Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.6865
Peer-review started: January 23, 2022
First decision: March 24, 2022
Revised: April 6, 2022
Accepted: May 17, 2022
Article in press: May 17, 2022
Published online: July 16, 2022
Processing time: 162 Days and 14.4 Hours
Major adverse cardiac events (MACE) in elderly patients with biliary diseases are the main cause of perioperative accidental death, but no widely recognized quantitative monitoring index of perioperative cardiac function so far.
To investigate the critical values of monitoring indexes for perioperative MACE in elderly patients with biliary diseases.
The clinical data of 208 elderly patients with biliary diseases in our hospital from May 2016 to April 2021 were retrospectively analysed. According to whether MACE occurred during the perioperative period, they were divided into the MACE group and the non-MACE group.
In the MACE compared with the non-MACE group, postoperative complications, mortality, hospital stay, high sensitivity troponin-I (Hs-TnI), creatine kinase isoenzyme (CK-MB), myoglobin (MYO), B-type natriuretic peptide (BNP), and D-dimer (D-D) levels were significantly increased (P < 0.05). Multivariate logistic regression showed that postoperative BNP and D-D were independent risk factors for perioperative MACE, and their cut-off values in the receiver operating characteristic (ROC) curve were 382.65 pg/mL and 0.965 mg/L, respectively.
The postoperative BNP and D-D were independent risk factors for perioperative MACE, with the critical values of 382.65 pg/mL and 0.965 mg/L respectively. Consequently, timely monitoring and effective maintenance of perioperative cardiac function stability are of great clinical significance to further improve the perioperative safety of elderly patients with biliary diseases.
Core Tip: This study focused on high-risk elderly patients with biliary diseases, and determined the monitoring indexes of perioperative major adverse cardiac events (MACE) by a logistic multivariate prediction model. It was found that postoperative BNP and D-dimer (D-D) were independent risk factors for perioperative MACE, with the critical values of 382.65 pg/mL and 0.965 mg/L, respectively. Therefore, timely monitoring, effective prevention and treatment measures are of great clinical significance to maintain the stability of perioperative cardiac function, and further improve the perioperative safety of elderly patients with biliary diseases.
- Citation: Zhang ZM, Xie XY, Zhao Y, Zhang C, Liu Z, Liu LM, Zhu MW, Wan BJ, Deng H, Tian K, Guo ZT, Zhao XZ. Critical values of monitoring indexes for perioperative major adverse cardiac events in elderly patients with biliary diseases. World J Clin Cases 2022; 10(20): 6865-6875
- URL: https://www.wjgnet.com/2307-8960/full/v10/i20/6865.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i20.6865
Biliary diseases are common in elderly patients[1], with the clinical characteristics of poor surgical tolerance, high surgical risk, more postoperative complications and high mortality[2,3]. Studies have suggested that major adverse cardiac events (MACE) in elderly patients with biliary diseases are the main cause of perioperative accidental death[4,5]. Therefore, timely monitoring and effective maintenance of perioperative cardiac function stability are of great significance in order to avoid the occurrence and development of MACE.
At present, the commonly used method for the clinical assessment of cardiac function is the New York Heart Association cardiac functional classification[6,7], which mainly divides cardiac function into four grades according to the patient's symptoms and activity ability. However, it is greatly affected by subjective factors such as doctors' personal judgment and patients' self-conscious symptoms, and there are some defects in its objectivity, accuracy and sensitivity.
MACE is different from heart failure caused by perioperative acute myocardial infarction with accidental, symptomatic and physical signs, cardiac dysfunction caused by perioperative myocardial injury has common, asymptomatic and physical signs. Perioperative myocardial injury is characterized by a lack of symptoms related to myocardial ischemia, can only be detected by troponin level, is closely associated with mortality, there are no safe and effective preventive measures and other characteristics[8], and has received more attention in recent years[9].
With the development of high-sensitivity troponin (Hs-TnI) for early diagnosis of perioperative acute myocardial infarction, etiological identification of perioperative myocardial injury and other related research[10], more biomarkers have been identified for use in cardiac risk assessment[11,12], but there is no widely recognized quantitative monitoring index of perioperative cardiac function[13,14].
The purpose of this study was to explore the critical values of the quantitative monitored indexes of perioperative cardiac and coagulation functions, so as to take effective prevention and treatment measures in time to maintain the stability of cardiac function to further improve the perioperative safety of elderly patients with biliary diseases.
A retrospective case–control study of elderly patients with biliary diseases treated in the Department of General Surgery, Beijing Electric Power Hospital, State Grid Corporation of China, Capital Medical University was carried out between May 2016 and April 2021. According to whether MACE occurred during the perioperative period, the patients were divided into the MACE group and the non-MACE group.
MACE diagnostic criteria were as follows[15]: Acute myocardial infarction (AMI), heart failure or pulmonary edema, ventricular fibrillation, cardiac arrest, and complete heart block, which occurred from the beginning of anesthesia induction to 30 days after surgery.
Inclusion criteria: (1) Age ≥ 60 years; (2) Definite diagnosis of biliary disease; (3) No uncontrollable cardiac and pulmonary insufficiency; (4) Complete preoperative and postoperative data on cardiac and coagulation functions; and (5) Patients and their families signed the informed consent for surgery.
Exclusion criteria: (1) Age < 60 years; (2) Incomplete preoperative and postoperative data on cardiac and coagulation functions; and (3) American Society of anesthesiologists grade IV and above.
The study was approved by the Ethics Committee of Beijing Electric Power Hospital, State Grid Corporation of China, Capital Medical University, with the approval number of KY-2018-101-01-X.
The indexes monitored were as follows: (1) Clinical data: age, gender, disease type, surgical method, intraoperative blood loss, operation time, postoperative hospital stay, postoperative complications, treatment effect; (2) Postoperative cardiac functions: high sensitivity troponin-I (Hs-TnI), creatine kinase isoenzyme (CK-MB), myoglobin (MYO), B-type natriuretic peptide (BNP), left ventricular ejection fraction (LVEF); and (3) Postoperative coagulation functions: Activated partial thromboplastin time (APTT), prothrombin time (PT), fibrinogen (FIB), and D-D.
The patients underwent regular collection of venous blood during the three preoperative days and on the first postoperative day, the concentrations of Hs-TnI, CK-MB, MYO and BNP were detected by the Abbott i2000 Automated Chemiluminescence Analyzer, the concentrations of APTT, PT, FIB and D-D were detected by the ACL-TOP700 Automatic Coagulation Analyzer of the American Wolfen Instrumentation Laboratory.
LVEF was detected by a Philips EPIQ7 Color Doppler Ultrasound during the three preoperative days.
SPSS version 21.0 was used for statistical analysis. If normal distribution was satisfied, the Student’s t-test was used for comparison between two independent samples. When the variance was uneven, the corrected t-test was used. If the data were not normally distributed, they were expressed by the median and quartile spacing (P25–P75) and compared by the Mann–Whitney U rank sum test. Continuity correction or Fisher’s exact probability test was used for results that did not satisfy the conditions. Logistic regression was used to analyze the independent risk factors of perioperative MACE, the cut-off value of the ROC curve was calculated, and the logistic multivariate prediction model was established.
From May 2016 to April 2021, 851 patients with biliary diseases were surgically treated, including 438 elderly patients, and 208 met the inclusion criteria.
In the MACE (9 cases) compared with the non-MACE (199 cases) group, postoperative hospital stay, postoperative complications and mortality were significantly increased (P < 0.05). There were no significant differences in age, gender, disease type, surgical method, intraoperative blood loss, and operation time between the two groups (P > 0.05), as shown in Table 1.
| MACE (n = 9) | Non-MACE (n = 199) | t/Z/χ2 value | P/F value | |
| Age (yr) | 76.6 ± 8.6 | 72.1 ± 8.5 | 1.559 | 0.121 |
| Gender | 0.738 | |||
| Men | 5 | 93 | ||
| Women | 4 | 106 | ||
| Disease type | 1.000 | |||
| A | 7 | 145 | ||
| B | 8 | 174 | ||
| C | 0 | 15 | ||
| Operation method | 0.585 | |||
| Laparoscopy | 8 | 181 | ||
| Laparotomy | 1 | 18 | ||
| Intraoperative blood loss (mL) | 56.7 ± 60.2 | 41.5 ± 81.9 | 0.547 | 0.585 |
| Operation time (min) | 132.0 ± 78.3 | 94.5 ± 57.9 | 1.872 | 0.063 |
| Postoperative hospital stay (d) | 16.0 ± 9.8 | 9.4 ± 6.3 | 2.982 | 0.003 |
| Postoperative complicationsa | -2.828 | 0.005 | ||
| I | 0 | 26 | ||
| II | 1 | 15 | ||
| III | 1 | 3 | ||
| IV | 5 | 32 | ||
| V | 2 | 0 | ||
| Treatment effect | 0.002 | |||
| Cure | 7 | 199 | ||
| Death | 2 | 0 |
Among the 208 elderly patients with biliary diseases, MACE occurred in 9 cases (4.32%, 9/208) underwent laparoscopic cholecystectomy (LC) during the perioperative period, including 5 cases of AMI, 2 cases of congestive heart failure, and 2 cases of cardiac arrest. Among them, 7 cases were cured, one 71-year-old female patient with acute gangrenous cholecystitis died of AMI in the 14th LC postoperative day, another 64-year-old female case with acute calculous cholecystitis died of cardiac arrest for the type of electrocardio mechanical separation in the 12th LC postoperative day.
Two patients had a history of coronary heart disease in the MACE group, and 55 cases had a history of coronary heart disease in the non-MACE group, with no significant difference between the two groups (χ2 = 0, P = 1.000).
Five patients had a history of hypertension in the MACE group, and 112 cases had a history of hypertension in the non-MACE group, with no significant difference between the two groups (χ2 = 0, P = 1.000).
There were no significant differences in preoperative LVEF (t = -0.341, P = 0.734) between the MACE group (63.449 ± 3.865%) and the non-MACE group (63.000 ± 3.969%).
The Hs-TnI, CK-MB, MYO, D-D, and PT levels were significantly increased in the postoperative group compared with those in the preoperative group (P < 0.05), but no significant differences in the APTT and FIB levels were observed between the two groups (P > 0.05), as shown in Table 2.
| Item | Preoperative (n = 208) | Postoperative (n = 208) | Z | P value |
| HsTn-I (ng/mL) | 0.004 (0.002, 0.008) | 0.005 (0.003, 0.010) | -2.345 | 0.019 |
| CKMB (ng/mL) | 0.700 (0.500, 1.200) | 0.800 (0.500, 1.200) | -2.214 | 0.027 |
| MYO (ng/mL) | 46.700 (30.875, 72.400) | 67.850 (41.975, 114.55) | -5.591 | 0.000 |
| BNP (pg/mL) | 76.700 (44.950, 134.525) | 152.500 (94.450, 302.675) | -8.777 | 0.000 |
| D-D (mg/L) | 0.330 (0.160, 0.683) | 0.510 (0.260, 1.025) | -3.890 | 0.000 |
| APTT (sec) | 31.100 (28.950, 32.900) | 30.700 (28.400, 32.700) | -1.512 | 0.130 |
| PT (sec) | 11.900 (11.100, 13.000) | 12.300 (11.600, 13.425) | -3.083 | 0.002 |
| FIB (g/L) | 3.710 (3.060, 4.683) | 3.625 (2.955, 4.460) | -1.141 | 0.254 |
Postoperative Hs-TnI, CK-MB, MYO, BNP and D-D levels were significantly increased in the MACE group compared with those in the non-MACE group (P < 0.05), but no significant differences in postoperative APTT, PT, and FIB levels were observed between the two groups (P > 0.05), as shown in Table 3.
| Item | MACE group (n = 9) | Non-MACE group (n = 199) | Z value | P value |
| HsTn-I (ng/mL) | 0.034 (0.006, 0.112) | 0.005 (0.003, 0.009) | -3.078 | 0.002 |
| CKMB (ng/mL) | 2.200 (1.000, 2.500) | 0.800 (0.500, 1.150) | -2.896 | 0.004 |
| MYO (ng/mL) | 230.300 (60.200, 454.400) | 67.200 (41.700, 109.000) | -2.013 | 0.044 |
| BNP (pg/mL) | 617.400 (200.200, 931.300) | 148.900 (93.450, 289.200) | -2.851 | 0.004 |
| D-D (mg/L) | 2.150 (1.060, 2.520) | 0.480 (0.250, 0.970) | -3.941 | 0.000 |
| APTT (sec) | 34.500 (28.700, 35.800) | 30.650 (28.400, 32.475) | -1.384 | 0.166 |
| PT (sec) | 12.700 (12.000, 19.200) | 12.300 (11.600, 13.400) | -1.235 | 0.217 |
| FIB (g/L) | 3.310 (2.850, 3.960) | 3.630 (2.965, 4.460) | -0.634 | 0.526 |
The indicators with statistically significant differences in Table 3 were analyzed by multivariate logistic regression, which showed that postoperative BNP and D-D were independent risk factors for MACE during the perioperative period, the P values were 0.046 and 0.042, OR values were 1.003 and 2.338, and 95%CI were 1.000-1.005 and 1.033-5.290, respectively, as shown in Table 4.
| Item | SE | Wald | P value | OR | 95%CI | |
| BNP | 0.003 | 0.001 | 3.983 | 0.046 | 1.003 | 1.000-1.005 |
| Hs-TnI | 1.781 | 4.499 | 0.157 | 0.692 | 5.934 | 0.001-40088.202 |
| D-D | 0.849 | 0.417 | 4.154 | 0.042 | 2.338 | 1.033-5.290 |
| CKMB | 0.025 | 0.300 | 0.007 | 0.934 | 1.025 | 0.569-1.847 |
| MYO | 0.000 | 0.002 | 0.021 | 0.884 | 1.000 | 0.996-1.005 |
| Constant | -5.312 | 0.893 | 35.403 | 0.000 | 0.005 |
Based on multivariate logistic regression analysis, it was suggested that postoperative BNP and D-D levels were related to the occurrence of perioperative MACE in elderly patients with biliary diseases. The logistic multivariate prediction model established by the logistic regression equation was P = ex/(1+ex), X = -5.312 + 0.003X1 + 0.849X2, where X1 was the postoperative BNP level and X2 was the postoperative D-D level. Taking the predictive probability value of 0.5 as the junction point, > 0.5 indicated that patients would develop MACE after surgery, and < 0.5 indicated that patients would not develop MACE after surgery. The above data were included into the logistic multivariate prediction model, and the results showed that the accuracy, specificity and sensitivity for predicting perioperative MACE in elderly patients with biliary diseases were 96.6% (201/208), 100.0% (199/199) and 22.2% (2/9).
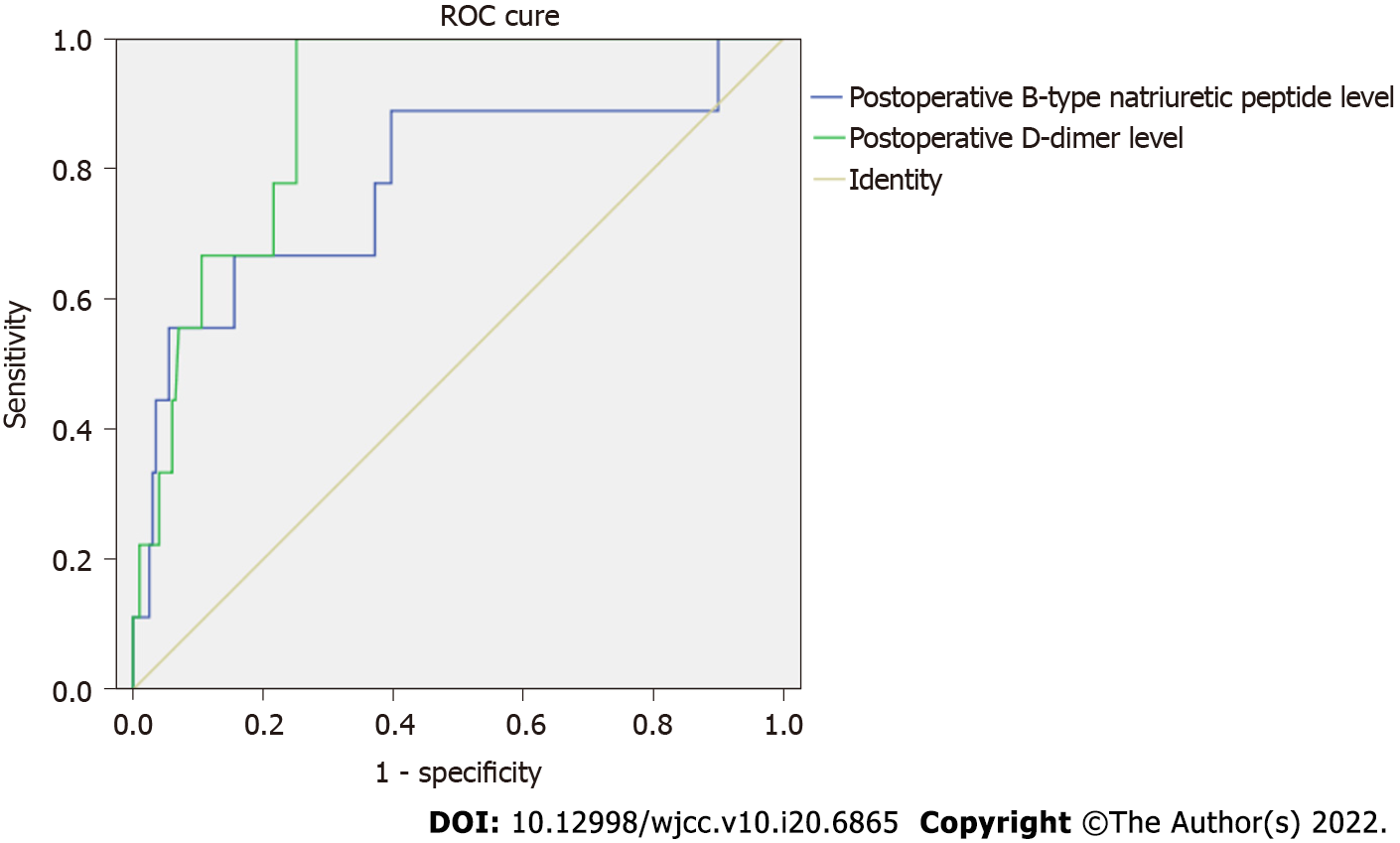
Based on the results of multivariate logistic regression, the ROC curve showed that the area under the curve of postoperative BNP and D-D levels for predicting perioperative MACE was 0.781 and 0.889, respectively, the cut-off values for BNP and D-D in the ROC curve were 382.65 pg/mL and 0.965 mg/L, 95%CI were 0.596-0.966 and 0.819-0.959, respectively, the sensitivity and specificity of BNP were 66.7% and 83.9%, respectively, and the sensitivity and specificity of D-D were 100% and 74.9%, respectively, as shown in Figure 1.
According to the latest information released by the National Bureau of Statistics of P. R. China, by the end of 2021, the elderly population aged 60 years and above reached 267.36 million, accounting for 18.9% of the total population, indicating that China has a rapidly aging society. With accelerated aging of the population, the number of elderly patients undergoing surgery is increasing. As elderly patients often have complications such as hypertension, coronary heart disease, diabetes and other diseases, the incidence of perioperative cardiovascular complications has increased significantly[16], especially in elderly patients over 70 years old[17].
Perioperative MACE refers to unstable angina pectoris, cardiac death, AMI, congestive heart failure, severe arrhythmia, non fatal cardiac arrest, etc. during and within 30 days after operation[18], which is the main cause of serious complications and even death in non-cardiac surgery patients during the perioperative period. Large scale research results have shown that the incidence of perioperative myocardial infarction in patients undergoing non-cardiac surgery is 0.3%-16%, accounting for 12%-40% of the mortality of hospitalized patients[9]. It has been reported that the perioperative risk factors in elderly patients undergoing non-cardiac surgery include coronary heart disease, coronary artery intervention and bypass surgery, heart valve disease, arrhythmia, preoperative LVEF < 50%, major surgery, long anesthesia time, increased preoperative high-sensitivity C-reactive protein and BNP, etc[16].
Perioperative acute myocardial infarction is an accidental cardiac event with symptoms and signs of myocardial ischemia and is life-threatening. It occurs within the first 3 d after non-cardiac surgery, and up to 1/3 of patients have ST-segment elevation myocardial infarction (STEMI), with a mortality rate as high as 30% within 30 d of surgery[19]. It was recently reported[20] that the incidence of perioperative acute myocardial infarction in non-cardiac surgery patients aged 45 years and above was approximately 0.02%, which increased significantly with age, and mostly occurred within 48 h after surgery.
Perioperative myocardial injury is a common myocardial injury, which lacks myocardial ischemia symptoms, can only be detected by troponin level, is closely related to mortality and there are no safe and effective preventive measures. It was reported in an international prospective cohort study, involving 15065 hospitalized patients aged 45 years and above undergoing non-cardiac surgery, with troponin T ≥ 0.03 ng/mL as the diagnostic criterion of perioperative myocardial injury, and without cardiac troponin elevation caused by non-cardiogenic diseases (such as sepsis, pneumonia, pulmonary embolism, renal failure, etc[21]), that the incidence of perioperative myocardial injury was as high as 8% and was associated with 30-d mortality[22].
As MACE is the main cause of perioperative death in elderly patients with biliary diseases, it is of great significance to actively carry out perioperative cardiac function evaluation to understand the condition, guide treatment, evaluate the curative effect and estimate prognosis[23].
A number of cardiac function evaluations have been carried out and constantly improved[7,24,25], such as the New York Heart Association functional classification, echocardiography, cardiac magnetic resonance imaging, cardiac computed tomography, biomarkers of myocardial injury, biomarkers of heart failure, gated single photon emission computed tomography myocardial perfusion imaging, and other examination methods, but so far there is no clear simple, objective and reliable quantitative index for perioperative cardiac function evaluation in elderly patients.
In this study, the monitoring indexes of cardiac function were used to evaluate myocardial ischemia and injury, with the principle of selection as follows: Hs-TnI, CK-MB and MYO as biomarkers of myocardial injury[26,27], BNP as a biomarker of heart failure, and LVEF as an index of left ventricular function. Hs-TnI is a myocardial enzyme, which is present in the cytoplasm of myocardial cells. When myocardial injury occurs, Hs-TnI can be released into the blood, with its concentration change reflecting the degree of myocardial injury, and is one of the best biomarkers for the diagnosis of myocardial injury[10]. Therefore, Hs-TnI is of great significance for the early diagnosis of AMI, and has become the "gold standard" for the diagnosis of myocardial damage, especially MI[28]. CK-MB is another myocardial enzyme, with a relatively high specificity for the diagnosis of myocardial injury and MI, and is helpful in predicting the size of MI, and its dynamic elevation can be used as one of the diagnostic indexes of AMI. MYO is also a myocardial enzyme, which can be used as a sensitive indicator in the early diagnosis of AMI, and is widely used in the early diagnosis and differential diagnosis of AMI. BNP is the earliest and most widely used heart failure biomarker synthesized and secreted by ventricular myocytes, which not only reflects left ventricular systolic dysfunction, but also reflects left ventricular diastolic dysfunction, valve dysfunction and right ventricular dysfunction[29]. BNP level is affected by ventricular load and increases with increasing load. LVEF, reflecting myocardial contractility, venous return blood volume (preload) and arterial blood pressure (afterload)[30], is used to evaluate left ventricular function[31,32].
The relationship between the imbalance of coagulation and the fibrinolysis system and ischemic heart disease has received increased attention. Experimental and clinical studies show that thrombosis is an important mechanism of acute coronary syndrome[33-35]. In this study, the single photon emission computed tomography monitored indexes of coagulation function were used to evaluate the occurrence of cardiovascular thrombosis, APTT reflects the endogenous coagulation system function, PT reflects the exogenous coagulation system function, and FIB reflects the content of fibrinogen. D-D is a fibrinolysis biomarker, and is one of the molecular biomarkers of the hypercoagulable state and hyperfibrinolysis in vivo, it can reflect both thrombin activity and fibrinolytic activity; therefore, is as an ideal index for evaluating coagulation function and the fibrinolysis system. Inflammation, trauma and stress can increase the concentration of D-D, and the concentration significantly increases with the severity of coronary heart disease, which is considered to be one of the risk factors for the occurrence and development of coronary heart disease.
Cardiac and coagulation functions on the first postoperative day were selected as the monitored indices of perioperative MACE in this study, this was because on the one hand, they were significantly higher than those during the three preoperative days (Table 2); on the other hand, they not only reflected the state of cardiac and coagulation functions before surgery, but also reflected the influence of intraoperative trauma and postoperative disease change on the first postoperative day. Following multivariate logistic regression analysis, we found that postoperative BNP and D-D were independent risk factors for perioperative MACE in elderly patients with biliary diseases. The cut-off values of BNP and D-D in the ROC the curve were 382.65 pg/mL and 0.965 mg/L, respectively, which could be used as critical values for monitoring perioperative MACE, and could also be of great significance in guiding clinical prevention and treatment of perioperative MACE.
Significant Hs-TnI increase: A report[10] showed that if Hs-TnI is more than 7.424 ng/mL, suggesting the occurrence of acute STEMI, the patient should be actively treated with thrombolysis (acute STEMI), anticoagulation, antiplatelet, lipid-lowering, and symptomatic treatment, and even percutaneous coronary intervention (PCI) when necessary[18].
Mild Hs-TnI increase: It is reported[10] that when Hs-TnI is greater than 0.372 ng/mL, indicating the possible AMI, the patient should be given isosorbide nitrate injection (Aibei, initial dose of the intravenous drip is 30 μg/min), to relax vascular smooth muscle, reduce cardiac preload and oxygen consumption. At the same time, clopidogrel bisulfate (75 mg, once daily) and other antiplatelet therapy can also be given. Anticoagulant drugs should be added when necessary.
Significant BNP increase: If BNP is more than 400 pg/mL, this suggests that the possibility of heart failure is very high. In this study, we found that the postoperative BNP critical value in elderly patients with biliary diseases was 382.65 pg/mL, which indicated the occurrence of heart failure, cardiotonic and diuretic agents should be given, and digitalis and other positive inotropic drugs should be administered when necessary (relatively forbidden within 72 h of AMF).
Mild BNP increase: According to the literature, 100-400 pg/mL of BNP suggests that there may be cardiac insufficiency, and the drug infusion volume and speed should be reduced, and the infusion speed could be strictly controlled using an infusion pump.
Significant D-D increase: A significant increase in D-D indicates an increased risk of thrombosis. In this study, we found that the postoperative D-D critical value in elderly patients with biliary disease was 0.965 mg/L, and patients should be given a subcutaneous injection of low molecular weight heparin calcium 0.4 mL or dalteparin sodium 2500 IU, once every 12 h, and oral aspirin enteric coated tablets (the first dose of 300 mg, then 100 mg daily) when necessary.
In general, perioperative monitoring of cardiac function in elderly patients is mainly realized through intraoperative and postoperative electrocardiography (ECG), blood pressure and central venous pressure (CVP) monitoring. For patients whose postoperative BNP is higher than the critical value of 382.65 pg/mL and D-D is higher than 0.965 mg/L, perioperative cardiac function and coagulation function should be dynamically monitored. When abnormalities are found, timely treatment should be carried out to ensure perioperative cardiac function.
Routine ECG monitoring, dynamic CVP and urine volume detection in the first 3 days after surgery should be carried out, and urine volume per hour should be recorded when necessary to guide the volume and speed of postoperative infusion and prevent heart failure caused by excessive and rapid infusion. When the signs of AMI are found, thrombolysis, anticoagulation, lipid-lowering and symptomatic treatment should be carried out immediately according to the above-mentioned principles, and PCI performed when necessary. In the case of heart failure, it should be treated with cardiotonic and diuretic agents, and infusion speed and infusion volume controlled according to the above mentioned principles.
This study focused on high-risk elderly patients with biliary diseases, and determined the monitoring indexes of perioperative MACE by a logistic multivariate prediction model. It was found that postoperative BNP and D-D were independent risk factors for perioperative MACE, with the critical values of 382.65 pg/mL and 0.965 mg/L, respectively. Therefore, timely monitoring, effective prevention and treatment measures are of great clinical significance to maintain the stability of perioperative cardiac function, and further improve the perioperative safety of elderly patients with biliary diseases.
Major adverse cardiac events (MACE) in elderly patients with biliary diseases are the main cause of perioperative accidental death, but no widely recognized quantitative monitoring index of perioperative cardiac function so far.
The purpose of this study was to explore the critical values of the quantitative monitored indexes of perioperative cardiac and coagulation functions, so as to take effective prevention and treatment measures in time to maintain the stability of cardiac function to further improve the perioperative safety of elderly patients with biliary diseases.
The clinical data of 208 elderly patients with biliary diseases in our hospital from May 2016 to April 2021 were retrospectively analysed.
According to whether MACE occurred during the perioperative period, they were divided into the MACE group and the non-MACE group. Multivariate logistic regression was used.
Multivariate logistic regression showed that postoperative B-type natriuretic peptide (BNP), and D-dimer (D-D) were independent risk factors for perioperative MACE, and their cut-off values in the receiver operating characteristic curve were 382.65 pg/mL and 0.965 mg/L, respectively.
The postoperative BNP and D-D were independent risk factors for perioperative MACE, with the critical values of 382.65 pg/mL and 0.965 mg/L respectively.
Consequently, timely monitoring and effective maintenance of perioperative cardiac function stability are of great clinical significance to further improve the perioperative safety of elderly patients with biliary diseases.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Muneer A, Malaysia; Tomizawa M, Japan S-Editor: Liu JH L-Editor: A P-Editor: Liu JH
| 1. | Zhang ZM, Dong JH, Lin FC, Wang QS, Xu Z, He XD, Zhang C, Liu Z, Liu LM, Deng H, Yu HW, Wan BJ, Zhu MW, Yang HY, Song MM, Zhao Y. Current Status of Surgical Treatment of Biliary Diseases in Elderly Patients in China. Chin Med J (Engl). 2018;131:1873-1876. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 2. | Zhang ZM, Zhang C, Liu Z, Liu LM, Zhu MW, Zhao Y, Wan BJ, Deng H, Yang HY, Liao JH, Zhu HY, Wen X, Liu LL, Wang M, Ma XT, Zhang MM, Liu JJ, Liu TT, Huang NN, Yuan PY, Gao YJ, Zhao J, Guo XA, Liao F, Li FY, Wang XT, Yuan RJ, Wu F. Therapeutic experience of an 89-year-old high-risk patient with incarcerated cholecystolithiasis: A case report and literature review. World J Clin Cases. 2020;8:4908-4916. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Zhang ZM, Liu Z, Liu LM, Zhang C, Yu HW, Wan BJ, Deng H, Zhu MW, Liu ZX, Wei WP, Song MM, Zhao Y. Therapeutic experience of 289 elderly patients with biliary diseases. World J Gastroenterol. 2017;23:2424-2434. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 12] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (3)] |
| 4. | Xu L, Yu C, Jiang J, Zheng H, Yao S, Pei L, Sun L, Xue F, Huang Y. Major adverse cardiac events in elderly patients with coronary artery disease undergoing noncardiac surgery: A multicenter prospective study in China. Arch Gerontol Geriatr. 2015;61:503-509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 34] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 5. | Zhang XD, Wang XH, Hu PJ, Du ZK. Application of N-terminal pro-brain natriuretic peptide concentration and the Global Registry of Acute Coronary Events risk score to predict major adverse cardiac events in patients with ST-elevation myocardial infarction after PCI. South China Journal of Cardiology. 22:171-176. [DOI] [Full Text] |
| 6. | Caraballo C, Desai NR, Mulder H, Alhanti B, Wilson FP, Fiuzat M, Felker GM, Piña IL, O'Connor CM, Lindenfeld J, Januzzi JL, Cohen LS, Ahmad T. Clinical Implications of the New York Heart Association Classification. J Am Heart Assoc. 2019;8:e014240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 189] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 7. | Heart Failure Group of Chinese Society of Cardiology of Chinese Medical Association; Chinese Heart Failure Association of Chinese Medical Doctor Association; Editorial Board of Chinese Journal of Cardiology. Chinese guidelines for the diagnosis and treatment of heart failure 2018. Zhonghua Xin Xue Guan Bing Za Zhi. 2018;46:760-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 99] [Reference Citation Analysis (0)] |
| 8. | Ruetzler K, Khanna AK, Sessler DI. Myocardial Injury After Noncardiac Surgery: Preoperative, Intraoperative, and Postoperative Aspects, Implications, and Directions. Anesth Analg. 2020;131:173-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 58] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 9. | Magoon R, Makhija N, Das D. Perioperative myocardial injury and infarction following non-cardiac surgery: A review of the eclipsed epidemic. Saudi J Anaesth. 2020;14:91-99. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Liang ZY, Guo J. Application value of high sensitivity troponin I in early diagnosis of acute myocardial infarction. [Article in Chinese]. Modern Medicine and Health Research, 201; 3: 83-85. |
| 11. | Yurttas T, Hidvegi R, Filipovic M. Biomarker-Based Preoperative Risk Stratification for Patients Undergoing Non-Cardiac Surgery. J Clin Med. 2020;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Gualandro DM, Twerenbold R, Boeddinghaus J, Nestelberger T, Puelacher C, Müller C. Biomarkers in cardiovascular medicine: towards precision medicine. Swiss Med Wkly. 2019;149:w20125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 13. | Lerman BJ, Popat RA, Assimes TL, Heidenreich PA, Wren SM. Association of Left Ventricular Ejection Fraction and Symptoms With Mortality After Elective Noncardiac Surgery Among Patients With Heart Failure. JAMA. 2019;321:572-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 85] [Article Influence: 14.2] [Reference Citation Analysis (0)] |
| 14. | Wang BS, Li DY, Chen XG, Wang Y. D-dimer, fibrinogen, etc for the application of joint detection in the diagnosis of acute myocardial infarction. [Article in Chinese]. Chinese Journal of Laboratory Diagnosis. 2017, 21(2): 205-207. |
| 15. | Liu LY, Liu ZJ, Xu GY, Zhang FY, Xu L, Huang YG. [Clinical Utility of Revised Cardiac Risk Index to Predict Perioperative Cardiac Events in Elderly Patients with Coronary Heart Disease Undergoing Non-cardiac Surgery]. Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2020;42:732-739. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Song H, He P, Liang JX, Shao TS, Li Y, Jia MY. Influence factors of adverse cardic events in perioperative period of noncardiac surgery in elderly patients. [Article in Chinese]. Journal of Cardiovascular and Pulmonary Diseases. 37:06-209. [DOI] [Full Text] |
| 17. | Li P, Lei Y, Li Q, Lakshmipriya T, Gopinath SCB, Gong X. Diagnosing Perioperative Cardiovascular Risks in Noncardiac Surgery Patients. J Anal Methods Chem. 2019;2019:6097375. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 18. | Ding YL, Liang LC, Liang MJ, Tan QP, Chen WQ, Liang JW. Risk factors of perioperative cardiac events in hypertensive patients undergone non-cardiac surgery Ding. [Article in Chinese]. Chin J Evid Based Cardiovasc Med. 10:360-362. [DOI] [Full Text] |
| 19. | Ratcliffe FM, Kharbanda R, Foëx P. Perioperative ST-elevation myocardial infarction: with time of the essence, is there a case for guidelines? Br J Anaesth. 2019;123:548-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Zhou X, Chen L, Su Z, Li Y, Tu M, Xiao J, Pan Z, Su D. Perioperative acute myocardial infarction in patients after non-cardiac surgery in China: Characteristics and risk factors. Medicine (Baltimore). 2019;98:e16929. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 21. | Kuthiah N, Er C. Myocardial injury in non-cardiac surgery: complexities and challenges. Singapore Med J. 2020;61:6-8. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 22. | Botto F, Alonso-Coello P, Chan MT, Villar JC, Xavier D, Srinathan S, Guyatt G, Cruz P, Graham M, Wang CY, Berwanger O, Pearse RM, Biccard BM, Abraham V, Malaga G, Hillis GS, Rodseth RN, Cook D, Polanczyk CA, Szczeklik W, Sessler DI, Sheth T, Ackland GL, Leuwer M, Garg AX, Lemanach Y, Pettit S, Heels-Ansdell D, Luratibuse G, Walsh M, Sapsford R, Schünemann HJ, Kurz A, Thomas S, Mrkobrada M, Thabane L, Gerstein H, Paniagua P, Nagele P, Raina P, Yusuf S, Devereaux PJ, McQueen MJ, Bhandari M, Bosch J, Buckley N, Chow CK, Halliwell R, Li S, Lee VW, Mooney J, Furtado MV, Suzumura E, Santucci E, Leite K, Santo JA, Jardim CA, Cavalcanti AB, Guimaraes HP, Jacka MJ, McAlister F, McMurtry S, Townsend D, Pannu N, Bagshaw S, Bessissow A, Duceppe E, Eikelboom J, Ganame J, Hankinson J, Hill S, Jolly S, Lamy A, Ling E, Magloire P, Pare G, Reddy D, Szalay D, Tittley J, Weitz J, Whitlock R, Darvish-Kazim S, Debeer J, Kavsak P, Kearon C, Mizera R, O'Donnell M, McQueen M, Pinthus J, Ribas S, Simunovic M, Tandon V, Vanhelder T, Winemaker M, McDonald S, O'Bryne P, Patel A, Paul J, Punthakee Z, Raymer K, Salehian O, Spencer F, Walter S, Worster A, Adili A, Clase C, Crowther M, Douketis J, Gangji A, Jackson P, Lim W, Lovrics P, Mazzadi S, Orovan W, Rudkowski J, Soth M, Tiboni M, Acedillo R, Garg A, Hildebrand A, Lam N, Macneil D, Roshanov PS, Srinathan SK, Ramsey C, John PS, Thorlacius L, Siddiqui FS, Grocott HP, McKay A, Lee TW, Amadeo R, Funk D, McDonald H, Zacharias J, Cortés OL, Chaparro MS, Vásquez S, Castañeda A, Ferreira S, Coriat P, Monneret D, Goarin JP, Esteve CI, Royer C, Daas G, Choi GY, Gin T, Lit LC, Sigamani A, Faruqui A, Dhanpal R, Almeida S, Cherian J, Furruqh S, Afzal L, George P, Mala S, Schünemann H, Muti P, Vizza E, Ong GS, Mansor M, Tan AS, Shariffuddin II, Vasanthan V, Hashim NH, Undok AW, Ki U, Lai HY, Ahmad WA, Razack AH, Valderrama-Victoria V, Loza-Herrera JD, De Los Angeles Lazo M, Rotta-Rotta A, Sokolowska B, Musial J, Gorka J, Iwaszczuk P, Kozka M, Chwala M, Raczek M, Mrowiecki T, Kaczmarek B, Biccard B, Cassimjee H, Gopalan D, Kisten T, Mugabi A, Naidoo P, Naidoo R, Rodseth R, Skinner D, Torborg A, Urrutia G, Maestre ML, Santaló M, Gonzalez R, Font A, Martínez C, Pelaez X, De Antonio M, Villamor JM, García JA, Ferré MJ, Popova E, Garutti I, Fernández C, Palencia M, Díaz S, Del Castillo T, Varela A, de Miguel A, Muñoz M, Piñeiro P, Cusati G, Del Barrio M, Membrillo MJ, Orozco D, Reyes F, Sapsford RJ, Barth J, Scott J, Hall A, Howell S, Lobley M, Woods J, Howard S, Fletcher J, Dewhirst N, Williams C, Rushton A, Welters I, Pearse R, Ackland G, Khan A, Niebrzegowska E, Benton S, Wragg A, Archbold A, Smith A, McAlees E, Ramballi C, Macdonald N, Januszewska M, Stephens R, Reyes A, Paredes LG, Sultan P, Cain D, Whittle J, Del Arroyo AG, Sun Z, Finnegan PS, Egan C, Honar H, Shahinyan A, Panjasawatwong K, Fu AY, Wang S, Reineks E, Blood J, Kalin M, Gibson D, Wildes T; Vascular events In noncardiac Surgery patIents cOhort evaluatioN (VISION) Writing Group, on behalf of The Vascular events In noncardiac Surgery patIents cOhort evaluatioN (VISION) Investigators; Appendix 1. The Vascular events In noncardiac Surgery patIents cOhort evaluatioN (VISION) Study Investigators Writing Group; Appendix 2. The Vascular events In noncardiac Surgery patIents cOhort evaluatioN Operations Committee; Vascular events In noncardiac Surgery patIents cOhort evaluatioN VISION Study Investigators. Myocardial injury after noncardiac surgery: a large, international, prospective cohort study establishing diagnostic criteria, characteristics, predictors, and 30-day outcomes. Anesthesiology. 2014;120:564-578. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 529] [Cited by in RCA: 651] [Article Influence: 59.2] [Reference Citation Analysis (0)] |
| 23. | Zhu ML, Huang YG, Liu XH, Zhang BZ, Liu Y, Liu DW, Yu JC, Chen W, He XD, Zhu L, Kang L, Tang S, Qin MW, Li ZJ, Yao HY. Expert consensus on perioperative management of elderly patients in Peking Union Medical College Hospital. [Article in Chinese]. Medical Journal of Peking Union Medical College Hospital. 2018;9:36-41. [DOI] [Full Text] |
| 24. | Triposkiadis F, Xanthopoulos A, Butler J. Cardiovascular Aging and Heart Failure: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;74:804-813. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 197] [Cited by in RCA: 175] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 25. | Strait JB, Lakatta EG. Aging-associated cardiovascular changes and their relationship to heart failure. Heart Fail Clin. 2012;8:143-164. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 477] [Cited by in RCA: 457] [Article Influence: 35.2] [Reference Citation Analysis (0)] |
| 26. | Pourafkari L, Tajlil A, Nader ND. Biomarkers in diagnosing and treatment of acute heart failure. Biomark Med. 2019;13:1235-1249. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 27. | Berezin AE. Circulating Biomarkers in Heart Failure. Adv Exp Med Biol. 2018;1067:89-108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 16] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 28. | Song CG, Xing XX, Chen HS, Zhang LZ. The value of combined detection of myocardial injury markers in the early diagnosis of acute myocardial infarction [J]. [Article in Chinese]. Chinese Journal of Diagnostics (Electronic Edition). 7:6-30. [DOI] [Full Text] |
| 29. | Sarhene M, Wang Y, Wei J, Huang Y, Li M, Li L, Acheampong E, Zhengcan Z, Xiaoyan Q, Yunsheng X, Jingyuan M, Xiumei G, Guanwei F. Biomarkers in heart failure: the past, current and future. Heart Fail Rev. 2019;24:867-903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 82] [Article Influence: 16.4] [Reference Citation Analysis (2)] |
| 30. | Tai WZ. Evaluation of early cardiac insufficiency by echocardiography. [Article in Chinese]. Journal of Imaging Research and Medical Applications. 2020;4:182-183. |
| 31. | Thomas L, Marwick TH, Popescu BA, Donal E, Badano LP. Left Atrial Structure and Function, and Left Ventricular Diastolic Dysfunction: JACC State-of-the-Art Review. J Am Coll Cardiol. 2019;73:1961-1977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 414] [Cited by in RCA: 453] [Article Influence: 75.5] [Reference Citation Analysis (0)] |
| 32. | Morris DA, Belyavskiy E, Aravind-Kumar R, Kropf M, Frydas A, Braunauer K, Marquez E, Krisper M, Lindhorst R, Osmanoglou E, Boldt LH, Blaschke F, Haverkamp W, Tschöpe C, Edelmann F, Pieske B, Pieske-Kraigher E. Potential Usefulness and Clinical Relevance of Adding Left Atrial Strain to Left Atrial Volume Index in the Detection of Left Ventricular Diastolic Dysfunction. JACC Cardiovasc Imaging. 2018;11:1405-1415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 135] [Cited by in RCA: 245] [Article Influence: 35.0] [Reference Citation Analysis (0)] |
| 33. | Cheng QR, Yuan L, Yu YP, Li JH. Clinical value of brain natriuretic peptide, D-dimer and high sensitive C-reactive protein in elderly acute coronary syndrome. [Article in Chinese]. Chin J Clinicians (Electronic Edition). 2014;8:2381-2384. [DOI] [Full Text] |
| 34. | Gallone G, Baldetti L, Pagnesi M, Latib A, Colombo A, Libby P, Giannini F. Medical Therapy for Long-Term Prevention of Atherothrombosis Following an Acute Coronary Syndrome: JACC State-of-the-Art Review. J Am Coll Cardiol. 2018;72:2886-2903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 69] [Article Influence: 11.5] [Reference Citation Analysis (0)] |
| 35. | Weitz JI, Fazio S. Overview of Therapeutic Approaches for Cholesterol Lowering and Attenuation of Thrombosis for Prevention of Atherothrombosis. Circ Res. 2019;124:351-353. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |