Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.7006
Peer-review started: November 18, 2021
First decision: April 7, 2022
Revised: April 14, 2022
Accepted: May 22, 2022
Article in press: May 22, 2022
Published online: July 16, 2022
Processing time: 228 Days and 10.8 Hours
Atrial fibrillation (AF) is one of the most common arrhythmias, and radiofrequency catheter ablation is the most effective treatment strategy. The inferior vena cava (IVC) is a common approach for radiofrequency ablation of AF. However, this approach may not be applied to some cases such as chronic venous occlusions, surgical ligation of the IVC, and heterotaxy syndrome (HS).
A 68-year-old man with HS suffered from severely symptomatic persistent AF for 9 years, and we successfully ablated by percutaneous transhepatic access.
In patients without femoral vein access, the use of the hepatic vein for pulmonary vein isolation is a viable alternative for invasive electrophysiology procedures.
Core Tip: The inferior vena cava (IVC) is a commonly used method for radiofrequency ablation of atrial fibrillation. In some situations, this method cannot be used such as chronic venous occlusions, surgical ligation of the IVC, and heterotaxy syndrome. In patients without femoral vein access, hepatic vein approach for pulmonary vein isolation is a viable option for invasive electrophysiology procedures.
- Citation: Wang HX, Li N, An J, Han XB. Percutaneous transhepatic access for catheter ablation of a patient with heterotaxy syndrome complicated with atrial fibrillation: A case report. World J Clin Cases 2022; 10(20): 7006-7012
- URL: https://www.wjgnet.com/2307-8960/full/v10/i20/7006.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i20.7006
The inferior vena cava (IVC) is usually used for left-heart related operations, with a catheter entering through the right or left femoral vein and following the inferior vena cava into the atrial septum. Atrial septal puncture facilitates access to the left atrium for catheter ablation or other interventional operations[1,2]. However, conditions such as chronic venous occlusions, surgical ligation of the IVC, and venous malformations seen in heterotaxy syndrome (HS) limit femoral venous access for interventional operations[3,4]. In the absence of the IVC, we need another access to the left atrium. Superior approaches through the right internal jugular vein or the right subclavian vein have been documented in the literature, using a rigid angulated sheath or a steerable sheath to enter the left atrium via the superior vena cava (SVC) into the atrial septum. A retrograde aortic approach can also be used to perform pulmonary vein isolation (PVI) using a remote magnetic catheter navigation system[2,3]. In the above case, the operation is not ideal due to lack of support mainly from the lower edge of the fossa ovalis[5]. In addition, the hepatic vein provides a shorter, more direct access to bypass the IVC than the superior and femoral vein or retrograde aortic access. Hepatic vein approaches generally offer greater catheter stability and more familiar operations compared with the superior approach. In various clinical manipulation, hepatic vein cannulation has been applied to obtain long-term access including hemodialysis and chemotherapy[6,7], and the complication rate of this method has only been reported in 5% of the pediatric population. Percutaneous transhepatic access has been reported in rare cases of late years as it is a feasible approach for left-sided ablations[8].
HS is a rare congenital disease, which is closely associated with atrial fibrillation (AF), with an incidence of 23%[4]. A common feature of this syndrome is interruption of the IVC with azygos continuation into the SVC[4].
Herein, we describe a case of PVI in patients with HS necessitating hepatic vein access for ablation.
A 68-year-old man was suffered from severely symptomatic persistent AF for 9 years.
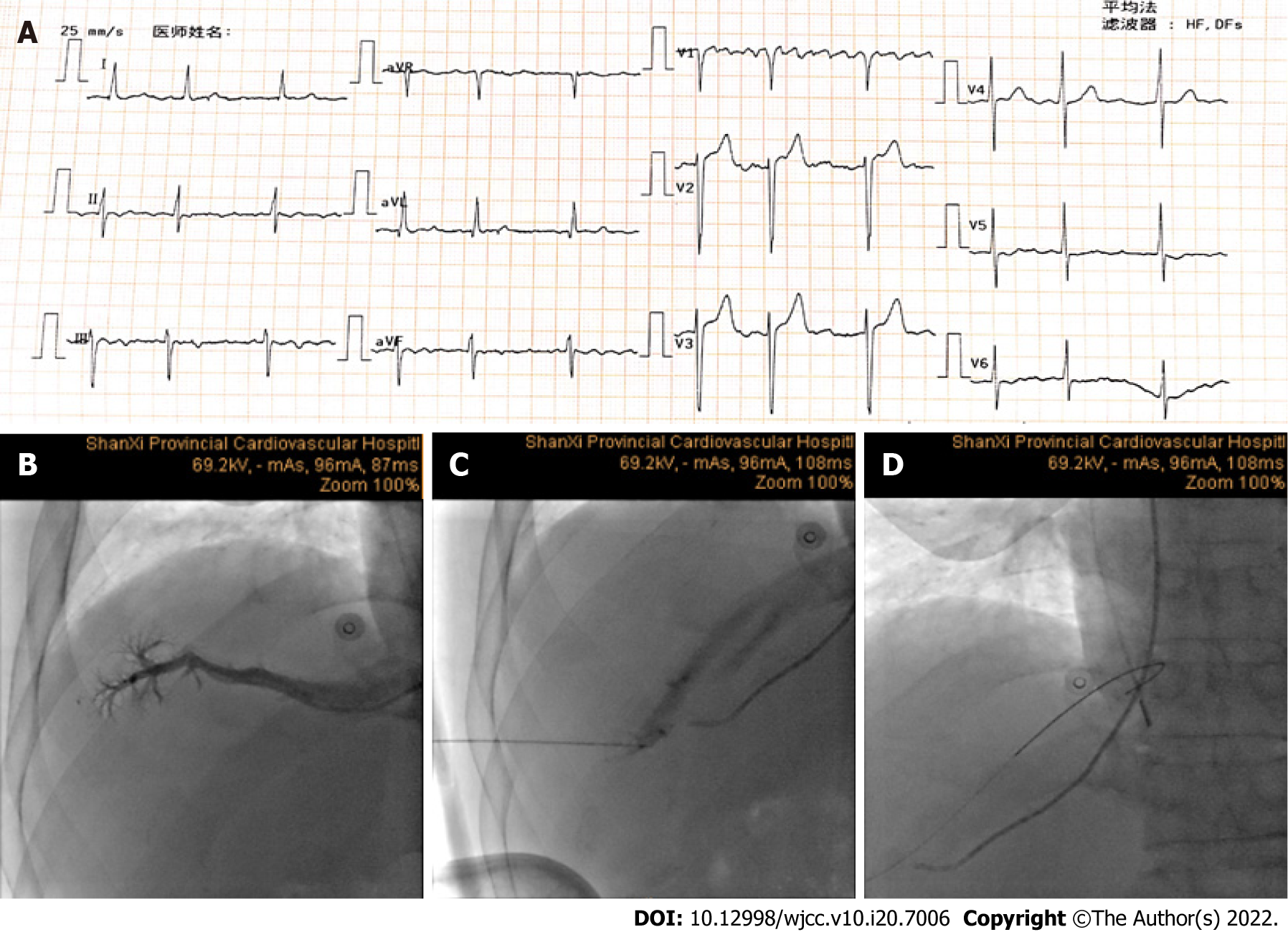
The patient reported a 9-year history of persistent AF (Figure 1A).
The patient had a history of ventricular septal defect occlusion and he suffered from HS, which was proved by computed tomography scan of the vena cava that showed that the IVC was interrupted. The azygos extended to the SVC and the hepatic veins drained directly to the right atrium.
The patient had no personal and family history.
Physical examination did not reveal any abnormalities.
Laboratory examination did not reveal any abnormalities.
Initial workup included an echocardiogram that showed an atrial septal defect (6 mm), with enlarged left atrial size and normal ejection fraction reported. Pulmonary vein mapping computed tomography also did not suggest any significant abnormalities.
Persistent atrial fibrillation.
Cardiac electrophysiological examination and radiofrequency ablation were performed using a Carto mapping system under general anesthesia and endotracheal intubation. Right internal jugular access and left subclavian vein access were obtained, with the placement of a 7F sheath (DECANAV; Biosense Webster, CA, United States) using a modified Seldinger technique for the subsequent placement of intracardiac echocardiography (ICE) catheter (CARTOSOUND, Biosense Webster, CA, United States) and a decapolar coronary sinus (CS) catheter. The JR4.0 catheter was inserted into the hepatic vein via the SVC and then a contrast agent was injected to determine the main direction of the hepatic vein (Figure 1B). With ultrasound and fluoroscopic assistance, an 18-gauge Chiba needle (Cook Medical, Bloomington, IN, United States) was steered into the middle hepatic vein, with positioning confirmed with contrast injection. A 0.035-inch Bentson wire (Cook Medical) was placed through the needle into the right atrium, and then an 8.5F SL1 long sheath (St. Jude Medical, St. Paul, MN, United States) was placed in the right atrium (Figure 1B-D). The ICE catheter (CARTOSOUND) was manipulated for visualization of the interatrial septum for a transseptal puncture (Figure 2A and B), and we constructed model of cardiac anatomy (Figure 2C). PVI was performed following single transseptal access using a SmartTouch surround flow catheter (Biosense Webster, Diamond Bar, CA, United States), with adequate anticoagulation on intravenous heparin (activated clotting time goal of 350 s). PVI was conducted in a standard procedure with one access to the left atrium (Figure 3A and B). AF was converted to sinus rhythm with electrical conversion energy of 200 watt-sec (Figure 3C). Rely on switching the ablation catheter to the PentaRay catheter (Biosense Webster), the bi-directional block was identified in the last stage of the process. The pericardium was monitored using the ICE catheter (CARTOSOUND), and no pericardial effusion was observed during the whole process. The 8F sheath was replaced to the hepatic vein, with a gelatin sponge placed along the hepatic tract for hemostasis. The gelatin sponge was infiltrated by the contrast agent for development.
In the present case, hemodynamics was carefully followed. Postoperative abdominal ultrasound suggested a small amount of leakage under the liver capsule. Full anticoagulation with rivaroxaban was deferred until the subsequent morning. In this case, no long-lasting complications were observed, and no recurrence was reported at 6 mo following ablation.
Left atrial arrhythmias correlate with HS[9,10]. Because of arrhythmia in patients with other reasons for IVC obstruction, ablation is often complicated by concerns for venous access. Alternative methods to access the IVC are needed in this type of patient, such as in our case with HS and unavailability of superior access owing to existing mapping, pacing, and ICE catheters. Therefore, ablation of the left atrium via hepatic vein access is a viable alternative in these patients. The large caliber of the hepatic veins, which accommodate sheaths used in arrhythmia ablation, provides an appropriate alternative to the femoral veins. Moreover, these veins have a large network of distal tributaries for access, and therefore this access could allow not only left-sided ablation but also repeat ablation when necessary[6].
Although congenital anomalies or venous occlusion is rare, which may inhibit the use of typical approach via IVC to achieve the performance of pulmonary vein isolation. In these rare circumstances, the transhepatic approach provide a safety and efficacy access among patients with congenital anomalies. The application of a transhepatic approach for electrophysiological examinations and ablation in adults is rare in clinical practice. To date, only about 10 cases have been reported[11-15]. By contrast, the technique is widely used applied in cardiac procedures for pediatric patients, for various purposes including diagnostic and interventional cardiac catheterizations, pacemaker placement, and electrophysiological procedures[11,16,17]. The largest study on the use of this approach in adult patients, which comprised 6 patients, showed that the technique could be applied to the management of cardiac arrhythmias and venous abnormalities through percutaneous transhepatic access[12]. It effectively ablated tachycardias, including atrial tachycardia, atrial flutter, atrioventricular nodal tachycardia, and atrial fibrillation, without causing complications. Previously, the cryoballoon catheter has been used to perform PVI via the percutaneous trans-hepatic venous approach[14].
Of note, the technical distinctions between this and traditional access warrant close attention. Hepatic veins enter the right atrium from a more posterior direction, which makes the transseptal sheath and needle more anterior than expected. Therefore, ablation of the right pulmonary vein is a challenge due to its steeper curve and the need for adequate tissue contact.
The reported complication rates in the related operation of percutaneous transhepatic access are relatively low (about 5%), and major complications include bleeding, infection, thrombosis, and pneumothorax. Intraperitoneal bleeding is a possible major complication. However, in the present case, hemodynamics was carefully followed and this complication was not observed. Subcutaneous hematomas have also been reported, especially in patients on warfarin[17-19]. In our case, the patient was routinely given rivaroxaban 15 mg until 1 d before the operation. Postoperative abdominal ultrasound suggested a small amount of leakage under the liver capsule. Full anticoagulation with rivaroxaban was deferred until the subsequent morning. As with other complex technologies and operations, low complication rates are associated with center experience and high volume, and thus this operation should be applied at medical institutions with experienced interventionalists, who have performed percutaneous transhepatic access for a wide range of indications including cardiac operations.
While performing ablation with double transseptal approach is feasible in these types of procedures, it is often hardly any need for PVI, and a single transseptal approach is probably to reduce complications from this puncture process. The application of proper landmarks, transesophageal echocardiographic, and fluoroscopy is crucial in minimizing complications. In the present case, no long-lasting complications were observed, and no recurrence was reported at 6 mo following ablation, making this approach a feasible alternative for ablation in these patients.
In patients without femoral vein access, the use of the hepatic vein for PVI is a viable alternative for invasive electrophysiology procedures.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Tsoulfas G, Greece A-Editor: Zhu JQ, China S-Editor: Ma YJ L-Editor: Filipodia P-Editor: Ma YJ
| 1. | Haegeli LM, Calkins H. Catheter ablation of atrial fibrillation: an update. Eur Heart J. 2014;35:2454-2459. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 90] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 2. | Lim HE, Pak HN, Tse HF, Lau CP, Hwang C, Kim YH. Catheter ablation of atrial fibrillation via superior approach in patients with interruption of the inferior vena cava. Heart Rhythm. 2009;6:174-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 3. | Rajappan K, Sporton SC, Schilling RJ. Left atrial tachycardia and inferior vena cava thrombotic occlusion complicating atrial fibrillation ablation successfully treated from the right subclavian vein. Heart. 2007;93:28. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Miyazaki A, Sakaguchi H, Ohuchi H, Yamamoto T, Igarashi T, Negishi J, Toyota N, Kagisaki K, Yagihara T, Yamada O. The incidence and characteristics of supraventricular tachycardia in left atrial isomerism: a high incidence of atrial fibrillation in young patients. Int J Cardiol. 2013;166:375-380. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Kato H, Kubota S, Goto T, Inoue K, Oku N, Haba T, Yamamoto M. Transseptal puncture and catheter ablation via the superior vena cava approach for persistent atrial fibrillation in a patient with polysplenia syndrome and interruption of the inferior vena cava: contact force-guided pulmonary vein isolation. Europace. 2017;19:1227-1232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 11] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Stavropoulos SW, Pan JJ, Clark TW, Soulen MC, Shlansky-Goldberg RD, Itkin M, Trerotola SO. Percutaneous transhepatic venous access for hemodialysis. J Vasc Interv Radiol. 2003;14:1187-1190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 70] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | Robertson LJ, Jaques PF, Mauro MA, Azizkhan RG, Robards J. Percutaneous inferior vena cava placement of tunneled silastic catheters for prolonged vascular access in infants. J Pediatr Surg. 1990;25:596-598. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 47] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Koc Z, Oguzkurt L. Interruption or congenital stenosis of the inferior vena cava: prevalence, imaging, and clinical findings. Eur J Radiol. 2007;62:257-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 115] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 9. | Malek E, Do D,Lu G,Murphy D, Aboulhosn J. The relationship between atrial flutter and atrial fibrillation in adults with congenital heart disease. Cardiology. 2015;65:A507. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 10. | Walsh EP, Cecchin F. Arrhythmias in adult patients with congenital heart disease. Circulation. 2007;115:534-545. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 278] [Cited by in RCA: 259] [Article Influence: 14.4] [Reference Citation Analysis (0)] |
| 11. | Singh SM, Neuzil P, Skoka J, Kriz R, Popelova J, Love BA, Mittnacht AJ, Reddy VY. Percutaneous transhepatic venous access for catheter ablation procedures in patients with interruption of the inferior vena cava. Circ Arrhythm Electrophysiol. 2011;4:235-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 62] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Nguyen DT, Gupta R, Kay J, Fagan T, Lowery C, Collins KK, Sauer WH. Percutaneous transhepatic access for catheter ablation of cardiac arrhythmias. Europace. 2013;15:494-500. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 34] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 13. | Ekeruo IA, Sharma S, Cohen A, Hematpour K. Hepatic vein access for pulmonary vein isolation in patients without femoral vein access. HeartRhythm Case Rep. 2019;5:395-398. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 14. | Orme GJ, Mendenhall C, Blair F, Wen Chen SY, Rhee E, Su W. Percutaneous transhepatic approach for cryoballoon pulmonary vein isolation in a patient with persistent atrial fibrillation and interruption of the inferior vena cava. HeartRhythm Case Rep. 2018;4:332-335. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 15. | Suryanarayana PG, Ayers M, Trerotola SO, Nazarian S. Direct hepatic vein puncture and transseptal access for atrial flutter and fibrillation ablation in a patient with prior ligation of the inferior vena cava. HeartRhythm Case Rep. 2020;6:382-385. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 16. | Shim D, Lloyd TR, Beekman RH 3rd. Transhepatic therapeutic cardiac catheterization: a new option for the pediatric interventionalist. Catheter Cardiovasc Interv. 1999;47:41-45. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Shim D, Lloyd TR, Cho KJ, Moorehead CP, Beekman RH 3rd. Transhepatic cardiac catheterization in children. Evaluation of efficacy and safety. Circulation. 1995;92:1526-1530. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 85] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 18. | Ebeid MR. Transhepatic vascular access for diagnostic and interventional procedures: techniques, outcome, and complications. Catheter Cardiovasc Interv. 2007;69:594-606. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 31] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Erenberg FG, Shim D, Beekman RH 3rd. Intraperitoneal hemorrhage associated with transhepatic cardiac catheterization: a report of two cases. Cathet Cardiovasc Diagn. 1998;43:177-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |