Published online Jan 14, 2022. doi: 10.12998/wjcc.v10.i2.502
Peer-review started: September 9, 2021
First decision: October 18, 2021
Revised: October 24, 2021
Accepted: December 3, 2021
Article in press: December 3, 2021
Published online: January 14, 2022
Processing time: 124 Days and 18.7 Hours
Complex tibial plateau fractures can seriously affect quality of life and physical and mental health of patients. The anatomical relationship between the proximal tibial bone and soft tissue is complex, resulting in different types of tibial plateau fractures. Violent trauma can lead to displaced fracture, serious soft tissue injury, and potentially, dislocation of the knee joint. Therefore, tibial plateau fractures are extremely unstable.
To assess the use of locking compression plate (LCP) + T-type steel plate for postoperative weight bearing and functional recovery of complex tibial plateau fractures.
Ninety-seven patients with complex tibial plateau fractures who underwent surgery at our hospital were selected for retrospective study. Forty-nine patients had been treated with LCP + T-type steel plate limited internal fixation (study group), and 48 patients with bilateral ordinary steel plate support (control group). The operation process index, postoperative rehabilitation related index, Rasmussen score of the knee joint, tibial plateau varus angle (TPA), tibial plateau retroversion angle (PA), and surgical complications of the two groups were compared.
The operation time and intraoperative bone graft volume in the study group were lower than those in the control group (P < 0.05). There were no significant differences in surgical bleeding, anterior external incision length, postoperative drainage, hospital stay duration, and fracture healing time between the groups (P > 0.05). There was no significant difference in the TPA and PA angle between the groups immediately and 18 mo after surgery (P > 0.05). At 12 mo after surgery, the Rasmussen scale score was higher in the study group than in the control group (P < 0.05). There was no significant difference in the Rasmussen scale score at 18 mo after surgery, and the radiology score at 12 and 18 mo after surgery, between the two groups (P > 0.05). The postoperative complication rate in the study group (3.77%) was lower than that in the control group (15.09%; P < 0.05).
LCP + T-type steel plate internal fixation has advantages in terms of minimizing trauma and enabling early postoperative functional exercise, promoting functional recovery and lower limb weight-bearing, and reducing postoperative complications.
Core Tip: Locking compression plate + T-type steel plate limited internal fixation treatment has the advantage of less trauma and enables early postoperative functional exercise to promote functional recovery and lower limb weight-bearing besides being associated with less postoperative complications.
- Citation: Li HF, Yu T, Zhu XF, Wang H, Zhang YQ. Locking compression plate + T-type steel plate for postoperative weight bearing and functional recovery in complex tibial plateau fractures. World J Clin Cases 2022; 10(2): 502-510
- URL: https://www.wjgnet.com/2307-8960/full/v10/i2/502.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i2.502
Tibial plateau fracture is one of the most common types of fractures in clinical practice. It is frequently caused by violent trauma to the tibial plateau that results in the fracture and even articular surface collapse. It can be accompanied by serious knee varus and joint instability, which has a major impact on the activity and function of the knee joint. Patients with complex tibial plateau fractures are prone to developing skin necrosis, incision site infection, and joint instability after surgery; thus, early active treatment is needed[1]. The clinical treatment criteria for complex tibial plateau fractures recommends anatomical reduction, firm and stable fixation, and early training. Currently, operational treatment requires good biomechanical function, anatomical reduction of the articular surface, and reduction of soft tissue damage. In the past, double plate internal fixation was used in clinical practice; however, the procedure involved adjunct stripping of soft tissue, resulting in increased postope
A total of 97 patients with complex tibial plateau fractures who underwent surgery at our hospital were selected for retrospective study. Based on the operation method, 49 patients who were treated with LCP + T-type steel plate limited internal fixation were included in the study group, and 48 patients who were treated with bilateral ordinary steel plate support were included in the control group. The inclusion criteria were as follows: (1) Complex tibial plateau fractures with a clear history of trauma; (2) Closed fracture type; (3) Main clinical symptoms of lower limb pain, swelling, deformity, and dysfunction; (4) Diagnosis of the complex tibial plateau fracture by X-ray and computed tomography; (5) Age 19 to 59 years; (6) Schatzker type V-VI; and (7) Surgery undertaken within 2 wk after the trauma. The exclusion criteria were as follows: (1) Fractures caused by diseases (malignant bone tumor, bone tuberculosis, severe osteoporosis); (2) Presence of hematological diseases; (3) Simultaneous occurrence of severe vascular and nerve injury or soft tissue defects, and a contaminated wound; (4) Mental or intellectual impairment; and (5) Presence of other diseases leading to muscle atrophy or neurological disorders.
In the study group, LCP + T-type steel plate limited internal fixation had been performed. The patient was placed half supine, and the affected knee was raised and flexed at approximately 30° with external rotation. A posteromedial incision 8–12 cm in length was made at the posterior edge of the semitendinosus muscle. Entry was at the muscle space between the gastrocnemius muscle and medial head of the semitendinosus muscle. The semi-membranous muscle was cut and pulled medially. The joint capsule was then cut. The medial meniscus was pulled to the femoral side with a meniscus hook to expose the medial and lateral articular surfaces of the tibial plateau. The posteromedial tibial plateau was fixed with a T-shaped plate, and the lateral tibial plateau condyle fracture was treated with a bone graft. After temporary fixation with a Kirschner wire, C-arm fluoroscopy was performed to confirm recovery of the articular surface height. The LCP was selected and adjusted to the best position. A cortical bone screw was temporarily screwed into the appropriate position of the plate, and several locking screws were screwed into the proximal and distal parts of the plate.
In the control group, bilateral ordinary steel plate support was used. The patient was placed semi-supine on the fluoroscopic operating table and an arc incision was made along the adductor tuberosity of the femur, terminating at the medial side of the tibial tuberosity. The skin and subcutaneous tissue were incised to expose the medial expansion of the quadriceps femoris. The sartorius muscle and goose foot were gently pulled back to open the medial joint capsule. At the same time, the meniscus was pulled to the femoral side to clearly expose the medial platform. After fracture reduction, Kirschner wire fixation was used to confirm that the reduction was satisfactory, and an ordinary supporting plate was inserted. After fracture block reduction, an appropriate amount of artificial bone or allogeneic bone was implanted in the bone defect. After confirming that the height of the articular surface was restored, the ordinary supporting plate was selected, and several cancellous lag screws and cortical screws were successively screwed into the proximal and distal parts of the plate.
Operation time, blood loss, anterior external incision length, intraoperative bone graft volume, postoperative drainage volume, hospitalization duration, fracture healing time, complete weight-bearing time, Rasmussen score, tibial plateau varus angle (TPA), tibial plateau retroversion angle (PA), and postoperative complications at different points after surgery in the two groups were assessed and compared.
The Rasmussen score was used to evaluate mainly two aspects the knee joint function: (1) Subjective aspects: degree of pain (6 points) and walking ability (6 points). Based on the findings of physical examination by clinicians, each item of knee stability, knee extension, and range of motion was scored, the highest score being 6; the total scores were classified as excellent (≥ 27), good (20–26), medium (10–19), or poor (< 10); and (2) Radiology: the main outcome measures included condylar widening, articular surface collapse, and angulation deformity, with the highest score of 6 for each evaluation item; the total scores were classified as excellent (18), good (12–17), medium (6–12), or poor (< 6).
The patients were followed up by telephone or by clinic visits for routine examination. The patients were examined and assessed for postoperative complications and knee function recovery. The follow-up duration was at least 18 mo.
SPSS 21.0 (IBM Corp., Armonk, NY, USA) was used for data analysis. Quantitative data such as the operation time and intraoperative bone graft volume were expressed as mean ± SD; t-test was used to analyze the differences between the two groups. Qualitative data, such as the complication rate, were analyzed using the χ2 test. P < 0.05 was considered statistically significant.
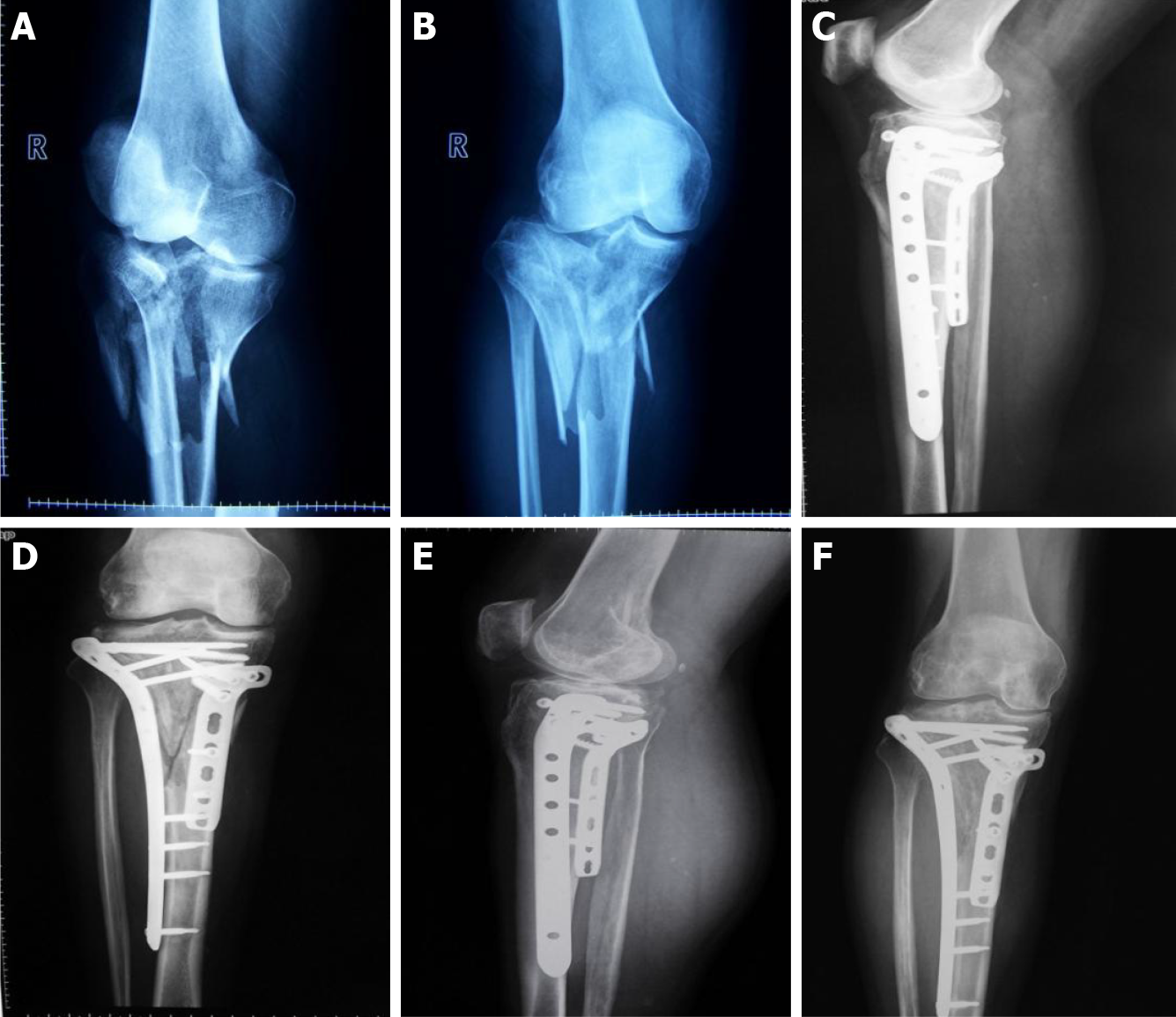
In the study group, the average age was 38.3 ± 8.5 years (range, 23-55 years). There were 31 males and 18 females. The time interval between the fracture and operation was 7.9 ± 1.2 d. There were 27 fractures on the left side and 22 on the right side. The Schatzker classifications were type V in 22 cases and type VI in 27 cases (Figure 1). The causes of injury were traffic accidents in 31 cases, falls in 11 cases, and other causes in 7 cases.
In the control group, the average age was 40.0 ± 7.2 years (range, 25-56 years). There were 28 males and 20 females. The time interval between the fracture and operation was 8.1 ± 1.1 d. There were 24 cases on the left side and 24 cases on the right side. The Schatzker classifications were type V in 20 cases and type VI in 28 cases. The causes of injury were traffic accidents in 27 cases, falls in 9 cases, and other causes in 12 cases. There was no significant difference in the baseline data between the two groups (P > 0.05).
Operation time and intraoperative bone graft volume were lower in the study group than in the control group (P < 0.05). There was no statistically significant difference between the two groups in surgical bleeding, anterior external incision length, postoperative drainage, and duration of hospital stay (P > 0.05) as shown in Table 1.
| Group | n | Operation time (min) | Surgical bleeding (mL) | Anterior external incision length (cm) | Intraoperative bone graft (g) | Postoperative drainage (mL) | Hospital stays (d) |
| Study group | 49 | 118.3 ± 14.0 | 339.4 ± 38.0 | 17.5 ± 2.2 | 7.10 ± 1.87 | 139.4 ± 34.0 | 7.4 ± 1.5 |
| Control group | 48 | 130.1 ± 16.3 | 344.1 ± 42.6 | 17.8 ± 2.6 | 9.23 ± 2.04 | 143.8 ± 39.6 | 7.8 ± 1.7 |
| t value | -3.827 | -0.574 | -0.614 | -5.362 | -0.588 | -1.229 | |
| P value | 0.000 | 0.568 | 0.541 | 0.000 | 0.558 | 0.222 |
Full load bearing was earlier in the study group than in the control group (P < 0.05). There was no statistically significant difference between the study group and the control group in the fracture healing time (P > 0.05, Table 2).
| Group | n | Fracture healing time (wk) | Full load time (wk) |
| Study group | 49 | 13.5 ± 1.7 | 14.6 ± 1.2 |
| Control group | 48 | 14.0 ± 2.0 | 16.2 ± 1.8 |
| t value | -1.328 | -5.161 | |
| P value | 0.187 | 0.000 |
There was no statistically significant difference between the two groups in the angles of TPA and PA both immediately after surgery and 18 mo thereafter (P > 0.05, Table 3).
| Group | n | TPA angle (°) | PA angle (°) | ||
| Immediately after surgery | 18 mo after surgery | Immediately after surgery | 18 mo after surgery | ||
| Study group | 49 | 86.34 ± 3.81 | 86.04 ± 2.51 | 9.54 ± 2.20 | 9.83 ± 1.72 |
| Control group | 48 | 86.51 ± 3.44 | 85.78 ± 2.92 | 9.31 ± 2.14 | 9.91 ± 1.84 |
| t value | -0.231 | 0.471 | 0.522 | -0.221 | |
| P value | 0.818 | 0.639 | 0.603 | 0.825 | |
At 12 mo after surgery, the Rasmussen scale subjective evaluation score was significantly higher in the study group than in the control group (P < 0.05). However, there was no significant difference between the two groups in the Rasmussen scale subjective evaluation score at 18 mo after surgery and in the radiology score at 12 and 18 mo after surgery (P > 0.05, Table 4).
| Group | n | Subjective evaluation score (points) | Radiology evaluation (points) | ||
| 12 mo after operation | 18 mo after surgery | 12 mo after operation | 18 mo after surgery | ||
| Study group | 49 | 18.84 ± 3.50 | 25.81 ± 2.50 | 10.41 ± 2.10 | 15.50 ± 1.32 |
| Control group | 48 | 16.57 ± 3.32 | 25.21 ± 2.64 | 10.13 ± 2.32 | 15.16 ± 1.27 |
| t value | 3.276 | 1.150 | 0.623 | 1.292 | |
| P value | 0.001 | 0.253 | 0.534 | 0.199 | |
The postoperative complication rate was significantly lower in the study group than in the control group (3.77% vs 15.09%, P < 0.05) as shown in Table 5.
| Group | n | Incision infection | Delayed fracture union | Traumatic arthritis | Complication rate |
| Study group | 49 | 1 | 0 | 1 | 2 (3.77) |
| Control group | 48 | 4 | 1 | 3 | 8 (15.09) |
| χ2 | 4.153 | ||||
| P value | 0.042 |
The tibial plateau consists of the medial platform, lateral platform, and intercondylar ridge. The bone density of the lateral platform is less than that of the medial platform. When suffering localized trauma, the lateral platform is more prone to split or collapse. The anterior and posterior cruciate ligaments connect the femoral condyles and tibial intercondylar parts to stabilize the knee joint[5,6]. The medial collateral ligament ends in the marginal compartment of the medial platform; thus, when the medial platform fractures, the medial collateral ligament is prone to contusion or even rupture[7]. Currently, the clinical treatment goal for tibial plateau fracture reduction is anatomical reduction of the articular surface, preventing articular surface collapse or step formation, and firm and stable fixation, so as to obtain a long-term stable, well-aligned, normal, and painless joint, and prevent the occurrence of post-traumatic arthritis and other complications[8]. However, studies have found that complex tibial plateau fractures are often accompanied by other conditions including peripheral ligament injury, surrounding soft tissue swelling, joint instability due to an uneven articular surface, and acute varus[9].
Surgery is the main treatment modality for complex tibial plateau fractures; to ensure correct reduction and prevention of related complications, it is important to choose the correct operative approach. High-energy injuries can cause Schatzker type V and VI tibial plateau fractures. Most of the knee joint surface becomes severely comminuted and is accompanied by severe soft tissue injury due to intra-articular fractures. The purpose of treating intra-articular fractures is to restore the smoothness of the articular surface, axial alignment, stability of the joint, and normal functional activities of the joint. The treatment chosen at the time of operation must provide enough stability and allow the patient to exercise properly at an early timepoint[10].
In our study, the differences in the outcomes of LCP + T-type steel plate limited internal fixation and bilateral ordinary steel plate support were compared. Bilateral ordinary steel plate operation allows the surgical field to be clearly exposed, thus exposing the joint surface. Through the comprehensive exploration of the articular surface and meniscus ligament injury, the disadvantage of the short distance between the predetermined incision line and the auxiliary incision line in the bilateral incision of the knee can be overcome. However, large soft tissue flaps need to be separated from the medial and lateral sides during the operation, which may cause more injury to patients and require physicians to have higher technical skill[11]. In LCP + T-type steel plate limited internal fixation, an anterolateral conventional incision combined with small posteromedial limited incision can be used to expose each part of the medial and lateral plateau, allowing for the accurate reduction of fracture fragments from different angles and orientations and enabling the management of posterior medial condyle or posterior lateral condyle fractures of the tibial plateau[12-14]. Studies have found that LCP + T-type steel plate limited internal fixation has the advantages of a smaller contact area with the periosteum, less soft tissue injury, and easier placement of plate. Through biomechanical studies, some scholars have found that the contact area between the ordinary double steel plate and the periosteum is large, which can easily affect the blood supply of the fractured ends after surgery, leading to delayed- or non-union of the fracture after the operation. However, using the medial plate is better because less soft tissue and periosteum removal is required to clearly expose the broken end of the fracture. It not only causes less soft tissue injury but also makes the plate easier to place, which is more conducive for the postoperative recovery of patients[15]. Studies have also found that the use of a medial plate requires a smaller amount of artificial bone or allograft to be inserted to prevent poor support than the traditional double plate; in order to ensure the postoperative reduction of the platform without loss, a large amount of artificial bone or allograft was inserted to support the articular surface height[16-18].
During the operation, we also found that the patient should be in the semi-supine position. By rotating the operating table and the affected limb, the posteromedial and anterolateral parts of the knee could be clearly exposed to facilitate intraoperative fracture reduction. At the same time, the anterolateral and anteromedial incisions can be made simultaneously during the operation to expose the posteromedial side, so that the affected limb is in a slightly flexed state, and the gastrocnemius muscle is relatively relaxed to fully expose the posterior side. In addition, attention should be paid to the protection of the great saphenous vein and saphenous nerve[19,20].
In our study, operation time and intraoperative bone graft volume in the study group was less in the study group than in the control group, indicating that LCP + T-type steel plate limited internal fixation for complex tibial plateau fractures can shorten the operation time and reduce intraoperative bone graft. Full load bearing in the study group was earlier than in the control group, but there was no statistically significant difference in the fracture healing time between the two groups, indicating that LCP + T-type steel plate limited internal fixation for complex tibial plateau fractures is helpful for early training in patients but has no significant effect on the fracture healing time; this finding may have been affected by the small number of patients enrolled. The comparison of TPA and PA angle between the study group and the control group immediately after the operation and at 6 mo after the operation showed no statistically significant differences between the groups, suggesting that the application of the two internal fixation methods in complex tibial plateau fractures will not have an effect on the varus angle and posterior angle. Three months after the operation, the subjective evaluation scores of the Rasmussen scale of the knee in the study group were higher than those in the control group, suggesting that LCP + T-type steel plate limited internal fixation for the treatment of complex tibial plateau fractures is beneficial for the recovery of knee function at the early stage. Furthermore, the rate of postoperative complications was significantly lower in the study group (3.77%) than in the control group (15.09%), suggesting that LCP + T-type steel plate limited internal fixation for the treatment of complex tibial plateau fractures can reduce the incidence of postoperative complications.
This study compared the effects of two internal fixation methods in patients with complex tibial plateau fractures and confirmed that LCP + T-type steel plate limited internal fixation can shorten the operation time and obtain strong and effective internal fixation, which is consistent with the results of previous studies. Meanwhile, this study also found that the LCP + T-type steel plate method has a further advantage of earlier full load bearing, which is conducive for early postoperative knee rehabilitation and exercise; thus, it is more in line with the concept of fracture internal fixation, which was relatively rare in previous studies. However, due to the small number of patients enrolled in this study and many factors affecting the postoperative recovery of patients with complex tibial plateau fractures, long-term follow-up was not carried out in this study. Therefore, it is necessary to expand the sample size, conduct long-term follow-up, and carry out prospective trials for an in-depth demonstration of the superiority of LCP + T-type steel plate limited internal fixation over bilateral ordinary steel plate support in the treatment of complex tibial plateau fractures.
In conclusion, LCP + T-type steel plate limited internal fixation treatment has the advantage of less trauma and enables early postoperative functional exercise to promote functional recovery and lower limb weight-bearing besides being associated with less postoperative complications.
Tibial plateau fracture has a serious impact on the movement and function of the knee joint, resulting in serious dysfunction. The clinical application of locking plate can not only reduce soft tissue injury, but also reduce the occurrence of postoperative necrosis, but the stability of articular surface of locking plate can not be guaranteed. In this study, locking compression plate (LCP) and T-shaped plate were used to treat complex tibial plateau fractures, in order to find a more reliable method of internal fixation for clinic.
This study compared the difference between bilateral common plate support and LCP+ T plate limited internal fixation. Bilateral common plate peeling during operation can make the operative visual field more clearly exposed and expose the articular surface. Through omni-directional exploration of articular surface and ligament meniscus injury, it can further improve the disadvantage of too short distance between predetermined incision line and auxiliary incision line in bilateral incision of knee joint.
This study aimed to explore a surgical method for the treatment of complex tibial plateau fractures with less trauma, faster postoperative recovery and fewer postope
Operation time, blood loss, anterior external incision length, intraoperative bone graft volume, postoperative drainage volume, hospitalization duration, fracture healing time, complete weight-bearing time, Rasmussen score, tibial plateau varus angle, tibial plateau retroversion angle, and postoperative complications at different points after surgery in the two groups were assessed and compared.
In our study, operation time and intraoperative bone graft volume in the study group was less in the study group than in the control group, indicating that LCP + T-type steel plate limited internal fixation for complex tibial plateau fractures can shorten the operation time and reduce intraoperative bone graft. LCP + T-type steel plate limited internal fixation for the treatment of complex tibial plateau fractures can reduce the incidence of postoperative complications.
LCP + T-type steel plate limited internal fixation treatment has the advantage of less trauma and enables early postoperative functional exercise to promote functional recovery and lower limb weight-bearing besides being associated with less postope
It is necessary to expand the sample size, conduct long-term follow-up, and carry out prospective trials for an in-depth demonstration of the superiority of LCP + T-type steel plate limited internal fixation over bilateral ordinary steel plate support in the treatment of complex tibial plateau fractures.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Orthopedics
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Catani F, Hassani K S-Editor: Wang JL L-Editor: A P-Editor: Wang JL
| 1. | Ramponi DR, McSwigan T. Tibial Plateau Fractures. Adv Emerg Nurs J. 2018;40:155-161. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 2. | Jirangkul P, Jitprapaikulsarn S, Songpatanaslip T. Outcomes Following Temporary Kapandji Pinning Technique and Distal Radial LCP Fixation for Intra-Articular Fractures of the Displaced Distal Radius. Tech Hand Up Extrem Surg. 2019;23:38-43. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Buranaphatthana T, Apivatthakakul T, Apivatthakakul V. Anteromedial minimally invasive plate osteosynthesis (MIPO) for distal third humeral shaft fractures - Is it possible? Injury. 2019;50:1166-1174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Baum C, Leimbacher M, Kriechling P, Platz A, Cadosch D. Treatment of Periprosthetic Femoral Fractures Vancouver Type B2: Revision Arthroplasty Versus Open Reduction and Internal Fixation With Locking Compression Plate. Geriatr Orthop Surg Rehabil. 2019;10:2151459319876859. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 39] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 5. | Zeman J, Matějka T, Zeman P, Belatka J, Matějka J. [Outcomes of Treatment of Calcaneal Fractures Using Locking Compression Plate with or without Augmentation]. Acta Chir Orthop Traumatol Cech. 2019;86:413-418. [PubMed] |
| 6. | Bernholt DL, Dornan GJ, DePhillipo NN, Aman ZS, Kennedy MI, LaPrade RF. High-Grade Posterolateral Tibial Plateau Impaction Fractures in the Setting of a Primary Anterior Cruciate Ligament Tear Are Correlated With an Increased Preoperative Pivot Shift and Inferior Postoperative Outcomes After Anterior Cruciate Ligament Reconstruction. Am J Sports Med. 2020;48:2185-2194. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 7. | McGonagle L, Cordier T, Link BC, Rickman MS, Solomon LB. Tibia plateau fracture mapping and its influence on fracture fixation. J Orthop Traumatol. 2019;20:12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 11] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 8. | Fabris V, Reginato VF, Smaniotto C, Bacchi A, Consani RLX. Treatment of Resorbed Mandibles with Titanium Plate and Immediate Implant-Supported Prosthesis - Case Series. Braz Dent J. 2019;30:244-251. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 9. | Santana A Junior, Debastiani JC, Kunz RI, Buratti P, Brancalhão RMC, de Fátima Chasko Ribeiro L, Torrejais MM, Bertolini GRF. Association of sericin and swimming on the phenotype, motor plate, and functionality of the denervated plantar muscle of Wistar rats. J Exerc Rehabil. 2018;14:24-31. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 10. | Garner MR, Warner SJ, Lorich DG. Surgical Approaches to Posterolateral Tibial Plateau Fractures. J Knee Surg. 2016;29:12-20. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 11. | Shur VB, Malezhik V, Svyatkovsky V. Posterolateral Spiral-Shaped One Third Tubular Plate Stabilization for a Long Spiral Fracture of the Lateral Malleolus. J Foot Ankle Surg. 2018;57:579-582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 12. | Kempthorne J, Kieser DC, Walker CG. Optimal plate fixation of distal femoral fractures in the presence of a well fixed cemented hip arthroplasty femoral stem. Hip Int. 2018;28:657-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Duan KD, Huang JR. [Progress in diagnosis and treatment of posterior condylar fracture of tibial plateau]. Zhongguo Gu Shang. 2019;32:1173-1176. [PubMed] |
| 14. | Garnavos C. Intramedullary Nailing with a Suprapatellar Approach and Condylar Bolts for the Treatment of Bicondylar Fractures of the Tibial Plateau. JB JS Open Access. 2017;2:e0017. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 15. | Karakasli A, Acar N, Uzun B. Straight-Forward versus Bicortical Fixation Penetrating Endplate in Lumbosacral Fixation-A Biomechanical Study. J Korean Neurosurg Soc. 2018;61:180-185. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 16. | Yuan GH, Zheng X, Chen K. [Combined surgical approaches in the treatment of complex tibial plateau fractures]. Zhongguo Gu Shang. 2017;30:89-92. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 17. | Adams JDJ Jr, Loeffler MF. Soft Tissue Injury Considerations in the Treatment of Tibial Plateau Fractures. Orthop Clin North Am. 2020;51:471-479. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 18. | Borrelli J Jr. Management of soft tissue injuries associated with tibial plateau fractures. J Knee Surg. 2014;27:5-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 15] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Tran AA, Shen J, Wernecke C, Gatewood CT, Harris AHS, Dragoo JL. A comparison of the Functional Movement ScreenTM and the Landing Error Scoring System: A cohort study. Curr Orthop Pract. 2020;31:8-12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 20. | Rudran B, Little C, Wiik A, Logishetty K. Tibial Plateau Fracture: Anatomy, Diagnosis and Management. Br J Hosp Med (Lond). 2020;81:1-9. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |