Published online Jul 6, 2022. doi: 10.12998/wjcc.v10.i19.6341
Peer-review started: January 8, 2022
First decision: March 9, 2022
Revised: March 17, 2022
Accepted: May 5, 2022
Article in press: May 5, 2022
Published online: July 6, 2022
Processing time: 166 Days and 21.9 Hours
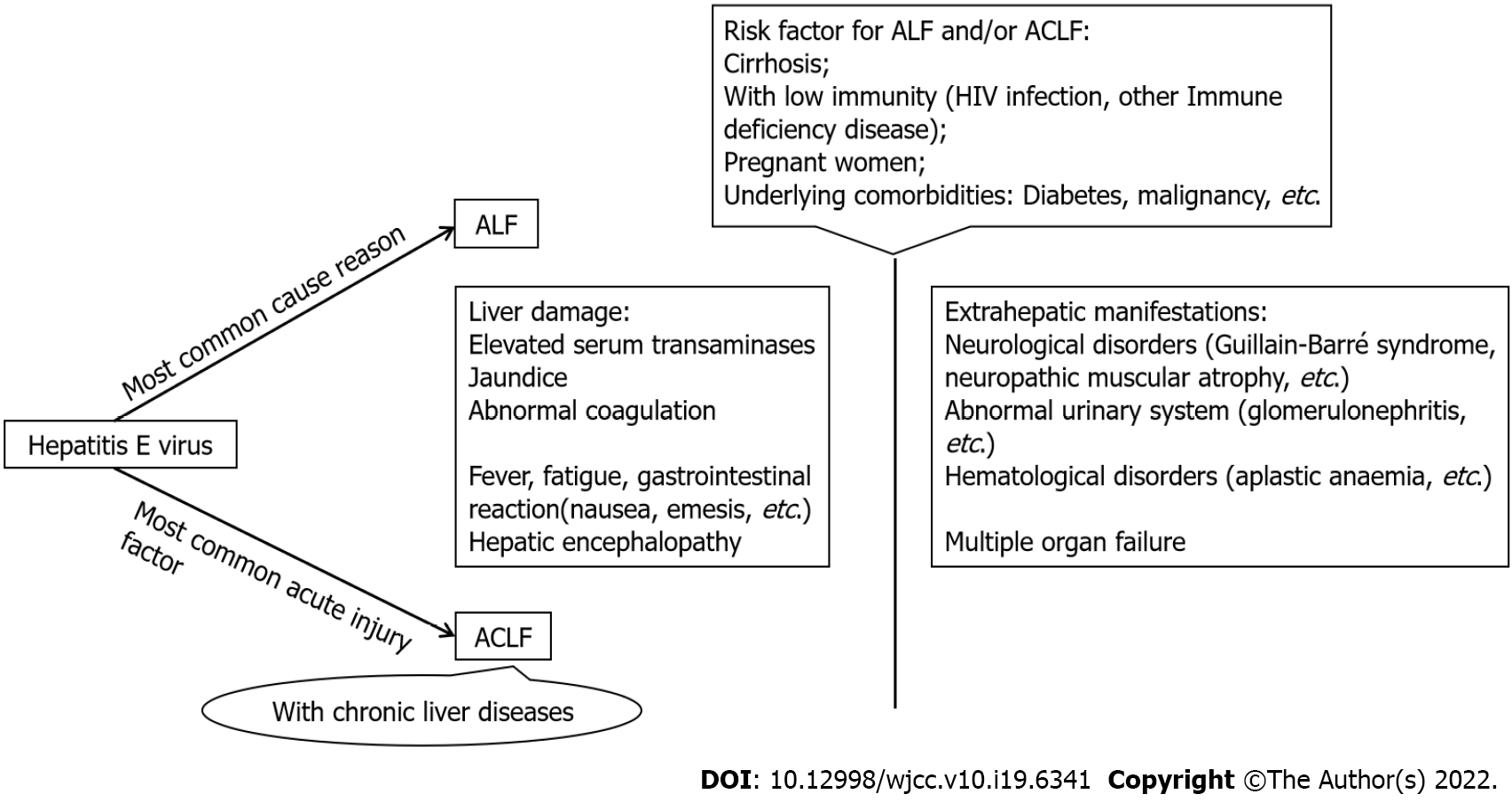
Hepatitis E virus (HEV) is the most common cause of acute liver failure (LF) and one of the most common factors causing acute injury in acute-on-chronic LF (ACLF). When HEV-related LF occurs, a series of changes take place in both the intrahepatic environment and extrahepatic microenvironment. The changed types and distribution of immune cells (infiltrating macrophages and increased lymphocytes) in liver tissue, as well the increased proinflammatory cytokines and chemokines in the blood, indicate that the occurrence and progression of HEV-related LF are closely related to immune imbalance. The clinical features and immune reaction in the body during HEV-related acute LF (ALF) and ACLF are complicated. This review highlights recent progress in elucidating the clinical manifestations of HEV-associated ALF and ACLF and discusses the corresponding systemic immune changes and possible regulatory mechanisms.
Core Tip: Hepatitis E virus (HEV) is the most common cause of acute liver failure (LF) and a common factor causing acute injury in acute-on-chronic LF (ACLF). The whole immune environment in the body during HEV-related LF is complicated. This review highlights recent progress in elucidating the clinical manifestations of HEV-associated acute LF and ACLF and discusses the corresponding systemic immune changes and possible regulatory mechanisms.
- Citation: Chen C, Zhang SY, Chen L. Review of clinical characteristics, immune responses and regulatory mechanisms of hepatitis E-associated liver failure. World J Clin Cases 2022; 10(19): 6341-6348
- URL: https://www.wjgnet.com/2307-8960/full/v10/i19/6341.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v10.i19.6341
The threat to public health from hepatitis virus-associated liver failure (LF) is serious[1,2]. Global epidemiological surveys have shown that hepatitis E virus (HEV) is the most common cause of acute LF (ALF) and one of the most common factors causing acute injury in acute-on-chronic LF (ACLF)[1,3]. HEV infection can develop into severe hepatitis in patients with underlying chronic liver disease (CLD), underlying comorbidities or altered immune responses, such as in pregnant women[4-6].
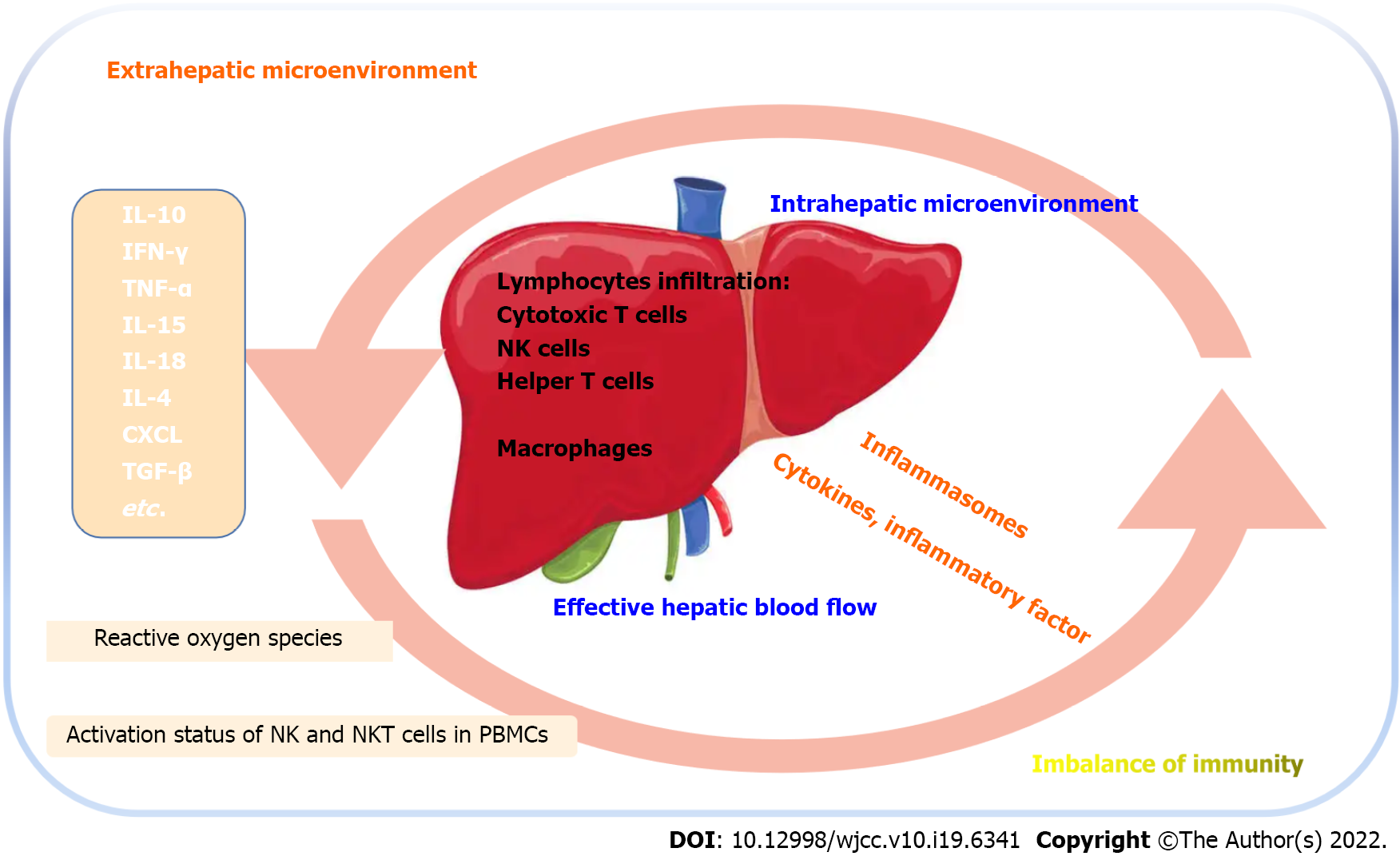
HEV infection can show symptoms of acute viral hepatitis and abnormal function of extrahepatic organs. According to international standards, coagulopathy, elevated serum transaminase, abnormal bilirubin and altered consciousness level are important indicators to judge LF[3,7]. When LF occurs, a series of changes take place in both the intrahepatic environment and extrahepatic microenvironment, which is actually a systemic disease response. The etiology of the systemic response to HEV-associated LF has not been well established, although many studies have shown that dysregulation of immune responses is the key factor driving the occurrence of HEV-associated LF[8-10]. The changed numbers of monocyte-macrophage cells and dendritic cells and increased proinflammatory cytokines [interferon (IFN)-γ, tumor necrosis factor (TNF)-α, interleukin (IL)-10, IL-18] in blood among HEV patients correlated with adverse outcomes. In addition, inflammasome activation in macrophages shows that immune response plays an important role in the development of HEV-associated LF[9,11,12], although the exact pathogenesis remains to be clarified.
This review aims to summarize data on the investigations of HEV-associated LF in an attempt to understand the incidence and clinical characteristics of the disease and most importantly to understand the corresponding systemic immune changes and regulatory mechanisms to facilitate control of the disease.
People infected by HEV manifest from subclinical infection to uncomplicated acute viral hepatitis and even severe fulminant LF[4,13]. In an individual without underlying CLD, a syndrome characterized by markers of liver damage (elevated serum transaminases), impaired liver function (jaundice and international normalized ratio > 1.5) and new hepatic encephalopathy is defined as ALF[14]. The Clinical Practice Guidelines produced by the European Association for the Study of the Liver state that hepatic viruses including hepatitis B virus, hepatitis A virus and HEV can cause ALF. The guidelines suggest that hepatitis B virus-associated ALF has higher mortality than hepatitis A virus and HEV-associated ALF. Nonetheless, the incidence of HEV-associated ALF is higher, suggesting the need for serological screening for HEV infection[14]. A systematic review by Patterson et al[1] analyzed the global epidemiology of virus-induced ALF. The 25 relevant studies published between 2009 and 2019 showed that the prevalence of HEV-induced ALF was 3%–70%. The high rate of ALF among pregnant women reported in previous studies was related to HEV[6,15], which likewise suggested the necessity to increase attention and extend the use of the hepatitis E vaccine (Figure 1).
Classically, HEV-associated ALF presents as an initial prodromal phase with symptoms of fever, fatigue and nausea. Then, jaundice and dark urine occur, and alanine transaminase and aspartate aminotransferase increase. Increased bilirubin level, sharply deteriorating coagulation and different degrees of hepatic encephalopathy are the most important features of HEV-associated ALF[14]. In addition, along with symptoms of acute liver deterioration, neurological disorders (Guillain–Barré syndrome and neuropathic muscular atrophy were most reported), abnormal urinary system (particularly glomerulonephritis) and hematological disorders (HEV-associated ALF combined with aplastic anemia) are increasingly recognized by clinicians[16-19].
We consider that the most important extrahepatic manifestations caused by HEV may be neurological (myelitis, myositis, bilateral peripheral facial paralysis, acute uniphasic brachial plexus disease). They have a high incidence (5%–30%) and serious clinical impact[16,20]. Yet, to facilitate the diagnosis and prediction of the HEV-associated LF, many researchers also suggest kidney function as a predictor. Elevated urea nitrogen is closely related to the occurrence and progression of HEV-related LF and plays an important role in clinical prognosis[21]. All the above information indicates that HEV-associated ALF is not a single organ injury but a systemic condition. Moreover, the involvement and deterioration of the extrahepatic systems accelerate disease progression and increases the mortality rate of HEV-associated ALF. Therefore, to better monitor the changes in the disease, apart from more frequent detection of liver enzyme indicators, bilirubin, coagulation profile and conscious state, there is a need to assess other systemic indicators, such as peripheral hemogram, electrolyte testing, arterial pH, creatinine clearance rate, etc[4,22].
ACLF is typically related to a precipitating event among patients with CLDs, such as acute liver damage or acute exacerbation of CLD. Although the definitions of ACLF from the Asia Pacific Association for the Study of the Liver, European Association for the Study of the Liver and American Association for the Study of Liver Diseases have some differences, the consensus is that of deterioration of liver function with high mortality for ACLF[7,23,24].
We know that there are significant differences in epidemic areas and disease characteristics among different HEV genotypes. The spectrum of CLDs also varies by region, such as chronic viral hepatitis is endemic in Asia, especially India, while alcoholic liver disease and fatty liver dominate in Europe and the Americas. The above factors result in different clinical manifestations of HEV-related ACLF in different countries and regions. There is significant controversy on the impact of HEV genotypes 3 and 4 in ACLF. In Europe and the Americas, the effect of HEV genotypes 3 and 4 on CLDs was observed to be limited, with low rates of liver decompensation and ACLF[25], while the occurrence in Asia can be up to 60%[5,26]. Furthermore, irrespective of the incidence rate of ACLF caused by HEV, the mortality of HEV-related ACLF was lower compared to alcohol-related ACLF and other forms of ACLF[27]. Generally, organ failure is the final progression of ACLF and determines the outcome of patients. Previous studies showed that the rates of renal failure, circulatory failure and respiratory failure in HEV-related ACLF were lower than those of other acute trigger factors, such as alcohol, hepatitis B virus and cryptogenic elements[27,28]. Does it means that despite HEV-related ACLF having a higher incidence, it appears to have a better clinical outcome than ACLF triggered by other acute factors? We think that more clinical data are needed to explore this further.
The differences in clinical presentations and outcomes among HEV-related ACLF patients are also due to prior body status. First, the functional status of hepatocytes in patients with different underlying CLDs is not the same. Our previous studies have shown a significantly higher mortality rate in patients with cirrhosis[5,29,30]. Second, some underlying comorbidities[5], such as diabetes, nephritis, chronic respiratory diseases and malignancy, particularly hematological malignancy (data from virology departments across nine NHS health boards in Scotland[31]), are significant predictors of mortality. Some laboratory tests (higher aspartate aminotransferase, lactate dehydrogenase and a-fetoprotein and lower triglyceride) can also provide some clues to identify the occurrence and prognosis of HEV-related ACLF and help tailor effective prevention. More attention to the above at-risk groups is essential. We believe that more precise and effective anti-HEV vaccination of at-risk populations is necessary and urgent.
It is well known that HEV infections are mostly self-limiting diseases and immune-capable individuals usually can eliminate the virus spontaneously[4,13]. Otherwise, infected persons with low immunity can develop acute viral hepatitis, leading to chronic infection, extrahepatic symptoms and even LF. Previous studies have shown that the host immune response, rather than the virus itself, is the driving factor for the occurrence of HEV-associated LF[32]. The gene expression profile of liver biopsy in HEV-infected LF patients shows that there are many upregulated and downregulated genes in liver tissue compared to normal liver tissue, and most of these differentially expressed genes are related to immunity[33]. What interaction is there between the virus and host immunity? In particular, what is the specific immune response when HEV-related LF occurs? Past studies may give us several clues (Figure 2).
The immune response process includes immune cell proliferation, differentiation of antigen recognition activation and production of immune substances with specific effects. This process is a comprehensive reflection of the functions of various parts of the immune system. During the process, the antigen-presented lymphocytes activate immune molecules to form a series of physiological reactions and immunological effects. The types and distribution of immune cells differ in patients with LF compared to normal subjects[8,34]. Intrahepatic immune cell count, especially lymphocytes, is many times more than in non-LF populations, which suggests that lymphocytes infiltration is one of the characteristic immune reactions of LF[8].
Wu et al[10] showed that the Th1/Th2 cytokine levels among acute hepatitis E patients, HEV-associated ALF patients and controls were significantly different. Th2 bias (IFN-γ/IL-4) was observed particularly among acute hepatitis E and HEV-associated ALF patients, which infers that hepatocyte damage was aggravated by the persistent imbalance of cellular immunity. The levels of cytotoxic T cells, such as CD3 and CD8 cells, were higher in HEV-infected liver tissues compared to healthy liver tissues. The numbers of natural killer (NK) cells (CD56) and helper T cells (CD4) also differed significantly between the two tissues[34]. NK cells are the main component of liver lymphocytes and play a role in killing hepatotropic viruses. When HEV and other hepatotropic viruses infect the liver, NK cells can be activated by a signaling factor and produce cytokines to exert further immune effects[35]. Importantly, intrahepatic lymphocytes (CD4+ T cells, CD8+ T cells and NK cells) among ACLF patients have significantly increased counts compared with those in healthy individuals[34,35].
Although the pathogenesis of ACLF is not fully elucidated, the differences in lymphocyte counts suggest that cellular immunity is involved in progression of the disease. In vitro and in vivo experiments showed that the number of inflammatory macrophages in a model of drug-induced ALF were significantly increased, which finally resulted in severe liver injury[36,37]. In conclusion, the difference in lymphocyte distribution in liver tissue is important in LF caused by various agents.
Different types of lymphocytes play different roles in immunoreactions. Immune monitoring mechanisms have advantages and disadvantages. NK cells act as sentinels and “vanguard troops” in the first step of battling against viral infection[35]. NK cells and differentiated NKT cells can be recruited by several cytokines from the peripheral blood and infiltrate the liver, participating in both fighting against HEV and impairing liver cells[38]. Through analysis of the frequency and activation status of NK and NKT cells in peripheral blood mononuclear cells, Srivastava et al[35] found that HEV-infected patients had higher numbers of cells in an activated state. The expression of NK group 2A (inhibitory receptor) on peripheral blood NK cells plays a pivotal negative regulatory role in the progression of hepatitis virus-associated ACLF[39]. In vivo and in vitro experiments have confirmed that NK group 2D (activating receptor) participates in aggravating liver inflammation (elevated level of IFN-γ and TNF-α) by activating NK cells[40]. The reciprocal action from above inhibitory and activating receptors regulates the function of NK cells and plays an important role in the progression of hepatitis virus-related ALF and ACLF.
Another important lymphocyte involved in HEV-associated LF is cytotoxic T cells. Although cytotoxic T cells differentiating from CD8+ T cells (which are promoted by CD4+ T cells) can directly kill HEV, they can also cause liver cell damage[8]. Innate and adaptive immune responses also depend on monocytes and macrophages recognizing pathogens to mediate phagocytosis. When HEV invades the liver, reactive oxygen species and TNF-α were activated and produced by infiltrated macrophages, which can exacerbate local inflammation of the liver and promote the development of LF while fighting the virus[10]. These studies have suggested that the occurrence and progression of HEV-related LF are closely related to the immune response, which acts as a double-edged sword in fighting against HEV infection.
Cytokines are small molecular proteins with extensive biological activities synthesized and secreted by immune cells (such as monocytes, macrophages, T cells, B cells and NK cells) and some nonimmune cells (such as endothelial cells, epidermal cells and fibroblasts) through stimulation. Cytokines can regulate cell growth and differentiation and promote an immune response by binding corresponding receptors[32,41]. Markers called inflammasomes act as a hallmark when inflammation occurs[42]. Inflammasomes are like sensors that act as a bridge between pathogens and cytokines and inflammatory factors in the pathogenesis and progression of many inflammatory diseases. A recent study reported the critical role of an important inflammasome (NLRP3) in HEV infection, which can be activated by macrophages and then further regulate host defense. Further research suggests that therapeutic targeting of NLRP3 could benefit treatment of HEV-associated severe liver disease[9].
Several previous studies on cytokines during the pathogenesis of liver injury have shown that many cytokines (including IL-15, IL-18, CXCR3, granzyme B, CXCL8, CXCL9 and CXCL10) promote chemotaxis of immune cells to liver tissue[43], like the migration of NK cells, CD8+ T cells, monocytes and macrophages described above. On the one hand, infiltration of macrophages in liver tissue is one of the main causes of severe liver injury due to excessive production of TNF-α, which can result in liver inflammation and even liver LF. On the other hand, inhibitory cytokines such as IL-10 and transforming growth factor-β also play an important role in the process of dysfunction and inactivation of the immune system. Impaired phagocytosis of monocytes and macrophages as well as the release of cytokines can result in inefficient treatment of HEV infection, which may advance liver deterioration toward LF[10].
IFN-γ is an effector molecule produced by various types of cells and is one of the most important factors in the process of HEV infection. In general, IFN-γ kills infected liver cells and causes liver damage by promoting the differentiation of CD8+ T cells into cytotoxic T cells, as well as helping to clear HEV[43]. In this process, its specific immune function is essentially a double-edged sword. On the one hand, it plays the role of virus removal. On the other hand, it can cause serious liver damage and even LF. Immune-inflammation response is the most important process against virus infection, which is also a balance between proinflammatory and anti-inflammatory immunity. The level of proinflammatory cytokines (IFN-γ and TNF-α) in the liver of HEV-related ACLF patients was significantly higher than that of normal subjects, while the expression of anti-inflammatory cytokines (IL-10) was not different between the two groups[10]. This suggests that the imbalance between the expression of proinflammatory and anti-inflammatory cytokines may be an important immune mechanism during the pathogenesis of HEV-related ACLF.
Last but not least, the liver is an organ with abundant blood flow. Massive perfusion of blood promotes immune cell migration from peripheral blood to the liver[43,44]. Various cytokines can also travel through the blood vessels of the liver to the rest of the body to affect organ function. Monitoring changes in liver blood flow is also one of the means to evaluate the severity of liver disease. The effective hepatic blood flow is closely related to the severity of hepatitis virus-related ACLF[45]. Effective blood flow is not only a reflection of liver function but also a necessary channel for the connection between intrahepatic and extrahepatic environments. Increased migration of proinflammatory factors and chemokines from the liver to the extrahepatic environment plays an important role in HEV-related LF, and the poor outcome is ultimately the result of multiple organ failure.
Here, we have reviewed relevant studies to understand the clinical characteristics of HEV-associated LF and related immunological mechanisms. Overall, HEV is a common cause of ALF and the most common factor causing acute injury in ACLF. The whole immune environment in the body during HEV-related LF is complicated, which involves complex cellular and humoral immunity. We hope this review can develop a better understanding of the mechanism of HEV-related LF and may eventually lead to improved prevention, diagnosis and treatment of the disease.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Lu J, China; Sergi C, Canada S-Editor: Fan JR L-Editor: Filipodia P-Editor: Fan JR
| 1. | Patterson J, Hussey HS, Silal S, Goddard L, Setshedi M, Spearman W, Hussey GD, Kagina BM, Muloiwa R. Systematic review of the global epidemiology of viral-induced acute liver failure. BMJ Open. 2020;10:e037473. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 2. | Patterson J, Hussey HS, Abdullahi LH, Silal S, Goddard L, Setshedi M, Spearman W, Hussey GD, Kagina B, Muloiwa R. The global epidemiology of viral-induced acute liver failure: a systematic review protocol. BMJ Open. 2019;9:e029819. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 3. | Koch A, Trautwein C, Tacke F. [Acute liver failure]. Med Klin Intensivmed Notfmed. 2017;112:371-381. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 14] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Horvatits T, Schulze Zur Wiesch J, Lütgehetmann M, Lohse AW, Pischke S. The Clinical Perspective on Hepatitis E. Viruses. 2019;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 70] [Cited by in RCA: 79] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 5. | Zhang S, Chen C, Peng J, Li X, Zhang D, Yan J, Zhang Y, Lu C, Xun J, Li W, Ling Y, Huang Y, Chen L. Investigation of underlying comorbidities as risk factors for symptomatic human hepatitis E virus infection. Aliment Pharmacol Ther. 2017;45:701-713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Ma XX, Ji Y, Jin L, Baloch Z, Zhang DR, Wang Y, Pan Q, Ma Z. Prevalence and clinical features of hepatitis E virus infection in pregnant women: A large cohort study in Inner Mongolia, China. Clin Res Hepatol Gastroenterol. 2021;45:101536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 7. | Sarin SK, Choudhury A, Sharma MK, Maiwall R, Al Mahtab M, Rahman S, Saigal S, Saraf N, Soin AS, Devarbhavi H, Kim DJ, Dhiman RK, Duseja A, Taneja S, Eapen CE, Goel A, Ning Q, Chen T, Ma K, Duan Z, Yu C, Treeprasertsuk S, Hamid SS, Butt AS, Jafri W, Shukla A, Saraswat V, Tan SS, Sood A, Midha V, Goyal O, Ghazinyan H, Arora A, Hu J, Sahu M, Rao PN, Lee GH, Lim SG, Lesmana LA, Lesmana CR, Shah S, Prasad VGM, Payawal DA, Abbas Z, Dokmeci AK, Sollano JD, Carpio G, Shresta A, Lau GK, Fazal Karim M, Shiha G, Gani R, Kalista KF, Yuen MF, Alam S, Khanna R, Sood V, Lal BB, Pamecha V, Jindal A, Rajan V, Arora V, Yokosuka O, Niriella MA, Li H, Qi X, Tanaka A, Mochida S, Chaudhuri DR, Gane E, Win KM, Chen WT, Rela M, Kapoor D, Rastogi A, Kale P, Sharma CB, Bajpai M, Singh V, Premkumar M, Maharashi S, Olithselvan A, Philips CA, Srivastava A, Yachha SK, Wani ZA, Thapa BR, Saraya A, Shalimar, Kumar A, Wadhawan M, Gupta S, Madan K, Sakhuja P, Vij V, Sharma BC, Garg H, Garg V, Kalal C, Anand L, Vyas T, Mathur RP, Kumar G, Jain P, Pasupuleti SSR, Chawla YK, Chowdhury A, Song DS, Yang JM, Yoon EL; APASL ACLF Research Consortium (AARC) for APASL ACLF working Party. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific association for the study of the liver (APASL): an update. Hepatol Int. 2019;13:353-390. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 614] [Cited by in RCA: 587] [Article Influence: 97.8] [Reference Citation Analysis (0)] |
| 8. | Wu J, Ling B, Guo N, Zhai G, Li M, Guo Y. Immunological Manifestations of Hepatitis E-Associated Acute and Chronic Liver Failure and Its Regulatory Mechanisms. Front Med (Lausanne). 2021;8:725993. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Li Y, Yu P, Kessler AL, Shu J, Liu X, Liang Z, Liu J, Li Y, Li P, Wang L, Wang Y, Ma Z, Liu A, Bruno MJ, de Man RA, Peppelenbosch MP, Buschow SI, Pan Q. Hepatitis E virus infection activates NOD-like receptor family pyrin domain-containing 3 inflammasome antagonizing interferon response but therapeutically targetable. Hepatology. 2022;75:196-212. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 29] [Article Influence: 9.7] [Reference Citation Analysis (0)] |
| 10. | Wu J, Guo Y, Lu X, Huang F, Lv F, Wei D, Shang A, Yang J, Pan Q, Jiang B, Yu J, Cao H, Li L. Th1/Th2 Cells and Associated Cytokines in Acute Hepatitis E and Related Acute Liver Failure. J Immunol Res. 2020;2020:6027361. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 31] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 11. | Sehgal R, Patra S, David P, Vyas A, Khanam A, Hissar S, Gupta E, Kumar G, Kottilil S, Maiwall R, Sarin SK, Trehanpati N. Impaired monocyte-macrophage functions and defective Toll-like receptor signaling in hepatitis E virus-infected pregnant women with acute liver failure. Hepatology. 2015;62:1683-1696. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 53] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 12. | Debes JD, Groothuismink ZMA, Doukas M, de Man RA, Boonstra A. Immune dissociation during acute hepatitis E infection. Int J Infect Dis. 2019;87:39-42. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Kar P, Karna R. A Review of the Diagnosis and Management of Hepatitis E. Curr Treat Options Infect Dis. 2020;1-11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 26] [Cited by in RCA: 23] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 14. | European Association for the Study of the Liver; Clinical practice guidelines panel, Wendon, J; Panel members, Cordoba J, Dhawan A, Larsen FS, Manns M, Samuel D, Simpson KJ, Yaron I; EASL Governing Board representative, Bernardi M. EASL Clinical Practical Guidelines on the management of acute (fulminant) liver failure. J Hepatol. 2017;66:1047-1081. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 417] [Cited by in RCA: 616] [Article Influence: 77.0] [Reference Citation Analysis (1)] |
| 15. | Kar P, Sengupta A. A guide to the management of hepatitis E infection during pregnancy. Expert Rev Gastroenterol Hepatol. 2019;13:205-211. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 25] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 16. | Wu J, Xiang Z, Zhu C, Yao Y, Bortolanza M, Cao H, Li L. Extrahepatic manifestations related to hepatitis E virus infection and their triggering mechanisms. J Infect. 2021;83:298-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Rose MQ, Santos CD, Rubin DI, Siegel JL, Freeman WD. Guillain-Barré Syndrome After Acute Hepatitis E Infection: A Case Report and Literature Review. Crit Care Nurse. 2021;41:47-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Abravanel F, Pique J, Couturier E, Nicot F, Dimeglio C, Lhomme S, Chiabrando J, Saune K, Péron JM, Kamar N, Evrard S, de Valk H, Cintas P, Izopet J; HEV study group. Acute hepatitis E in French patients and neurological manifestations. J Infect. 2018;77:220-226. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 51] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 19. | Shah SA, Lal A, Idrees M, Hussain A, Jeet C, Malik FA, Iqbal Z, Rehman Hu. Hepatitis E virus-associated aplastic anaemia: the first case of its kind. J Clin Virol. 2012;54:96-97. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 38] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Ripellino P, Pasi E, Melli G, Staedler C, Fraga M, Moradpour D, Sahli R, Aubert V, Martinetti G, Bihl F, Bernasconi E, Terziroli Beretta-Piccoli B, Cerny A, Dalton HR, Zehnder C, Mathis B, Zecca C, Disanto G, Kaelin-Lang A, Gobbi C. Neurologic complications of acute hepatitis E virus infection. Neurol Neuroimmunol Neuroinflamm. 2020;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 21] [Cited by in RCA: 40] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 21. | Hoefer J, Ulmer H, Kilo J, Margreiter R, Grimm M, Mair P, Ruttmann E; Innsbruck Liver-in-Heart-Failure Program. Antithrombin III is associated with acute liver failure in patients with end-stage heart failure undergoing mechanical circulatory support. J Thorac Cardiovasc Surg. 2017;153:1374-1382. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 22. | Aslan AT, Balaban HY. Hepatitis E virus: Epidemiology, diagnosis, clinical manifestations, and treatment. World J Gastroenterol. 2020;26:5543-5560. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 61] [Cited by in RCA: 113] [Article Influence: 22.6] [Reference Citation Analysis (4)] |
| 23. | Duseja A, Singh SP. Toward a Better Definition of Acute-on-Chronic Liver Failure. J Clin Exp Hepatol. 2017;7:262-265. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Jalan R, Gines P, Olson JC, Mookerjee RP, Moreau R, Garcia-Tsao G, Arroyo V, Kamath PS. Acute-on chronic liver failure. J Hepatol. 2012;57:1336-1348. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 447] [Cited by in RCA: 456] [Article Influence: 35.1] [Reference Citation Analysis (1)] |
| 25. | Frias M, López-López P, Rivero A, Rivero-Juarez A. Role of Hepatitis E Virus Infection in Acute-on-Chronic Liver Failure. Biomed Res Int. 2018;2018:9098535. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 20] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 26. | Kumar M, Sharma BC, Sarin SK. Hepatitis E virus as an etiology of acute exacerbation of previously unrecognized asymptomatic patients with hepatitis B virus-related chronic liver disease. J Gastroenterol Hepatol. 2008;23:883-887. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 60] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 27. | Shalimar, Kedia S, Mahapatra SJ, Nayak B, Gunjan D, Thakur B, Acharya SK. Severity and Outcome of Acute-on-Chronic Liver Failure is Dependent on the Etiology of Acute Hepatic Insults: Analysis of 368 Patients. J Clin Gastroenterol. 2017;51:734-741. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 28. | Khuroo MS, Kamili S. Aetiology and prognostic factors in acute liver failure in India. J Viral Hepat. 2003;10:224-231. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 126] [Cited by in RCA: 96] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 29. | Chen C, Zhang SY, Zhang DD, Li XY, Zhang YL, Li WX, Yan JJ, Wang M, Xun JN, Lu C, Ling Y, Huang YX, Chen L. Clinical features of acute hepatitis E super-infections on chronic hepatitis B. World J Gastroenterol. 2016;22:10388-10397. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 22] [Cited by in RCA: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 30. | Wang Y, Liu H, Liu S, Yang C, Jiang Y, Wang S, Liu A, Peppelenbosch MP, Kamar N, Pan Q, Zhao J. Incidence, predictors and prognosis of genotype 4 hepatitis E related liver failure: A tertiary nested case-control study. Liver Int. 2019;39:2291-2300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 31. | Wallace SJ, Swann R, Donnelly M, Kemp L, Guaci J, Murray A, Spoor J, Lin N, Miller M, Dalton HR, Hussaini SH, Gunson R, Simpson K, Stanley A, Fraser A. Mortality and morbidity of locally acquired hepatitis E in the national Scottish cohort: a multicentre retrospective study. Aliment Pharmacol Ther. 2020;51:974-986. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 22] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 32. | Krain LJ, Nelson KE, Labrique AB. Host immune status and response to hepatitis E virus infection. Clin Microbiol Rev. 2014;27:139-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 112] [Cited by in RCA: 106] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 33. | Naik A, Goel A, Agrawal V, Sarangi AN, Chhavi N, Singh V, Jameel S, Aggarwal R. Changes in gene expression in liver tissue from patients with fulminant hepatitis E. World J Gastroenterol. 2015;21:8032-8042. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 8] [Cited by in RCA: 7] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 34. | Prabhu SB, Gupta P, Durgapal H, Rath S, Gupta SD, Acharya SK, Panda SK. Study of cellular immune response against Hepatitis E virus (HEV). J Viral Hepat. 2011;18:587-594. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 53] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 35. | Srivastava R, Aggarwal R, Bhagat MR, Chowdhury A, Naik S. Alterations in natural killer cells and natural killer T cells during acute viral hepatitis E. J Viral Hepat. 2008;15:910-916. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 54] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 36. | Possamai LA, Antoniades CG, Anstee QM, Quaglia A, Vergani D, Thursz M, Wendon J. Role of monocytes and macrophages in experimental and human acute liver failure. World J Gastroenterol. 2010;16:1811-1819. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 60] [Cited by in RCA: 54] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 37. | Holt MP, Cheng L, Ju C. Identification and characterization of infiltrating macrophages in acetaminophen-induced liver injury. J Leukoc Biol. 2008;84:1410-1421. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 288] [Cited by in RCA: 337] [Article Influence: 19.8] [Reference Citation Analysis (0)] |
| 38. | Das R, Tripathy A. Increased expressions of NKp44, NKp46 on NK/NKT-like cells are associated with impaired cytolytic function in self-limiting hepatitis E infection. Med Microbiol Immunol. 2014;203:303-314. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 39. | Yi RT, Niu YH, Liu HL, Zhang TY, Yang YC, Zhang Y, Yin DL, Chen TY, Zhao YR. Natural Killer Group 2A Expressed on Both Peripheral CD3-CD56+NK Cells and CD3+CD8+T Cells Plays a Pivotal Negative Regulatory Role in the Progression of Hepatitis B Virus-Related Acute-on-Chronic Liver Failure. J Interferon Cytokine Res. 2016;36:689-697. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 40. | Wang Y, Wang W, Shen C, Wang Y, Jiao M, Yu W, Yin H, Shang X, Liang Q, Zhao C. NKG2D modulates aggravation of liver inflammation by activating NK cells in HBV infection. Sci Rep. 2017;7:88. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 21] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 41. | Soehnlein O, Lindbom L. Phagocyte partnership during the onset and resolution of inflammation. Nat Rev Immunol. 2010;10:427-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 685] [Cited by in RCA: 771] [Article Influence: 51.4] [Reference Citation Analysis (0)] |
| 42. | Szabo G, Csak T. Inflammasomes in liver diseases. J Hepatol. 2012;57:642-654. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 339] [Cited by in RCA: 404] [Article Influence: 31.1] [Reference Citation Analysis (0)] |
| 43. | El Costa H, Gouilly J, Abravanel F, Bahraoui E, Peron JM, Kamar N, Jabrane-Ferrat N, Izopet J. Effector memory CD8 T cell response elicits Hepatitis E Virus genotype 3 pathogenesis in the elderly. PLoS Pathog. 2021;17:e1009367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 22] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 44. | Hwang ES, Hong JH, Glimcher LH. IL-2 production in developing Th1 cells is regulated by heterodimerization of RelA and T-bet and requires T-bet serine residue 508. J Exp Med. 2005;202:1289-1300. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 109] [Cited by in RCA: 122] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 45. | Chen D, Wen S, Wu Z, Gu Y, Chen Y, Chen X, Zhang Y, Lin B, Peng L, Zheng Y, Gao Z. Association between effective hepatic blood flow and the severity and prognosis of hepatitis B virus-related acute on chronic liver failure. Eur J Gastroenterol Hepatol. 2021;32:246-254. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |