Published online Jul 16, 2022. doi: 10.12998/wjcc.v10.i20.6794
Peer-review started: December 18, 2021
First decision: January 25, 2022
Revised: February 16, 2022
Accepted: March 16, 2022
Article in press: March 16, 2022
Published online: July 16, 2022
Processing time: 198 Days and 13.8 Hours
Transurethral columnar balloon dilatation of the prostate (TUCBDP) is a new surgical treatment, but its efficacy remains controversial because of limited clinical application.
To investigate the clinical effect of TUCBDP for benign prostatic hyperplasia (BPH).
Overall, 140 patients with BPH who underwent surgical treatment were included in the study. A random number table was used to divide the participants into study and control groups (n = 70 per group). The study group underwent TUCBDP. The prostate resection surgical time, intraoperative blood loss, bladder irrigation time, catheter indwelling time, length of hospital stay, International Prostate Symptom Score (IPSS), maximum urine flow rate (Qmax), residual urine volume (RUV), changes in the International Erectile Function Score (IIEF-5) score, serum prostate-specific antigen (PSA), quality of life (QOL) score, and surgical complications were compared in both groups.
The operation time, intraoperative blood loss volume, bladder flushing time, urinary catheter indwelling time, and length of hospital stay were significantly lower in the study group than in the control group (P < 0.05). There were no significant differences in the IPSS, Qmax, and RUV measurements between the study and control groups (P > 0.05). However, at 3 mo post-surgery, the IPSS and RUV measurements were both lower (P < 0.05) and Qmax values were higher (P < 0.05) compared to the pre-surgery results in both groups. The IIEF-5 scores before and 3 mo after surgery were not significantly different between the study and control groups (P > 0.05). At 1 mo after surgery, the IIEF-5 score was higher in the study group than in the control group (P < 0.05). The serum PSA levels and QOL scores before treatment and at 1 and 3 mo after treatment were not significantly different between the study and control groups (P > 0.05). However, lower serum PSA levels and QOL scores were observed after 1 and 3 mo of treatment compared to pre-treatment levels in the study group (P < 0.05). The surgical complication rate of the study group (4.29%) was lower than that of the control group (12.86%; P < 0.05).
TUCBDP for BPH and transurethral resection of the prostate can achieve better results, but the former method is associated with less surgical trauma.
Core Tip: By comparing the clinical effects of transurethral columnar balloon dilatation of the prostate (TUCBDP) to the gold standard transurethral resection of the prostate in patients with benign prostatic hyperplasia, it was observed that although both procedures can achieve similar therapeutic effects, TUCBDP offers the additional benefits of less surgical trauma, improved recovery, and fewer surgery-associated complications.
- Citation: Zhang DP, Pan ZB, Zhang HT. Urinary and sexual function changes in benign prostatic hyperplasia patients before and after transurethral columnar balloon dilatation of the prostate. World J Clin Cases 2022; 10(20): 6794-6802
- URL: https://www.wjgnet.com/2307-8960/full/v10/i20/6794.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i20.6794
Benign prostatic hyperplasia (BPH), which refers to the proliferation of epithelial cells and the interstitium in the transitional zone of the prostate, is one of the most common encountered urological problems. The main clinical manifestation of BPH is lower urinary tract obstruction, which is more common in middle-aged and older men[1,2]. The quality of life (QOL) of patients with BPH is greatly affected because they often suffer from lower urinary tract symptoms, such as frequent micturition, urgent urination, and dysuria[3]. At present, surgical treatment is routinely advocated for patients with poor symptom control after oral drug administration, including transurethral resection of the prostate (TURP) and transurethral laser vaporization, which can significantly improve the symptoms of lower urinary tract obstruction and achieve a better curative effect. However, it can cause great harm to patients, with slow postoperative recovery, high intraoperative blood loss, and a high incidence of perioperative complications[4,5]. TUCBDP is a new surgical treatment, but its efficacy remains controversial owing to its small clinical application[6]. To explore the clinical effect of TURP with a cylindrical water bladder for the treatment of BPH, a total of 140 BPH patients who intended to undergo surgical treatment in our hospital were selected for this study.
A total of 140 patients with BPH who were scheduled to undergo surgical treatment at our hospital from March 2016 to January 2019 were selected as research participants. The participants were then randomly allocated to the study and control groups (n = 70 for each group) based on a random number table. The inclusion criteria for this study were as follows: (1) Diagnosis of BPH based on the criteria in the second edition of the Journal of Endourology, People’s Health Press[7]; (2) Presence of typical indications for surgery, including repeated symptoms, such as urinary retention, hematuria, and urinary system infection, which were treated poorly by conservative treatment; and an (3) International Prostate Symptom Score (IPSS) score ≥ 8 points. The exclusion criteria were as follows: (1) Severe heart, lung, and renal dysfunction; (2) Urinary tumors, urethral strictures, extremely reduced bladder capacity caused by severe bladder contractures, etc.; (3) Myasthenia gravis; (4) Mental illness and intellectual disability; and (5) Coagulopathy. This study conformed to the requirements of the medical ethics committee and signed informed consent was obtained from each participant.
Patients in the study group were aged 42–63 years (mean 53.5 ± 4.4 years) and had a disease duration ranging from 10–55 mo (mean 29.6 ± 9.0 mo), pre-treatment mean IPSS score of 24.6 ± 3.5 points, and a mean prostate volume of 81.3 ± 8.5 mL on preoperative ultrasonography. In the control group, patients were aged 44–65 years (mean 54.2 ± 4.9 years) and had a disease duration ranging from 12–60 mo (mean 31.8 ± 11.2 mo) a pre-treatment mean IPSS score of 24.2 ± 3.9 points, and a mean prostate volume of 83.0 ± 10.7 mL on preoperative ultrasonography. There were no significant differences in these baseline data between the two groups (P > 0.05).
Patients in the study group underwent TUCBDP. Based on the size of the patient's prostate, a suitable cylindrical water balloon catheter was chosen. The patient was placed in the lithotomy position and provided epidural plus spinal anesthesia. After successful anesthesia, the sac catheter was inserted through the urethra in a posterior direction, and then water was injected into the balloon to secure the catheter. The water injection tube was closed at a pressure of 0.3 MPa, at which time the outer balloon was located in the prostatic urethra and the inner balloon in the membranous urethra. Six hours after surgery, regular water injections were used to reduce the water pressure.
In the control group, an Olympus bipolar plasma electrotonic was used. The resection and coagulation power were 280 W and 60 W, respectively. Epidural anesthesia was provided to patients who were placed in the lithotomy position. After successful anesthesia, the resection microscope was inserted directly into the bladder. If the patient had bilateral BPH, the surgical capsule layer was cut at the bladder neck at the 1 o’clock position, and most of the lateral lobe and apical tissues were excised along with the capsule. In patients with trilobar hyperplasia, the middle lobe was excised until the capsule layer was flushed with the triangular area, and the hyperplastic glands were removed as described above. There was no obvious bleeding after careful examination, and a three-cavity catheter remained in-situ after the operation.
The operative time, intraoperative blood loss volume, bladder washing time, catheter retention time, hospital stay length, IPSS, maximum urine flow rate (Qmax), residual urine volume (RUV), International Erectile Function Score (IIEF-5), serum prostate-specific antigen (PSA) levels, and the QOL score of the two groups were compared along with the operative complication rates.
To obtain serum PSA levels, fasting venous blood (4 mL) was collected from pre- and postoperative patients and centrifuged at 3000 r/min for 5 min. The serum was separated and detected by enzyme-linked immunosorbent assay (ELISA). To prepare the ELISA plate, the standard substance was diluted by multiple ratios. The ELISA plate had separate wells for the test, standard, and blank samples. To prepare the test sample wells, we added 40 µL of sample diluent to the wells of the ELISA plate followed by 10 µL of the test sample (the final degree of sample dilution was 5 times). The plates were sealed with a sealing membrane and incubated at 37 ºC for 30 min. The washing liquid was diluted 30 times with 30 times distilled water for later use. The sealing plate membrane was carefully removed, the liquid was discarded, and the plate was spin dried. The ELISA plate was allowed to stand for 30 s after the discard and then each well was filled with washing liquid; this process was repeated 5 times and the plate was patted dry. All wells, except for the blank wells, was coated with 50 µL of tetramethylbenzidine developing base solution (YSRIBIO, Huzhou Yingchuang Biotechnology Co., Ltd., Huzhou, Zhejiang province, China). The ELISA plate was then incubated and washed. We then added 50 µL of stop solution into each well to stop the coloration, and the plate was placed in the dark at 37 ºC for 15 min to facilitate color development. The solution changed from blue to yellow, and the absorbance of each well was measured sequentially at a wavelength of 450 nm using the BioTek microplate reader (Bertone Instruments Co., Ltd., USA).
The IIEF-5 mainly includes the following five questions: (1) How confident are you in achieving and maintaining a penile erection? (2) After stimulation, how many times has the penis been erect to achieve successful vaginal penetration? (3) How many times were you able to maintain erection after vaginal penetration? (4) How many times were you able to maintain erection until the completion of sexual intercourse? and (5) Are you satisfied with your sexual experience? Patients with erectile dysfunction scored < 21 points out of a total score of 25 points.
The QOL was mainly assessed based on the subjective feelings of patients regarding the impact of nocturia, frequent micturition, urgent urination, difficulty in defecation, and urinary incontinence on their QOL. The QOL was scored as follows: very good (0 points), good (1 point), mostly satisfied (2 points), basic satisfied (3 points), mostly dissatisfied (4 points), unhappy (5 points), and very painful (6 points)[8].
Statistical analysis was performed using SPSS software version 21.0. Measured data (i.e., operation time, intraoperative blood loss, and bladder flushing time) in the two groups were represented by mean ± SD. The t-test was used to compare data between group, and intergroup comparisons of complication rates and other count data were performed using the χ2 test. P values < 0.05 were considered statistically significant.
The operation time, bleeding volume during surgery, bladder washing time, catheter indwelling time, and length of hospital stay of patients in the study group were lower than those in the control group (P < 0.05; Table 1).
| Group | n | Operation time (min) | Intraoperative blood loss (mL) | Bladder irrigation time (h) | Catheter indwelling time (d) | Hospital stay (d) |
| Study group | 70 | 18.6 ± 3.2 | 13.2 ± 4.0 | 6.3 ± 2.0 | 2.5 ± 0.5 | 2.9 ± 0.7 |
| Control group | 70 | 80.0 ± 14.8 | 66.5 ± 18.4 | 45.1 ± 13.8 | 5.1 ± 1.2 | 5.6 ± 1.5 |
| t value | -33.926 | -23.683 | -23.280 | -16.733 | -13.647 | |
| P value | 0.000 | 0.000 | 0.000 | 0.000 | 0.000 |
There were no significant differences in the IPSS score, Qmax, and RUV values between the study and control groups pre-operation and 3 mo post-operation (P > 0.05). Three months after surgery, the IPSS and RUV values of the two groups were lower than those before surgery (P < 0.05), and the Qmax measured value was higher than that before surgery (P < 0.05; Table 2).
| Group | n | Qmax (mL/s) | RUV (mL) | IPSS scores (Score) | |||
| Before therapy | Treatment for 3 mo | Before therapy | Treatment for 3 mo | Before therapy | Treatment for 3 mo | ||
| Study group | 70 | 7.69 ± 2.05 | 20.51 ± 3.04a | 98.5 ± 14.3 | 8.6 ± 2.7a | 24.6 ±3 .5 | 5.1 ± 1.6a |
| Control group | 70 | 8.20 ± 2.18 | 19.68 ± 2.88a | 101.0 ± 16.5 | 9.0 ± 3.0a | 24.2 ± 3.9 | 5.3 ± 1.9a |
| t value | -1.426 | 1.658 | -0.958 | -0.829 | 0.639 | -0.674 | |
| P value | 0.156 | 0.100 | 0.340 | 0.408 | 0.524 | 0.502 | |
There were no significant differences in the IIEF-5 scores between the study and control groups before and 3 mo after surgery (P > 0.05). One month after surgery, the IIEF-5 score of the study group was higher than that of the control group (P < 0.05; Table 3).
There was no significant difference in serum PSA levels before treatment and 1 and 3 mo after treatment between the study and control groups (P > 0.05). However, after 1 and 3 mo of treatment, the serum PSA levels of both groups were lower than those before treatment (P < 0.05; Table 4).
No significant differences in the QOL scores were observed between the two groups before treatment and after 1 and 3 mo of treatment (P > 0.05). However, the QOL scores of the two groups after 1 and 3 mo of treatment were lower than those before treatment (P < 0.05; Table 5).
The surgical complication rate in the study group was 4.29%, which was significantly lower than that of the control group (12.86%; P < 0.05; Table 6).
| Group | n | Secondary bleeding | Urinary retention | Bladder neck spasm | Urinary incontinence | Complication rate (%) |
| Study group | 70 | 1 | 0 | 1 | 1 | 3 (4.29) |
| Control group | 70 | 4 | 1 | 2 | 3 | 9 (12.86) |
| χ2 value | 4.115 | |||||
| P value | 0.042 |
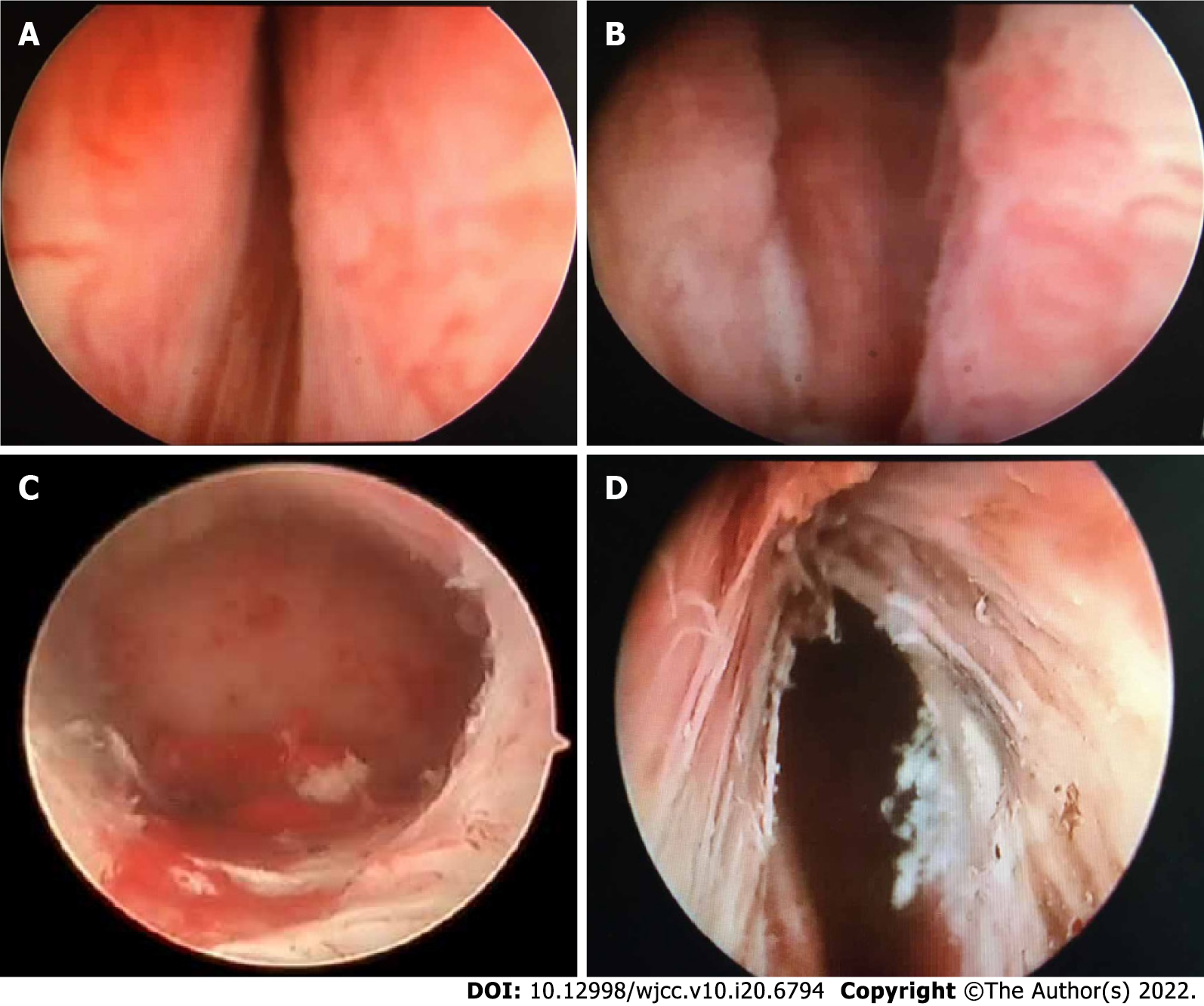
A 53-year-old male patient presented with the main clinical symptoms of frequent urination, urgency, incontinence, dysuria, repeated urinary retention, hematuria, and urinary tract infection. Postoperatively, the patient's urination symptoms were satisfactory, and quality of life was significantly improved. Intraoperative photographs are shown in Figure 1.
BPH is the main cause of urethral obstruction and lower urinary tract symptoms in elderly men, and its incidence increases with age[7]. The clinical progression of BPH may be related to hypertension and the size and index of the prostatic transitional zone. Surgery is usually required if drug control is poor. Traditional open surgery is associated with a long operation time, relatively large bleeding volume, high risk of urinary incontinence, long postoperative recovery period, high surgical tolerance requirement in patients, and relatively expensive equipment[8,9]. TURP is considered the "gold standard" treatment for BPH, but serious complications may occur, such as resection syndrome and urinary incontinence[10]. The question of how to improve patient urinary symptoms without removing the prostate needs to be urgently solved. TUCBDP is a new technology with independent intellectual property rights in China. Its greatest advantage is that it can retain the prostate organ and complete the operation in a very short time, thus minimizing the occurrence of related complications. It is a complementary surgical approach for BPH[11-13].
Mannitol, which is used in TURP surgery, inevitably penetrates blood in the human body. The longer the operation time, the greater the blood volume and lower the concentration of electrolytes in the blood[14]. TUCBDP surgery is safe and reliable, associated with minimal trauma and shorter operation time than TURP, and does not require resection of the prostate. It can easily solve the problems of obstruction and urination caused by hyperplasia and maintain patency[15]. The results of this study showed that the operation time, bleeding volume during surgery, bladder washing time, catheter indwelling time, and hospital stay of patients in the study group were significantly lower than those in the control group. Based on our findings, TUCBDP was safer and more effective than TURP for the treatment of patients with BPH. The reason for this was because after the water was directly filled in the cylindrical water sac expansion, the membranous part, the full length of the posterior urethra, and the bladder neck were dilated under high pressure and the capsule was directly and completely dehisced forward leading to a shorter forward arrival time of bilateral lobular gland dilatation and a smaller bleeding volume. It is difficult to control the depth of the excised tissue during TURP surgery, resulting in poor control of incision accuracy. The excised tissue easily adheres to the resection ring, which can block the line of sight of the surgeon, increase the operation time, and delay the operation progress. Furthermore, the placement of an indwelling urinary catheter for prolonged periods after surgery results in slow recovery.
PSA is a glycoprotein produced in prostate epithelial cells and is expressed at high levels in the serum of patients with prostate cancer. It is positively correlated with disease progression, making it a preferred marker for the detection of prostate cancer. Based on our findings, the serum PSA levels of both groups were lower after 1 and 3 mo of treatment compared to those before treatment, indicating that both surgical methods could effectively control disease progression of patients with good treatment effects. The difference between the two groups was not significant, and the accuracy of the results could be confirmed by further increasing the sample size.
The IPSS scores, QQL, Qmax, and post voiding residual urine were the main observation indices in this study[16]. The main disease progression of BPH was the aggravation of lower urinary tract symptoms, which leads to a decline in QOL, progressive decline in Qmax, and occurrence of complications (i.e., hematuria, repeated urinary infections, and renal impairment)[17]. The decline in QOL due to worsening lower urinary tract symptoms needs to be quantified by the IPSS and QOL scores[18]. In this study, the IPSS and RUV measured values of the patients were significantly lower than those before surgery, and the Qmax value was significantly higher than that before surgery. TUCBDP successfully clears the obstruction caused by hyperplasia and successfully expands the obstructed area of the urethral membrane without compromising the urethral sphincter; therefore, the risk of lower urinary tract deterioration is greatly reduced. The operation complication rate in the research group was significantly lower than that in the control group because repeated electrocoagulation is required to stop bleeding during TURP surgery. However, if the patient fails to mobilize properly or there is a sudden change in blood pressure after surgery, the wound site may coagulate and become compromised by re-bleeding. Hence, relatively more tissues need to be removed, and adverse reactions, such as resection syndrome, are more likely to occur. The IIEF-5 score of the research group was significantly higher than that of the control group because the prostate was preserved during the enlargement procedure, and high-temperature tools (i.e., electric knife and lasers) were not used during the operation. Therefore, postoperative complications were significantly reduced, and no sexual dysfunction occurred after the operation.
At present, clinical research on patients with BPH is mainly aimed at selecting safe and effective treatments. TUCBDP has been used, with good effect, for the treatment of BPH[19,20]. However, there are only few studies that have been conducted to compare longitudinal and transverse cylindrical water balloon dilatation and TURP. In the present study, the therapeutic effects of the two surgeries were compared, and the IIEF-5 score was used to diagnose penile erectile function and effectively evaluate the prognosis of d.
In summary, TUCBDP surgery for BPH and TURP have both achieved good therapeutic effects, but the former has advantages of less surgical trauma, rapid and early postoperative recovery, and fewer complications.
Benign prostatic hyperplasia (BPH) is one of the most common encountered urological problems.
Surgical treatment can cause great harm to patients, with slow postoperative recovery, high intraoperative blood loss, and a high incidence of perioperative complications.
This study aimed to explore the clinical effect of transurethral resection of the prostate (TURP) with a cylindrical water bladder for the treatment of BPH.
A total of 140 BPH patients who intended to undergo surgical treatment in our hospital were selected for this study. And randomly allocated to the study and control groups (n = 70 for each group) based on a random number table.
Lower serum prostate-specific antigen levels and quality of life scores were observed after 1 and 3 mo of treatment compared to pre-treatment levels in the study group. The surgical complication rate of the study group (4.29%) was lower than that of the control group (12.86%)
Transurethral columnar balloon dilatation of the prostate surgery for BPH and TURP have both achieved good therapeutic effects, but the former has advantages of less surgical trauma.
There are only few studies that have been conducted to compare longitudinal and transverse cylindrical water balloon dilatation and TURP. Further studies are required.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Urology and nephrology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Caliskan S, Turkey; Iwata Y, Japan S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Rajpar S, Surya B, Mobin K, Kumar S. Experience of hundred cases of transurethral resection of prostate at tertiary care hospital in Karachi. J Pak Med Assoc. 2018;68:783-786. [PubMed] |
| 2. | Pathak A, Singh M, Ramappa A, Jain S, Rasool S, Kaswan RS, Patel B. Intravesical explosion during transurethral resection of prostate: Prevention and management. Urol Ann. 2018;10:111-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Chung ASJ, Woo HH. Update on minimally invasive surgery and benign prostatic hyperplasia. Asian J Urol. 2018;5:22-27. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 28] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 4. | Watanabe D, Yamashita A, Miura K, Mizushima A. Effects on sexual function in Japanese patients with benign prostatic hyperplasia upon switching from combination therapy with α1 blocker and dutasteride to combination therapy with tadalafil and dutasteride. Aging Male. 2020;23:501-506. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Erkoc M, Otunctemur A, Besiroglu H, Altunrende F. Evaluation of quality of life in patients undergoing surgery for benign prostatic hyperplasia. Aging Male. 2018;21:238-242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Pascal LE, Mizoguchi S, Chen W, Rigatti LH, Igarashi T, Dhir R, Tyagi P, Wu Z, Yang Z, de Groat WC, DeFranco DB, Yoshimura N, Wang Z. Prostate-Specific Deletion of Cdh1 Induces Murine Prostatic Inflammation and Bladder Overactivity. Endocrinology. 2021;162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 12] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 7. | Langan RC. Benign Prostatic Hyperplasia. Prim Care. 2019;46:223-232. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 111] [Article Influence: 18.5] [Reference Citation Analysis (0)] |
| 8. | Mallikarjuna C, Nayak P, Ghouse SM, Reddy PC, Ragoori D, Bendigeri MT, Reddy S. Transurethral enucleation with bipolar energy for surgical management of benign prostatic hyperplasia: Our initial experience. Indian J Urol. 2018;34:219-222. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 9. | Kumar N, Vasudeva P, Kumar A, Singh H. Prospective Randomized Comparison of Monopolar TURP, Bipolar TURP and Photoselective Vaporization of the Prostate in Patients with Benign Prostatic Obstruction: 36 Months Outcome. Low Urin Tract Symptoms. 2018;10:17-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 10. | Zhao L, Ma YH, Chen Q, Chen YB, Gu M, Gao JF, Zhang GT, Mou JN, Bao ZH, Wang Z. [Shovel-shaped electrode transurethral plasmakinetic enucleation vs plasmakinetic resection of the prostate in the treatment of benign prostatic hyperplasia]. Zhonghua Nan Ke Xue. 2018;24:133-137. [PubMed] |
| 11. | Walker SM, Turkbey B. Role of mpMRI in Benign Prostatic Hyperplasia Assessment and Treatment. Curr Urol Rep. 2020;21:55. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Sarier M, Duman I, Kilic S, Yuksel Y, Demir M, Aslan M, Yucetin L, Tekin S, Yavuz AH, Emek M. Comparative Results of Transurethral Incision with Transurethral Resection of The Prostate in Renal Transplant Recipients with Benign Prostate Hyperplasia. Urol J. 2018;15:209-213. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 13. | Romero-Otero J, García-Gómez B, García-González L, García-Rojo E, Abad-López P, Justo-Quintas J, Duarte-Ojeda J, Rodríguez-Antolín A. Critical analysis of a multicentric experience with holmium laser enucleation of the prostate for benign prostatic hyperplasia: outcomes and complications of 10 years of routine clinical practice. BJU Int. 2020;126:177-182. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 14. | Inzunza G, Rada G, Majerson A. Bipolar or monopolar transurethral resection for benign prostatic hyperplasia? Medwave. 2018;18:e7134. [PubMed] |
| 15. | Jung JH, Park J, Kim WT, Kim HW, Kim HJ, Hong S, Yang HJ, Chung H. The association of benign prostatic hyperplasia with lower urinary tract stones in adult men: A retrospective multicenter study. Asian J Urol. 2018;5:118-121. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Schoenthaler M, Sievert KD, Schoeb DS, Miernik A, Kunit T, Hein S, Herrmann TRW, Wilhelm K. Combined prostatic urethral lift and remodeling of the prostate and bladder neck: a modified transurethral approach in the treatment of symptomatic lower urinary tract obstruction. World J Urol. 2018;36:1111-1116. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Kobe A, Donati O, Pfammatter T. [Diagnosis and Minimal Invasive Treatment of Benign Prostatic Hyperplasia]. Ther Umsch. 2020;77:53-56. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Liu FC, Hua KC, Lin JR, Pang ST, Yu HP. Prostate resected weight and postoperative prostate cancer incidence after transurethral resection of the prostate: A population-based study. Medicine (Baltimore). 2019;98:e13897. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 19. | Tenuta M, Tarsitano MG, Mazzotta P, Lucchini L, Sesti F, Fattorini G, Pozza C, Olivieri V, Naro F, Gianfrilli D, Lenzi A, Isidori AM, Pofi R. Therapeutic use of pulsed electromagnetic field therapy reduces prostate volume and lower urinary tract symptoms in benign prostatic hyperplasia. Andrology. 2020;8:1076-1085. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Heidler S, Drerup M, Lusuardi L, Bannert U, Bretterbauer K, Bures J, Dietersdorfer F, Dlouhy-Schütz E, Hessler C, Karpf R, Mittellehner LA, Mitlöhner B, Schwarz S, Thomay G, Lösch G, Freibauer C, Albrecht W. The Correlation of Prostate Volume and Prostate-specific Antigen Levels With Positive Bacterial Prostate Tissue Cultures. Urology. 2018;115:151-156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |