Published online Jan 14, 2022. doi: 10.12998/wjcc.v10.i2.437
Peer-review started: June 14, 2021
First decision: October 18, 2021
Revised: October 25, 2021
Accepted: December 10, 2021
Article in press: December 10, 2021
Published online: January 14, 2022
Processing time: 211 Days and 4.7 Hours
Digital radiography has recently been used in dentistry as a substitute for conventional film radiography worldwide. Digital imaging has many advantages and provides new possibilities for recording and interpreting radiographic data. This system uses different types of digital receptors.
To detect the frequency, type, and reasons behind the appearance of intraoral image artifacts acquired by photostimulable phosphor plates (PSP).
This retrospective descriptive study was conducted in the oral and maxillofacial radiology unit of the dental clinics of the College of Dentistry, Princess Nourah University (PNU). All intraoral digital radiographs were acquired using (Gendex Expert DC., United States) an intraoral X-ray machine with 7 -mA, 65-kVP using a PSP system (Soredex DIGORA Optime imaging plate) and laser scanners (Soredex DIGORA Optime), which can house all sizes of reusable intraoral PSP sensor plates with image acquisition software (MIPACS Dental Enterprise viewer 3.2.2). A total of 50000 intraoral radiographs were retrieved from the clinical database from April 2018 to April 2020 to evaluate the reason, type, and solutions to these image artifacts.
Overall, 50000 intraoral digital radiographs were acquired in a two-year-period; that is, from April 2018 to April 2020. Of these, 3550 (7.1%) retakes were per
Our study discussed intraoral image artifacts that were characteristic of PSP, where the most common artifacts were bitemarks, image size reduction, scratches, and delayed scanning.
Core Tip: Digital radiography has been used widely in dentistry as a substitute to conventional film radiography. Digital radiography holds many advantages and provides a wide range of possibilities to interpret and archive radiographic images. The latter system uses different types of digital receptors, and as any recent technology, different types of image pitfalls are expected. Therefore, these pitfalls render improper diagnosis for the radiographic images. The appearance of intraoral radiographic image artifacts can be produced by using the reusable intraoral photostimulable phosphor sensor plates. Thus, recognizing these errors and defining the causes and their trouble-shooting are crucial factors in making images possess great clinical impacts.
- Citation: Elkhateeb SM, Aloyouny AY, Omer MMS, Mansour SM. Analysis of photostimulable phosphor image plate artifacts and their prevalence. World J Clin Cases 2022; 10(2): 437-447
- URL: https://www.wjgnet.com/2307-8960/full/v10/i2/437.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i2.437
Digital radiography has recently been used in dentistry as a substitute for conventional film radiography worldwide. Digital imaging provides new possibilities for recording and interpreting radiographic data in a user-friendly digital way for archiving and teleradiography[1]. Digital imaging has many advantages over film-based radiography, such as real-time imaging, not needing the use of darkroom chemicals, having image manipulation tools, better archiving, and decreased patient and operator radiation exposure[2-6].
Dental radiography is provided by two main types of radiography: Conventional and digital radiography. Conventional radiography uses dental films that require chemical solutions for processing, more human resources, is time consuming, and with a higher radiation dose. This traditional type of radiography provides a permanent record of imaging without any possibility for archiving, and any error requires the retake of the radiograph, which exposes the patient to unnecessary additional radiation exposure. This is in contrast to digital radiography, which allows image manipulation to correct the visual characteristics of the image, such as contrast, brightness, and density, thus enhancing image quality without the need to retake the image. Digital radiography permits easy archiving of images and their electronic transfer between different specialties in the dental field. Digital radiographic technology uses electronic image receptors (digital sensors or plates), which are based on two main techniques in acquiring the image: A direct method using a charge-coupled device (CCD) or complementary metal oxide semiconductor (CMOS) sensors[7] that transmit the signal of the exposed plate directly over a wire with a real-time image on the monitor or indirect method using a photostimulable phosphor storage plate (PSP), which forms a latent image when exposed to radiation. The stored energy is then transported to a computer for display using a laser scanner[8-10].
The scanning times of PSP plates vary from a few seconds to several minutes, depending on the type of laser scanner used and the spatial and contrast resolutions of the image[5]. PSP plates are available in a variety of sizes in a way similar to conventional films, so they are vulnerable to bending and scratching during handling[2,11].
Moreover, PSP plates must be handled more carefully than films because they are reusable after erasing the image[12]. PSP plates are selected by most dental practitioners because of their easy intraoral placement with little patient discomfort, as well as them being cordless and resembling conventional films. This is in comparison to the more difficult intraoral placement of CCD plates, with more patient discomfort caused by the stiffness of these plates with a cord linking them to the computer even though an image can be obtained promptly by the practitioner after exposure of the plate in this system[11,12].
Digital radiography, like any evolving technology, produces a new type of image pitfall that remains a problem for clinicians in that it can be overwhelming. To the best of our knowledge, a systematic review of dental digital radiography artifacts in clinical usage has not yet been reported[13]. In addition, few studies have assessed PSP image errors using illustrative figures[14].
This retrospective descriptive study was conducted in the oral and maxillofacial radiology unit of the dental clinics of the College of Dentistry, Princess Nourah University (PNU), where conventional film-based radiography was gradually replaced by digital radiography starting in 2018. All the intraoral digital radiographs were acquired using (Gendex Expert DC., United States) an intraoral X-ray machine with 7 -mA 65-kVP using a PSP system (Soredex DIGORA Optime imaging plate) and laser scanners (Soredex DIGORA Optime), which can house all sizes of reusable intraoral PSP sensor plates with image acquisition software (MIPACS Dental Enterprise viewer 3.2.2).
The investigators retrieved all the digital intraoral periapical and bitewing radiographs that were taken and approved by the clinicians from all dental specialties in our college and with the consent of the patients from April 2018 to April 2020. We used the Medicor Imaging/MIPACS Toolkit software, which regularly detects and records all deleted radiographs due to retakes performed by all oral radiology technicians in the radiology unit with clarification of the image type. All the retakes were screened by two well-experienced oral and maxillofacial radiologists for evaluation of the present artifact type and cause, while the remaining images without errors were excluded from the study. Artifacts were classified into three categories: plate errors, scanning errors, and operator errors. First, two observers sat together in a collaboration session to determine the criteria and subtypes for each category of digital artifacts to unify the interpretation process.
The observers independently evaluated and agreed on image artifacts. When disagreement existed among them, consensus was reached through discussion. Out of the selected cases, 1000 images with errors were reevaluated by both investigators after 2 wk for the calculation of interobserver reliability. Our retrospective study was approved by the institutional review board (IRB) of PNU.
Statistical analysis was performed using SPSS Statistics version 23 (IBM Corp., New York, NY; formerly SPSS Inc., Chicago, IL, United States), and the frequencies and percentages of PSP artifacts were calculated. Interobserver reliability was analyzed with kappa analyses, which was interpreted as follows: P value < 0 denoted less than chance agreement, 0.01-0.20 denoted slight agreement, 0.21-0.40 denoted fair agreement, 0.41-0.60 denoted moderate agreement, 0.61-0.80 indicated substantial agreement, and 0.81-0.99 was considered almost perfect agreement[13].
A total of 50000 intraoral digital radiographs were acquired in the 2 year-period from April 2018 to April 2020. Of these, 3550 (7.1%) retakes were performed due to the presence of image artifacts. Of these retakes, 5% was related to operator errors and 2.1% was related to plate and scanning errors. The calculated kappa value for interobserver reliability was 0.99, indicating almost perfect interobserver agreement.
Intraoral radiographs requiring retakes due to image artifacts included 2869 (80.8%) periapical (PA) images, 518 (14.6%) bite wing images, and 163 blank images (4.6%).
Imaging artifacts were divided into three categories. Of the 3550 retakes, operator errors were the most common and were observed in 2500 images (70.4%), while plate errors were detected in 685 images (19.3%) and scanning errors in 365 images (10.3%).
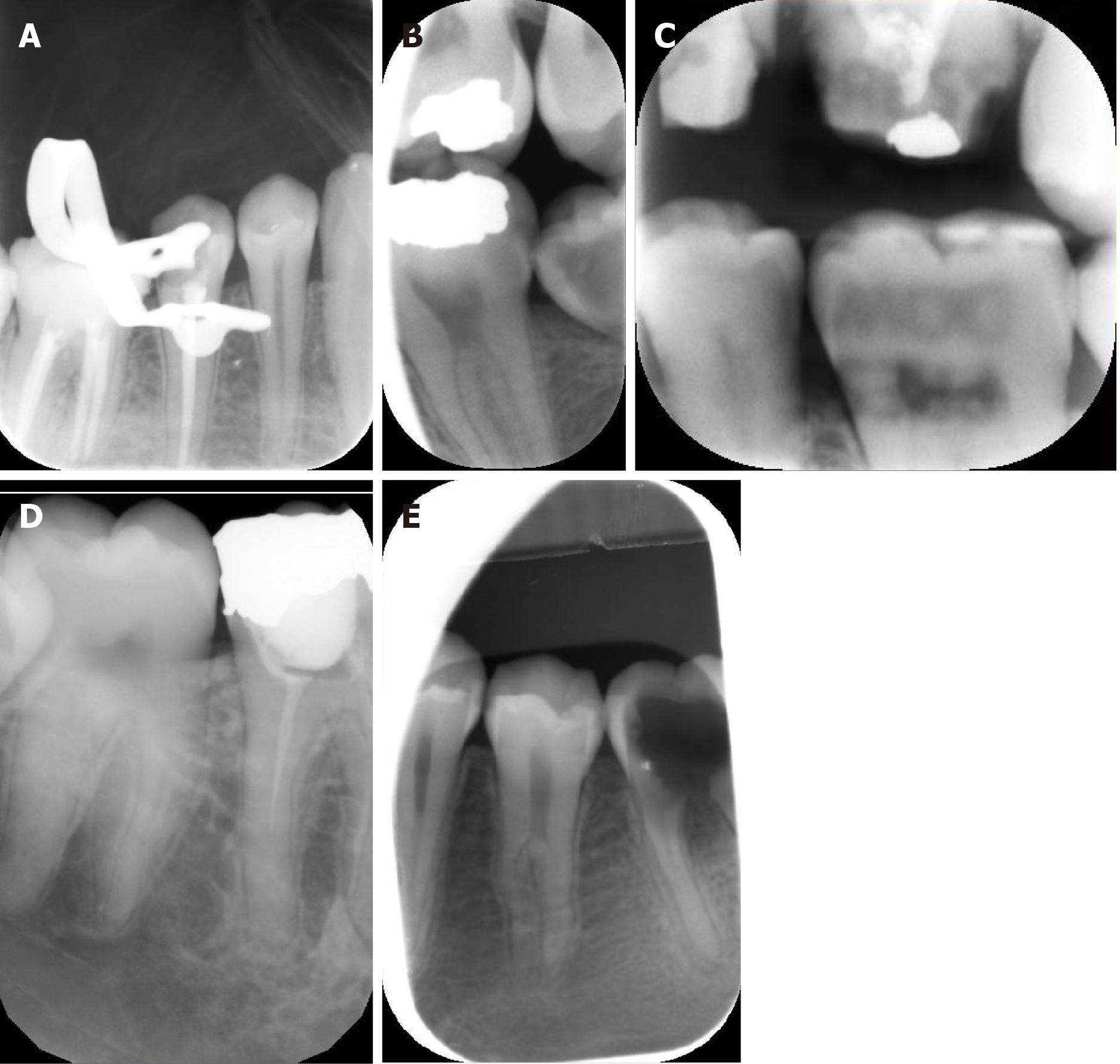
In this study, the operator error category consisted of eight subtypes that were closely similar to the same error categories in conventional film radiography, as this type of artifact does not depend on the type of image receptor except for the reversed or mirror image, movement of the plate inside the packet, and double exposure in the plate either due to partial erasing of the previous image or failure of the image scanning.
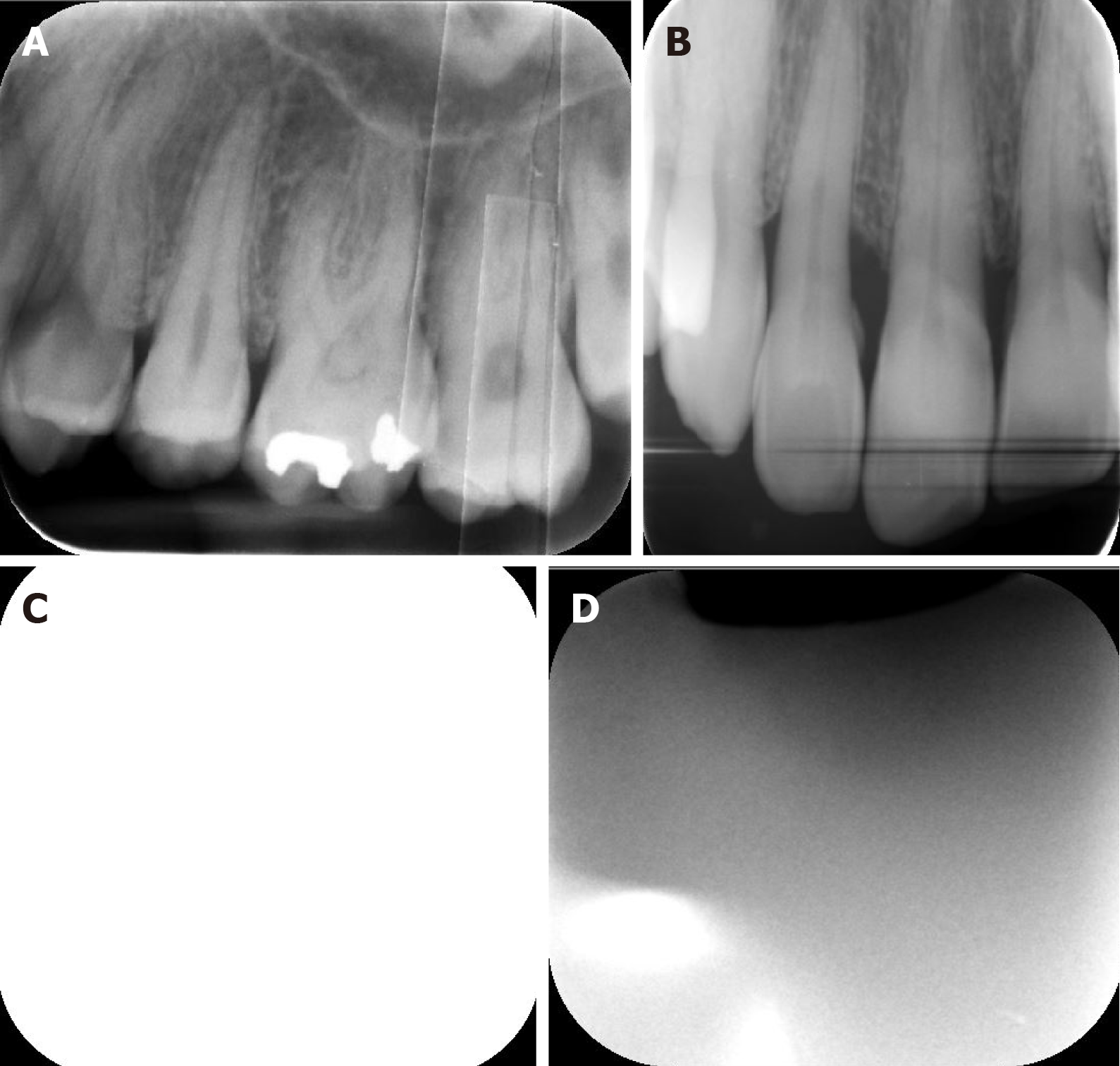
The cone cut was the most common error observed in 988 images (39.5%) out of 3550 images (Figure 1A), followed by the artifacts of improper PSP placement in the mouth (30.4%), projection geometry (22.4%), unexposed plate (4.5%), movement of phosphor plate in the disposable pocket (1.6%) (Figure 1A and B), reversed image (0.8%) (Figure 1c and d), overexposed (0.6%), and plate bending (0.3%).
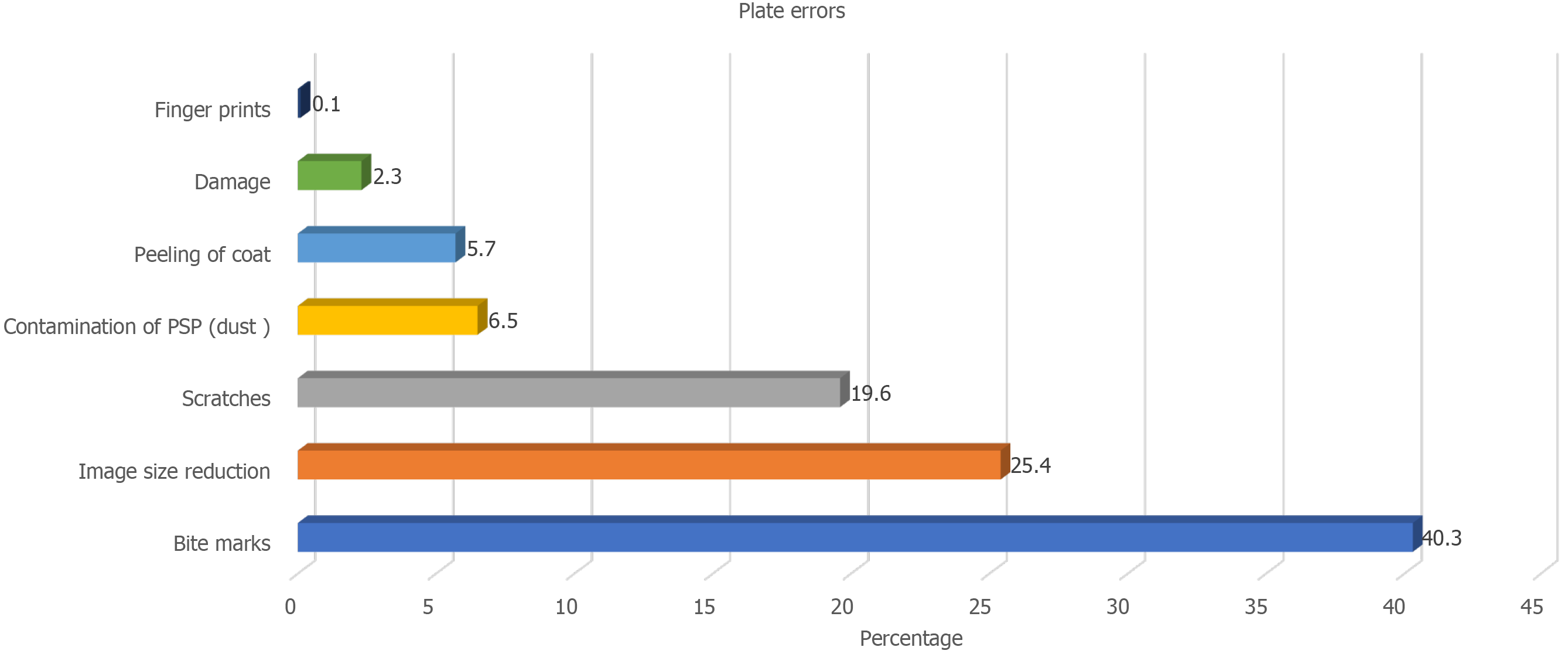
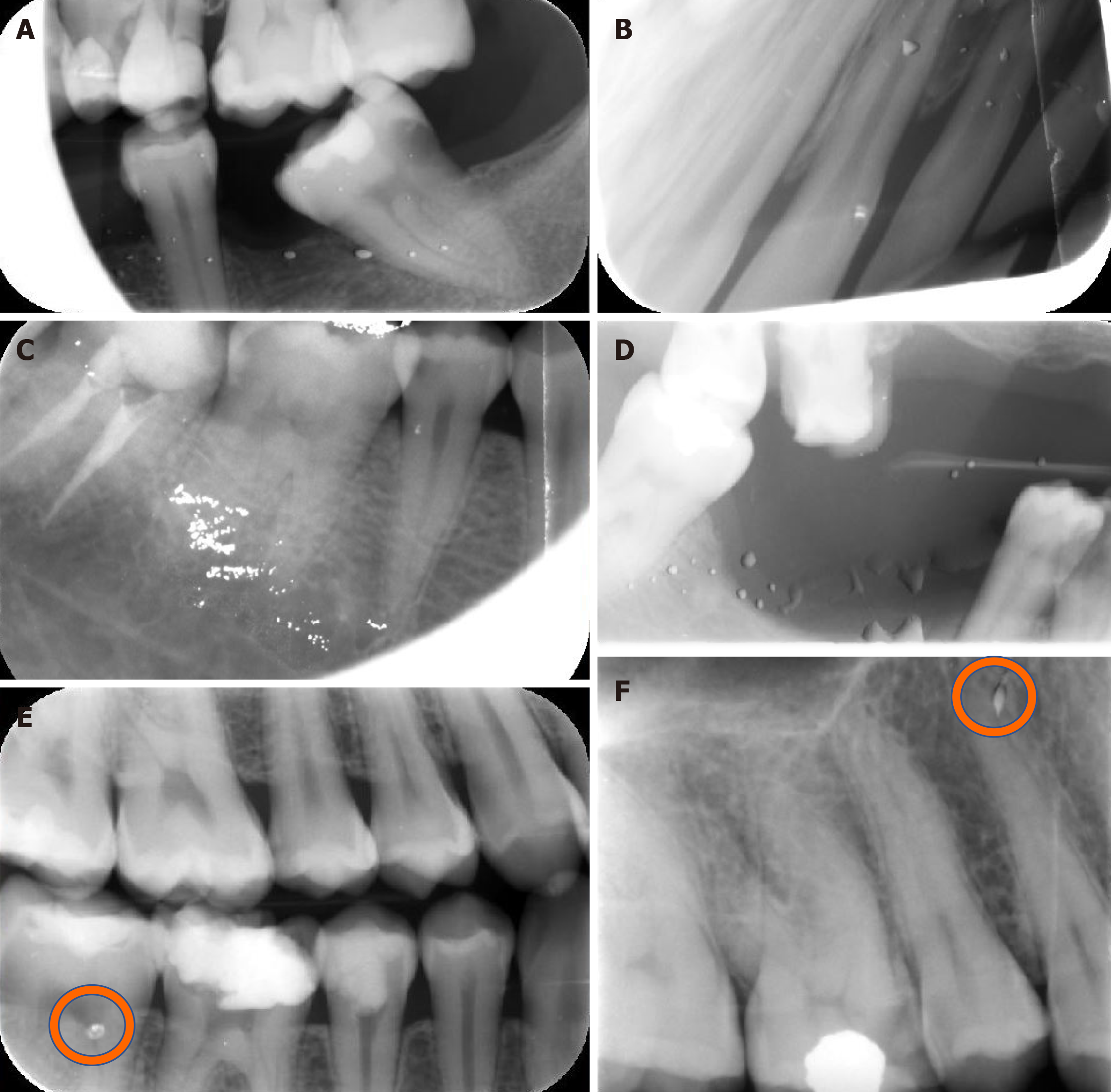
Bite marks were the most common error observed in 276 images (40.3%), while image size reduction was detected in 174 images (25.4%). In addition, plate scratches were detected in 19.6% of cases, with other errors being contamination of PSP (6.5%), peeling of the coat (5.7%), plate damage (2.3%), and fingerprints (0.1%)(Figures 2, 3 and 4).
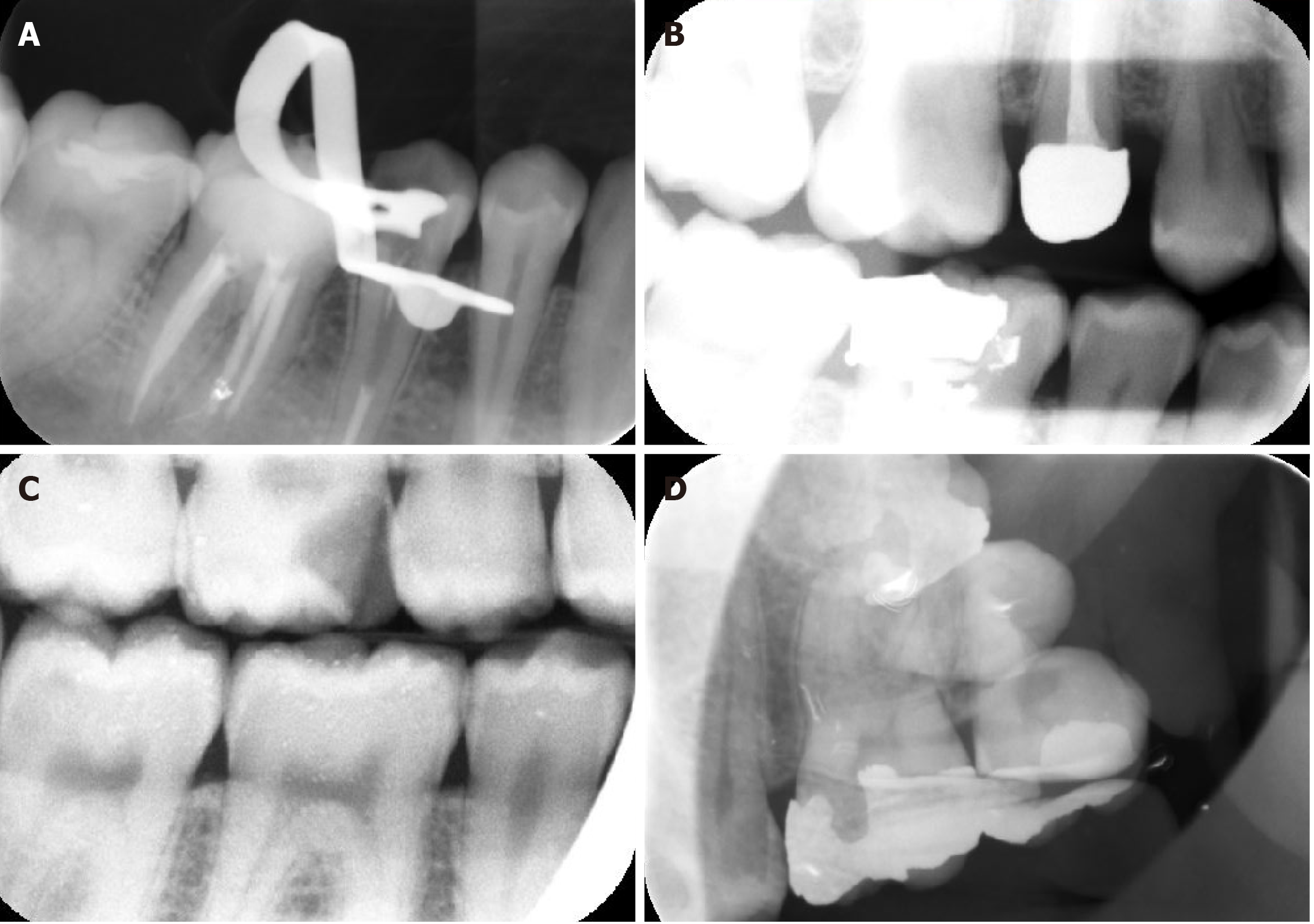
Delayed scanning artifacts (non-uniform density or bright image) were the most common errors observed in 145 images (39.9%). White (radiopaque) lines (37.2%), blank images (13.4%), black (radiolucent) lines (5.5%), and double images (incomplete or partial erasing) (4.1%) were also seen. (Table 1, Figures 5 and 6).
| Subtype | Frequency | Percent |
| Delayed scanning | 145 | 39.9 |
| White lines | 136 | 37.2 |
| Blank | 49 | 13.4 |
| Black lines | 20 | 5.5 |
| Double image | 15 | 4.1 |
| Total | 365 | 100 |
Digital intraoral imaging systems have gradually replaced film-based imaging in recent years, as this technology has many advantages over conventional imaging. Two types of receptors are used for digital intraoral radiography: solid-state sensors of either CCD or CMOS, which are used with a wire and PSP plates that are cordless. Solid‐state sensors have been used for more than two decades, while systems that use PSP plates have only recently been used in clinical practice. Each receptor type has its own advantages and disadvantages[2].
PSP and CCD digital systems are preferred over traditional films because of the lower radiation dose for both patients and operators, less time needed, ability to perform image manipulation as well as enhancement without the need for retake, better archiving, and environmental friendliness.
PSP plates are more comfortable to the patient than CCD because they are cordless, more flexible, and thin, which resembles standard films. However, despite their superiority, PSP plates are more susceptible to bending and scratches, require more time for scanning, and subsequently develop more image artifacts, which consequently affects image quality[15]. In previous studies, it has been stated that 95% of PSP plates used for 10 wk (used approximately 50 times) became non-diagnostic and needed to be substituted[16,17].
Radiographic artifacts that occur with plain film radiography are well-identified and documented. However, to the best of our knowledge, few studies have reported and categorized the artifacts of PSP plates[17-21]. Most of these studies investigated them in medical radiology; however, very few studies were correlated to the dental field[14,15,20,22].
Moreover, to reduce the radiation exposure of the patient, it is clinically important to avoid the occurrence of image artifacts in order to minimize repeated radiographs, which could happen through proper understanding of the reasons and solutions for incidence of image artifacts and thus lessen its frequency, especially in the recent commonly used dental digital imaging technology[14].
Therefore, the aim of this study was to detect the type, frequency, and reasons for the occurrence of intraoral image artifacts acquired by PSP plates in our dental clinics, and to propose probable methods to avoid these image artifacts.
In the present study, the examined intraoral radiographic errors were categorized into three main categories: operator, plate, and scanning errors. Operator errors were the most common and were observed in 2500 out of 50000 intraoral images (5%) and in 70% of 3550 retakes, which is in accordance with the findings of Hui-Lin Chiu et al[23] 2008. regarding the increased incidence of operator errors as seen in the current study. In addition, this reflects the need for broader training of radiology technicians.
In the present study, only 0.07% of 50000 intraoral images reported in the existing study presented with movement artifacts of the PSP plate inside the disposable packet. However, in Gulsahi and Secgin study in 2016, it was recorded frequently, whereas other studies did not report this type of artifact. It has been stated that this artifact is detected only with the Digora system, where both cardboard cover and disposable plastic envelopes should be used. While the cardboard cover is used to protect the PSP plates, they may unfortunately cause motion of the plates, resulting in these artifacts[24].
The second most common errors in the current study were plate errors that were detected in 685 intraoral images (1.37% of total images and 19.3% of retakes), followed by scanning errors seen in 365 intraoral images (0.73% of total images and 10.3% of retakes). Chiu et al[23] 2008 reported that scanning errors were the second most common error, followed by plate errors.
In the current study, bite marks were the most common plate error subtypes observed in 276 images (40.3%).
The most probable cause of the increased incidence of bitemarks in our study is the disposable plastic packet. It is used for infection control and acts as a light barrier, but it does not provide proper safety against plate damage from bite marks, bending, or pressure. Another possible reason for plate bitemarks would be the patient unintentionally biting on the plate. Thus, the patient must be comprehensively instructed to avoid doing so before the exposure.
It was reported that pediatric periapical radiographs of primary incisors that were taken by a modified technique by making the child bite on a size 2 PSP plate to keep it in place during exposure simulating occlusal radiograph could be one of the reasons for PSP bite marks. Snap-A ray film holding devices with teeth-like edges were used. Roberts, Mol, 2004 reported that the risk of teeth biting in pediatric primary incisors can be reduced by placing “adhesive backed sponge-like pads” on each side of the disposable sleeve that holds the reusable size 2 plate[2].
Image size reduction artifact after scanning was reported in 174 images (25.4% of retakes) and 0.3% of all intraoral images, which can be related to scanning errors. This was also reported by various studies[20].
In the present study, PSP plate scratches were detected in 19.6% of patients, while surface contamination of PSP was seen in 6.5%. To the best of our knowledge, the actual reasons for plate surface contamination and scratches have not been completely recognized and investigated. Kalathingal et al[17] 2010 stated that the possible cause of plate surface contamination could be the adhesive utilized in the barrier sheath, which could have affected the plate before scanning. The same study found that the plates that were used in dental colleges, as in our study, were more susceptible to scratches because of the increased number of people handling the plate, especially when they were discovered after scanning and before packaging the plate with a new protective sheath. Also, Kalathingal et al[17] 2010 reported that the hard rubbing of PSP plates with alcohol could be a cause for more scratches, and recommended that only the plates with visible surface contamination should be lightly wiped to remove any contaminants[17].
In the current study, peeling of the coat was found in 5.7%, plate damage was recorded in 2.3%, and fingerprints were found in 0.1% of plates. These findings were in the line with those reported by Gulsahi and Secgin in 2016, wherein they found damaged plates to occur in only a few images[20]. The most probable causes of plate damage are tough handling of PSP plates during their placement in the mouth, extensive bending, forceful placement of the plate into the scanner, or mechanical stresses exerted by the scanner roller during scanning[15].
Scanning errors were detected in 365 images (0.73% of all intraoral images), where delayed scanning was the most common error in this type and was seen in 145 images (0.29%). Despite Gulsahi and Secgin[24] reporting 12.6% of all images exhibited non-uniform brightness in their 2016 study, Chiu et al[23] recorded 0.4% delayed scanning errors in their 2008 study.
Although PSP plates can be exposed to regular light while being uncovered and imported into the scanner, it is recommended that exposure to regular light should not exceed 10 minutes, and that the scanning procedure should not be delayed more than that. Otherwise, the information in the plate will fade away[24], which will lead to increased signal loss and a reduction in the signal-to-noise ratio[25,26]. It could appear as total image fading with too bright an image or non-uniform image density caused by partial exposure of PSP to excessive ambient light before scanning. In addition, fluctuating signal loss leads to a noisy image[24].
In the current study, the most common subtype of scanning error was delayed scanning (39.9% of retakes), which was comparable to the results of Çalışkan and Sumer in their study in 2017, who affirmed that the probable cause for this artifact is the elimination of the plate from its cover after radiation exposure to inhibit infection before scanning[24].
It has been reported that the higher the light intensity and the longer the exposure time, the greater the loss of plate information[27]. This was supported by the study of Ang DB in 2006, which reported that plates were not exposed to any light before scanning presented no change in image quality even after many days of storage[25,28].
The second scanning error was the presence of white lines in 136 images (37.2%), which were reported to be due to dust or dirt particles on the slim scanning opening of the scanner. This caused them to remain fixed during the scanning process or dirt on the rollers, which acted as a blockage to the laser light. Thus, resulting in production of areas devoid of signals. Therefore, the mechanical scanner transport system should be checked and cleaned regularly, with additional replacement of the belt, if necessary[15].
The black or radiolucent lines that were detected in 20 images (5.5%) were hypothesized by a previous study to have resulted from electromagnetic interfering artifacts that were caused by anything that interfered, interrupted, decreased, or limited efficient scanner performance[15,29].
Moreover, Çalışkan A and Sumer AP[26] denoted this artifact as a ridging artifact, and advocated that these black lines occurred due to fast variations in the intensity of the light of the stimulating lasers as well as the loss of harmonization between rapid scan cycles and image plate movement. It is recommended to add proper electromagnetic shielding, appropriate voltage supply, uninterrupted power supply, and regular maintenance of scanner performance to avoid the occurrence of artifacts in radiolucent lines[15].
The previously mentioned errors observed in our study could be limited by proper regular orientation and enforcement by all operators, technicians, and students of the appropriate procedures of gentle handling of the PSP plates during exposure, scanning, and after scanning. This also includes focusing on the correct light rubbing of the PSP plates only with visible surface contamination to increase their longevity and usability. Moreover, regular checkups of PSP plates should be regularly performed to check the integrity of the plates. In addition, periodic maintenance, cleaning, and calibration of scanning devices would significantly reduce the number of scanning errors. Furthermore, additional comprehensive training of radiology technicians regarding application of proper radiographic techniques using the PSP system would be very beneficial in reducing operator errors.
The use of digital imaging in dental practice has recently made a revolution in image recording and analysis. Our institution made a significant modification by digitizing all dental images recently acquired using mainly the PSP system. Our study investigated the prevalence of intraoral image artifacts in our clinics, which were characteristic of PSP plates wherein the most common artifacts were bitemarks, image size reduction, scratches, and delayed scanning. Defining the causes of these artifacts and identifying methods for preventing them are of great clinical significance. Further research on PSP artifacts for further error identification and proper handling is needed and is a process that is essential to produce superior diagnostic images needed for instituting proper dental care.
Nowadays, digital imaging outweighs conventional imaging and has been used widely in dentistry. Digital radiography allows image manipulation to adjust the visual characteristics of the image, such as contrast, brightness, and density, thus enhancing image quality without the need to retake the image.
Digital imaging provides an easier, comfortable, and user-friendly way for recording and interpreting radiographic data for archiving and teleradiography.
To detect the frequency, type, and reasons behind the appearance of intraoral image artifacts acquired by photostimulable phosphor plates (PSP).
This retrospective descriptive study. A total of 50000 intraoral radiographs were retrieved from the clinical database from April 2018 to April 2020 to evaluate the reason, type, and solutions to these image artifacts.All intraoral digital radiographs were acquired using an intraoral X-ray machine with 7 -mA, 65-kVP using a PSP system and laser scanners, which can house all sizes of reusable intraoral PSP sensor plates with image acquisition software.
Imaging artifacts were divided into three categories; operator, plate, and scanning errors. Out of 3550 retakes, 5%, 1.37%, and 0.73% were related to the operator, plate, and scanning errors, respectively. The cone cut was the most common operator error (988 images), Bite marks were the most common plate error (276 images), and delayed scanning artifacts were the most common scanning errors (145 images).
Our study discussed intraoral image artifacts that were characteristic of PSP, where the most common artifacts were bitemarks, image size reduction, scratches, and delayed scanning.
Thus, recognizing intraoral radiographic image errors and defining the causes and their trouble-shooting are crucial factors in making images possess great clinical impacts.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership in Professional Societies: American Academy of Oral Medicine.
Specialty type: Medicine, research and experimental
Country/Territory of origin: Saudi Arabia
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Aoun G S-Editor: Wang LL L-Editor: A P-Editor: Wang LL
| 1. | White SC, Pharoah MJ. White and pharoah’s oral radiology: principles and interpretation. 8th edition. St. Louis: Elsevier Health Sciences, 2019: 40-60. |
| 2. | Roberts MW, Mol A. Clinical techniques to reduce sensor plate damage in PSP digital radiography. J Dent Child (Chic). 2004;71:169-170. [PubMed] |
| 3. | Malleshi SN, V G M, Raina A, Patil K. A Subjective Assessment of Perceived Clarity of Indirect Digital Images and Processed Digital Images with Conventional Intra-oral Periapical Radiographs. J Clin Diagn Res. 2013;7:1793-1796. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 4. | Ludlow JB MA. Digital imaging. In: White SC, Pharoah MJ, editors. Oral Radiology: Principles and Interpretation. St. Louis, Missouri: Mosby, Elsevier, 2014: 41-62. |
| 5. | Berkhout WE, Sanderink GC, Van der Stelt PF. A comparison of digital and film radiography in Dutch dental practices assessed by questionnaire. Dentomaxillofac Radiol. 2002;31:93-99. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 26] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Wenzel A, Møystad A. Work flow with digital intraoral radiography: a systematic review. Acta Odontol Scand. 2010;68:106-114. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 86] [Cited by in RCA: 72] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 7. | Ajmal M, Elshinawy MI. Subjective image quality comparison between two digital dental radiographic systems and conventional dental film. Saudi Dent J. 2014;26:145-150. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 8. | van der Stelt PF. Better imaging: the advantages of digital radiography. J Am Dent Assoc. 2008;139 Suppl:7S-13S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 57] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 9. | Parks ET, Williamson GF. Digital radiography: an overview. J Contemp Dent Pract. 2002;3:23-39. [PubMed] |
| 10. | Chiu HL, Wei YW, Wang WC, Chen YK. Simple and effective methods to protect the photostimulable phosphor storage plate sensor. J Dent Sci. 2018;13:85-86. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 11. | Macdonald R. Digital imaging for dentists. Aust Dent J. 2001;46:301-305. [DOI] [Full Text] |
| 12. | Kitagawa H, Farman AG, Scheetz JP, Brown WP, Lewis J, Benefiel M. Comparison of three intra-oral storage phosphor systems using subjective image quality. Dentomaxillofac Radiol. 2000;29:272-276. [RCA] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 13. | Borg E. Some characteristics of solid-state and photo-stimulable phosphor detectors for intra-oral radiography. Swed Dent J Suppl. 1999;139:i-viii, 1. [PubMed] |
| 14. | Hildebolt CF, Couture RA, Whiting BR. Dental photostimulable phosphor radiography. Dent Clin North Am. 2000;44:273-297, vi. [PubMed] |
| 15. | Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37:360-363. [PubMed] |
| 16. | Deniz Y, Kaya S. Determination and classification of intraoral phosphor storage plate artifacts and errors. Imaging Sci Dent. 2019;49:219-228. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 17. | Kalathingal SM, Shrout MK, Comer C, Brady C. Rating the extent of surface scratches on photostimulable storage phosphor plates in a dental school environment. Dentomaxillofac Radiol. 2010;39:179-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Shetty CM, Barthur A, Kambadakone A, Narayanan N, Kv R. Computed radiography image artifacts revisited. AJR Am J Roentgenol. 2011;196:W37-W47. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 19] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 19. | Oestmann JW, Prokop M, Schaefer CM, Galanski M. Hardware and software artifacts in storage phosphor radiography. Radiographics. 1991;11:795-805. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 28] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 20. | Willis CE, Thompson SK SS. Artifacts and misadventures in digital radiography. Appl Radiol. 2004;33:11-21. |
| 21. | Cesar LJ, Schueler BA, Zink FE, Daly TR, Taubel JP, Jorgenson LL. Artefacts found in computed radiography. Br J Radiol. 2001;74:195-202. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 20] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 22. | Bedard A, Davis TD, Angelopoulos C. Storage phosphor plates: how durable are they as a digital dental radiographic system? J Contemp Dent Pract. 2004;5:57-69. [PubMed] |
| 23. | Chiu HL, Lin SH, Chen CH, Wang WC, Chen JY, Chen YK, Lin LM. Analysis of photostimulable phosphor plate image artifacts in an oral and maxillofacial radiology department. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106:749-756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 24. | Gulsahi A, Secgin CK. Assessment of intraoral image artifacts related to photostimulable phosphor plates in a dentomaxillofacial radiology department. Niger J Clin Pract. 2016;19:248-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 25. | Akdeniz BG, Gröndahl HG, Kose T. Effect of delayed scanning of storage phosphor plates. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;99:603-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 26. | Çalışkan A, Sumer AP. Definition, classification and retrospective analysis of photostimulable phosphor image artefacts and errors in intraoral dental radiography. Dentomaxillofac Radiol. 2017;46:20160188. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 27. | Ramamurthy R, Canning CF, Scheetz JP, Farman AG. Impact of ambient lighting intensity and duration on the signal-to-noise ratio of images from photostimulable phosphor plates processed using DenOptix and ScanX systems. Dentomaxillofac Radiol. 2004;33:307-311. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 23] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 28. | Ang DB, Angelopoulos C, Katz JO. How does signal fade on photo-stimulable storage phosphor imaging plates when scanned with a delay and what is the effect on image quality? Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:673-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 18] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 29. | Seeram E. Computed radiography: physics and technology. In: Digital radiography. Singapore: Springer, 2019: 41-63. |