most common symptoms. The patients with symptoms had a higher rate of initial shockable rhythm, restoration of spontaneous circulation (ROSC) and survival than patients without symptoms. The out-of-hospital cardiac arrest symptoms subgroup had a higher rate of bystander cardiopulmonary resuscitation, a shorter no flow time, and a higher ROSC rate. The in-hospital cardiac arrest symptoms subgroup had higher ROSC and survival rates.
This was a retrospective study. We included all adult patients with all-cause cardiac arrest who visited Peking University Third Hospital or Beijing Friendship Hospital between January 2012 and December 2014. Data on population, symptoms, resuscitation parameters, and outcomes were analysed and compared between cardiac arrest patients with warning symptoms and those without warning symptoms.
We sought to investigate the characteristics of the warning symptoms of cardiac arrest, and to determine the correlation between cardiac arrest symptoms and patient prognosis.
We found that different etiologies of sudden cardiac arrest correlate with certain symptoms and that the immediate and correct recognition of symptoms and etiology can improve patient survival.
In the future, we should carry out more research on the characteristics of symptoms, such as the point of time, frequency and severity of warning symptoms.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: El-Gendy HA, Egypt; Pop TL, Romania S-Editor: Fan JR L-Editor: A P-Editor: Fan JR
| 1. | Zimmerman DS, Tan HL. Epidemiology and risk factors of sudden cardiac arrest. Curr Opin Crit Care. 2021;27:613-616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 2. | Berg KM, Cheng A, Panchal AR, Topjian AA, Aziz K, Bhanji F, Bigham BL, Hirsch KG, Hoover AV, Kurz MC, Levy A, Lin Y, Magid DJ, Mahgoub M, Peberdy MA, Rodriguez AJ, Sasson C, Lavonas EJ; Adult Basic and Advanced Life Support, Pediatric Basic and Advanced Life Support, Neonatal Life Support, and Resuscitation Education Science Writing Groups. Part 7: Systems of Care: 2020 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2020;142:S580-S604. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 113] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 3. | Abella BS. High-quality cardiopulmonary resuscitation: current and future directions. Curr Opin Crit Care. 2016;22:218-224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 31] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Scquizzato T, Pallanch O, Belletti A, Frontera A, Cabrini L, Zangrillo A, Landoni G. Enhancing citizens response to out-of-hospital cardiac arrest: A systematic review of mobile-phone systems to alert citizens as first responders. Resuscitation. 2020;152:16-25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 93] [Cited by in RCA: 78] [Article Influence: 15.6] [Reference Citation Analysis (0)] |
| 5. | Andelius L, Malta Hansen C, Lippert FK, Karlsson L, Torp-Pedersen C, Kjær Ersbøll A, Køber L, Collatz Christensen H, Blomberg SN, Gislason GH, Folke F. Smartphone Activation of Citizen Responders to Facilitate Defibrillation in Out-of-Hospital Cardiac Arrest. J Am Coll Cardiol. 2020;76:43-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 127] [Article Influence: 31.8] [Reference Citation Analysis (0)] |
| 6. | Twohig CJ, Singer B, Grier G, Finney SJ. A systematic literature review and meta-analysis of the effectiveness of extracorporeal-CPR vs conventional-CPR for adult patients in cardiac arrest. J Intensive Care Soc. 2019;20:347-357. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 56] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 7. | Virani SS, Alonso A, Aparicio HJ, Benjamin EJ, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Cheng S, Delling FN, Elkind MSV, Evenson KR, Ferguson JF, Gupta DK, Khan SS, Kissela BM, Knutson KL, Lee CD, Lewis TT, Liu J, Loop MS, Lutsey PL, Ma J, Mackey J, Martin SS, Matchar DB, Mussolino ME, Navaneethan SD, Perak AM, Roth GA, Samad Z, Satou GM, Schroeder EB, Shah SH, Shay CM, Stokes A, VanWagner LB, Wang NY, Tsao CW; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2021 Update: A Report From the American Heart Association. Circulation. 2021;143:e254-e743. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3854] [Cited by in RCA: 3588] [Article Influence: 897.0] [Reference Citation Analysis (0)] |
| 8. | Shao F, Li H, Ma S, Li D, Li C. Outcomes of out-of-hospital cardiac arrest in Beijing: a 5-year cross-sectional study. BMJ Open. 2021;11:e041917. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 9. | Shao F, Li CS, Liang LR, Qin J, Ding N, Fu Y, Yang K, Zhang GQ, Zhao L, Zhao B, Zhu ZZ, Yang LP, Yu DM, Song ZJ, Yang QL. Incidence and outcome of adult in-hospital cardiac arrest in Beijing, China. Resuscitation. 2016;102:51-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 57] [Article Influence: 6.3] [Reference Citation Analysis (0)] |
| 10. | Andersen LW, Holmberg MJ, Berg KM, Donnino MW, Granfeldt A. In-Hospital Cardiac Arrest: A Review. JAMA. 2019;321:1200-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 361] [Cited by in RCA: 575] [Article Influence: 95.8] [Reference Citation Analysis (0)] |
| 11. | Matsuyama T, Scapigliati A, Pellis T, Greif R, Iwami T. Willingness to perform bystander cardiopulmonary resuscitation: A scoping review. Resusc Plus. 2020;4:100043. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 29] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 12. | Ong MEH, Perkins GD, Cariou A. Out-of-hospital cardiac arrest: prehospital management. Lancet. 2018;391:980-988. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 162] [Article Influence: 23.1] [Reference Citation Analysis (0)] |
| 13. | Marijon E, Uy-Evanado A, Dumas F, Karam N, Reinier K, Teodorescu C, Narayanan K, Gunson K, Jui J, Jouven X, Chugh SS. Warning Symptoms Are Associated With Survival From Sudden Cardiac Arrest. Ann Intern Med. 2016;164:23-29. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 96] [Cited by in RCA: 121] [Article Influence: 13.4] [Reference Citation Analysis (0)] |
| 14. | Nehme Z, Bernard S, Andrew E, Cameron P, Bray JE, Smith K. Warning symptoms preceding out-of-hospital cardiac arrest: Do patient delays matter? Resuscitation. 2018;123:65-70. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 22] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 15. | Chen Y, Yue P, Wu Y, Li J, Lei Y, Gao D, Liu J, Han P. Trend in survival after out-of-hospital cardiac arrest and its relationship with bystander cardiopulmonary resuscitation: a six-year prospective observational study in Beijing. BMC Cardiovasc Disord. 2021;21:625. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 16. | Majewski D, Ball S, Finn J. Systematic review of the relationship between comorbidity and out-of-hospital cardiac arrest outcomes. BMJ Open. 2019;9:e031655. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 17. | Drezner JA, Fudge J, Harmon KG, Berger S, Campbell RM, Vetter VL. Warning symptoms and family history in children and young adults with sudden cardiac arrest. J Am Board Fam Med. 2012;25:408-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 54] [Cited by in RCA: 60] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 18. | Arora G, Bittner V. Chest pain characteristics and gender in the early diagnosis of acute myocardial infarction. Curr Cardiol Rep. 2015;17:5. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 19. | Brush JE Jr, Krumholz HM, Greene EJ, Dreyer RP. Sex Differences in Symptom Phenotypes Among Patients With Acute Myocardial Infarction. Circ Cardiovasc Qual Outcomes. 2020;13:e005948. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 38] [Article Influence: 7.6] [Reference Citation Analysis (0)] |
| 20. | Kirchberger I, Heier M, Kuch B, Wende R, Meisinger C. Sex differences in patient-reported symptoms associated with myocardial infarction (from the population-based MONICA/KORA Myocardial Infarction Registry). Am J Cardiol. 2011;107:1585-1589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 47] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 21. | DeFroda SF, McDonald C, Myers C, Cruz AI, Owens BD, Daniels AH. Sudden Cardiac Death in the Adolescent Athlete: History, Diagnosis, and Prevention. Am J Med. 2019;132:1374-1380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Myat A, Song KJ, Rea T. Out-of-hospital cardiac arrest: current concepts. Lancet. 2018;391:970-979. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 351] [Article Influence: 50.1] [Reference Citation Analysis (0)] |
| 23. | Houmsse M, Franco V, Abraham WT. Epidemiology of sudden cardiac death in patients with heart failure. Heart Fail Clin. 2011;7:147-155, vii. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 24. | Arabi AR, Patel A, Al Suwaidi J, Gehani AA, Singh R, Albinali HA. Clinical Profile, Management, and Outcome in Patients With Out-of-Hospital Cardiac Arrest and ST Segment Elevation Myocardial Infarction: Insights From a 20-Year Registry. Angiology. 2018;69:249-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 6] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 25. | Lundelin K, Graciani A, García-Puig J, Guallar-Castillón P, Taboada JM, Rodríguez-Artalejo F, Banegas JR. Knowledge of stroke warning symptoms and intended action in response to stroke in Spain: a nationwide population-based study. Cerebrovasc Dis. 2012;34:161-168. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 41] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 26. | Yousefifard M, Vazirizadeh-Mahabadi MH, Neishaboori AM, Alavi SNR, Amiri M, Baratloo A, Saberian P. Intranasal vs Intramuscular/Intravenous Naloxone for Pre-hospital Opioid Overdose: A Systematic Review and Meta-analysis. Adv J Emerg Med. 2020;4:e27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 27. | Javaudin F, Lascarrou JB, Le Bastard Q, Bourry Q, Latour C, De Carvalho H, Le Conte P, Escutnaire J, Hubert H, Montassier E, Leclère B; Research Group of the French National Out-of-Hospital Cardiac Arrest Registry (GR-RéAC). Thrombolysis During Resuscitation for Out-of-Hospital Cardiac Arrest Caused by Pulmonary Embolism Increases 30-Day Survival: Findings From the French National Cardiac Arrest Registry. Chest. 2019;156:1167-1175. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 56] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 28. | Paal P, Gordon L, Strapazzon G, Brodmann Maeder M, Putzer G, Walpoth B, Wanscher M, Brown D, Holzer M, Broessner G, Brugger H. Accidental hypothermia-an update : The content of this review is endorsed by the International Commission for Mountain Emergency Medicine (ICAR MEDCOM). Scand J Trauma Resusc Emerg Med. 2016;24:111. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 195] [Cited by in RCA: 182] [Article Influence: 20.2] [Reference Citation Analysis (0)] |
| 29. | Andersen LW, Kurth T, Chase M, Berg KM, Cocchi MN, Callaway C, Donnino MW; American Heart Association’s Get With The Guidelines-Resuscitation Investigators. Early administration of epinephrine (adrenaline) in patients with cardiac arrest with initial shockable rhythm in hospital: propensity score matched analysis. BMJ. 2016;353:i1577. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 75] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 30. | Kudenchuk PJ, Brown SP, Daya M, Rea T, Nichol G, Morrison LJ, Leroux B, Vaillancourt C, Wittwer L, Callaway CW, Christenson J, Egan D, Ornato JP, Weisfeldt ML, Stiell IG, Idris AH, Aufderheide TP, Dunford JV, Colella MR, Vilke GM, Brienza AM, Desvigne-Nickens P, Gray PC, Gray R, Seals N, Straight R, Dorian P; Resuscitation Outcomes Consortium Investigators. Amiodarone, Lidocaine, or Placebo in Out-of-Hospital Cardiac Arrest. N Engl J Med. 2016;374:1711-1722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 267] [Cited by in RCA: 327] [Article Influence: 36.3] [Reference Citation Analysis (0)] |
| 31. | Bircher NG, Chan PS, Xu Y; American Heart Association’s Get With The Guidelines–Resuscitation Investigators. Delays in Cardiopulmonary Resuscitation, Defibrillation, and Epinephrine Administration All Decrease Survival in In-hospital Cardiac Arrest. Anesthesiology. 2019;130:414-422. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 95] [Article Influence: 19.0] [Reference Citation Analysis (0)] |